
DSM-5 CHANGES:
IMPLICATIONS FOR CHILD
SERIOUS EMOTIONAL
DISTURBANCE
DISCLAIMER
SAMHSA provides links to other Internet sites as a service to its users and is not responsible for the availability
or content of these external sites. SAMHSA, its employees, and contractors do not endorse, warrant, or guarantee
the products, services, or information described or offered at these other Internet sites. Any reference to a
commercial product, process, or service is not an endorsement or recommendation by SAMHSA, its employees,
or contractors. For documents available from this server, the U.S. Government does not warrant or assume any
legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus,
product, or process disclosed.
Substance Abuse and Mental Health Services Administration
Center for Behavioral Health Statistics and Quality
Rockville, Maryland 20857
June 2016
This page intentionally left blank
DSM-5 CHANGES:
IMPLICATIONS FOR CHILD
SERIOUS EMOTIONAL
DISTURBANCE
Contract No. HHSS283201000003C
RTI Project No. 0212800.001.108.008.008
RTI Authors:
Heather Ringeisen
Cecilia Casanueva
Leyla Stambaugh
SAMHSA Authors:
Jonaki Bose
Sarra Hedden
RTI Project Director:
David Hunter
SAMHSA Project Officer:
Peter Tice
For questions about this report, please e-mail [email protected].
Prepared for Substance Abuse and Mental Health Services Administration,
Rockville, Maryland
Prepared by RTI International, Research Triangle Park, North Carolina
June 2016
Recommended Citation: Center for Behavioral Health Statistics and Quality.
(2016). 2014 National Survey on Drug Use and Health: DSM-5 Changes:
Implications for Child Serious Emotional Disturbance (unpublished internal
documentation). Substance Abuse and Mental Health Services
Administration, Rockville, MD.
ii
Acknowledgments
This publication was developed for the Substance Abuse and Mental Health Services
Administration (SAMHSA), Center for Behavioral Health Statistics and Quality (CBHSQ), by
RTI International, a trade name of Research Triangle Institute, Research Triangle Park, North
Carolina, under Contract No. HHSS283201000003C. Contributors to this report include Lisa
Colpe and Peggy Barker. At RTI, Michelle Back edited and Roxanne Snaauw formatted the
report.
iii
Table of Contents
Chapter Page
1. Introduction ......................................................................................................................... 1
1.1 Definition of SED ................................................................................................... 1
1.2 Published SED Estimates ........................................................................................ 2
2. DSM-IV to DSM-5 Changes: Overview ............................................................................. 5
2.1 Elimination of the Multi-Axial System and GAF Score ......................................... 5
2.2 Disorder Reclassification ........................................................................................ 5
3. DSM-5 Child Mental Disorder Classification .................................................................... 9
3.1 New Childhood Mental Disorders Added to the DSM-5 ........................................ 9
3.1.1 Social (Pragmatic) Communication Disorder (SCD, under
Neurodevelopmental Disorders) ................................................................. 9
3.1.2 Disruptive Mood Dysregulation Disorder (or DMDD) (under
Depressive Disorders) ............................................................................... 11
3.2 Age-Related Diagnostic Criteria Changes to Mental Disorders in the DSM-5 .... 16
3.2.1 Attention-Deficit/Hyperactivity Disorder (ADHD, under
Neurodevelopmental Disorders ................................................................ 16
3.2.2 Post-traumatic Stress Disorder (PTSD, under Trauma- and
Stressor-Related Disorders) ...................................................................... 20
3.3 Changes to Other Mental Disorders with Minor to No Implication for SED
Prevalence Estimates ............................................................................................ 24
3.3.1 Major Depressive Episode/Disorder (under Depressive Disorders) ......... 24
3.3.2 Persistent Depressive Disorder (formerly Dysthymic Disorder,
under Depressive Disorders) ..................................................................... 25
3.3.3 Manic Episode and Bipolar I Disorder (under Bipolar and Related
Disorders) .................................................................................................. 26
3.3.4 Generalized Anxiety Disorder (under Anxiety Disorders) ....................... 34
3.3.5 Panic Disorder and Agoraphobia (under Anxiety Disorders) ................... 35
3.3.6 Separation Anxiety Disorder (under Anxiety Disorders) ......................... 39
3.3.7 Social Anxiety Disorder (formerly Social Phobia [Social Anxiety
Disorder], under Anxiety Disorders) ........................................................ 40
3.3.8 Conduct Disorder (under Disruptive, Impulse-Control, and
Conduct Disorders) ................................................................................... 42
3.3.9 Oppositional Defiant Disorder (under Disruptive, Impulse-Control,
and Conduct Disorders) ............................................................................ 45
3.3.10 Eating Disorders (under Feeding and Eating Disorders) .......................... 47
3.3.11 Body Dysmorphic Disorder (under Obsessive-compulsive and
Related Disorders) .................................................................................... 52
4. Instrumentation ................................................................................................................. 55
5. Summary and Conclusions ............................................................................................... 59
References ..................................................................................................................................... 61
iv
List of Tables
Table Page
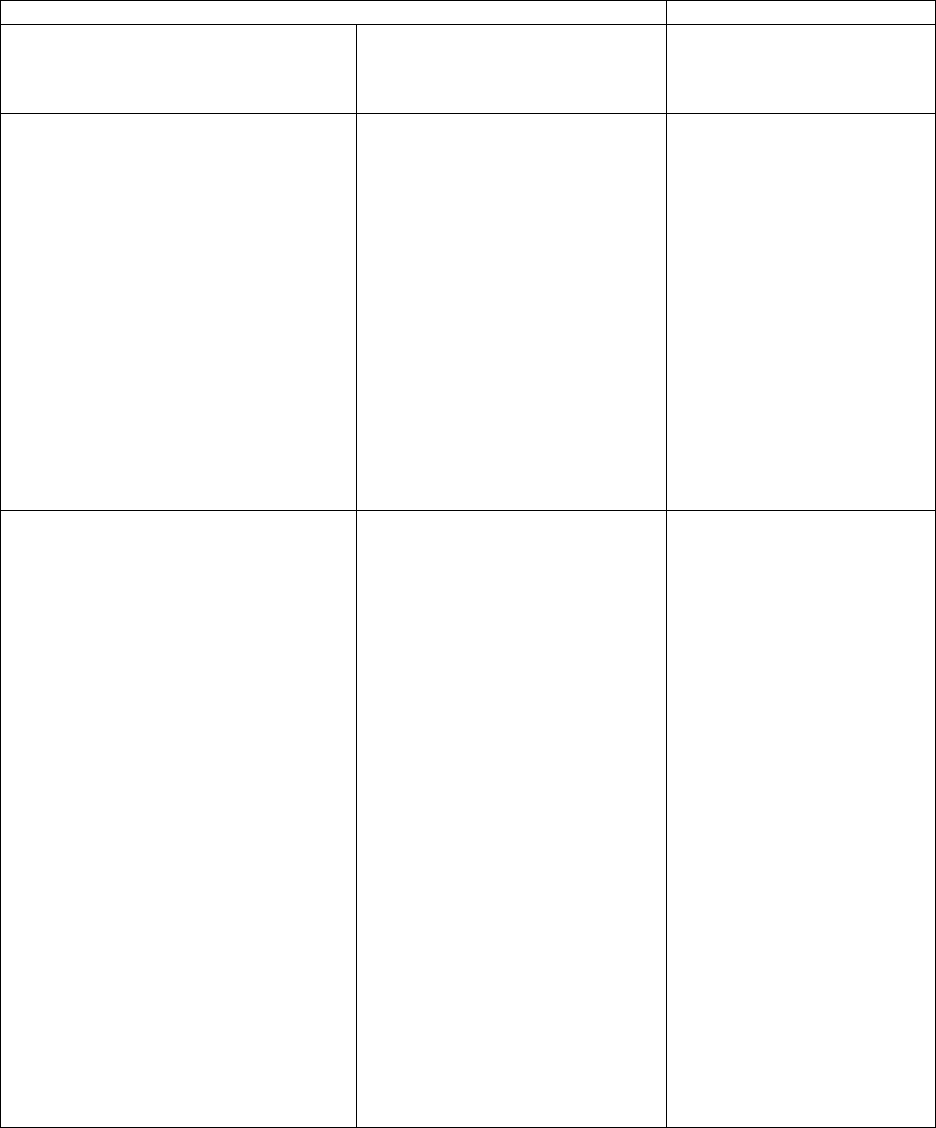
1. DSM-IV Childhood Mental Disorders Assessed in Leading Studies with Published
Estimates of SED ................................................................................................................ 3
2. Past 12-month Prevalence of Mental Disorders Based upon the NCS-A, NHANES
Special Study, and GSMS, by Functional Impairment and Child Age ............................... 4
3. Disorder Classes Presented by the DSM-IV and DSM-5, as Ordered in DSM-IV ............ 6
4. Disorder Classification in the DSM-IV and DSM-5 for Disorders Usually First
Diagnosed in Infancy, Childhood, or Adolescence ............................................................ 7
5. DSM-IV Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS)
to DSM-5 Social (Pragmatic) Communication Disorder (SCD) Comparison .................. 10
6. DSM-IV Bipolar Disorder-Manic Episode and Oppositional Defiant Disorder to
DSM-5 Disruptive Mood Dysregulation Disorder (or DMDD) Comparison ................... 12
7. DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison .................... 17
8. DSM-IV to DSM-5 Post-traumatic Stress Disorder Comparison Children 6 Years
and Younger ...................................................................................................................... 21
9. DSM-IV to DSM-5 Major Depressive Episode/Disorder Comparison ............................ 25
10. DSM-IV to DSM-5 Dysthymic Disorder/Persistent Depressive Disorder
Comparison ....................................................................................................................... 26
11. DSM-IV to DSM-5 Manic Episode Criteria Comparison ................................................ 28
12. DSM-IV to DSM-5 Bipolar I Disorder Comparison ........................................................ 29
13. DSM-IV to DSM-5 Generalized Anxiety Disorder Comparison ..................................... 34
14. Panic Disorder and Agoraphobia Criteria Changes from DSM-IV to DSM-5 ................. 36
15. DSM-IV to DSM-5 Separation Anxiety Disorder Comparison ........................................ 39
16. DSM-IV to DSM-5 Social Phobia/Social Anxiety Disorder Comparison ........................ 41
17. DSM-IV to DSM-5 Conduct Disorder Comparison ......................................................... 43
18. DSM-IV to DSM-5 Oppositional Defiant Disorder Comparison ..................................... 46
19. DSM-IV to DSM-5 Anorexia Nervosa Comparison ........................................................ 48
20. DSM-IV to DSM-5 Bulimia Nervosa Comparison .......................................................... 49
21. DSM-IV to DSM-5 Binge Eating Disorder Comparison .................................................. 50
22. DSM-IV to DSM-5 Avoidant/Restrictive Food Intake Disorder Comparison ................. 52
23.
D
SM-IV to DSM-5 Body Dysmorphic Disorder Comparison ......................................... 54
24. Summary of Diagnostic Instruments Used to Assess Child Mental Disorders ................ 55
v
This page intentionally left blank
1
1. Introduction
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the manual used by
clinicians and researchers to diagnose and classify mental disorders (including substance use
disorders [SUDs]). The DSM specifically classifies child disorders by symptoms, duration, and
functional impact across home, school, and other community settings. The American Psychiatric
Association (APA) published the DSM-5 in 2013, culminating a 14-year revision process. This
latest revision takes a new approach to defining the criteria for mental disorders—a lifespan
perspective. This perspective is very relevant to diagnosing childhood mental disorders. The
perspective recognizes the importance of age and development in the onset, manifestation, and
treatment of mental disorders. The purpose of this report is to describe the differences between
the DSM-IV and DSM-5 diagnostic criteria that could affect national estimates of childhood
serious emotional disturbance (SED). The report also provides a description of DSM-5 updates
that have been made (or are being made) to existing diagnostic instruments and screeners of
childhood emotional and behavioral health.
1.1 Definition of SED
The DSM has never offered a definition of SED. This term has been defined historically
by the Substance Abuse and Mental Health Services Administration (SAMHSA) and released as
a Federal Register notice. The SAMHSA definition was crafted in order to inform state block
grant allocations for community mental health services provided to children with an SED and
adults with a serious mental illness (SMI). The Federal Register definition is intended to identify
and estimate the size of the group of children with SED within the general population of each
state. An accurate and up-to-date estimate of childhood SED is critical for SAMHSA to plan
future block grant allocations and financial supports to states serving children with SED.
The Federal Register notice defines the terms "children with a serious emotional
disturbance" and "adults with a serious mental illness" (SAMHSA, 1993, p. 29422). Pub. L. 102-
321 defines children with an SED to be people "from birth up to age 18 who currently or at any
time during the past year have had a diagnosable mental, behavioral, or emotional disorder of
sufficient duration to meet diagnostic criteria specified within the Diagnostic and Statistical
Manual of Mental Disorders, Third Edition, Revised (DSM-III-R; American Psychiatric
Association, 1987) that resulted in functional impairment, which substantially interferes with or
limits the child's role or functioning in family, school, or community activities" (SAMHSA,
1993, p. 29425).
The 1992 and 1993 Federal Register notices also offer several notes that are helpful in
considering the age, symptom duration, and diagnostic exclusions related to the definition of
childhood SED:
• Age: "Although the definition of SED in children is restricted to persons up to age 18, it
is recognized that some states extend this age range to persons less than age 22. To
accommodate this variability, states using an extended age range for children's services
should provide separate estimates for persons below age 18 and persons aged 18 to 22
within block grant applications" (SAMHSA, 1993, p. 29425).
2
• Duration: "The reference year…refers to a continuous 12-month period because this is a
frequently used interval in epidemiological research and because it relates to commonly
used [state] planning cycles" (SAMHSA, 1993, p. 29425).
• Diagnostic exclusions: "These disorders include any mental disorders listed in the DSM-
III-R…with the exception of DSM-III-R "V" codes, substance use and developmental
disorders, which are excluded unless they co-occur with another diagnosable serious
emotional disturbance" (SAMHSA, 1993, p. 29425).
A November 6, 1992, Federal Register notice requests public comments to a preliminary
definition of childhood SED (SAMHSA, 1992). The May 20, 1993, Federal Register describes
responses to public comments received in response to the 1992 notice. Public comments to the
proposed SED definition primarily focused on the impairment criteria, with support for
considering a broad definition of impairment and also concerns that including less impairing
disorders would dilute resources for those with the most severely debilitating conditions. A
smaller set of comments focused on the inclusion or exclusion of certain disorders such as
substance abuse, developmental disorders, and attention deficit disorder.
The 1993 Federal Register offers clarification on final decisions about disorders to be
included and excluded in the SED definition. Public comments included concerns about whether
attention-deficit disorder (ADD) should be included for two main reasons: (1) parental concerns
about the negative stigma associated with labelling ADD as a "serious emotional disturbance"
and (2) treatment providers/educators noting difficulties making definitive ADD diagnoses.
Ultimately, ADD was included in the definition of SED because "a significant group of children
with functional impairments associated with this disorder might otherwise be excluded from
service" (p. 29423). SUDs were excluded based upon the rationale that the federal government
administered a separate state block grant intended to fund substance abuse treatment and
prevention services. Developmental disorders (mental retardation, autism, pervasive
developmental disorders) were also excluded. The rationale described for this decision was as
follows: "while comments received cited the frequent involvement of mental health practitioners
in treatment planning and service delivery for these individuals (particularly autistic children),
separate Federal block grant funds and processes for needs assessment cover these population
groups" (SAMHSA, 1993, p. 29424). Finally, DSM-III "V" codes were excluded because "they
represent conditions that may be a focus of treatment but are not attributed to a mental disorder"
(p. 29424).
In summary, DSM mental disorder classifications are relevant to SED as they form the
basis for an essential part of the SED criteria—the presence of a DSM-based mental disorder.
Changes in the number of mental disorders (as defined by the DSM) that fall under the
operationalized definition of SED, and breadth of the diagnostic criteria for existing DSM-based
mental disorders might impact the prevalence rates of SED. The current operationalized
definition of SED may need to be updated to ensure consistent and precise measurement of the
prevalence of SED within epidemiological studies at the national level.
1.2 Published SED Estimates
Three large-scale epidemiological studies have provided estimates of SED based upon
the administration of child and adolescent diagnostic interviews. These studies include a

3
supplemental study to the National Health and Nutrition Examination Survey (NHANES;
Merikangas et al., 2010), the National Comorbidity Survey Adolescent Cohort (NCS-A; Kessler
et al., 2012), and the Great Smoky Mountain Study (GSMS; Costello, Mustillo, Erkanli, Keeler,
& Angold, 2003). These three studies assess slightly different age groups, use different
diagnostic instruments, and include the assessment of slightly different childhood mental
disorders (see Table 1). The disorders assessed in these studies reflect diagnostic categories to be
considered when estimating the prevalence of SED.
Table 1. DSM-IV Childhood Mental Disorders Assessed in Leading Studies with Published
Estimates of SED
Disorder
Category
NCS-A (13–17 years)
Composite International
Diagnostic Interview
(CIDI)
NHANES (8–15 years)
Diagnostic Interview
Schedule for Children
(DISC)
GSMS (9–16 years)
Child and Adolescent
Psychiatric Assessment
(CAPA)
Mood
Disorder
Major depression
Dysthymia
Bipolar disorder
Major depression
Dysthymia
Major depression
Dysthymia
Bipolar disorder
Mania
Depression NOS
Anxiety
Disorders
Generalized anxiety disorder
Panic disorder
Agoraphobia
Specific phobia
Separation anxiety disorder
Posttraumatic stress disorder
Social phobia
Generalized anxiety disorder
Panic disorder
Generalized anxiety disorder
Panic disorder
Agoraphobia
Simple phobia
Separation anxiety disorder
Posttraumatic stress disorder
Obsessive compulsive
disorder
Behavior
Disorders
ADHD
Conduct disorder
Oppositional defiant disorder
ADHD
Conduct disorder
ADHD
Conduct disorder
Oppositional defiant disorder
Substance
Disorders
Alcohol abuse
Drug abuse
Alcohol abuse
Drug abuse
Other Eating disorders Eating disorder Eating disorders
Trichotillomania
Enuresis
Encopresis
Psychosis
ADHD = attention-deficit/hyperactivity disorder; NOS = not otherwise specified.
Each study defines SED to include any assessed DSM-IV Axis I disorder. The R.C.
Kessler et al. (2012) and Costello et al. (2003) publications include substance disorders within
the SED estimates, while the Federal Register definition of SED excludes substance abuse.
"Serious functional impairment" is defined differently in each study based upon how the study's
diagnostic interview measured impairment. One study, (Costello et al., 2003), defined SED using
the Child and Adolescent Psychiatric Assessment (CAPA) as any Axis I disorder with
"significant functional impairment." CAPA-based definitions of SED include a child who
(1) meets diagnostic criteria for at least one of the assessed Axis I disorders by parent or child
report, and (2) has a report of any partial or severe impairment rating by parent or child report

4
(personal communication with G. Keeler, October 2012). R.C. Kessler et al. (2012) defined the
serious impairment criteria for SED as a Children's Global Assessment Scale (CGAS) score of
50 or less (having moderate functional impairment in most areas of living or severe impairment
in at least one area). Moderate impairment was defined as one or more Axis I disorders plus a
CGAS score of 51 to 60 (variable functioning with sporadic difficulties in several but not all
areas of living). Meanwhile, Merikangas and colleagues (2010) operationalized four levels of
impairment for each disorder assessed: level A, intermediate or severe rating on ≥ one question;
level B, intermediate or severe rating on ≥ two questions (level A and B are not mutually
exclusive); level C, severe rating on ≥ one question; and level D (severe impairment), included
meeting criteria for either level B or C. Impairment items assessed impairment in six domains,
including interference with the respondent's own life, family life, social life, peers, teachers, and
school performance. "Any DSM-IV Disorder with Severe Impairment," or SED, was defined as a
case with level D impairment.
These definitions of SED result in prevalence estimates that range from 6.8 to 11.5
percent depending on the study and age of children included (see Table 2). The following
sections of this report describe how recent updates to the DSM may or may not result in likely
changes to these prevalence estimates of SED. This report does not summarize DSM-IV to
DSM-5 changes to SUDs since they are excluded from the Federal Register definition of SED.
Another SAMSHA report Impact of the DSM-IV to DSM-5 Conversion on the National Survey
on Drug Use and Health and the Mental Health Surveillance Study includes a detailed
description of changes from DSM-IV to DSM-5 for SUDs among youths aged 12 to 17 years
(Center for Behavioral Health Statistics and Quality, in review).
Table 2. Past 12-month Prevalence of Mental Disorders Based upon the NCS-A, NHANES
Special Study, and GSMS, by Functional Impairment and Child Age
Prevalence Estimate (%, SE)
NCS-A (13-17 years)
Past 12 Months
NHANES Special
Study (12-15
years)
Past 12 Months
NHANES Special
Study (8-11 years)
Past 12 Months
GSMS (9-16
years)
Past 3 Months
Any DSM-IV
Disorder
42.6 (1.2) 13.4 (1.2) 12.8 (1.3) 13.3
SED (and
associated
definition)
8.0 (1.3)
Moderate impairment
rating in most areas of
living or severe in 1
area
11.5 (1.3)
Level A or B:
Intermediate
impairment rating on
2 of 6 items or at
least 1 severe rating
11.0 (1.1)
Level A or B:
Intermediate
impairment rating on
2 of 6 items or at
least 1 severe rating
6.8
Any Axis I plus
"significant
functional
impairment"
Disorder with
moderate or
severe
impairment in
any area of living
17.8 (n/a)
Moderate impairment
was defined as variable
functioning, with
sporadic difficulties in
several, but not all
areas of living.
Not provided Not provided Not provided
5
2. DSM-IV to DSM-5 Changes: Overview
The American Psychiatric Association (APA) published the DSM-5 in 2013. This latest
revision takes a lifespan perspective recognizing the importance of age and development on the
onset, manifestation, and treatment of mental disorders. Other changes in the Diagnostic and
Statistical Manual of Mental Disorders, 5th ed. (DSM-5) include eliminating the multi-axial
system; removing the Global Assessment of Functioning (GAF score); reorganizing the
classification of the disorders; and changing how disorders that result from a general medical
condition are conceptualized. Many of these general changes from Diagnostic and Statistical
Manual of Mental Disorders, 4th ed. (DSM-IV) to DSM-5 are summarized in the report Impact
of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. This report
will supplement that information by providing details specifically about changes to disorders of
childhood and their implications for generating estimates of child serious emotional disturbance
(SED).
2.1 Elimination of the Multi-Axial System and GAF Score
One of the key changes from DSM-IV to DSM-5 is the elimination of the multi-axial
system. DSM-IV approached psychiatric assessment and organization of biopsychosocial
information using a multi-axial formulation (American Psychiatric Association, 2013b). There
were five different axes. Axis I consisted of mental health and substance use disorders (SUDs);
Axis II was reserved for personality disorders and mental retardation; Axis III was used for
coding general medical conditions; Axis IV was to note psychosocial and environmental
problems (e.g., housing, employment); and Axis V was an assessment of overall functioning
known as the GAF. The GAF scale was dropped from the DSM-5 because of its conceptual lack
of clarity (i.e., including symptoms, suicide risk, and disabilities in the descriptors) and
questionable psychometric properties (American Psychiatric Association, 2013b).
Although the impact of removing the overall multi-axial structure in DSM-5 is unknown,
there is concern among clinicians that eliminating the structured approach for gathering and
organizing clinical assessment data will hinder clinical practice (Frances, 2010). However, the
direct impact on the prevalence rates of childhood mental disorders is likely to be negligible as it
will not affect the characteristics of diagnoses.
2.2 Disorder Reclassification
DSM-IV and DSM-5 categorize disorders into "classes" with the intent of grouping
similar disorders (particularly those that are suspected to share etiological mechanisms or have
similar symptoms) to help clinician and researchers use of the manual. From DSM-IV to DSM-5,
there has been a reclassification of many disorders that reflects a better understanding of the
classifications of disorders from emerging research or clinical knowledge. Table 3 lists the
disorder classes included in DSM-IV and DSM-5. In DSM-5, six classes were added and four
were removed. As a result of these changes in the overall classification system, numerous
individual disorders were reclassified from one class to another (e.g., from "mood disorders" to
"bipolar and related disorders" or "depressive disorders"). The reclassification of disorder classes

6
will not have a direct effect on any SED estimation; however, it does warrant consideration when
documenting disorders that may have changed classes.
Table 3. Disorder Classes Presented by the DSM-IV and DSM-5, as Ordered in DSM-IV
DSM-IV DSM-5
1. Disorders usually first diagnosed in infancy,
childhood, or adolescence
Dropped
1
2. Delirium, Dementia, and Amnestic and other
cognitive disorders
17. Neurocognitive Disorders
3. Mental Disorders due to a general medical
condition
Dropped
1
4. Substance-related disorders 16. Substance-Related and Addictive Disorders
5. Schizophrenia and other psychotic disorders 2. Schizophrenia Spectrum and Other Psychotic
Disorders
6. Mood Disorders 3. Bipolar and Related Disorders
4. Depressive Disorders
7. Anxiety Disorders 5. Anxiety Disorders
8. Somatoform Disorders 9. Somatic Symptom and Related Disorders
9. Factitious Disorders Dropped
1
10. Dissociative Disorders 8. Dissociative Disorders
11. Sexual and Gender Identity Disorders 13. Sexual Dysfunctions
14. Gender Dysphoria
19. Paraphilic Disorders
12. Eating Disorders 10. Feeding and Eating Disorders
13. Sleep Disorders 12. Sleep-Wake Disorders
14. Impulse-Control Disorders not elsewhere
classified
15. Disruptive, Impulse-Control, and Conduct Disorders
15. Adjustment Disorders Dropped
1
16. Personality Disorders 18. Personality Disorders
N/A 1. Neurodevelopmental Disorders
N/A 6. Obsessive-Compulsive and Related Disorders
N/A 7. Trauma- and Stressor-Related Disorders
N/A 11. Elimination Disorders
N/A 20. Other Mental Disorders
N/A 21. Medication-Induced Movement Disorders and Other
Adverse Effects of Medication
1
A notation of "dropped" does not imply that the specific disorders were removed; rather the overall classification
is not included in DSM-5. Disorders in those classes were mainly recategorized.
Of particular note for childhood mental disorders, the DSM-5 eliminated a class of
"disorders usually first diagnosed in infancy, childhood, or adolescence." Those disorders are
now placed within other classes. See Table 4 for a summary the new DSM-5 disorder classes for
those disorders formally classified as "disorders usually first diagnosed in infancy, childhood, or
adolescence."

7
Table 4. Disorder Classification in the DSM-IV and DSM-5 for Disorders Usually First
Diagnosed in Infancy, Childhood, or Adolescence
Disorder Types (version) DSM-IV Disorder Class DSM-5 Disorder Class
Mental Retardation (DSM-IV)
Intellectual Disabilities (DSM-5)
Disorders usually first diagnosed in
infancy, childhood, or adolescence
Neurodevelopmental Disorders
Learning Disorders Disorders usually first diagnosed in
infancy, childhood, or adolescence
Neurodevelopmental Disorders
Motor Skills Disorder Disorders usually first diagnosed in
infancy, childhood, or adolescence
Neurodevelopmental Disorders
Communication Disorders Disorders usually first diagnosed in
infancy, childhood, or adolescence
Neurodevelopmental Disorders
Pervasive Developmental Disorders
(DSM-IV)
Autism Spectrum Disorder (DSM-
5)
Disorders usually first diagnosed in
infancy, childhood, or adolescence
Neurodevelopmental Disorders
Attention-Deficit/Hyperactivity
Disorder
Disorders usually first diagnosed in
infancy
Neurodevelopmental Disorders
Conduct Disorder Disorders usually first diagnosed in
infancy
Disruptive, Impulse-Control, and
Conduct Disorders
Oppositional Defiant Disorder Disorders usually first diagnosed in
infancy
Disruptive, Impulse-Control, and
Conduct Disorders
Feeding and Eating Disorders of
Infancy or Early Childhood
Disorders usually first diagnosed in
infancy
Feeding and Eating Disorders
Tic Disorders Disorders usually first diagnosed in
infancy
Neurodevelopmental Disorders
Elimination Disorders Disorders usually first diagnosed in
infancy
Elimination Disorders
Separation Anxiety Disorder Disorders usually first diagnosed in
infancy
Anxiety Disorders
Selective Mutism Disorders usually first diagnosed in
infancy
Anxiety Disorders
Reactive Attachment Disorder Disorders usually first diagnosed in
infancy
Trauma- and Stressor-Related
Disorders
8
This page intentionally left blank
9
3. DSM-5 Child Mental Disorder
Classification
The Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-5) includes
changes to some key disorders of childhood. Two new childhood mental disorders were added in
the DSM-5: social communication disorder (or SCD) and disruptive mood dysregulation disorder
(or DMDD). There were age-related diagnostic criteria changes for two other mental disorder
categories particularly relevant to the definition of serious emotional disturbance (SED):
attention-deficit/hyperactivity disorder (ADHD) and post-traumatic stress disorder (PTSD). An
ADHD diagnosis now requires symptoms to be present prior to the age of 12 (rather than 7, the
age of onset from the Diagnostic and Statistical Manual of Mental Disorders, 4th ed. [DSM-
IV]). PTSD includes a new subtype specifically for children younger than 6 years of age.
Sections 3.1 and 3.2 provide detailed descriptions of these disorders as well as summaries
of the research that has been conducted around their impact on the prevalence of childhood
mental disorders. Other disorders did not have specific DSM-5 changes related to childhood, but
these changes would be relevant to both adults and children (e.g., major depressive disorder
[MDD], generalized anxiety disorder [GAD]). Section 3.3 provides a brief overview of DSM-5
changes to these remaining disorders. In the report sections that follow we reference prevalence
rates found in studies of community samples using the DSM-5. For some disorders, we also
reference prevalence rates in clinical samples where direct comparisons were performed between
DSM-IV and DSM-5 ratings. The prevalence rates from clinical samples are relevant to this
report in demonstrating the magnitude of change that might be expected in prevalence rates from
DSM-IV to DSM-5.
3.1 New Childhood Mental Disorders Added to the DSM-5
3.1.1 Social (Pragmatic) Communication Disorder (SCD, under Neurodevelopmental
Disorders)
Description. The DSM-5 communication disorders include a new condition for persistent
difficulties in the social uses of verbal and nonverbal communication: social (pragmatic)
communication disorder or SCD. SCD is characterized by a primary difficulty with pragmatics—
the social use of language or communication—resulting in functional limitations in effective
communication, social participation, development of social relationships, and academic
achievement (see Table 5 for a description of DSM-5 SCD diagnostic criteria). Symptoms of SCD
include difficulties in the acquisition and use of spoken language and inappropriate responses in
conversation. Although diagnosis is rare for children younger than 4 years old, symptoms must be
present in early childhood even if not recognized until later. Individuals with SCD have never had
effective social communication. This new disorder cannot be diagnosed if social communication
deficits are part of the two main characteristics of the new autism spectrum disorder (ASD). ASD
is characterized by (1) deficits in social communication and social interaction and (2) restricted
repetitive behaviors, interests, and activities (RRBs). Because both components are required for an
ASD diagnosis, SCD is diagnosed if no RRBs are present or there is no past history of RRBs. As
described by the American Psychiatric Association (APA), the symptoms of some patients

10
diagnosed with DSM-IV pervasive developmental disorder not otherwise specified (PDD-NOS)
may meet the DSM-5 criteria for SCD (American Psychiatric Association, 2013c).
Table 5. DSM-IV Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) to
DSM-5 Social (Pragmatic) Communication Disorder (SCD) Comparison
DSM-IV DSM-5
Disorder Class: Pervasive Developmental
Disorders
Disorder Class: Neurodevelopmental Disorders
Severe and pervasive impairment in the
development of reciprocal social interaction or
verbal and nonverbal communication skills, or
when stereotyped behavior, interests, and
activities are present but are not met for a
specific pervasive developmental disorder.
This category includes "atypical autism" (late
age of onset, atypical symptomatology).
A. Persistent difficulties in the social use of verbal and
nonverbal communication as manifested by all of the
following:
1. Deficits in using communication for social purposes
2. Impairment of the ability to change communication to
match context
3. Difficulties for following rules for conversation
(taking turns, use of verbal/nonverbal signs to regulate
interaction)
4. Difficulties understanding what is not explicitly stated
B. The deficits result in functional limitations in effective
communication, social participation, social relationships,
and academic achievement.
C. The onset of the symptoms is in the early development
period, but may not fully manifest until social
communication demands exceed limited capabilities.
D. The symptoms are not attributable to another medical or
neurological condition or to low abilities in the domains
of word structure and grammar, and are not better
explained by autism spectrum disorder, intellectual
disability, or developmental delay.
Estimated Prevalence. Although a few studies have reported empirical support for a
conceptualization of SCD distinguishable from ASD (Gibson, Adams, Lockton, & Green, 2013)
and ADHD (St Pourcain et al., 2011), there is one practitioner review publication describing
concern that the inclusion/exclusion criteria and differential diagnosis with ASD, ADHD, social
anxiety disorders, intellectual disabilities, and developmental delays, may mean that very few
individuals will meet diagnostic criteria for SCD (Norbury, 2014).
No study was found on the general population's prevalence of SCD. In one study that
analyzed three datasets (1) data from the Simons Simplex Collection, a genetic consortium study
focusing on families having just one child with an ASD; (2) the Collaborative Programs of
Excellence in Autism, a multicenter study of ASD; and (3) the University of Michigan Autism
and Communication Disorders Center data bank that included a total of 4,453 children with
DSM-IV clinical PDD diagnoses and 690 with non-PDD diagnoses (e.g., language disorder), the
proposed ASD DSM-5 criteria identified 91 percent of children with clinical DSM-IV PDD
diagnoses (Huerta, Bishop, Duncan, Hus, & Lord, 2012). In this samples of children with DSM-
IV diagnosis for PPD (86.6 percent of the pooled sample) and non-PPD (13.4 percent of the
pooled sample), only 75 of 5,143 (1.5 percent) met social communication criteria for ASD, but
did not meet threshold criteria for RRBs. This study concluded that few children with ASD are
likely to be misclassified as having SCD or will be reclassified as SCD under the DSM-5 (Huerta
11
et al., 2012). In contrast, a second study based on the multisite field trial of the DSM-IV of adults
and children (mean age 9 years old), of which 657 had a clinical diagnosis of PDD and 276 had a
diagnosis other than PDD (mental retardation, language disorders, childhood schizophrenia),
almost 40 percent of cases with a clinical diagnosis of PDD and 71.7 percent of those with PDD-
NOS did not met revised DSM-5 diagnostic criteria for ASD, concluding that proposed DSM-5
criteria could substantially alter the composition and estimate of the autism spectrum
(McPartland, Reichow, & Volkmar, 2012). In the DSM-5 field trials in the United States and
Canada based on child clinical populations (general child psychiatry outpatient services), one of
the sites (Baystate Medical Center, Springfield, MA) found the DSM-IV and DSM-5 prevalence
of ASD was almost the same (23 percent and 24 percent), but a second site (Stanford University
Hospital, Palo Alto, CA) found the prevalence of ASD decreased from 26 percent to 19 percent.
A review of the data (no tables provided in the publication) showed that the decrease at Stanford
was offset by movement into the new SCD diagnosis (Regier et al., 2013).
Overall, these studies suggest that between 1.5 percent to 40 percent or more of children
who would have been classified as PDD before, will not meet diagnostic criteria of ASD under
the DSM-5 and some of them would likely be reclassified as SCD and be included in the SED
estimate, if SCD is part of the SED definition (McPartland, Reichow, & Volkmar, 2012).
It
should be noted that there is concern in the field that SCD could be over diagnosed by speech-
language pathologists. If SCD is treated as a residual category (like the previous PDD-NOS) for
communication disorders diagnosed by speech-language pathologists, children who should be
diagnosed as ASD would be classified as SCD since identifying ASD may prove challenging for
speech-language pathologists (Norbury, 2014).
Implications for Estimate of SED. As SCD would be under the purview of speech-
language pathology, the inclusion/exclusion of SCD on the Federal Register definition of SED
needs to be determined. If SCD is included in the definition of SED, some increase can be
expected in the estimate of SED from the reclassification of children previously classified as
PDD and PDD-NOS to SCD. An additional increase in the SED estimate can be expected from
the diagnoses of SCD by speech-language pathologists if they are not obtaining differential
diagnosis from other professionals.
3.1.2 Disruptive Mood Dysregulation Disorder (or DMDD) (under Depressive Disorders)
Description. DMDD is a new addition to DSM-5 that aims to combine bipolar disorder
that first appears in childhood with oppositional behaviors (Axelson, 2013). DMDD is
characterized by severe and recurrent temper outbursts that are grossly out of proportion in
intensity or duration to the situation. These occur, on average, three or more times each week for
1 year or more (see Table 6 for a description of DSM-5 DMDD diagnostic criteria). The key
feature of DMDD is chronic irritability that is present in between episodes of anger or temper
tantrums. A diagnosis requires symptoms to be present in at least two settings (at home, at
school, or with peers) for 12 or more months, and symptoms must be severe in at least one of
these settings. Onset of DMDD must occur before age 10, and a child must be at least 6 years old
to receive a diagnosis of DMDD. The main driver behind the conceptualization of DMDD was
concern that diagnosis of bipolar disorder was being applied inconsistently across clinicians
because of the disagreement about how to classify irritability in the DSM-IV. In addition,
chronic childhood irritability has not been shown to predict later onset of bipolar disorder,
12
suggesting that irritability may be best contained within a separate mood dysregulation category
(Leigh, Smith, Milavic, & Stringaris, 2012).
Table 6. DSM-IV Bipolar Disorder-Manic Episode and Oppositional Defiant Disorder to DSM-5
Disruptive Mood Dysregulation Disorder (or DMDD) Comparison
DSM-IV Criteria DSM-5
Disorder Class: Mood Disorders
Manic Episode
Disorder Class: Attention-Deficit
and Disruptive Behavior Disorders
Oppositional Defiant Disorder
Disorder Class: Depressive
Disorders
Disruptive Mood
Dysregulation Disorder
A. A distinct period of abnormally and
persistently elevated, expansive, or
irritable mood, lasting at least 1 week
(or any duration if hospitalization is
necessary).
A. A pattern of negativistic, hostile,
and defiant behavior lasting at
least 6 months, during which
four (or more) of the following
are present
1. Often loses temper
2. Often argues with adults
3. Often actively defies or
refuses to comply with
adults' requests or rules
4. Often deliberately annoys
people
5. Often blames others for his
or her mistakes
6. Is often touchy or easily
annoyed by others
7. Is often angry or resentful
8. Is often spiteful or vindictive
A. Severe recurrent temper
outbursts manifested
verbally (e.g., verbal rages)
and or behaviorally (e.g.,
physical aggression) that
are grossly out of
proportion in intensity or
duration to the situation or
provocation
B. During the period of mood
disturbance, three (or more) of the
following symptoms have persisted
(four if the mood is only irritable) and
have been present to a significant
degree:
1. Inflated self-esteem or grandiosity
2. Decreased need for sleep (e.g.,
feels rested after only 3 hours of
sleep)
3. More talkative than usual or
pressure to keep talking
4. Flight of ideas or subjective
experience that thoughts are racing
5. Distractibility (i.e., attention too
easily drawn to unimportant or
irrelevant external stimuli)
6. Increase in goal-directed activity
(either socially, at work or school,
or sexually) or psychomotor
agitation
7. Excessive involvement in
pleasurable activities that have a
high potential for painful
consequences (e.g., engaging in
unrestrained buying sprees, sexual
indiscretions, or foolish business
investments)
B. The temper outbursts are
inconsistent with
developmental level
(continued)

13
Table 6. DSM-IV Bipolar Disorder-Manic Episode and Oppositional Defiant Disorder to DSM-5
Disruptive Mood Dysregulation Disorder (or DMDD) Comparison (continued)
DSM-IV Criteria DSM-5
Disorder Class: Mood Disorders
Manic Episode
Disorder Class: Attention-Deficit
and Disruptive Behavior Disorders
Oppositional Defiant Disorder
Disorder Class: Depressive
Disorders
Disruptive Mood
Dysregulation Disorder
C. The temper outbursts
occur, on average, three or
more times per week.
D. The mood between temper
outbursts is persistently
irritable or angry most of
the day, nearly every day,
and it is observable by
others
E. Criteria A-D have been
present for 12 or more
months. Throughout that
time, the individual has not
had a period lasting 3 or
more consecutive months
without all of the
symptoms in criteria A-D.
D. The mood disturbance is sufficiently
severe to cause marked impairment in
occupational functioning or in usual
social activities or relationships with
others, or to necessitate
hospitalization to prevent harm to self
or others, or there are psychotic
features.
B. The disturbance in behavior
causes clinically significant
impairment in social, academic,
or occupational functioning
F. Criteria A-D are present in
at least two of three
settings
(home/school/peers) and
are severe in at least one
setting
D. Criteria are not met for conduct
disorder, and if the individual is
age 18 years or older, criteria are
not met for Antisocial
Personality Disorder.
G. The diagnosis should not
be made for the first time
before age 6 or after 18
H. The age oat onset of
criteria A-E is before 10
years
(continued)

14
Table 6. DSM-IV Bipolar Disorder-Manic Episode and Oppositional Defiant Disorder to DSM-5
Disruptive Mood Dysregulation Disorder (or DMDD) Comparison (continued)
DSM-IV Criteria DSM-5
I. There has never been a
distinct period lasting more
than 1 day during which
the full symptom criteria,
except duration, for a
manic or hypomanic
episode have been met.
Note: Developmentally
appropriate mood elevation,
such as occurs in the context of
a highly positive event or its
anticipation, should not be
considered as a symptom of
mania or hypomania.
Disorder Class: Mood Disorders
Manic Episode
Disorder Class: Attention-Deficit
and Disruptive Behavior Disorders
Oppositional Defiant Disorder
Disorder Class: Depressive
Disorders
Disruptive Mood
Dysregulation Disorder
J. The behaviors do not occur
exclusively during an
episode of major
depressive disorder and are
not better explained by
another mental disorder
(e.g., autism spectrum
disorder, PTSD, separation
anxiety disorder).
C. The behaviors do not occur
exclusively during the course of
a Psychotic or Mood Disorder
Note: This diagnosis cannot
coexist with oppositional
defiant disorder, intermittent
explosive disorder, or bipolar
disorder, thought it can coexist
with others, including major
depressive disorder, ADHD,
conduct disorder, and
substance use disorders
(SUDs). Individuals whose
symptoms meet criteria for
both DMDD and oppositional
defiant disorder (ODD) should
only be given the diagnosis of
DMDD. If an individual has
ever experienced a manic or
hypomanic episode, the
diagnosis o DMDD should not
be assigned.
(continued)

15
Table 6. DSM-IV Bipolar Disorder-Manic Episode and Oppositional Defiant Disorder to DSM-5
Disruptive Mood Dysregulation Disorder (or DMDD) Comparison (continued)
DSM-IV Criteria DSM-5
E. The symptoms are not due to the
direct physiological effects of a
substance (e.g., a drug of abuse, a
medication, or other treatment) or a
general medical condition (e.g.,
hyperthyroidism).
Note: Manic-like episodes that are clearly
caused by somatic antidepressant
treatment (e.g., medication,
electroconvulsive therapy, light therapy)
should not count toward a diagnosis of
bipolar I disorder.
K. The symptoms are not
attributable to the
physiological effects of a
substance or to another
medical or neurological
condition
Estimated Prevalence. A study combining data from three community surveys: (1) a
representative sample of 918 preschoolers (aged 2-5) attending a large primary care pediatric
clinic in central North Carolina; (2) a representative sample of 1,420 children aged 9, 11, and 13
years in 11 predominantly rural counties of North Carolina; and (3) representative study of 920
children aged 9 to 17 years from four rural counties in North Carolina, found that prevalence of
DMDD ranges from less than 1 percent to 3.3 percent depending on child age. DMDD is most
prevalent among young children (aged 2 to 5) whose parents report high rates of temper tantrums
and irritable moods (Copeland, Angold, Costello, & Egger, 2013). However, according to
DSM-5, DMDD cannot be diagnosed in children under 6 years old; therefore, the real DSM-5
prevalence in the population will be closer to 1 percent. In the DSM-5 field trials in the United
States and Canada based on child clinical populations (general child psychiatry outpatient
services), estimates for DSM-IV were considered "not applicable because the diagnosis is new to
DSM-5," and the DSM-5 prevalence was 5 percent for Baystate Medical Center, 8 percent for
Columbia, and 15 percent for Colorado (Regier et al., 2013). Importantly, estimates for ODD in
Columbia decreased from 22 percent using DSM-IV to 17 percent using DSM-5, but no
additional analyses were reported to determine if children with ODD under the DSM-IV were
reclassified as DMDD under DSM-5 (Regier et al., 2013).
Implications for Estimate of SED. The comorbidity of DMDD with other disorders is
extremely high as described in the DSM-5, indicating that the prevalence increase in the SED
estimates, if DMDD is included, will not increase as "it is rare to find individuals whose
symptoms meet criteria for DMDD alone" (American Psychiatric Association, 2013b, p. 160).
However, if children have symptoms that meet criteria for ODD or intermittent explosive
disorders and DMDD, only DMDD should be assigned. Thus with this new diagnosis, children
will be reclassified. When all symptom, severity, and frequency criteria are applied, DMDD is
only present in roughly 1 percent of school-aged children (Copeland et al., 2013). DMDD should
include many of the children who would have been diagnosed with bipolar disorder using the
DSM-IV. Because these children would receive the new diagnosis of DMDD instead of ODD or
bipolar disorder, the addition of DMDD to the DSM-5 should not affect prevalence estimates of
SED.
16
3.2 Age-Related Diagnostic Criteria Changes to Mental Disorders in the
DSM-5
3.2.1 Attention-Deficit/Hyperactivity Disorder (ADHD, under Neurodevelopmental
Disorders)
Description. ADHD is a chronic neurodevelopmental disorder according to DSM-5 that
is characterized by a persistent and pervasive pattern of inattention and/or hyperactivity-
impulsivity that interferes with functioning or development. ADHD was placed in the
neurodevelopmental disorders chapter to reflect brain developmental correlates with ADHD and
the DSM-5 decision to eliminate the DSM-IV chapter that includes all diagnoses usually first
made in infancy, childhood, or adolescence. The diagnostic criteria for ADHD in DSM-5 are
similar to those in DSM-IV. The same 18 symptoms noted in the DSM-IV are used, and continue
to be divided into two symptom domains (inattention and hyperactivity/impulsivity), of which at
least six symptoms in one domain are required for diagnosis. The majority of ADHD criteria
changes were geared toward improving detection of ADHD among adults. However, one change
may have relevance to the estimation of SED: the onset criterion has been changed from
"symptoms that caused impairment were present before age 7 years" to "several inattentive or
hyperactive-impulsive symptoms were present prior to age 12." Table 7 shows a comparison
between DSM-IV and DSM-5 diagnostic criteria for ADHD.
Estimated Prevalence. In the DSM-5 field trials in the United States and Canada based on
child clinical populations (general child psychiatry outpatient services), using DSM-IV, ADHD
prevalence at Baystate Medical Center was 59 percent and at Columbia it was 55 percent.
Applying the DSM-5 criteria, the prevalence of ADHD was 69 percent at Baystate and 58
percent at Columbia, representing a 10 percent and 3 percent absolute difference, respectively
(Regier et al., 2013). In a birth cohort study of 2,232 British children who were prospectively
evaluated at ages 7 and 12 years for ADHD, the outcome of extending the age-of-onset criterion
to age 12 resulted in the increase in ADHD prevalence by age 12 years by only 0.1 percent
(Polanczyk et al., 2010). This negligible increase is in line with previous findings indicating that
95 percent of adults with a diagnosis of ADHD recall their symptoms starting before age 12 (R.
C. Kessler et al., 2005).
Implications for Estimate of SED. Some increase can be expected in the SED estimate
based on expanding ADHD criteria in the DSM-5 and more cases might be diagnosed. Based on
studies from community samples comparing DSM-IV and DSM-5 criteria, ADHD is expected to
have a modest increase (under 10 percent absolute difference).

17
Table 7. DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison
DSM-IV DSM-5
Disorder Class: Disorders Usually Diagnosed in
Infancy, Childhood, and Adolescence
Disorder Class: Neurodevelopmental Disorders
A. Either (1) or (2): A. A persistent pattern of inattention and/or
hyperactivity-impulsivity that interferes with
functioning or development, as characterized by
(1) and/or (2):
1. Six (or more) of the following symptoms of
inattention have persisted for at least 6 months to a
degree that is maladaptive and inconsistent with
developmental level:
1. Inattention: Six (or more) of the following
symptoms have persisted for at least 6 months to a
degree that is inconsistent with developmental level
and that negatively impacts directly on social and
academic/occupational activities:
Note: The symptoms are not solely a manifestation of
oppositional behavior, defiance, hostility, or failure to
understand tasks or instructions. For older adolescents
and adults (age 17 or older), at least five symptoms are
required.
Inattention
a. often fails to give close attention to details or makes
careless mistakes in schoolwork, work, or other
activities
a. Often fails to give close attention to details or
makes careless mistakes in schoolwork, at work, or
during other activities (e.g., overlooks or misses
details, work is inaccurate).
b. often has difficulty sustaining attention in tasks or
play activity
b. Often has difficulty sustaining attention in tasks or
play activities (e.g., has difficulty remaining
focused during lectures, conversations, or lengthy
reading).
c. often does not seem to listen when spoken to
directly
c. Often does not seem to listen when spoken to
directly (e.g., mind seems elsewhere, even in the
absence of any obvious distraction).
d. often does not follow through on instructions and
fails to finish schoolwork, chores or duties in the
workplace (not due to oppositional behavior or
failure to understand instructions)
d. Often does not follow through on instructions and
fails to finish schoolwork, chores, or duties in the
workplace (e.g., starts tasks but quickly loses focus
and is easily sidetracked).
e. often has difficulty organizing tasks and activities e. Often has difficulty organizing tasks and activities
(e.g., difficulty managing sequential tasks; difficulty
keeping materials and belongings in order; messy,
disorganized work; has poor time management; fails
to meet deadlines).
f. often avoids, dislikes, or is reluctant to engage in
tasks that require sustained mental effort (such as
schoolwork or homework)
f. Often avoids, dislikes, or is reluctant to engage in
tasks that require sustained mental effort (e.g.,
schoolwork or homework; for older adolescents and
adults, preparing reports, completing forms,
reviewing lengthy papers).
(continued)

18
Table 7. DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Disorders Usually Diagnosed in
Infancy, Childhood, and Adolescence
Disorder Class: Neurodevelopmental Disorders
g. often loses things necessary for tasks or activities
(e.g., toys, school assignments, pencils, books or
tools)
g. Often loses things necessary for tasks or activities
(e.g., school materials, pencils, books, tools, wallets,
keys, paperwork, eyeglasses, mobile telephones).
h. is often easily distracted by extraneous stimuli h. Is often easily distracted by extraneous stimuli (for
older adolescents and adults, may include unrelated
thoughts).
i. is often forgetful in daily activities i. Is often forgetful in daily activities (e.g., doing
chores, running errands; for older adolescents and
adults, returning calls, paying bills, keeping
appointments).
2. Six (or more) of the following symptoms of
hyperactivity-impulsivity have persisted for at least
6 months to a degree that is maladaptive and
inconsistent with developmental level:
2. Hyperactivity and impulsivity: Six (or more) of the
following symptoms have persisted for at least 6
months to a degree that is inconsistent with
developmental level and that negatively impacts
directly on social and academic/occupational
activities:
Note: The symptoms are not solely a manifestation of
oppositional behavior, defiance, hostility, or a failure to
understand tasks or instructions. For older adolescents
and adults (age 17 or older), at least five symptoms are
required.
Hyperactivity
a. Often fidgets with hands or feet or squirms in seat a. Often fidgets with or taps hands or feet or squirms
in seat.
b. Often leaves seat in classroom or in other situations
in which remaining seated is expected
b. Often leaves seat in situations when remaining
seated is expected (e.g., leaves his or her place in
the classroom, in the office or other workplace, or in
other situations that require remaining in place).
c. Often runs about or climbs excessively in situations
in which it is inappropriate (in adolescents or adults,
may be limited to subjective feelings of
restlessness)
c. Often runs about or climbs in situations where it is
inappropriate. (Note: In adolescents or adults, may
be limited to feeling restless).
d. Often has difficulty playing or engaging in leisure
activities quietly
d. Often unable to play or take part in leisure activities
quietly.
e. Is often "on the go" or often acts as if "driven by a
motor"
e. Is often "on the go" acting as if "driven by a motor"
(e.g., is unable to be or uncomfortable being still for
extended time, as in restaurants, meetings; may be
experienced by others as being restless or difficult
to keep up with).
f. Often talks excessively f. Often talks excessively.
Impulsivity
g. Often blurts out answers before questions have been
completed
g. Often blurts out an answer before a question has
been completed (e.g., completes people's sentences;
cannot wait for turn in conversation).
h. Often has difficulty awaiting turn h. Often has trouble waiting his/her turn (e.g., while
waiting in line).
(continued)

19
Table 7. DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Disorders Usually Diagnosed in
Infancy, Childhood, and Adolescence
Disorder Class: Neurodevelopmental Disorders
i. Often interrupts or intrudes on others (e.g., butts
into conversations or games)
i. Often interrupts or intrudes on others (e.g., butts
into conversations, games, or activities; may start
using other people's things without asking or
receiving permission; for adolescents and adults,
may intrude into or take over what others are
doing).
B. Some hyperactive-impulsive or inattentive
symptoms must have been present before age 7
years.
B. Several inattentive or hyperactive-impulsive
symptoms were present before age 12 years.
C. Some impairment from the symptoms is present in
at least two settings (e.g., at school [or work] and at
home).
C. Several inattentive or hyperactive-impulsive
symptoms are present in two or more settings, (e.g.,
at home, school or work; with friends or relatives; in
other activities).
D. There must be clear evidence of clinically
significant impairment in social, academic or
occupational functioning.
D. There is clear evidence that the symptoms interfere
with, or reduce the quality of, social, school, or
work functioning.
E. The symptoms do not occur exclusively during the
course of a pervasive developmental disorder,
schizophrenia, or other psychotic disorders and is
not better accounted for by another mental disorder
(e.g., mood disorder, anxiety disorder, dissociative
disorder, or a personality disorder).
E. The symptoms do not occur exclusively during the
course of schizophrenia or another psychotic
disorder and are not better explained by another
mental disorder (e.g., mood disorder, anxiety
disorder, dissociative disorder, personality disorder,
substance intoxication or withdrawal).
Code based on type:
314.01 Attention-Deficit/Hyperactivity Disorder,
Combined Type: if both Criteria A1 and A2 are met
for the past 6 months
314.00 Attention-Deficit/Hyperactivity Disorder,
Predominantly Inattentive Type: if Criterion A1 is
met but Criterion A2 is not met for the past 6
months
314.01 Attention-Deficit/Hyperactivity Disorder,
Predominantly Hyperactive-Impulsive Type: if
Criterion A2 is met but Criterion A1 is not met for
the past 6 months
Coding note: For individuals (especially adolescents
and adults) who currently have symptoms that no
longer meet full criteria, "In Partial Remission" should
be specified.
Specify whether:
Combined presentation: If enough symptoms of
both criteria inattention and hyperactivity-
impulsivity were present for the past 6 months
Predominantly inattentive presentation: If enough
symptoms of inattention, but not hyperactivity-
impulsivity, were present for the past 6 months
Predominantly hyperactive-impulsive presentation:
If enough symptoms of hyperactivity-impulsivity
but not inattention were present for the past 6
months.
Specify if:
In partial remission: When full criteria were
previously met, fewer than the full criteria have
been met for the past 6 months, and the symptoms
still results in impairment in social, academic, or
occupational functioning.

20
Table 7. DSM-IV to DSM-5 Attention-Deficit/Hyperactivity Disorder Comparison (continued)
DSM-IV DSM-5
Specify current severity:
Mild: Few, if any, symptoms in excess of those
required to make the diagnosis are present, and
symptoms result in no more than minor impairments
in social or occupational functioning.
Moderate: Symptoms or functional impairment
between "mild" and "severe" are present.
Severe: Many symptoms in excess of those required
to make the diagnosis, or several symptoms that are
particularly severe, are present, or the symptoms
result in marked impairment in social or
occupational functioning.
3.2.2 Post-traumatic Stress Disorder (PTSD, under Trauma- and Stressor-Related
Disorders)
Description. DSM-5 criteria for PTSD differ significantly from those in DSM-IV for
children and adolescents. The arousal cluster will now include irritability or angry outbursts and
reckless behaviors. PTSD in the DSM-5 is more developmentally sensitive in that diagnostic
thresholds have been lowered for children and adolescents.
Separate criteria have been added for children aged 6 years or younger. These criteria
have been designed to be more developmentally appropriate for young children by including
caregiver-child–related losses as a main source of trauma and focus on behaviorally expressed
PTSD symptoms. According to the DSM-5, PTSD can develop at any age after 1 year of age.
Clinical re-experiencing can vary according to developmental stage, with young children having
frightening dreams not specific to the trauma. Young children are more likely to express
symptoms through play, and they may lack fearful reactions at the time of exposure or during re-
experiencing phenomena. It is also noted that parents may report a wide range of emotional or
behavioral changes, including a focus on imagined interventions in their play. The preschool
subtype excludes symptoms such as negative self-beliefs and blame, which are dependent on the
ability to verbalize cognitive constructs and complex emotional states. The developmental
preschool PTSD subtype lowers the Cluster C threshold from three to one symptom.
The new criteria were based on Scheeringa and colleagues' proposed alternative
algorithm, which was derived from studies performed in young children using modified DSM-IV
PTSD criteria (Scheeringa, Zeanah, & Cohen, 2011). These studies showed that children's loss of
a parent/caregiver through death, abandonment, foster care placement, and other main caregiver-
related events can be experienced as traumatic events. Given young children's need for a
parent/child relationship to feel safe, caregiver loss may be perceived as a serious threat to a
child's own safety and psychological/physical survival, which is part of the criteria defining a
traumatic event. The relevance of caregiver loss as a source of trauma also applies among older
children, since the loss of parents/caregivers is more associated with trauma than high-magnitude
events, like a motor vehicle crash. One report of children in foster care found that the most
common trauma identified by children aged 6 to12 to their therapists was ''placement in foster

21
care" (Scheeringa et al., 2011). Table 8 shows a comparison between DSM-IV and DSM-5
diagnostic criteria for PTSD.
Estimated Prevalence. Rates of PTSD in preschool children diagnosed with DSM-IV
criteria have been lower than in other age groups. This was in part related to DSM-IV language
stipulating that a child must have an intense response to the event—intense fear, helplessness, or
horror—that in children could be expressed by disorganized or agitated behavior. This language
has been deleted from the DSM-5, because the criterion proved to have no utility in predicting
the onset of PTSD and because the diagnostic criteria were not developmentally informed
(American Psychiatric Association, 2013d). With DSM-IV criteria, even in severely traumatized
young children, the frequencies of PTSD ranged only between 13 percent and 20 percent. With
the new algorithm proposed for DSM-5, 44 percent to 69 percent of children in the same studies
would be diagnosed with PTSD (Scheeringa et al., 2011).
Based on a total of 1,073 parents of children attending a large pediatric clinic that
completed the Child Behavior Checklist Age 1.5-5 Years and a new interviewer-based
psychiatric diagnostic measure (the Preschool Age Psychiatric Assessment), 0.1 percent of 2 to 5
year olds in one study qualified for PTSD under DSM-IV and 0.6 percent qualified with the new
algorithm proposed for DSM-5 (Egger et al., 2006). In other community studies of children 1 to
6 years old recruited after mixed-traumatic events, the estimate for PTSD was 0 to 1.7 percent
using DSM-IV criteria and 10 percent to 26 percent with the proposed DSM-5 algorithm
(Scheeringa et al., 2011).
Table 8. DSM-IV to DSM-5 Post-traumatic Stress Disorder Comparison Children 6 Years and
Younger
DSM-IV: PTSD DSM-5: PTSD
Disorder Class: Anxiety Disorders Disorder Class: Trauma- and Stressor-Related Disorders
A. The person has been exposed to a traumatic
event in which both of the following were
present:
1. The person experienced, witnessed or was
confronted with an event or events that
involved actual or threatened death or
serious injury, or a threat to the physical
integrity of self or others.
2. The person's response involved intense fear,
helplessness, or horror.
Note: In children, this may be expressed instead
by disorganized or agitated behavior.
A. Exposure to actual or threatened death, serious injury, or
sexual violence in one or more of the following ways:
1. Directly experiencing the traumatic event(s).
2. Witnessing, in person, the event(s) as it occurred to
others, especially primary caregivers.
3. Learning that the traumatic event(s) occurred to a
parent or caregiving figure.
Note: Witnessing does not include events that are
witnessed only in electronic media, television, movies,
or pictures.
(continued)

22
Table 8. DSM-IV to DSM-5 Post-traumatic Stress Disorder Comparison Children 6 Years and
Younger (continued)
DSM-IV: PTSD DSM-5: PTSD
Disorder Class: Anxiety Disorders Disorder Class: Trauma- and Stressor-Related Disorders
B. The traumatic event is persistently re-
experienced in one or more of the following
ways.
1. Recurrent and intrusive distressing
recollections of the event, including images
thoughts or perceptions. Note: In young
children, repetitive play may occur in which
themes or aspects of the trauma expressed.
2. Recurrent distressing dreams of the event.
Note: In children, there may be frightening
dreams without recognizable content.
3. Acting or feeling as if the traumatic event
were recurring (includes a sense of reliving
the experience, illusions, hallucinations, and
dissociative flashback episodes, including
those that occur on awakening or when
intoxicated). Note: In young children,
trauma-specific reenactment may occur.
4. Intense psychological distress at exposure to
the internal or external cues that symbolize
or resemble an aspect of the traumatic
event.
5. Physiological reactivity on exposure to
internal or external cues that symbolize or
resemble an aspect of the traumatic event.
B. Presence of one or more of the following intrusion
symptoms associated with the traumatic event(s),
beginning after the traumatic event(s) occurred:
1. Recurrent, involuntary, and intrusive distressing
memories of the traumatic event(s).
Note: Spontaneous and intrusive memories may not
necessarily appear distressing and may be expressed as
play reenactment.
2. Recurrent distressing dreams in which the content
and/or effect of the dream are related to the traumatic
event(s).
3. Dissociative reactions (e.g., flashbacks) in which the
child feels or acts as if the traumatic event(s) were
recurring. (Such reactions may occur on a
continuum, with the most extreme expression being a
complete loss of awareness of present surroundings.)
Such trauma reenactment may occur in play.
4. Intense or prolonged psychological distress at
exposure to internal or external cues that symbolize
or resemble an aspect of the traumatic event(s).
5. Marked psychological reactions to reminders of the
traumatic event(s).
C. Persistent avoidance of stimuli associated with
the trauma and the numbing of general
responsiveness (not present before trauma), as
indicated by three or more of the following:
1. Efforts to avoid thoughts, feelings, or
conversations associated with the trauma.
2. Efforts to avoid the activities, places, or
people that arouse recollections of the
trauma.
3. Inability to recall important aspect of the
trauma.
4. Markedly diminished interest or
participation in significant activities.
5. Feelings of detachment or estrangement
from others.
6. Restricted range of affect (e.g., unable to
have loving feelings).
7. Sense of a foreshortened future (e.g., does
not expect to have a career, marriage,
children, or a normal life span).
C. One or more of the following symptoms, representing
either persistent avoidance of stimuli associated with the
traumatic event(s), or negative alterations in cognitions
and mood associated with the traumatic event, must be
present, beginning after the traumatic event(s) or
worsening after the event.
Persistent avoidance of stimuli
1. Avoidance of or efforts to avoid places or physical
reminders that arouse recollections of the traumatic
event(s).
2. Avoidance of or efforts to avoid people,
conversations, or interpersonal situations that arouse
recollections of the traumatic event(s).
Negative alterations in cognitions
3. Substantially increased frequency of negative
emotional states (e.g., fear, guilt, sadness, shame,
confusion).
4. Markedly diminished interest or participation in
significant activities, including constriction play
5. Social withdrawn behavior
6. Persistent reduction in expression of positive
emotions.
(continued)

23
Table 8. DSM-IV to DSM-5 Post-traumatic Stress Disorder Comparison Children 6 Years and
Younger (continued)
DSM-IV: PTSD DSM-5: PTSD
Disorder Class: Anxiety Disorders Disorder Class: Trauma- and Stressor-Related Disorders
D. Persistent symptoms of increased arousal (not
present before the trauma), as indicated by two
or more of the following:
1. Difficulty falling or staying asleep
2. Irritability or outbursts of anger
3. Difficulty concentrating
4. Hyper vigilance
5. Exaggerated startle response
D. Alterations in arousal and reactivity associated with the
traumatic event(s), beginning or worsening after the
traumatic event(s) occurred, as evidence by two (or
more) of the following:
5. Sleep disturbance (e.g., difficulty falling or staying
asleep or restless sleep).
1. Irritable behavior and angry outbursts (with little or
no provocation) typically expressed as verbal or
physical aggression toward people or objects
(including extreme temper tantrums).
4. Problems with concentration.
2. Hyper-vigilance.
3. Exaggerated startle response.
E. Duration of the disturbance (symptoms in
criteria B, C, and D) is more than 1 month.
E. Duration of the disturbance is more than 1 month.
F. The disturbance causes clinically significant
distress or impairment in social, occupational,
or other important areas of functioning.
F. The disturbance causes clinically significant distress or
impairment in relationships with parents, sibling, peers,
or other caregivers or with school behavior.
Specify if: Acute: if duration of symptoms is less
than 3 months.
Specify if: Chronic: if duration of symptoms is 3
months or more.
DROPPED
Specify whether:
With dissociative symptoms: The individual's symptoms
meet the criteria for post-traumatic stress disorder, and in
addition, in response to the stressor, the individual
experiences persistent or recurrent symptoms of either of the
following:
1. Depersonalization: Persistent or recurrent
experiences of feeling detached from, and as if one
were an outside observer of, one's mental processes
or body (e.g., feeling as though one were in a dream;
feeling a sense of unreality of self or body or of time
moving slowly).
2. Derealization: Persistent or recurrent experiences of
unreality of surroundings (e.g., the world around the
individual is experienced as unreal, dreamlike,
distant, or distorted).
Note: To use this subtype, the dissociative symptoms must
not be attributable to the physiological effects of a substance
(e.g., blackouts) or another medical condition (e.g., complex
partial seizures).
Specify if: With delayed onset: If onset of
symptoms is at least 6 months after the stressor.
Specify if: With delayed expression: If the full diagnostic
criteria are not met until at least 6 months after the event
(although the onset and expression of some symptoms may
be immediate).
24
A study based on a representative population sample of 1,420 children aged 9 to 13 at
baseline and followed annually through age 16 (Great Smoky Mountains Study) found that less
than 0.5 percent met the criteria for full-blown DSM-IV PTSD (lifetime prevalence was 0.1
percent, while the 3-month prevalence was 0.03 percent) (Copeland, Keeler, Angold, & Costello,
2007). Other studies with clinical populations of school-age children exposed to traumatic events
have shown between 4 percent and 52 percent estimates of DSM-IV PTSD, but there is no
equivalent work using these studies to estimate PTSD based on DSM-5 proposed criteria as it
was done for younger children (Scheeringa et al., 2011). It is unknown how the changes
proposed by Scheeringa et al. (2011) on PTSD criteria for school children will impact the
estimate, since some changes will improve applicability, while others may limit it.
Implications for Estimate of SED. Some increase can be expected in the SED estimate
from the inclusion of PTSD criteria in the DSM-5, particularly for younger children.
3.3 Changes to Other Mental Disorders with Minor to No Implication for
SED Prevalence Estimates
Several minor changes have been made to other mental disorders sometimes assessed in
psychiatric epidemiological studies of children and adolescents. These changes are summarized
below, but are largely expected to have little to no impact on SED estimates either because of
minimal DSM-5 changes or their very low base rate in children and adolescents.
3.3.1 Major Depressive Episode/Disorder (under Depressive Disorders)
A major depressive episode (MDE) is characterized by the combination of depressed
mood or loss of interest or pleasure lasting for most of the day, nearly every day for 2 weeks or
more (American Psychiatric Association, 2013b). The primary symptom (depressed mood or loss
of interest/pleasure) must be accompanied by four or more additional symptoms and must cause
clinically significant distress or impairment. The primary difference between MDE and MDD is
that MDD includes all of the criteria for MDE as well as MDE exclusionary criteria for mania
and hypomania.
Changes in the MDE/MDD criteria from DSM-IV to DSM-5 have been minimal. There
have been some changes in the way that "mixed states" are described for diagnostic coding
(mixed states now fall under the specifier "with mixed features"). In addition, the examples
provided to describe a depressed mood have been expanded in DSM-5 from "e.g., feels sad or
empty" (American Psychiatric Association, 1994, p. 327) to "e.g., feels sad, empty, hopeless"
(American Psychiatric Association, 2013b, p. 160). This change in wording has not received
much attention (Uher, Payne, Pavlova, & Perlis, 2013). However, the wording change has the
possibility of increasing the prevalence of MDE/MDD if survey respondents and clinicians were
not already equating feeling hopeless with feeling sad, empty, or depressed.
The more substantive change is that the formal bereavement exclusion for MDE/MDD in
DSM-IV has been removed from DSM-5. The bereavement exclusion criterion has been a
longstanding feature of MDE/MDD, designed to allow clinicians to distinguish between normal
grieving and a mental illness (Fox & Jones, 2013). It has been replaced with text noting that
MDE/MDD should not be confused with normal and appropriate grief but that the presence of

25
bereavement is not prohibitive of an MDE/MDD diagnosis. All MDE/MDD changes are
expected to have minimal impact on the estimation of SED in children and adolescents. Table 9
shows a comparison between DSM-IV and DSM-5 diagnostic criteria for MDE/MDD.
Table 9. DSM-IV to DSM-5 Major Depressive Episode/Disorder Comparison
Criteria
1
DSM-IV DSM-5
2
Class: Mood Disorders
Class: Depressive Disorders
Five or more of the following A Criteria (at least one includes A1 or A2)
A1 Depressed mood—indicated by subjective report or observation by others (in
children and adolescents, can be irritable mood).
A2 Loss of interest or pleasure in almost all activities—indicated by subjective
report or observation by others.
A3 Significant (more than 5 percent in a month) unintentional weight loss/gain or
decrease/increase in appetite (in children, failure to make expected weight gains).
A4 Sleep disturbance (insomnia or hypersomnia).
A5 Psychomotor changes (agitation or retardation) severe enough to be observable
by others.
A6 Tiredness, fatigue, or low energy, or decreased efficiency with which routine
tasks are completed.
A7 A sense of worthlessness or excessive, inappropriate, or delusional guilt (not
merely self-reproach or guilt about being sick).
A8 Impaired ability to think, concentrate, or make decisions—indicated by
subjective report or observation by others.
A9 Recurrent thoughts of death (not just fear of dying), suicidal ideation, or
suicide attempts.
The symptoms cause clinically significant distress or impairment in social,
occupational, or other important areas of functioning.
The symptoms are not due to the direct physiological effects of a substance (e.g., drug
abuse, a prescribed medication's side effects) or a medical condition (e.g.,
hypothyroidism).
The symptoms do not meet criteria for a mixed episode
3
There has never been a manic episode or hypomanic episode.
MDE is not better explained by schizophrenia spectrum or other psychotic disorders.
The symptoms are not better accounted for by bereavement (i.e., after the loss of a
loved one, the symptoms persist for longer than 2 months or are characterized by
marked functional impairment, morbid preoccupation with worthlessness, suicidal
ideation, psychotic symptoms, or psychomotor retardation).
4
1
The symptom must either be new or must have clearly worsened compared with the person's pre-episode status and
must persist most of the day, daily, for at least 2 weeks in a row. Exclude symptoms that are clearly due to a
general medical condition, mood-incongruent delusions, or mood-incongruent hallucinations.
2
Symptom must persist most of the day, daily, for at least 2 weeks in a row, excluding A3 and A9.
3
A mixed episode is characterized by the symptoms of both a major depressive episode and a manic episode
occurring almost daily for at least a 1-week period. This exclusion does not include episodes that are substance
induced (e.g., caffeine) or the side effects of a medication.
4
This differentiation requires clinical judgment based on cultural norms and the individual's history.
3.3.2 Persistent Depressive Disorder (formerly Dysthymic Disorder, under Depressive
Disorders)
Dysthymic disorder is a disorder characterized by a persistently depressed mood that
occurs most of the day, for more days than not, for a period of at least 2 years. In children and
adolescents, mood can be irritable and duration must be at least 1 year (American Psychiatric

26
Association, 2013b). In the DSM-5 it has been re-named persistent depressive disorder. This
name change reflects the consolidation of DSM-IV chronic MDD and dysthymic disorder.
Previously, in DSM-IV, a diagnosis of dysthymic disorder was contraindicated if the patient met
criteria for MDD in the first 2 years after the symptoms arose. In DSM-5 this exclusion has been
removed. This change should have no impact on the estimation of SED because most if not all
adolescents with chronic major depression would be classified as having MDE/MDD, and
therefore would be counted as having SED already. Table 10 shows a comparison between
DSM-IV and DSM-5 diagnostic criteria for dysthymic disorder/persistent depressive disorder.
Table 10. DSM-IV to DSM-5 Dysthymic Disorder/Persistent Depressive Disorder Comparison
DSM-IV DSM-5
Name: Dysthymic Disorder Name: Persistent Depressive Disorder
Class: Mood Disorders Class: Depressive Disorders
Depressed mood for most of the day, for more days
than not, as indicated by subjective account or
observation by others, for at least 2 years.
Same
Note: In children and adolescents, mood can be
irritable and duration must be at least a year.
Presence while depressed of two or more of the
following:
• Poor appetite or overeating
• Insomnia or hypersomnia
• Low energy or fatigue
• Low self-esteem
• Poor concentration or difficulty making
decisions
• Feelings of hopelessness
Same
During the 2 year period of the disturbance, the person
has never been without symptoms from the above two
criteria for more than 2 months at a time.
Same
The disturbance is not better accounted for by MDD or
MDD in partial remission.
Criteria for MDD may be continuously present for 2
years, in which case patients should be given comorbid
diagnoses of persistent depressive disorder and MDD.
There has never been a manic episode, a mixed
episode, or a hypomanic episode and the criteria for
cyclothymia have never been met.
Same
The disturbance does not occur exclusively during the
course of a chronic psychotic disorder.
The symptoms are not better explained by a psychotic
disorder.
The disturbance is not due to the direct physiological
effects of a substance (e.g., a drug of abuse or a
medication) or a general medical condition.
Same
The symptoms cause clinically significant distress or
impairment in important areas of functioning.
Same
3.3.3 Manic Episode and Bipolar I Disorder (under Bipolar and Related Disorders)
Bipolar I disorder, at one time referred to as manic-depressive disorder, is defined by the
occurrence of at least one manic episode, which is a period of abnormally and persistently
elevated, expansive, or irritable mood that is accompanied by increased energy or activity, which
results in clinically significant impairment in functioning or the need for hospitalization
(American Psychiatric Association, 2013b). The prevalence rate of child/adolescent mania and/or
27
bipolar disorder is extremely rare. In the DSM-5 field trials in the United States and Canada
based on child clinical populations (general child psychiatry outpatient services), the combined
bipolar I and II prevalence was 6 percent using DSM-IV and 5 percent using DSM-5. Bipolar I
disorders are characterized by one or more manic episodes or mixed episodes and one or more
MDEs; bipolar II disorders are characterized by one or more MDEs and at least one hypomanic
episode (Regier et al., 2013).
The diagnostic criteria for manic episodes have undergone several changes between
DSM-IV and DSM-5. Criterion A now requires that mood changes are accompanied by
abnormally and persistently goal-directed behavior or energy. Second, wording has been added
to clarify that (1) symptoms must represent a noticeable change from usual behavior, and
(2) these changes have to be present most of the day, nearly every day during the minimum 1-
week duration.
Exclusion criteria for manic episodes have also changed, mania that emerges after
antidepressant treatment can be classified as bipolar I disorder diagnosis in the DSM-5, whereas
this was a substance-induced manic disorder in DSM-IV. The criteria for bipolar I disorder have
also undergone a slight change. However, in DSM-5, these subtypes were converted to specifiers
instead (i.e., specify most recent episode type according to its features).
In addition to the changes in manic episode criteria, there have been changes to the
overall diagnostic criteria for bipolar I disorder. In DSM-IV, bipolar I disorder was diagnosed by
"type," which was characterized by the nature of the most recent episode (bipolar I disorder,
single manic episode; bipolar I disorder, most recent episode hypomanic; bipolar I disorder, most
recent episode manic; bipolar I disorder, most recent episode mixed; bipolar I disorder, most
recent episode depressed; and bipolar I disorder, most recent episode unspecified). Each of these
"types" had slightly varying criteria. In DSM-5, the diagnostic description has been simplified
and these "types" have been relegated to the role of specifiers. Diagnostic procedure indicates
that clinicians should first provide the bipolar I diagnosis then specify the characteristics of the
most recent episode, in addition to several other specifiers. Although important to understanding
the general change in diagnostic approach, these changes are geared toward communicating a
more streamlined diagnostic description rather than reflecting a change in the diagnostic criteria
and will not have an impact on SED prevalence estimates. Table 11 shows a comparison between
DSM-IV and DSM-5 diagnostic criteria for manic episode, and Table 12 shows a comparison
between DSM-IV and DSM-5 diagnostic criteria for bipolar I.

28
Table 11. DSM-IV to DSM-5 Manic Episode Criteria Comparison
DSM-IV Criteria DSM-5 Criteria
Name: Bipolar I Disorder Single Manic Episode Name: Bipolar I Disorder Manic Episode
Class: Bipolar Disorders Class: Bipolar and Related Disorders
A. A distinct period of abnormally and persistently
elevated, expansive, or irritable mood, lasting at
least 1 week (or any duration if hospitalization is
necessary).
A. A distinct period of abnormally and persistently
elevated, expansive, or irritable mood and
abnormally and persistently goal-directed behavior
or energy, lasting at least 1 week and present most of
the day, nearly every day (or any duration if
hospitalization is necessary).
B. During the period of mood disturbance, three (or
more) of the following symptoms have persisted
(four if the mood is only irritable) and have been
present to a significant degree:
B. During the period of mood disturbance and
increased energy or activity, three (or more) of the
following symptoms have persisted (four if the
mood is only irritable) are present to a significant
degree and represent a noticeable change from usual
behavior:
1. Inflated self-esteem or grandiosity 1. Same
2. Decreased need for sleep (e.g., feels rested after
only 3 hours of sleep)
2. Same
3. More talkative than usual or pressure to keep
talking
3. Same
4. Flight of ideas or subjective experience that
thoughts are racing
4. Same
5. Distractibility (i.e., attention too easily drawn to
unimportant or irrelevant external stimuli)
5. Distractibility (i.e., attention too easily drawn to
unimportant or irrelevant external stimuli), as
reported or observed.
6. Increase in goal-directed activity (either
socially, at work or school, or sexually) or
psychomotor agitation
6. Same
7. Excessive involvement in pleasurable activities
that have a high potential for painful
consequences (e.g., engaging in unrestrained
buying sprees, sexual indiscretions, or foolish
business investments)
7. Excessive involvement in activities that have a
high potential for painful consequences (e.g.,
engaging in unrestrained buying sprees, sexual
indiscretions, or foolish business investments).
C. The symptoms do not meet criteria for a mixed
episode.
Dropped
D. The mood disturbance is sufficiently severe to
cause marked impairment in occupational
functioning or in usual social activities or
relationships with others, or to necessitate
hospitalization to prevent harm to self or others, or
there are psychotic features.
C. The mood disturbance is sufficiently severe to cause
marked impairment in social or occupational
functioning or to necessitate hospitalization to
prevent harm to self or others, or there are psychotic
features.
E. The symptoms are not due to the direct
physiological effects of a substance (e.g., a drug of
abuse, a medication, or other treatment) or a general
medical condition (e.g., hyperthyroidism).
D. The episode is not attributable to the direct
physiological effects of a substance (e.g., a drug of
abuse, a medication, or other treatment) or another
medical condition.
Note: Manic-like episodes that are clearly caused by
somatic antidepressant treatment (e.g., medication,
electroconvulsive therapy, light therapy) should not
count toward a diagnosis of bipolar I disorder.
Note: A full manic episode that emerges during
antidepressant treatment (e.g., medication,
electroconvulsive therapy) but persists at fully
syndromal level beyond the physiological effect of that
treatment is sufficient evidence for a manic episode and
therefore a bipolar I diagnosis.

29
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Disorder
Class
Mood Disorders Disorder
Class
Bipolar and Related Disorders
Bipolar
Disorder
DSM-IV specified 6 "types" of bipolar I
disorder:
• Bipolar I disorder, single manic
episode
• Bipolar I disorder, most recent
episode hypomanic
• Bipolar I disorder, most recent
episode manic
• Bipolar I disorder, most recent
episode mixed
• Bipolar I disorder, most recent
episode depressed
• Bipolar I disorder, most recent
episode unspecified
Bipolar I
Disorder
A. Criteria have been met for at
least one manic episode
(Table 11). The manic episode
may have been preceded by and
may be followed by hypomanic
or major depressive episodes
(see Table 9).
B. The occurrence of the manic and
major depressive episode(s) is
not better explained by
schizoaffective disorder,
schizophreniform disorder,
delusional disorder, or other
specified or unspecified
schizophrenia spectrum and
other psychotic disorder.
Note: Major depressive episodes are
common in bipolar I disorder but are
not required for the diagnosis of
bipolar I disorder.
Note: Hypomanic episodes are
common in bipolar I disorder but are
not required for the diagnosis of
bipolar I disorder.
Specify:
With anxious distress
With mixed features
With rapid cycling
With melancholic features
With atypical features
With mood-congruent psychotic
features
With mood-incongruent
psychotic features
With catatonia
With peripartum onset
With seasonal pattern
Specify: Remission status if full
criteria are not currently met for a
manic, hypomanic, or major
depressive episode.
(continued)

30
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison (continued)
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Disorder
Class
Mood Disorders Disorder
Class
Bipolar and Related Disorders
Bipolar I
Disorder,
Single Manic
Episode
A. Presence of only one manic episode
(see Table 11) and no past major
depressive episodes (see Table 9).
Note: Recurrence is defined as either a
change in polarity from depression or an
interval of at least 2 months without
manic symptoms.
B. The manic episode is not better
accounted for by schizoaffective
disorder and is not superimposed on
schizophrenia, schizophreniform
disorder, delusional disorder, or
psychotic disorder not otherwise
specified.
Specify if:
Mixed: if symptoms meet criteria for
a mixed episode
Specify (for current or most recent
episode):
Severity/psychotic/remission
specifiers
With catatonic features
With postpartum onset
Bipolar I episode "types" dropped
from criteria tables, but diagnostic
procedure still includes noting most
recent episode type.
Bipolar I
Disorder,
Most Recent
Episode
Hypomanic
A. Currently (or most recently) in a
hypomanic episode.
B. There has previously been at least one
manic episode or mixed episode.
C. The mood symptoms cause clinically
significant distress or impairment in
social, occupational, or other
important areas of functioning.
D. The mood episodes in Criteria A and
B are not better accounted for by
schizoaffective disorder and are not
superimposed on schizophrenia,
schizophreniform disorder, delusional
disorder, or psychotic disorder not
otherwise specified.
Specify:
Longitudinal course specifiers (with
and without interepisode recovery)
With seasonal pattern (applies only to
the pattern of major depressive
episodes)
With rapid cycling
Bipolar I episode "types" dropped
from criteria tables, but diagnostic
procedure still includes noting most
recent episode type.
(continued)

31
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison (continued)
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Disorder
Class
Mood Disorders Disorder
Class
Bipolar and Related Disorders
Bipolar I
Disorder,
Most Recent
Episode
Manic
A. Currently (or most recently) in a
manic episode.
B. There has previously been at least one
major depressive episode, manic
episode, or mixed episode.
C. The mood episodes in Criteria A and
B are not better accounted for by
schizoaffective disorder and are not
superimposed on schizophrenia,
schizophreniform disorder, delusional
disorder, or psychotic disorder not
otherwise specified.
Specify (for current or most recent
episode):
Severity/psychotic/remission
specifiers
With catatonic features
With postpartum onset
Specify:
Longitudinal course specifiers (with
and without interepisode recovery)
With seasonal pattern (applies only to
the pattern of major depressive
episodes)
With rapid cycling
Bipolar I episode "types" dropped
from criteria tables, but diagnostic
procedure still includes noting most
recent episode type.
(continued)

32
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison (continued)
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Bipolar I
Disorder,
Most Recent
Episode
Mixed
A. Currently (or most recently) in a
mixed episode.
B. There has previously been at least one
major depressive episode, manic
episode, or mixed episode.
C. The mood episodes in Criteria A and
B are not better accounted for by
schizoaffective disorder and are not
superimposed on schizophrenia,
schizophreniform disorder, delusional
disorder, or psychotic disorder not
otherwise specified.
Specify (for current or most recent
episode):
Severity/psychotic/remission
specifiers
With catatonic features
With postpartum onset
Specify:
Longitudinal course specifiers (with
and without interepisode recovery)
With seasonal pattern (applies only to
the pattern of major depressive
episodes)
With rapid cycling
Bipolar I episode "types" dropped
from criteria tables, but diagnostic
procedure still includes noting most
recent episode type.
(continued)

33
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison (continued)
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Disorder
Class
Mood Disorders Disorder
Class
Bipolar and Related Disorders
Bipolar I
Disorder,
Most Recent
Episode
Depressed
A. Currently (or most recently) in a
major depressive episode.
Bipolar I episode "types" dropped
from criteria tables, but diagnostic
procedure still includes noting most
recent episode type.
B. There has previously been at least one
manic episode or mixed episode.
C. The mood episodes in Criteria A and
B are not better accounted for by
schizoaffective disorder and are not
superimposed on schizophrenia,
schizophreniform disorder, delusional
disorder, or psychotic disorder not
otherwise specified.
Specify (for current or most recent
episode):
Severity/psychotic/remission
specifiers
Chronic
With catatonic features
With melancholic features
With atypical features
With postpartum onset
Specify:
Longitudinal course specifiers (with
and without interepisode recovery)
With seasonal pattern (applies only to
the pattern of major depressive
episodes)
With rapid cycling
Bipolar I
Disorder,
Most Recent
Episode
Unspecified
A. Criteria, except for duration, are
currently (or most recently) met for a
manic, a hypomanic, a mixed, or a
major depressive episode.
B. There has previously been at least one
manic episode or mixed episode.
C. The mood symptoms cause clinically
significant distress or impairment in
social, occupational, or other
important areas of functioning.
D. The mood symptoms in Criteria A
and B are not better accounted for by
schizoaffective disorder and are not
superimposed on schizophrenia,
schizophreniform disorder, delusional
disorder, or psychotic disorder not
otherwise specified.
(continued)

34
Table 12. DSM-IV to DSM-5 Bipolar I Disorder Comparison (continued)
DSM-IV
Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Disorder
Class
Mood Disorders Disorder
Class
Bipolar and Related Disorders
E. The mood symptoms in Criteria A
and B are not due to the direct
physiological effects of a substance
(e.g., a drug of abuse, a medication,
or other treatment) or a general
medical condition (e.g.,
hyperthyroidism).
Specify:
Longitudinal course specifiers (with
and without interepisode recovery)
With seasonal pattern (applies only to
the pattern of major depressive
episodes)
With rapid cycling
Dropped
3.3.4 Generalized Anxiety Disorder (under Anxiety Disorders)
Generalized anxiety disorder (GAD) is an anxiety disorder characterized by excessive
anxiety and worry that is not focused on a single trigger (e.g., fear of social situations, fear of
having a panic attack, or fear of a specific event/situation). There have been very few changes
made to GAD criteria in DSM-5. The DSM-IV criteria for GAD included that the anxiety and
worry does not occur exclusively during PTSD, a mood disorder, a psychotic disorder, or PDD.
In DSM-5, this has been replaced with text indicating that "the disturbance is not better
explained by another mental disorder." This will have no impact on any estimate of SED
prevalence. Table 13 shows a comparison between DSM-IV and DSM-5 diagnostic criteria for
generalized anxiety disorder.
Table 13. DSM-IV to DSM-5 Generalized Anxiety Disorder Comparison
DSM-IV DSM-5
Disorder Class: Anxiety Disorders SAME
A. Excessive anxiety and worry (apprehensive expectation),
occurring more days than not for at least 6 months,
about a number of events or activities (such as work or
school performance).
SAME
B. The person finds it difficult to control the worry. SAME
(continued)

35
Table 13. DSM-IV to DSM-5 Generalized Anxiety Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Anxiety Disorders SAME
C. The anxiety and worry are associated with three or more
of the following six symptoms (with at least some
symptoms present for more days than not for the past 6
months).
Note: Only one item is required in children
1. Restlessness or feeling keyed up or on edge
2. Being easily fatigued
3. Difficulty concentrating or mind going blank
4. Irritability
5. Muscle tension
6. Sleep disturbance (difficulty falling or staying
asleep, or restless unsatisfying sleep)
SAME
Note: Only one item is required in children
1. Restlessness or feeling keyed up or on edge
2. Being easily fatigued
3. Difficulty concentrating or mind going
blank
4. Irritability
5. Muscle tension
6. Sleep disturbance (difficulty falling or
staying asleep, or restless unsatisfying
sleep)
D. The focus of the anxiety and worry is not confined to
features of an Axis I disorder (e.g., the anxiety or worry
is not about having a panic attack [as in panic disorder],
being embarrassed in public [as in social phobia], being
contaminated [as in obsessive-compulsive disorder]
being away from home or close relatives [as in
separation anxiety disorder], gaining weight [as in
anorexia nervosa], or having a serious illness [as in
hypochondriasis]), and the anxiety and worry do not
occur exclusively during post-traumatic stress disorder.
F. The disturbance is not better explained by
another mental disorder (e.g., anxiety or worry
about having panic attacks in panic disorder,
negative evaluation in social anxiety disorder
[social phobia], contamination or other
obsessions in obsessive-compulsive disorder,
separation from attachment figures in
separation anxiety disorder, reminders of
traumatic events in post-traumatic stress
disorder, gaining weight in anorexia nervosa,
physical complaints in somatic symptom
disorder, perceived appearance flaws in body
dysmorphic disorder, having a serious illness in
illness anxiety disorder, or the content of
delusional beliefs in schizophrenia or delusional
disorder).
E. The anxiety, worry, or physical symptoms cause
clinically significant distress or impairment in social,
occupational, or other important areas of functioning.
SAME (part D)
F. The disturbance is not due to the direct physiological
effects of a substance (e.g., a drug of abuse, a
medication) or a general medical condition (e.g.,
hyperthyroidism) and does not occur exclusively during
a mood disorder, a psychotic disorder, or a pervasive
developmental disorder.
E. The disturbance is not attributable to the
physiological effects of a substance (e.g., a drug
of abuse, a medication) or another medical
condition (e.g., hyperthyroidism).
3.3.5 Panic Disorder and Agoraphobia (under Anxiety Disorders)
Panic disorder is an anxiety disorder characterized by panic attack(s) and the ongoing
concern about experiencing additional panic attacks (American Psychiatric Association, 2013b).
A panic attack is an abrupt, but quickly peaking, surge of intense fear or discomfort,
accompanied by a series of physical symptoms. In DSM-IV, panic disorder and agoraphobia
were conceptually linked. Agoraphobia is an anxiety disorder characterized by an intense fear or
anxiety triggered by the real or anticipated exposure to a number of situations (i.e., using public
transportation, being in open spaces), which causes clinically significant distress or impairment.
The diagnoses in DSM-IV included panic disorder with agoraphobia, panic disorder without

36
agoraphobia, and agoraphobia without history of panic disorder. In DSM-5, however, panic
disorder and agoraphobia have been separated and individuals meeting criteria for both disorders
are considered to have comorbid mental disorders. Examining the comparison of panic disorder
criteria specifically (Table 14), with the exception of the disaggregation of agoraphobia, the
criteria are similar between DSM-IV and DSM-5. There are minor wording changes to the
description of panic attacks that may have slight implications to the prevalence of panic disorder
under DSM-5. Under DSM-IV, the specification was made that panic attacks were discrete
periods of intense fear or discomfort that peaked within 10 minutes. In DSM-5, panic attacks are
described as an abrupt surge of intense fear or intense discomfort that peak within a few minutes.
The wording changes reflect two conceptual issues. First, the change in wording from a discrete
event to an abrupt surge broadens criteria based on evidence that panic attacks do not necessarily
arise "out of the blue" but can arise during periods of anxiety or other distress and that it is the
sudden increase in fear/discomfort that is the hallmark of a panic attack. In addition, they have
removed the 10-minute criterion, in favor of the less precise but implicitly shorter descriptive of
"within minutes" (American Psychiatric Association, 2013b, p. 214). This was only a change in
classification and is expected to have no impact on overarching prevalence estimates of SED.
Table 14 shows a comparison between DSM-IV and DSM-5 diagnostic criteria for panic
disorder and agoraphobia.
Table 14. Panic Disorder and Agoraphobia Criteria Changes from DSM-IV to DSM-5
DSM-IV Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Diagnostic Class:
Anxiety Disorders
SAME
Panic Attack
1
A discrete period of intense fear or
discomfort, in which four or more of the
following symptoms developed abruptly
and reached a peak within 10 minutes
• Palpitations, pounding heart, or
accelerated heart rate
• Sweating
• Trembling or shaking
• Sensations of shortness of breath or
smothering
• Feeling of choking
• Chest pain or discomfort
• Nausea or abdominal distress
• Feeling dizzy, unsteady,
lightheaded, or faint
• Derealization (feelings of unreality)
or depersonalization (being
detached from oneself)
• Fear of losing control or "going
crazy"
• Fear of dying
• Paresthesias (numbness or tingling
sensation)
• Chills or hot flushes.
Panic
Attack
1
An abrupt surge of
intense fear or intense
discomfort that reaches a
peak within minutes and
during which time four or
more of the following
symptoms occur.
• List is unchanged,
except that "hot
flushes" has been
modified to "heat
sensations" and
there has been a
reordering of
symptoms.
(continued)

37
Table 14. Panic Disorder and Agoraphobia Criteria Changes from DSM-IV to DSM-5 (continued)
DSM-IV Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Diagnostic Class:
Anxiety Disorders
SAME
Agoraphobia
1
Anxiety about being in places or situations
from which escape might be difficult (or
embarrassing) or in which help may not be
available in the event of having an
unexpected or situationally predisposed
panic attack or panic-like symptoms.
Agoraphobic fears typically involve
characteristic clusters of situations that
include being outside the home alone;
being in a crowd or standing in a line;
being on a bridge; and traveling in a bus,
train, or automobile.
Agoraphobia A marked fear or anxiety
about two (or more) of
the following five
situations:
• Using public
transportation
• Being in open
spaces
• Being in enclosed
spaces (e.g., shops,
theaters, cinemas)
• Standing in line or
being in a crowd
• Being outside the
home alone.
The situations are avoided (e.g., travel is
restricted) or else are endured with marked
distress or with anxiety about having a
panic attack or panic-like symptoms, or
require the presence of a companion.
SAME
N/A The agoraphobic
situations almost always
provoke fear or anxiety.
N/A The fear or anxiety is out
of proportion to the actual
danger posed by the
agoraphobic situations
and to the sociocultural
context.
N/A
The fear, anxiety, or
avoidance is persistent,
typically lasting 6 months
or more.
N/A The fear, anxiety, or
avoidance causes
clinically significant
distress or impairment in
important areas of
functioning.
The anxiety or phobic avoidance is not
better accounted for by another mental
disorder.
SAME
(continued)
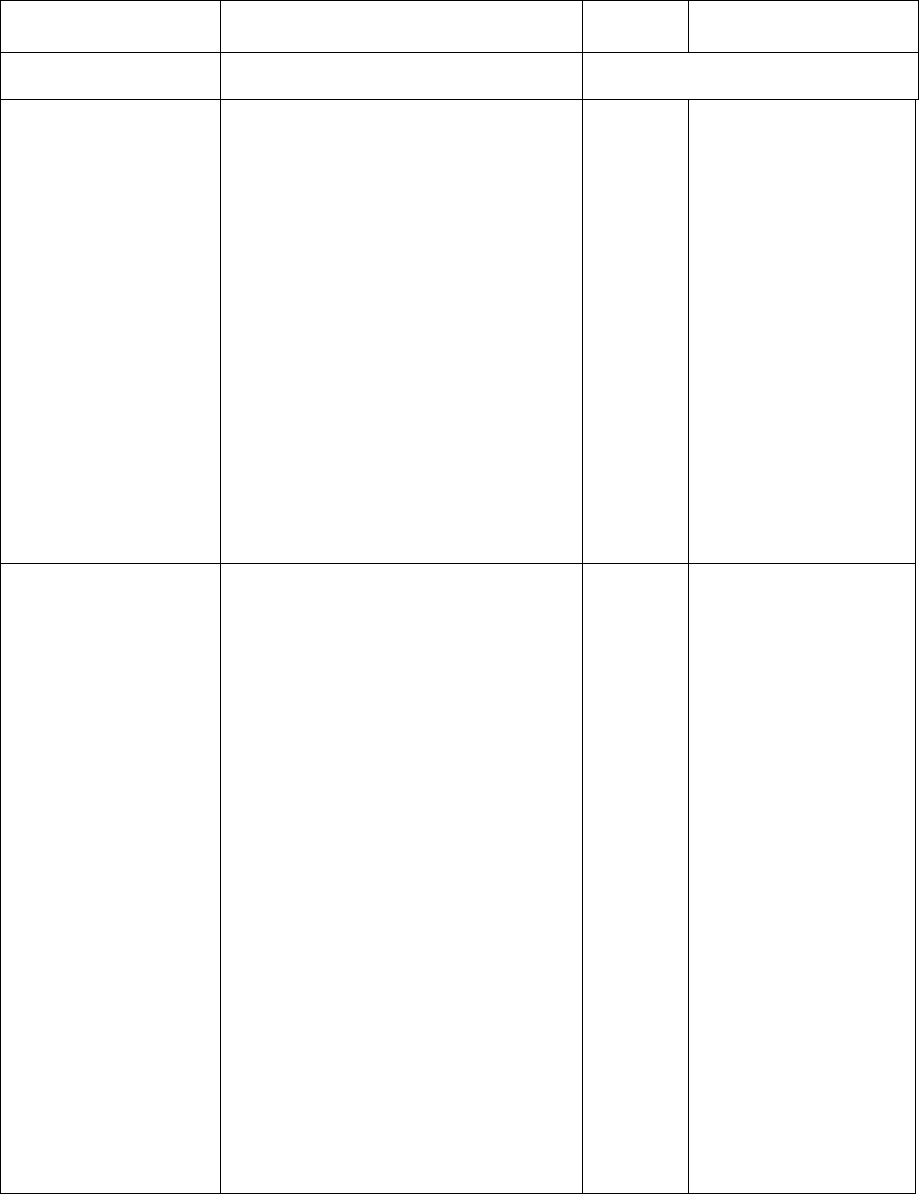
38
Table 14. Panic Disorder and Agoraphobia Criteria Changes from DSM-IV to DSM-5 (continued)
DSM-IV Disorder DSM-IV Criteria
DSM-5
Disorder DSM-5 Criteria
Diagnostic Class:
Anxiety Disorders
SAME
Agoraphobia without
history of Panic
Disorder
The presence of agoraphobia related to
fear of developing panic-like symptoms.
The individual fears or
avoids these situations
because of thoughts that
escape might be difficult
or help might not be
available in the event of
developing panic-like
symptoms or other
incapacitating or
embarrassing symptoms.
Criteria for panic disorder have never
been met.
DROPPED
The disturbance not due to the direct
physiological effects of a substance (e.g.,
a drug of abuse or a medication) or a
general medical condition
DROPPED
If an associated general medical condition
is present, the fear described in Criterion
A is clearly in excess of that usually
associated with the condition.
SAME
Panic Disorder,
with/without
Agoraphobia
Both:
• Recurrent and unexpected panic
attacks (see below)
• ≥ 1 attack has been followed by 1
month or more of 1 or more of the
following
Persistent concern about additional
attacks
Worry about the implications of the attack
or its consequences
A significant change in behavior related
to the attacks
Panic
Disorder
Both:
• Recurrent and
unexpected panic
attacks (see
below)
• ≥ 1 attack has
been followed by
1 month or more
of 1 or both of the
following
Persistent concern about
additional attacks or
their consequences
A significant
maladaptive change in
behavior related to the
attacks
The panic attacks are not due to the direct
physiological effects of a substance (e.g.,
a drug of abuse or a medication) or a
general medical condition
SAME
The panic attacks are not better accounted
for by another mental disorder.
SAME
• Without agoraphobia: Absence of
agoraphobia (see below)
DROPPED
• With agoraphobia: Presence of
agoraphobia
DROPPED
1
Not a codable disorder, considered a feature of the specific disorder in which the panic attack/agoraphobia occurs.

39
3.3.6 Separation Anxiety Disorder (under Anxiety Disorders)
Separation anxiety disorder (SAD) is a psychological condition in which an individual
experiences excessive anxiety, fear, or distress regarding separation from home or from people to
whom the individual has a strong emotional attachment (e.g., a parent, grandparents, or siblings;
Table 15). SAD is the inappropriate and excessive display of fear and distress when faced with
situations of separation from the home or from a specific attachment figure. The anxiety that is
expressed is categorized as being atypical of the expected developmental level and age. The
severity of the symptoms ranges from anticipatory uneasiness to full-blown anxiety about
separation. SAD may cause significant negative effects within a child's everyday life, as well.
These effects can be seen in areas of social and emotional functioning, family life, physical
health, and within the academic context. The duration of this problem must persist for at least 4
weeks and must present itself before a person is 18 years of age to be diagnosed as SAD
(American Psychiatric Association, 2013b).
Table 15. DSM-IV to DSM-5 Separation Anxiety Disorder Comparison
DSM-IV DSM-5
Disorder Class: Disorders Usually Diagnosed in Infancy,
Childhood, and Adolescence
Disorder Class: Anxiety Disorders
A. Developmentally inappropriate and excessive anxiety
concerning separation from home or from those to
whom the individual is attached, as evidenced by three
or more of the following:
A. Developmentally inappropriate and excessive
fear or anxiety concerning separation from those
to whom the individual is attached, as evidenced
by at least three of the following:
1. Recurrent excessive distress when separation from
home or major attachment figures occurs or is
anticipated
1. Recurrent excessive distress when
anticipating or experiencing separation from
home or from major attachment figures.
2. Persistent and excessive worry about losing, or
about possible harm befalling, major attachment
figures
2. Persistent and excessive worry about losing
major attachment figures or about possible
harm to them, such as illness, injury,
disasters, or death.
3. Persistent and excessive worry that an untoward
event will lead to separation from a major
attachment figure (e.g., getting lost or being
kidnapped)
3. Persistent and excessive worry about
experiencing an untoward event (e.g., getting
lost, being kidnapped, having an accident,
becoming ill) that causes separation from a
major attachment figure.
4. Persistent reluctance or refusal to go to school or
elsewhere because of fear of separation
4. Persistent reluctance or refusal to go out,
away from home, to school, to work, or
elsewhere because of fear of separation.
5. Persistently and excessively fearful or reluctant to
be alone or without major attachment figures at
home or without significant adults in other settings
5. Persistent and excessive fear of or reluctance
about being alone or without major
attachment figures at home or in other
settings.
6. Persistent reluctance or refusal to go to sleep
without being near a major attachment figure or to
sleep away from home
6. Persistent reluctance or refusal to sleep away
from home or to go to sleep without being
near a major attachment figure.
7. Repeated nightmares involving the theme of
separation
7. SAME
8. Repeated complaints of physical symptoms (such as
headaches, stomachaches, nausea, or vomiting)
when separation from major attachment figures
occurs or is anticipated
8. SAME
(continued)

40
Table 15. DSM-IV to DSM-5 Separation Anxiety Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Disorders Usually Diagnosed in Infancy,
Childhood, and Adolescence
Disorder Class: Anxiety Disorders
B. The duration of the disturbance is at least 4 weeks. B. The fear, anxiety, or avoidance is persistent,
lasting at least 4 weeks in children and
adolescents and typically 6 months or more in
adults.
C. The onset is before age 18 years. DROPPED
D. The disturbance causes clinically significant distress or
impairment in social, academic (occupational), or other
important areas of functioning.
SAME (now part C)
E. The disturbance does not occur exclusively during the
course of a pervasive developmental disorder,
schizophrenia, or other psychotic disorder and, in
adolescents and adults, is not better accounted for by
panic disorder with agoraphobia.
D. The disturbance is not better explained by
another mental disorder, such as refusing to leave
home because of excessive resistance to change
in autism spectrum disorder; delusions or
hallucinations concerning separation in psychotic
disorders; refusal to go outside without a trusted
companion in agoraphobia; worries about ill
health or other harm befalling significant others
in generalized anxiety disorder; or concerns
about having an illness in illness anxiety
disorder.
Specify if:
Early Onset: if onset occurs before age 6 years
DROPPED
The primary change from DSM-IV to DSM-5 has been the reclassification of SAD from
the disorders usually diagnosed in infancy, childhood, and adolescence section to anxiety
disorders. Criteria changes from DSM-IV to DSM-5 are largely wording changes rather than
major conceptual differences. The largest differences are related to broadening the criteria to
better align with the presentation of SAD among adults; consequently, this should have minimal
impact on childhood estimates.
3.3.7 Social Anxiety Disorder (formerly Social Phobia [Social Anxiety Disorder], under
Anxiety Disorders)
Social anxiety disorder is an anxiety disorder characterized by fear of social situations
wherein the individual may be exposed to scrutiny by others (American Psychiatric Association,
2013b). In children, the anxiety must occur in peer settings and not just during interactions with
adults. In addition, for children, the fear or anxiety may be expressed by crying, tantrums,
freezing, clinging, shrinking, or failing to speak in social situations.
Diagnostic criteria for social phobia have undergone several minor wording changes from
DSM-IV to DSM-5 (Table 16). One additional change is anticipated to have a broader impact on
estimates of social phobia. In DSM-IV, criteria for social phobia required that an individual
"recognizes that the fear is excessive or unreasonable." In DSM-5 this has been changed to note
that "the fear or anxiety is out of proportion to the actual threat posed by the social situation and
to the sociocultural context." This means that the patient does not need to recognize that their
fear is unreasonable, so long as the clinician can determine that the fear is unreasonable.

41
Table 16. DSM-IV to DSM-5 Social Phobia/Social Anxiety Disorder Comparison
DSM-IV DSM-5
Disorder Class: Anxiety Disorders SAME
A. A marked and persistent fear of one or more social or
performance situations in which the person is exposed to
unfamiliar people or to possible scrutiny by others. The
individual fears that he or she will act in a way (or show
anxiety symptoms) that will be humiliating or
embarrassing.
Note: In children, there must be evidence of the capacity for
age-appropriate social relationships with familiar people
and the anxiety must occur in peer settings, not just in
interactions with adults.
A. Marked fear or anxiety about one or more
social situations in which the individual is
exposed to possible scrutiny by others.
Examples include social interactions (e.g.,
having a conversation, meeting unfamiliar
people), being observed (e.g., eating or
drinking), and performing in front of others
(e.g., giving a speech).
Note: In children, the anxiety must occur in peer
settings and not just during interactions with
adults.
The individual fears that he or she will act in a way
or show anxiety symptoms that will be
negatively evaluated (i.e., will be humiliating or
embarrassing; will lead to rejection or offend
others).
B. Exposure to the feared social situation almost invariably
provokes anxiety, which may take the form of a
situationally bound or situationally predisposed panic
attack.
Note: In children, the anxiety may be expressed by crying,
tantrums, freezing, clinging, shrinking, or failing to speak
in social situations.
C. The social situations almost always provoke
fear or anxiety.
Note: In children, the fear or anxiety may be
expressed by crying, tantrums, freezing,
clinging, shrinking, or failing to speak in social
situations.
C. The person recognizes that the fear is excessive or
unreasonable.
Note: In children, this feature may be absent.
B. The fear or anxiety is out of proportion to the
actual threat posed by the social situation and to
the sociocultural context.
D. The feared social or performance situations are avoided
or else are endured with intense anxiety or distress.
D. The social situations are avoided or endured
with intense fear or anxiety.
E. The avoidance, anxious anticipation, or distress in the
feared social or performance situation(s) interferes
significantly with the person's normal routine,
occupational (academic) functioning, or social activities
or relationships, or there is marked distress about having
the phobia.
G. The fear, anxiety, or avoidance causes clinically
significant distress or impairment in social,
occupational, or other important areas of
functioning.
F. In individuals under age 18 years, the duration is at least
6 months.
F. The fear, anxiety, or avoidance is persistent,
typically lasting for 6 months or more.
G. The fear or avoidance is not due to the direct
physiological effects of a substance (e.g., a drug of abuse,
a medication) or a general medical condition and is not
better accounted for by another mental disorder (e.g.,
panic disorder with or without agoraphobia, separation
anxiety disorder, body dysmorphic disorder, a pervasive
developmental disorder, or schizoid personality disorder).
H. The fear, anxiety, or avoidance is not
attributable to the physiological effects of a
substance (e.g., a drug of abuse, a medication)
or another medical condition.
I. The fear, anxiety, or avoidance is not better
explained by the symptoms of another mental
disorder, such as panic disorder, body
dysmorphic disorder, or autism spectrum
disorder.
H. If a general medical condition or another mental disorder
is present, the fear in Criterion A is unrelated to it (e.g.,
the fear is not of stuttering, trembling in Parkinson's
disease, or exhibiting abnormal eating behavior in
anorexia nervosa or bulimia nervosa).
J. If another medical condition (e.g., Parkinson's
disease, obesity, disfigurement from burns or
injury) is present, the fear, anxiety, or
avoidance is clearly unrelated or is excessive.
(continued)

42
Table 16. DSM-IV to DSM-5 Social Phobia/Social Anxiety Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Anxiety Disorders SAME
Specify if: Generalized: if the fears include most social
situations (also consider the additional diagnosis of avoidant
personality disorder)
Specify if: Performance only: if the fear is restricted
to speaking or performing in public.
For the new social anxiety disorder, which replaces social phobia, the "generalized" (if
the fears include most social situations) specifier has been deleted and replaced with a
"performance only" specifier (if the fear is restricted to speaking or performing in public). The
rationale is that the DSM-IV generalized specifier was difficult to operationalize. The DSM-5
describes that individuals who fear only performance situations (i.e., speaking or performing in
front of an audience) appear to represent a distinct subset of social anxiety disorder in terms of
etiology, age at onset, physiological response, and treatment response.
Epidemiological work in the U.S. population using data from the National Comorbidity
Survey-Adolescent Supplement found that only 0.7 percent of adolescents meeting criteria for
social anxiety disorder could be classified as having the performance-only social anxiety disorder
(Burstein et al., 2011). Subsequent work based on a clinical sample in Boston of 204 youth
seeking treatment for anxiety disorders at a university-affiliated center, found that no children
endorsed discrete fear in performance situations only in the absence of fear in other social
situations (Kerns, Comer, Pincus, & Hofmann, 2013). No impact in the prevalence of SED is
expected from the new social anxiety disorder specifier when applied to youth.
3.3.8 Conduct Disorder (under Disruptive, Impulse-Control, and Conduct Disorders)
Conduct disorder (CD) is usually first diagnosed in childhood and was categorized in
DSM-IV under the category of the same name. Conduct disorder is characterized by a repetitive
and persistent pattern of behavior that violates either the rights of others or major age appropriate
societal norms or rules. People with CD often show aggression to people and animals,
destruction of property, deceitfulness or theft, and/or serious violations of rules. At least 3
symptoms out of 15 must be present in the past 12 months with 1 symptom having been present
in the past 6 months. To be diagnosed with CD, the symptoms must cause significant impairment
in social, academic, or occupational functioning. The disorder is typically diagnosed prior to
adulthood (American Psychiatric Association, 2013a).
The main change to the diagnostic criteria for CD is the addition of a subtype grouping
around callous and unemotional traits. The callous–lack-of-empathy trait is defined as a
disregard and lack of concern about the feelings of others and more concerned about the effects
of his or her actions on himself/herself than their effects on others even when they may result in
substantial harm to others (American Psychiatric Association, 2013a). The purpose of this
change was to better account for heterogeneity within CD. As such, this change is not expected
to impact prevalence estimates of CD. In the DSM-5 field trials in the United States and Canada
based on child clinical populations (general child psychiatry outpatient services), CD prevalence
was the same (8 percent) using DSM-IV and DSM-5. The estimated prevalence using DSM-5 for

43
the new callous/unemotional specifier for CD was 5 percent (Regier et al., 2013). Table 17
shows a comparison between DSM-IV and DSM-5 diagnostic criteria for CD.
Table 17. DSM-IV to DSM-5 Conduct Disorder Comparison
DSM-IV: Conduct Disorder DSM-5: Conduct Disorder
Disorder Class: Attention deficit and
disruptive behavior disorders
Disorder Class: Disruptive, Impulse-Control, and Conduct
Disorders
A. A repetitive and persistent pattern of
behavior in which the basic rights of others
or major age-appropriate societal norms or
rules are violated, as manifested by the
presence of three (or more) of the
following criteria in the past 12 months,
with at least one criterion present in the
past 6 months:
A. A repetitive and persistent pattern of behavior in which the
basic rights of others or major age-appropriate societal
norms or rules are violated, as manifested by the presence
of three (or more) of the following 15 criteria in the past 12
months from any of the categories below, with at least one
criterion present in the past 6 months:
Aggression to people and animals
1. often bullies, threatens, or intimidates
others
2. often initiates physical fights
3. has used a weapon that can cause
serious physical harm to others (e.g., a
bat, brick, broken bottle, knife, gun)
4. has been physically cruel to people
5. has been physically cruel to animals
6. has stolen while confronting a victim
(e.g., mugging, purse snatching,
extortion, armed robbery)
7. has forced someone into sexual activity
Aggression to people and animals
1. SAME
2. SAME
3. SAME
4. SAME
5. SAME
6. SAME
7. SAME
Destruction of property
8 has deliberately engaged in fire setting
with the intention of causing serious
damage
9. has deliberately destroyed others'
property (other than by fire setting)
Destruction of property
8. SAME
9. SAME
Deceitfulness or theft
10. has broken into someone else's house,
building, or car
11. often lies to obtain goods or favors or
to avoid obligations (i.e., "cons" others)
12. has stolen items of nontrivial value
without confronting a victim (e.g.,
shoplifting, but without breaking and
entering; forgery)
Deceitfulness or theft
10. SAME
11. SAME
12. SAME
Serious violations of rules
13. often stays out at night despite parental
prohibitions, beginning before age 13
years
14. has run away from home overnight at
least twice while living in parental or
parental surrogate home (or once
without returning for a lengthy period)
15. is often truant from school, beginning
before age 13 years
Serious violations of rules
13. SAME
14. SAME
15. SAME
(continued)

44
Table 17. DSM-IV to DSM-5 Conduct Disorder Comparison (continued)
DSM-IV: Conduct Disorder DSM-5: Conduct Disorder
Disorder Class: Attention deficit and disruptive
behavior disorders
Disorder Class: Disruptive, Impulse-Control, and Conduct
Disorders
B. The disturbance in behavior causes clinically
significant impairment in social, academic,
or occupational functioning.
B. SAME
C. If the individual is age 18 years or older,
criteria are not met for Antisocial
Personality Disorder.
C. SAME
Code based on age at onset:
312.81 Conduct Disorder, Childhood-Onset
Type: onset of at least one criterion
characteristic of Conduct Disorder prior to
age 10 years
312.82 Conduct Disorder, Adolescent-Onset
Type: absence of any criteria characteristic
of Conduct Disorder prior to age 10 years
312.89 Conduct Disorder, Unspecified
Onset: age at onset is not known
Specify whether:
312.81 (F91.1) Conduct Disorder, Childhood-Onset Type:
Individuals show at least one symptom characteristic of
conduct disorder prior to age 10 years
312.82 (F91.2) Conduct Disorder, Adolescent-Onset Type:
Individuals show now symptom characteristic of conduct
disorder prior to age 10 years
312.89 (F91.9) Conduct Disorder, Unspecified Onset:
Criteria for a diagnosis or conduct disorder are met, but
there is not enough information available to determine
whether the onset of the first symptom was before or after
age 10 years.
N/A Specify if:
With limited prosocial emotions: To qualify for this
specifier, an individual must have displayed at least two of
the following characteristics persistently over at least 12
months and in multiple relationships and setting. These
characteristics reflect the individual's typical pattern of
interpersonal and emotional functioning over this period
and not just occasional occurrences in some situations.
Thus, to assess the criteria for the specifier, multiple
information sources are necessary. In addition to the
individual's self-report, it is necessary to consider reports
by others who have known the individual for extended
periods of time (e.g., parents, teachers, coworkers,
extended family members, peers).
Lack of remorse or guilt: Does not feel bad or guilty when
he/she does something wrong (excluding remorse when
expressed only when caught and/or facing punishment).
The individual shows a general lack of concern about the
negative consequences of his or her actions. For example,
the individual is not remorseful after hurting someone or
does not care about the consequences of breaking rules.
Callous—lack of empathy: Disregards and is unconcerned
about the feelings of others. The individual is described as
cold and uncaring. The person appears more concerned
about the effects of his or her actions on himself or herself,
rather than their effects on others, even when they result in
substantial harm to others.
(continued)
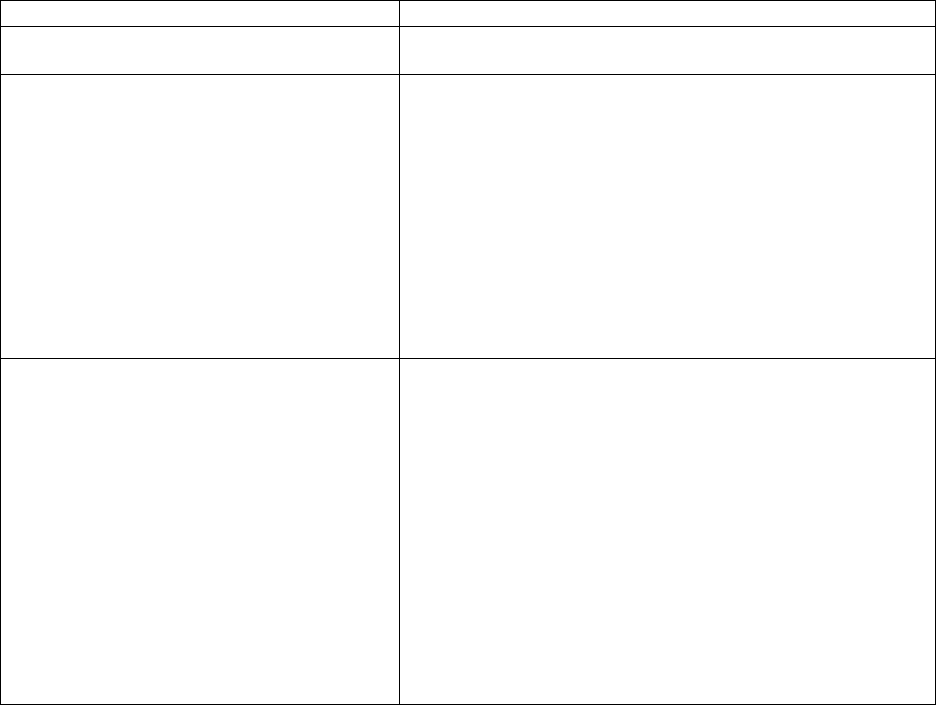
45
Table 17. DSM-IV to DSM-5 Conduct Disorder Comparison (continued)
DSM-IV: Conduct Disorder DSM-5: Conduct Disorder
Disorder Class: Attention deficit and
disruptive behavior disorders
Disorder Class: Disruptive, Impulse-Control, and Conduct
Disorders
Unconcerned about performance: Does not show concern
about poor/problematic performance at school, work, or in
other important activities. The individual does not put forth
the effort necessary to perform well, even when
expectations are clear, and typically blames others for his or
her poor performance.
Shallow or deficient affect: Does not express feelings or
show emotions to others, except in ways that seem shallow,
insincere, or superficial (e.g., actions contradict the emotion
displayed; can turn emotions "on" or "off" quickly) or when
emotional expressions are used for gain (e.g., emotions
displayed to manipulate or intimidate others).
Specify severity:
Mild: few if any conduct problems in
excess of those required to make the
diagnosis and conduct problems cause only
minor harm to others
Moderate: number of conduct problems
and effect on others intermediate between
"mild" and "severe"
Severe: many conduct problems in excess
of those required to make the diagnosis or
conduct problems cause considerable harm
to others
Specify current severity:
Mild: Few if any conduct problems in excess of those
required to make the diagnosis are present, and conduct
problems cause relatively minor harm to others (e.g., lying,
truancy, staying out after dark without permission, other
rule breaking).
Moderate: The number of conduct problems and the effect
on others are intermediate between those specified in "mild"
and those in "severe" (e.g., stealing without confronting a
victim, vandalism).
Severe: Many conduct problems in excess of those required
to make the diagnosis are present, or conduct problems
cause considerable harm to others (e.g., forced sex, physical
cruelty, use of a weapon, stealing while confronting a
victim, breaking and entering).
3.3.9 Oppositional Defiant Disorder (under Disruptive, Impulse-Control, and Conduct
Disorders)
Oppositional defiant disorder's (ODD) is characterized by a frequent and persistent
pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness that may
significantly impair social functioning (American Psychiatric Association, 2013b). ODD is
primarily viewed as a younger-child version of CD and it emerges mostly during the preschool
years (before 5 years old), where symptoms of aggression and defiance are present but the acts
committed by the child are less severe. Most research on changes to the categorization of ODD
in DSM-5 have focused on understanding the underlying dimensions of ODD, towards the goal
of being better able to predict different outcomes in later childhood (which children with ODD
develop CD, which children develop other mental disorders, which children become
nonsymptomatic) (Barry et al, 2013; Krieger et al., 2013). As such, there is no expectation that
children previously diagnosed with something else will necessarily move into the ODD category
in the DSM-5. However, some children previously diagnosed with ODD using DSM-IV criteria
may move into the DMDD category under DSM-5 if their symptoms include chronic irritability
along with anger and severe tantrums.

46
As described in the DSM-5 manual (American Psychiatric Association, 2013b, p, 64),
cases with DMDD and ADHD should be diagnosed separately. In the DSM-5 field trials in the
United States and Canada based on child clinical populations (general child psychiatry outpatient
services), estimates for ODD were described for one of the sites (Columbia/Cornell Medical
Centers-New York) as decreasing from 22 percent using DSM-IV to 17 percent using DSM-5
(Regier et al., 2013).Thus, the prevalence of ODD may decrease very slightly when DSM-5
criteria are applied, but given that DMDD only occurs in 1 percent of the school-age population,
this effect is expected to be minimal. In terms of SED, DSM-5 recategorization of irritability
from ODD to DMDD is expected to result in no difference in the SED prevalence estimate.
Table 18 shows a comparison between DSM-IV and DSM-5 oppositional defiant disorder.
Table 18. DSM-IV to DSM-5 Oppositional Defiant Disorder Comparison
DSM-IV: Oppositional Defiant Disorder DSM-5: Oppositional Defiant Disorder
Disorder Class: Attention Deficit and Disruptive
Behavior Disorders
Disorder Class: Disruptive, Impulse-Control, and Conduct
Disorders
A. A pattern of negativistic; hostile, and defiant
behavior lasting at least 6 months, during which
four (or more of the following are present:
1. Often loses temper
2. Often argues with adults
3. Often actively defies or refuses to comply with
adults requests or rules
4. Often deliberately annoys people
5. Often blames others for his or her mistakes or
misbehavior
6. Is often touchy or easily annoyed by others
7. Is often angry and resentful
8. Is often vindictive
Note: Consider a criterion met only if the behavior
occurs more frequently that is typically observed in
individuals of comparable age and developmental
level.
A. A pattern of angry/irritable mood, argumentative/
defiant behavior, or vindictiveness lasting at least 6
months as evidenced by at least four symptoms of the
following categories, and exhibited during interaction
with at least one individual who is not a sibling:
Angry/Irritable Mood
1. Often loses temper
2. Is often touchy or easily annoyed
3. Is often angry and resentful
Argumentative/Defiant Behavior
4. Often argues with authority figures or, for children
and adolescents, with adults
5. Often actively defies or refuses to comply with
requests from authority figures or with rules
6. Often deliberately annoys others
7. Often blames others for his or her mistakes or
misbehavior
Vindictiveness
8. Has been spiteful or vindictive at least twice within
the past 6 months.
Note: The persistence and frequency of these behaviors
should be used to distinguish a behavior that is within
normal limits from a behavior that is symptomatic. For
children younger than 5 years, the behavior should occur
on most days for a period of at least 6 months unless
otherwise noted (Criterion AB). For individuals 5 years or
older, the behavior should occur at least once per week for
at least 6 months. Unless otherwise noted (Criterion AB).
While these frequency criteria provide guidance on a
minimal level of frequency to define symptoms, other
factors should also be considered, such as whether the
frequency and intensity of the behaviors are outside a
range that is normative for the individual's developmental
level, gender, and culture.
(continued)

47
Table 18. DSM-IV to DSM-5 Oppositional Defiant Disorder Comparison (continued)
DSM-IV: Oppositional Defiant Disorder DSM-5: Oppositional Defiant Disorder
Disorder Class: Attention Deficit and Disruptive
Behavior Disorders
Disorder Class: Disruptive, Impulse-Control, and Conduct
Disorders
B. The disturbance in behavior causes clinically
significant impairment in social, academic, or
occupational functioning,
B. The disturbance in behavior is associated with distress
in the individual or others in his or her immediate
social context (e.g., family, peer group, work
colleagues) or it impacts negatively on social,
educational, occupational, or other important areas of
functioning,
C. The behavior does not occur exclusively during
the course of a Psychiatric or Mood Disorder.
C. The behavior does not occur exclusively during the
course of a psychotic, substance use, depressive, or
bipolar disorder. Also the criteria are not met for
disruptive mood dysregulation disorder.
D. Criteria are not met for Conduct Disorder, and, if
the individual is age 18 or older, criteria are not
met for Antisocial Personality Disorder
Dropped
Specify current severity:
Mild: Symptoms are confined to only one setting (e.g.,
at home, at school, at work, with peers).
Moderate: Some symptoms are present in at least two
settings
Severe: Some symptoms are present in three or more
settings.
3.3.10 Eating Disorders (under Feeding and Eating Disorders)
Anorexia Nervosa. Anorexia nervosa is an eating disorder characterized by an intense
fear of gaining weight and the refusal to maintain a minimally normal body weight. Individuals
with anorexia also exhibit a misperception of body shape and/or size. There have been several
DSM-5 criteria changes. In DSM-IV, a diagnosis of anorexia nervosa was excluded if the patient
maintained bodyweight at or above the 85th percentile for his or her height/age. In DSM-5 this
criterion is similar, but adds sex, developmental norms, and physical health and uses body mass
index data. The DSM-5 adds "persistent behavior that interferes with weight gain" as an added
way to meet a criterion. The DSM-5 does not include criteria on menstruating females' absence
of three consecutive menses, as the DSM-IV does. The restrictive type and binge-eating/purging
types differ in that DSM-IV specifies "during the current episode" and DSM-5 specifies "during
the past 3 months." The DSM-5 adds criteria for partial and full remission, while the DSM-IV
does not include this information. Data from a U.S. sample of 215 youth 8 to 21 years enrolled as
new patients with eating disorders in six clinics showed an increase from 30 percent to 40
percent in anorexia nervosa when comparing DSM-IV and DSM-5 criteria (Ornstein et al.,
2013). Table 19 shows a comparison between DSM-IV and DSM-5 for anorexia nervosa.
Bulimia Nervosa. Bulimia nervosa is an eating disorder characterized by binge eating
followed by inappropriate compensatory behaviors designed to prevent weight gain. In addition,
the self-evaluation of individuals with bulimia nervosa is excessively influenced by weight and
body shape. The major change in criteria for diagnosis of bulimia nervosa is reducing the binge
frequency threshold from twice per week in DSM-IV to once per week in DSM-5. The other

48
differences include the DSM-IV differentiating between purging and nonpurging type (the
DSM-5 does not) and the DSM-5 specifying criteria for partial remission, full remission, and
severity, while the DSM-IV does not. DSM-IV to DSM-5 criteria changes may increase the
prevalence rate. Data from an Australian cohort study of 2,822 adolescents and young adults
(57.0 percent female) whose parents were recruited from antenatal clinics at a single hospital and
followed through age 20, indicate that rates of bulimia nervosa are higher when applying the
DSM-5 criteria versus the DSM–IV (Allen, Byrne, Oddy, & Crosby, 2013). Similarly, data from
a U.S. sample of 215 youth 8 to 21 years enrolled as new patients with eating disorders in six
clinics showed an increase in bulimia nervosa from 7.3 percent to 11.8 percent when comparing
DSM-IV and DSM-5 criteria (Ornstein et al., 2013). Table 20 shows a comparison between
DSM-IV and DSM-5 for bulimia nervosa.
Table 19. DSM-IV to DSM-5 Anorexia Nervosa Comparison
DSM-IV DSM-5
Disorder Class: Eating Disorders Disorder Class: Feeding and Eating Disorders
A. Refusal to maintain bodyweight at or above
minimally normal weight for height/age (less
than 85th percentile).
A. Restriction of energy intake relative to requirements,
leading to a significant low body weight in the context of
the age, sex, developmental trajectory, and physical health
(less than minimally normal/expected
1
).
B. Intense fear of gaining weight or becoming
obese, even though underweight.
B. Intense fear of gaining weight or becoming fat or
persistent behavior that interferes with weight gain.
C. Disturbed by one's body weight or shape, self-
worth influenced by body weight or shape, or
persistent lack of recognition of seriousness of
low bodyweight.
SAME
D. In menstruating females, absence of at least 3
consecutive non-synthetically induced
menstrual cycles.
DROPPED
Specify type:
Restricting type: During the current episode, has
not regularly engaged in binge-eating or purging.
2
Specified whether:
Restricting type: During the last 3 months…SAME.
Binge-eating/purging type: During the current
episode, has regularly engaged in binge-eating or
purging.
2
Binge-eating/purging type: During the last 3
months…SAME.
Partial remission: After full criteria met, low bodyweight has
not been met for sustained period, BUT at least one of the
following two criteria still met:
Intense fear of gaining weight/becoming obese or
behavior that interferes with weight gain
OR
Disturbed by weight and shape.
Full remission: After full criteria met, none of the criteria met
for sustained period of time.
1
Severity is based on body mass index (BMI) derived from World Health Organization categories for thinness in
adults; corresponding percentiles should be used for children and adolescents: Mild: BMI greater than or equal to
17 kg/m
2
, Moderate: BMI 16-16.99 kg/m
2
, Severe: BMI 15-15.99 kg/m
2
, Extreme: BMI less than 15 kg/m
2
.
2
Purging is self-induced vomiting or misuse of laxatives, diuretics, or enemas.

49
Table 20. DSM-IV to DSM-5 Bulimia Nervosa Comparison
DSM-IV DSM-5
Disorder Class: Eating Disorders Disorder Class: Feeding and Eating Disorders
A. Recurrent episodes of binge eating, as characterized
by both:
1. Eating, within any 2-hour period, an amount of
food that is definitively larger than what most
individuals would eat in a similar period of time
under similar circumstances.
2. A feeling that one cannot stop eating or control
what or how much one is eating.
SAME
B. Recurrent inappropriate compensatory behaviors in
order to prevent weight gain such as self-induced
vomiting; misuse of laxatives, diuretics, or other
medications; fasting or excessive exercise.
SAME
C. The binge eating and inappropriate compensatory
behaviors occur, on average, at least twice a week for
3 months.
C. The binge eating and inappropriate compensatory
behaviors occur, on average, at least once a week
for 3 months.
D. Self-evaluation is unjustifiability influenced by body
shape and weight.
SAME
E. The disturbance does not occur exclusively during
episodes of anorexia nervosa.
SAME
Specify type:
Purging type: During the current episode, the person
has regularly engaged in self-induced vomiting or the
misuse of laxatives, diuretics, or enemas.
Nonpurging Type: During the current episode, the
person has used inappropriate compensatory
behaviors, such as fasting or excessive exercise, but
has not regularly engaged in self-induced vomiting or
the misuse of laxatives, diuretics, or enemas.
Not a criterion.
Not a criterion. Specify if:
Partial remission: After full criteria were previously
met, some but not all of the criteria have been met
for a sustained period of time.
Full remission: After full criteria were previously
met, none of the criteria have been met for a
sustained period of time.
Not a criterion. Current severity
1
:
Mild: An average of 1-3 episodes of inappropriate
compensatory behaviors per week.
Moderate: An average of 4-7 episodes of
inappropriate compensatory behaviors per week.
Severe: An average of 8-13 episodes of
inappropriate compensatory behaviors per week.
Extreme: An average of 14 or more episodes of
inappropriate compensatory behaviors per week.
1
The level of severity may be increased to reflect other symptoms and the degree of functional disability.

50
Binge Eating Disorder. Binge eating disorder had been included in DSM-IV as a "criteria
set provided for further study," and has been included in DSM-5 as a disorder. This disorder is
characterized by binge or out of control eating accompanied by significant distress about eating.
Binge eating disorder is differentiated from bulimia nervosa in that there are no inappropriate
compensatory behaviors (e.g., purging or excessive exercise) seen in binge eating disorder. As
noted previously, this disorder was added into DSM-5 because a significant subset of people
presenting with an eating disorder had exhibited binge eating behaviors that were not
accompanied by any behaviors intended to compensate for the binge eating (Call, Walsh, &
Attia, 2013; Crow et al., 2012; Striegel-Moore & Franko, 2008). Changes between the criteria
enumerated in DSM-IV and those in DSM-5 are minimal. The only change, which represents a
less stringent requirement in DSM-5, reduces the minimum frequency/duration of the binge
eating behavior to at least once a week for 3 months (it had been at least 2 days a week for 6
months). Table 21 shows a comparison between DSM-IV and DSM-5 for binge eating disorder.
Table 21. DSM-IV to DSM-5 Binge Eating Disorder Comparison
DSM-IV DSM-5
Disorder Class: Criteria Sets and Axes Provided for Further
Study
Disorder Class: Feeding and Eating Disorders
A. Recurrent episodes of binge eating. An episode of binge
eating is characterized by both of the following:
1. Eating, in a discrete period of time (e.g., within any
2-hour period), an amount of food that is definitely
larger than most people would eat in a similar period
of time under similar circumstances
2. A sense of lack of control over eating during the
episode (e.g., a feeling that one cannot stop eating or
control what or how much one is eating)
SAME
B. The binge-eating episodes are associated with three (or
more) of the following:
1. Eating much more rapidly than normal
2. Eating until feeling uncomfortably full
3. Eating large amounts of food when not feeling
physically hungry
4. Eating alone because of feeling embarrassed by how
much one is eating
5. Feeling disgusted with oneself, depressed, or very
guilty after overeating
SAME
C. Marked distress regarding binge eating is present. SAME
D. The binge eating occurs, on average, at least 2 days a
week for 6 months.
Note: The method of determining frequency differs from
that used for bulimia nervosa; future research should
address whether the preferred method of setting a frequency
threshold is counting the number of days on which binges
occur or counting the number of episodes of binge eating.
D. The binge eating occurs, on average, at least
once a week for 3 months.
E. The binge eating is not associated with the regular use
of inappropriate compensatory behaviors (e.g., purging,
fasting, excessive exercise) and does not occur
exclusively during the course of anorexia nervosa or
bulimia nervosa.
SAME
(continued)

51
Table 21. DSM-IV to DSM-5 Binge-Eating Disorder Comparison (continued)
DSM-IV DSM-5
Disorder Class: Criteria Sets and Axes Provided for Further
Study
Disorder Class: Feeding and Eating Disorders
Specify if:
In partial remission: After full criteria for
binge-eating disorder were previously met,
binge eating occurs at an average frequency of
less than one episode per week for a sustained
period of time.
In full remission: After full criteria for binge-
eating disorder were previously met, none of
the criteria have been met for a sustained
period of time.
Specify current severity:
Severity is also noted in the diagnosis, from
mild to extreme:
Mild: 1-3 binge-eating episodes per week
Moderate: 4-7 binge-eating episodes per
week
Severe: 8-13 binge-eating episodes per
week
Extreme: 14 or more binge-eating episodes
per week
Avoidant/Restrictive Food Intake Disorder. DSM-IV feeding disorder of infancy or early
childhood has been renamed avoidant/restrictive food intake disorder, and the criteria have been
significantly expanded. The DSM-IV disorder was rarely used, and limited information is
available on its course and outcome or the characteristics of children with this disorder. A large
number of children and adolescents substantially restrict their food intake and experience
significant associated physiological or psychosocial problems but do not meet criteria for any
DSM-IV eating disorder. Avoidant/restrictive food intake disorder is a broad category intended
to capture this range of presentations. In the DSM-5 field trials in the United States and Canada
based on child clinical populations (general child psychiatry outpatient services),
avoidant/restrictive food intake disorder prevalence was described for one site
(Columbia/Cornell Medical Centers-New York) and it was 11 percent using DSM-5 (not
applicable for DSM-IV) (Regier et al., 2013). Table 22 shows a comparison between DSM-IV
and DSM-5 for avoidant/restrictive food intake disorder.

52
Table 22. DSM-IV to DSM-5 Avoidant/Restrictive Food Intake Disorder Comparison
DSM-IV DSM-5
Name: Feeding Disorder of Infancy or Early
Childhood
Name: Avoidant/Restrictive Food Intake Disorder
Disorder Class: Feeding and Eating Disorders of
Infancy or Early Childhood
Disorder Class: Feeding and Eating Disorders
A. Feeding disturbance as manifested by
persistent failure to eat adequately with
significant failure to gain weight or
significant loss of weight over at least 1
month.
A. An eating or feeding disturbance (e.g., apparent lack of
interest in eating or food; avoidance based on the sensory
characteristics of food; concern about aversive
consequences of eating) as manifested by persistent
failure to meet appropriate nutritional and/or energy needs
associated with one (or more) of the following:
1. Significant weight loss (or failure to achieve expected
weight gain or faltering growth in children)
2. Significant nutritional deficiency.
3. Dependence on enteral feeding or oral nutritional
supplements.
4. Marked interference with psychosocial functioning.
B. The disturbance is not due to an associated
gastrointestinal or other general medical
condition (e.g., esophageal reflux).
D. The eating disturbance is not attributable to a concurrent
medical condition or not better explained by another
mental disorder. When the eating disturbance occurs in
the context of another mental disorder, the severity of the
eating disturbance exceeds that routinely associated with
the condition or disorder and warrants additional clinical
attention.
C. The disturbance is not better accounted for
by another mental disorder (e.g., Rumination
Disorder) or by lack of available food.
B. The disturbance is not better explained by lack of
available food or by an associated culturally sanctioned
practice.
-- C. The eating disturbance does not occur exclusively during
the course of anorexia nervosa or bulimia nervosa, and
there is no evidence of a disturbance in the way in which
one's body weight or shape is experienced.
D. The onset is before age 6 years. DROPPED
D. The eating disturbance is not attributable to a concurrent
medical condition on not better explained by another
mental disorder. When the eating disturbance the eating
disturbance occurs in the context of another condition or
disorder, the severity of the eating disturbance exceeds
that routinely associated with the condition or disorder
and warrants additional clinical attention.
Specify if: In remission: After full criteria for
avoidance/restrictive food intake disorder were previously
met, the criteria have not been met for a sustained period of
time.
3.3.11 Body Dysmorphic Disorder (under Obsessive-compulsive and Related Disorders)
Body dysmorphic disorder (BDD) is a mental illness characterized by an excessive
preoccupation with a perceived physical defect or flaw that causes significant distress or
functional impairment. There have been several important changes in BDD criteria from
DSM-IV to DSM-5. First, BDD has been reclassified from somatoform disorders in DSM-IV to
53
obsessive-compulsive and related disorders under DSM-5. Second, DSM-5 BDD has an added
diagnostic criterion indicating that the patient must have had repetitive behaviors or mental acts
that were in response to preoccupations with perceived defects or flaws in physical appearance.
Third, a "with muscle dysmorphia" specifier has been added to reflect a growing literature on the
diagnostic validity and clinical utility of making this distinction in individuals with BDD.
Finally, the delusional variant of BDD (which identifies individuals who are completely
convinced that their perceived defects or flaws are truly abnormal in appearance) is no longer
coded as both a delusional disorder (somatic type) and BDD. Under DSM-5, this presentation is
designated only as BDD with the "absent insight/delusional beliefs" specifier and not as a
delusional disorder.
Under DSM-IV criteria, BDD was a fairly common disorder affecting approximately 2.4
percent of the general population at any time (point prevalence) as estimated by a random sample
telephone survey conducted in 2004 among 2,513 adults residing in the United States (Keel,
Brown, Holm-Denoma, & Bodell, 2011). As a comparison, this is similar to point prevalence
estimates of DSM-IV defined GAD. Estimates under DSM-5 criteria are not currently available
for children or adults. However, criteria-induced changes in the estimates are likely to be minor.
Over 90 percent of people with BDD report repetitive behaviors or mental acts in response to
their preoccupation with a perceived physical deficit (Able, Johnston, Adler, & Swindle, 2007),
and this was the only restrictive change to diagnostic criteria. BDD affects both males and
females and has been identified in children as young as age 5 and as old as age 80 (Able et al.,
2007). Moreover, patients with BDD report that unwanted, anxiety provoking obsessions related
to BDD cause significant distress (e.g., avoidance of social situations due to anxiety of being
ridiculed) and the repetitive behaviors are time consuming, functionally impairing (e.g., being
late for work due to compulsive compensatory behavior), and can be dangerous (e.g., skin
picking leading to infection). Suicidal thoughts is a significant concern among people with BDD;
suicidal ideation is as high as 80 percent in this population and one in four make a suicide
attempt (Able et al., 2007). There are very few prospective studies of BDD, but retrospective
studies suggest a mean onset of BDD around age 16 and indicate a chronic course with a low
probability of remission without treatment (Able et al., 2007). Since approximately 75 percent of
those with BDD meeting criteria for MDD as well, even if BDD was not assessed in a clinical
instrument, the majority of the cases with BDD would be classified as having SED due to co-
morbidity. Table 23 shows a comparison between DSM-IV and DSM-5 for body dysmorphic
disorder.

54
Table 23. DSM-IV to DSM-5 Body Dysmorphic Disorder Comparison
DSM-IV DSM-5
Disorder Class: Somatoform Disorders Disorder Class: Obsessive-Compulsive and Related
Disorders
A. Preoccupation with an imagined defect in
appearance. If a slight physical anomaly is
present, the person's concern is markedly
excessive.
A. Preoccupation with one or more perceived defects or
flaws in physical appearance that are not observable or
appear slight to others.
B. At some point during the course of the disorder, the
individual has performed repetitive behaviors (e.g.,
mirror checking, excessive grooming, skin picking,
reassurance seeking) or mental acts (e.g., comparing his
or her appearance with that of others) in response to the
appearance concerns.
B. The preoccupation causes clinically significant
distress or impairment in social, occupational,
or other important areas of functioning.
C. The preoccupation causes clinically significant distress or
impairment in social, occupational or other areas of
functioning.
C. The preoccupation is not better accounted for by
another mental disorder (e.g., dissatisfaction
with body shape and size in anorexia nervosa).
D. The appearance preoccupation is not better explained by
concerns with body fat or weight in an individual whose
symptoms meet diagnostic criteria for an eating disorder.
--
Specify if:
With muscle dysmorphia: The individual is preoccupied
with the idea that his or her body build is too small or
insufficiently muscular. This specifier is used even if the
individual is preoccupied with other body areas, which is
often the case.
Specify if:
Indicate degree of insight regarding body dysmorphic
disorder beliefs (e.g., "I look ugly" or "I look
deformed").
With good or fair insight: The individual recognizes
that the body dysmorphic disorder beliefs are
definitely or probably not true or that they may or
may not be true.
With poor insight: The individual thinks that the
body dysmorphic beliefs are probably true.
With absent insight/delusional beliefs: The individual
is completely convinced that the body dysmorphic
beliefs are true.

55
4. Instrumentation
The purpose of this section is to describe current plans to integrate the Diagnostic and
Statistical Manual of Mental Disorders, 5th ed. (DSM-5) changes into the leading diagnostic
instruments for assessing childhood mental disorders. Instrument developers provided
information about plans to update diagnostic interviews. Table 24 describes the major diagnostic
instruments, including both structured and semistructured interviews. Table 24 also describes the
diagnostic coverage for each instrument. The final column provides an update on the status of
each instrument's DSM-5 compatibility.
Table 24. Summary of Diagnostic Instruments Used to Assess Child Mental Disorders
Instrument
Age
Range Rater Mode
Diagnostic
Criteria
Diagnostic
Coverage
Administered
By DSM-5 Update
K-SADS 6-18
years
Child
Parent
In person
Phone
DSM-IV Affective, anxiety,
behavioral, eating,
psychotic,
substance abuse
Clinician Interview is DSM-5
compatible.
Computer version
under construction.
DISC-IV 6-17
years
Child
Parent
In person DSM-IV
ICD-10
Anxiety, mood,
schizophrenia,
behavior, substance
use, miscellaneous
disorders (30
disorders total)
Trained lay
interviewer
Not DSM-5
compatible.
Will possibly
update in the future.
CAPA 9-18
years
Child
Parent
In person
Phone
DSM-IV Anxiety, mood,
behavioral,
substance, and
antisocial
personality
Trained lay
interviewer (at
least bachelor
degree)
Scoring algorithms
will be updated.
NCS-A
CIDI
13-17
years
Child
Parent
In person
Phone
DSM-IV Mood, anxiety,
disruptive behavior,
substance use,
eating,
neurasthenia, and
suicidality (19
total)
Trained lay
interviewer
No plans to update.
PAPA 2-5
Years
Parent In person
Phone
DSM-IV Mood, anxiety,
disruptive
behaviors,
psychosis,
attachment,
enuresis, encopresis
Trained lay
interviewer
Scoring algorithms
will be updated.
YAPA 19-21
years
Self In person DSM-IV Mood, anxiety,
behavior disorders,
personality
disorders,
substance abuse,
risk factors, living
situations,
relationships
Trained lay
interviewer
Unknown
CAPA = Child and Adolescent Psychiatric Assessment; DISC-IV = Diagnostic Interview Schedule for Children, Version 4; DSM-IV =
Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; ICD-10 = International Classification of Disease, revision 10; K-SADS =
Kiddie-Schedule for Affective Disorders and Schizophrenia; NCS-A-CIDI = National Comorbidity Survey Replication Adolescent Supplement-
Composite International Diagnostic Interview; PAPA = Preschool Age Psychiatric Assessment; YAPA = Young Adult Psychiatric Assessment
56
In addition to their measurement of disorders and symptoms, these diagnostic interviews
also measure functional impairment. Each instrument measures functional impairment slightly
differently.
• The version of the Composite International Diagnostic Interview (CIDI) used in the
National Comorbidity Survey (NCS) for adults and adolescents includes an expanded
version of the Sheehan Disability Scale after each diagnostic module to assess overall
level of impairment associated with a disorder.
• The Child and Adolescent Psychiatric Assessment (CAPA), Preschool Age Psychiatric
Assessment (PAPA) and Young Adult Psychiatric Assessment (YAPA) interviews
incorporate some assessment of impairment within the diagnostic algorithms to establish
the presence of an Axis I disorder. For example, problems in school, arguments with
peers and family members, and legal actions are all assessed at the beginning of the
CAPA/PAPA/YAPA instruments prior to the diagnosis-specific modules on attention-
deficit/hyperactivity disorder (ADHD), depression, anxiety, oppositional defiant disorder
(ODD), and conduct disorder (CD). The CAPA/PAPA/YAPA instruments close with a
separate "incapacities" module that assesses impairment for all endorsed symptoms.
Interviewers are asked to review all problems or symptoms that emerged during the
interview. Then, taking these one at a time, they must determine whether symptoms in
that area caused incapacity. The interviewer is asked to distinguish two levels of
disturbance or impaired functioning—partial and severe. "Partial incapacity" refers to a
notable reduction of function in a particular area. If a person is still able to do things, but
does them less well or more slowly, then it is coded as a partial incapacity. "Severe
incapacity" refers to a complete, or almost complete, inability to function in a particular
area. If neither of these applies, the interviewer codes "absent."
• The Diagnostic Interview Schedule for Children (DISC) incorporates a series of
impairment questions at the end of each diagnostic section, which are only asked if a
"clinically significant" number of symptoms have already been endorsed, usually half or
more of those required for the diagnosis. These questions are uniform across all
diagnoses. They inquire as to whether the symptoms present during the last year have
resulted in any degree of impairment in six different social domains. Each set of
questions has a two-part structure, the first determining whether impairment is present
and the second measuring severity or frequency. The DISC assesses three levels of
impairment severity. The Clinical Report produced by the C-DISC generates a tally of the
degree of impairment. The separate SAS algorithms can also be used to generate
diagnoses with varying degrees of diagnosis-specific impairment.
• The Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS) determines
severity of a disorder using the Child Global Assessment of Functioning (C-GAF)
(Shaffer et al. 1983), which is administered as the sixth and final module of the
instrument. Severe impairment is indicated by a C-GAF score of 50 or less when a
diagnosis of an Axis I mental disorder is present. Moderate severity is indicated by a C-
GAF score in the range of 51-70 along with presence of an Axis 1 disorder. Mild severity
is indicated by a C-GAF score greater than 70 in the presence of an Axis 1 disorder.
One goal of the project is to develop a model that can predict SED using a mental health
screener and other predictor variables. One possible screener is the Strengths and Difficulties
57
Questionnaire (SDQ), which has been the subject of one validation study comparing parent SDQ
ratings with clinician ratings using the K-SADS (Kessler, Gruber, & Sampson, 2006), as well as
the Centers for Disease Control and Prevention's (CDC's) SDQ validation study, which
compared the SDQ with the CAPA/PAPA. These studies found that the SDQ had some limited
ability to predict presence of a disorder, depending on reporter (parent versus child) and severity
of disorder. For the purpose of this report, it should be noted that screeners are not directly tied to
DSM symptom classifications. Accordingly, the developers of the SDQ have confirmed that they
do not consider the SDQ to be a diagnostic instrument and therefore do not anticipate any
adaptations based on DSM-5 changes.
Finally, with increasing evidence about the comparable validity and reliability between
telephone and face-to-face administration of mental health interviews, psychiatric researchers
have been conducting clinical interviews over the telephone for the past 20 years (Aneshensel,
Frerichs, Clark, & Yokopenic, 1982; Reich & Earls, 1990; Rohde, Lewinsohn, & Seeley, 1997;
Sobin et al., 1993). In fact, telephone administration has become widely accepted as a way to
conduct clinical appraisals of both adults and adolescents (Kessler et al., 2009). However, most
of the research conducted with telephone administrations of diagnostic mental health interviews
has been done with adults. The only adolescent instrument to be directly compared by telephone
and face-to-face administration was the CIDI in an appraisal study performed by Kessler et al.
(2009). The CAPA and PAPA instruments have only been used in a limited fashion by
telephone, and no formal studies have compared CAPA or PAPA diagnostic outcomes (or for
many of the other diagnostic tools) when gathered in person versus by telephone. Duke
University investigators estimated that approximately 112 CAPA interviews were completed
over the telephone with 15- and 16-year-old adolescents in the Great Smoky Mountain Study
(GSMS). Among these 112 telephone CAPA interviews, the Duke investigators reported no
adverse events (e.g., reports to the Institutional Review Board for suspected child abuse or child
suicidal or homicidal ideation). The published literature does indicate that reliability, validity,
and epidemiological studies have been conducted by telephone with adolescents and children as
young as 12 years of age (Merikangas, Avenevoli, Costello, Koretz, & Kessler, 2009; Reich &
Earls, 1990; Rohde et al., 1997; Sobin, Weissman, Goldstein, & Adams, 1993). However, no
methodological work has been done to evaluate the specific impact of a change in the mode of
administration (from face to face to telephone) on the CAPA or PAPA outcomes.
58
This page intentionally left blank
59
5. Summary and Conclusions
Changes included in the fifth edition of the Diagnostic and Statistical Manual of Mental
Disorders (DSM-5) raise issues relevant to the definition of childhood serious emotional
disturbance (SED). Within the original Federal Register definition, SED was defined as
including "any diagnosable mental, behavioral, or emotional disorder of sufficient duration to
meet diagnostic criteria specified within the Diagnostic and Statistical Manual of Mental
Disorders, Third Edition, Revised (DSM-III-R)." Diagnostic "V" codes and Axis II disorders
(personality disorders and mental retardation) as well as substance use disorders (SUDs),
pervasive developmental disorder (PDD), and autism were all specifically excluded. The Federal
Register made no specific mention of learning disorders; however, these are not usually
considered in operational definitions of SED. With the release of the DSM-5, three specific
issues could be considered:
1. Due to the DSM-5 removal of the Axis system, the operational definition of SED may
now need to explicitly state which DSM-5 mental disorders are excluded from the
SED definition of "any DSM-5 mental disorder."
2. A decision will need to be made about which disorders within the new DSM-5
neurodevelopmental disorders class should be included versus excluded within the
definition of SED. Many, but not all, disorders within the neurodevelopmental
disorders were previously excluded from the 1993 definition.
3. A decision will need to be made as to whether one of the new DSM-5 childhood
disorders, social communication disorder (SCD), should be included as meeting
criteria for SED. If SCD is considered a "developmental disorder," it might be
excluded based upon the 1993 SED definition.
DSM-5 changes also will impact the diagnostic instruments used to assess the presence of
a mental disorder in childhood. Only one diagnostic interview for children and adolescents, the
Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS), has already been
updated to explicitly use DSM-5 diagnostic criteria. The scoring algorithms associated with the
Child and Adolescent Psychiatric Assessment (CAPA) and Preschool Age Psychiatric
Assessment (PAPA) will be updated to accommodate new DSM-5 diagnostic changes. This is
possible within the CAPA and PAPA interviews as they are symptom and functioning based and
not structured in diagnostic-specific modules like the other diagnostic interviews. CAPA and
PAPA scoring algorithms use questions embedded in the entire instrument to indicate the
presence of particular mental disorders. The Diagnostic Interview Schedule for Children (DISC)
will possibly be updated in the future, but the developers did not articulate a specific plan to do
so. Particularly in the near future, the release of the DSM-5 will narrow the number of diagnostic
measures to be considered for use in children's mental health surveillance efforts.
Research examining the impact of DSM-5 changes suggests that there may be a slight
increase in the overarching prevalence of diagnosed mental disorders among children and
adolescents. The potential for this slight increase stems mainly from the changed criteria for
attention-deficit/hyperactivity disorder (ADHD)—the new impulsivity criteria and lower
percentage of criteria needed for the diagnosis. A much smaller increase may be due to the
60
lowered age of onset for post-traumatic stress disorder (PTSD). Epidemiological studies,
including an assessment of eating disorders among adolescents, may also see an increase in
eating disorder-specific prevalence estimates. Most DSM-5 changes for children reclassified
disorders from one category to another. These changes would have no overarching impact on an
estimate of "any mental disorder." For instance, the prevalence of ODD is expected to decrease
using DSM-5 as some cases will now be diagnosed under the new disruptive mood dysregulation
disorder (DMDD).
The definition of SED includes the presence of both a childhood mental disorder and
functional impairment. If the additional cases identified with updated DSM-5 criteria are not
accompanied by functional impairments that substantially interfere with a child's ability to
function at home, school, or in the community, an SED prevalence estimate would not be
significantly impacted. DSM-5 field trials examined impact on prevalence estimates without
consideration of functioning. Additional research will be necessary to determine the full impact
of DSM-5 changes specifically on estimates of the prevalence of SED among children and
adolescents.
61
References
Aneshensel, C. S., Frerichs, R. R., Clark, V. A., & Yokopenic, P. A. (1982).Measuring
depression in the community: A comparison of telephone and personal interviews. Public
Opinion Quarterly, 46(1), 110-121.
Able, S. L., Johnston, J. A., Adler, L. A., & Swindle, R. W. (2007). Functional and psychosocial
impairment in adults with undiagnosed ADHD. Psychological Medicine, 37(01), 97-107. doi:
doi:10.1017/S0033291706008713
Allen, K. L., Byrne, S. M., Oddy, W. H., & Crosby, R. D. (2013). DSM-IV-TR and DSM-5
eating disorders in adolescents: Prevalence, stability, and psychosocial correlates in a population-
based sample of male and female adolescents. Journal of Abnormal Psychology, 122(3), 720-
732. doi: 10.1037/a0034004
American Psychiatric Association. (1987). Diagnostic and Statistical Manual of Mental
Disorders, 3rd revised edition. Arlington, VA: Author.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental
disorders, 4th edition. Arlington, VA: Author.
American Psychiatric Association. (2013a). Conduct Disorder. Retrieved April 28, 2014, from
http://www.dsm5.org/Documents/Conduct%20Disorder%20Factsheet%20Rev%209%206%2013
.pdf
American Psychiatric Association. (2013b). Diagnosis and statistical manual of mental
disorders, 5th edition. Arlington, VA: Author.
American Psychiatric Association. (2013c). Highlight of changes from DSM-IV-TR to DSM 5.
Retrieved April 28, 2014, from http://www.dsm5.org/Documents/changes%20from%20dsm-iv-
tr%20to%20dsm-5.pdf
American Psychiatric Association. (2013d). Posttraumatic stress disorder. Retrieved April 28,
2014, from http://www.dsm5.org/Documents/PTSD%20Fact%20Sheet.pdf
Axelson, D. (2013). Taking disruptive mood dysregulation disorder out for a test drive.
American Journal of Psychiatry, 170(2), 136-139. doi: 10.1176/appi.ajp.2012.12111434
Barry, T. D., Marcus, D. K., Barry, C. T., & Coccaro, E. F. (2013). The latent structure of
oppositional defiant disorder in children and adults. Journal of Psychiatric Research, 47(12),
1932-1939. doi:10.1016/j.jpsychires.2013.08.016
Burstein, M., He, J. P., Kattan, G., Albano, A. M., Avenevoli, S., & Merikangas, K. R. (2011).
Social phobia and subtypes in the National Comorbidity Survey-Adolescent Supplement:
Prevalence, correlates, and comorbidity. Journal of the American Academy of Child and
Adolescent Psychiatry, 50(9), 870-880. doi: 10.1016/j.jaac.2011.06.005
62
Call, C., Walsh, B. T., & Attia, E. (2013). From DSM-IV to DSM-5: changes to eating disorder
diagnoses. Current Opinion in Psychiatry, 26(6), 532-536. doi:
10.1097/YCO.0b013e328365a321
Center for Behavioral Health Statistics and Quality. (in review). Impact of the DSM-IV to DSM-
5 Conversion on the National Survey On Drug Use and Health and the Mental Health
Surveillance Study. Substance Abuse and Mental Health Services Administration, Rockville,
MD
Copeland, W. E., Angold, A., Costello, E. J., & Egger, H. (2013). Prevalence, comorbidity, and
correlates of DSM-5 proposed disruptive mood dysregulation disorder. American Journal of
Psychiatry, 170(2), 173-179. doi: 10.1176/appi.ajp.2012.12010132
Copeland, W. E., Keeler, G., Angold, A., & Costello, E. J. (2007). Traumatic events and
posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577-584. doi:
10.1001/archpsyc.64.5.577
Costello, E. M., Mustillo, S., Erkanli, A., Keeler, G., & Angold, A. (2003). Prevalence and
Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General
Psychiatry, 60(8), 837-844.
Crow, S. J., Swanson, S. A., Peterson, C. B., Crosby, R. D., Wonderlich, S. A., & Mitchell, J. E.
(2012). Latent class analysis of eating disorders: Relationship to mortality. Journal of Abnormal
Psychology, 121(1), 225-231. doi: 10.1037/a0024455
Egger, H. L., Erkanli, A., Keeler, G., Potts, E., Walter, B. K., & Angold, A. (2006). Test-retest
reliability of the Preschool Age Psychiatric Assessment (PAPA). Journal of the American
Academy of Child and Adolescent Psychiatry, 45(5), 538-549. doi:
10.1097/01.chi.0000205705.71194.b8
Fox, J., & Jones, K. D. (2013). DSM-5 and bereavement: The loss of normal grief? Journal of
Counseling and Development, 91(1), 113-119. doi: DOI 10.1002/j.1556-6676.2013.00079.x
Frances, A. (2010). Opening Pandora's box: The 19 worst suggestions for DSM-5. Psychiatric
Times, 27(9).
Gibson, J., Adams, C., Lockton, E., & Green, J. (2013). Social communication disorder outside
autism? A diagnostic classification approach to delineating pragmatic language impairment, high
functioning autism and specific language impairment. Journal of Child Psychology and
Psychiatry, 54(11), 1186-1197. doi: 10.1111/jcpp.12079
Huerta, M., Bishop, S. L., Duncan, A., Hus, V., & Lord, C. (2012). Application of DSM-5
Criteria for Autism Spectrum Disorder to Three Samples of Children With DSM-IV Diagnoses
of Pervasive Developmental Disorders. American Journal of Psychiatry, 169(10), 1056-1064.
doi: 10.1176/appi.ajp.2012.12020276
63
Keel, P. K., Brown, T. A., Holm-Denoma, J., & Bodell, L. P. (2011). Comparison of DSM-IV
versus proposed DSM-5 diagnostic criteria for eating disorders: Reduction of eating disorder not
otherwise specified and validity. International Journal of Eating Disorders, 44(6), 553-560. doi:
10.1002/eat.20892
Kerns, C. E., Comer, J. S., Pincus, D. B., & Hofmann, S. G. (2013). Evaluation of the proposed
social anxiety disorder specifier change for DSM-5 in a treatment seeking sample of anxious
youth. Depression and Anxiety, 30(8), 709-715. doi: 10.1002/da.22067
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005).
Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national
comorbidity survey replication. Archives of General Psychiatry, 62(7), 768-768.
Kessler, R. C., Gruber, M., & Sampson, N. (2006, December 21). Validation studies of mental
health indices in the National Health Interview Survey (presented to the Centers for Disease
Control and Prevention). Retrieved from http://www.hcp.med.harvard.edu/ncs/scales.php
Kessler, R. C., Avenevoli, S., Green, J., Gruber, M. J., Guyer, M., He, Y., Jin, R., Kaufman, J.,
Sampson, N. A., & Zaslavsky, A. M. (2009, April). National Comorbidity Survey Replication
Adolescent Supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical
reassessments. Journal of the American Academy of Child & Adolescent Psychiatry, 48, 386-
399. doi: 10.1097/CHI.0b013e31819a1cbc
Kessler, R. C., Avenevoli, S., Costello, J., Green, J. G., Gruber, M. J., McLaughlin, K. A., . . .
Merikangas, K. R. (2012). Severity of 12-month DSM-IV disorders in the National Comorbidity
Survey Replication Adolescent Supplement. Archives of General Psychiatry, 69, 381-389.
Krieger, F. V., Polanczyk, G. V., Goodman, R., Rohde, L. A., Graeff-Martins, A. S., Salum, G., .
. . Stringaris, A. (2013). Dimensions of oppositionalay in a Brazilian community sample: Testing
the DSM-5 proposal and etiological links. Journal of the American Academy of Child and
Adolescent Psychiatry, 52(4), 389-400. doi: 10.1016/j.jaac.2013.01.004
Leigh, E., Smith, P., Milavic, G., & Stringaris, A. (2012). Mood regulation in youth: research
findings and clinical approaches to irritability and short-lived episodes of mania-like symptoms.
Current Opinion in Psychiatry, 25(4), 271-276. doi: 10.1097/YCO.0b013e3283534982
McPartland, J. C., Reichow, B., & Volkmar, F. R. (2012). Sensitivity and specificity of proposed
DSM-5 diagnostic criteria for autism spectrum disorder. Journal of the American Academy of
Child and Adolescent Psychiatry, 51(4), 368-383. doi: 10.1016/j.jaac.2012.01.007
Merikangas, K. R., Avenevoli, S., Costello, E. J., Koretz, D., & Kessler, R. C. (2009). National
Comorbidity Survey Replication Adolescent Supplement (NCS-A): I. Background and
Measures. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 367-369.
Merikangas, K. R., He, J. P., Brody, D., Fisher, P. W., Bourdon, K., & Koretz, D. S. (2010).
Prevalence and treatment of mental disorders among U.S. children in the 2001-2004 NHANES.
Pediatrics, 125, 75-81.
64
Norbury, C. F. (2014). Practitioner review: Social (pragmatic) communication disorder
conceptualization, evidence and clinical implications. Journal of Child Psychology and
Psychiatry, 55(3), 204-216.
Ornstein, R. M., Rosen, D. S., Mammel, K. A., Callahan, S. T., Forman, S., Jay, M. S., . . .
Walsh, B. T. (2013). Distribution of eating disorders in children and adolescents using the
proposed DSM-5 criteria for feeding and eating disorders. Journal of Adolescent Health, 53(2),
303-305. doi: 10.1016/j.jadohealth.2013.03.025
Polanczyk, G., Caspi, A., Houts, R., Kollins, S. H., Rohde, L. A., & Moffitt, T. E. (2010).
Implications of extending the ADHD age-of-onset criterion to age 12: Results from a
prospectively studied birth cohort. Journal of the American Academy of Child and Adolescent
Psychiatry, 49(3), 210-216. doi: 10.1016/j.jaac.2009.12.014
Regier, D. A., Narrow, W. E., Clarke, D. E., Kraemer, H. C., Kuramoto, S. J., Kuhl, E. A., &
Kupfer, D. J. (2013). DSM-5 field trials in the United States and Canada, Part II: Test-Retest
Reliability of Selected Categorical Diagnoses. American Journal of Psychiatry, 170(1), 59-70.
doi: 10.1176/appi.ajp.2012.12070999
Reich, W., & Earls, F. (1990). Interviewing adolescents by telephone: Is it a useful
methodological strategy? Comprehensive Psychiatry, 31, 211-215.
Rohde, P., Lewinsohn, P. M., & Seeley, J. R. (1997). Comparability of telephone and face-to-
face interviews in assessing axis I and axis II disorders. American Journal of Psychiatry, 154,
1593-1598.
Scheeringa, M. S., Zeanah, C. H., & Cohen, J. A. (2011). PTSD in children and adolescents:
Toward an empirically based algorithm. Depression and Anxiety, 28(9), 770-782. doi:
10.1002/da.20736
Shaffer, D., Gould, M. S., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., & Aluwahlia, S. (1983).
A children's global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228-
1231.
Sobin, E., Weissman, M. M., Goldstein, R. B., & Adams, P. (1993). Diagnostic interviewing for
family studies: Comparing telephone and face-to-face methods for the diagnosis of lifetime
psychiatric disorders. Psychiatric Genetics, 3, 227-233. doi: 10.1097/00041444-199324000-
00005
St Pourcain, B., Mandy, W. P., Heron, J., Golding, J., Smith, G. D., & Skuse, D. H. (2011).
Links between co-occurring social-communication and hyperactive-inattentive trait trajectories.
Journal of the American Academy of Child and Adolescent Psychiatry, 50(9), 892-902. doi:
10.1016/j.jaac.2011.05.015
Striegel-Moore, R. H., & Franko, D. L. (2008). Should binge eating disorder be included in the
DSM-V? A critical review of the state of the evidence. Annual Review of Clinical Psychology, 4,
305-324. doi: 10.1146/annurev.clinpsy.4.022007.141149
65
Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
(1992, November 6). Community Mental Health Services Block Grant. Federal Register, 57 FR
53118
Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
(1993, May 20). Defining serious emotional disturbance in children: Final notice. Federal
Register, 58(96), 29422-29425.
Uher, R., Payne, J. L., Pavlova, B., & Perlis, R. H. (2013). Major Depressive Disorder in DSM-
5: Implications for Clinical Practice and Research of Changes from DSM-IV. Depression and
Anxiety. doi: 10.1002/da.22217
66
This page intentionally left blank
