
AUTISM COMPANION
TSHA SI DISABILITY
DETERMINATION GUIDELINES FOR
LANGUAGE DISORDER
REVISED 2021
Autism Companion – Language Guidelines Revision Team
Laura Bray, MS, CCC-SLP
Nichole Brezel, MS, CCC-SLP
Janie Life, MS, CCC-SLP
Jennifer Negron, MS, CCC-SLP
Mandy Staton, MS, CCC-SLP
Sara Wilkerson, MS, CCC-SLP
With input from Maeghan R. Medina, LSSP, NCSP
Autism Companion - Language Guidelines Peer Reviewers
Jessica Carter, MS, CCC-SLP
Dana Eckles, MS, CCC-SLP
Nancy Lontos, MS, CCC-SLP
JoAnn Wiechmann, EdD, CCC-SLP
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 1
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Table of Contents
General Information ......................................................................................................................4
Purpose and Intended Use of the Autism Companion to SI Disability
Determination for Language Disorders ...............................................................................5
Definitions............................................................................................................................6
Classification System for Autism ........................................................................................7
Core Characteristics of Autism Spectrum Disorder ...........................................................11
Data Collection for District Referral/RTI/MTSS Process .......................................................14
Data Collection ..................................................................................................................15
Referral Considerations .....................................................................................................15
Components of a Comprehensive Autism Evaluation ..............................................................17
Comprehensive Multidisciplinary Team Evaluations ........................................................18
Four Phases of the Language Evaluation ...........................................................................19
Phase I of Evaluation: Assessment Plan ....................................................................................21
Assessment Planning Activities .........................................................................................22
Assessment Questions ........................................................................................................23
Assessment Plan.................................................................................................................24
Phase II of Evaluation: Data Collection.....................................................................................26
Step-by-Step for Disability Determination ........................................................................27
Formal Assessment for Autism Spectrum Disorder ..........................................................28
Formal Assessment of Pragmatic Language ......................................................................30
Indirect Formal Assessment of Pragmatic Language ........................................................32
Criterion-Referenced and Informal Assessment of Pragmatic Language ..........................33
Phase III of Evaluation: Analysis and Interpretation ..............................................................36
Disability Determination ....................................................................................................37
Recommendation to Admission, Review, Dismissal Committee ......................................44
Phase IV of Evaluation: Evaluation Report ..............................................................................46
Report Writing Considerations ..........................................................................................47
Sample Wording in Full Individual Evaluation Report .....................................................47
Sample Intervention Goals Based on Core Characteristics in ASD ..................................49
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 2
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Re-Evaluation ...............................................................................................................................50
Re-evaluation Considerations ............................................................................................51
Dismissal .......................................................................................................................................52
Dismissal Considerations ...................................................................................................53
Forms ............................................................................................................................................56
Guiding Questions to Assist in Determining Need for Referral ........................................57
Evaluation Phase I: Assessment Plan ................................................................................60
Assessment Planning Worksheet ...........................................................................61
Assessment Plan.....................................................................................................64
Evaluation Phase II: Data Collection Forms ......................................................................65
Parent Teacher Communication Survey ................................................................66
Encuesta de Communicaciόn Entre Padres/Maestros ............................................70
Observation of Student Communication within the School Environment .............75
Observation of the School Environment to Facilitate Communication .................77
Play-Based Skills Assessment ...............................................................................80
Communicative Intent Checklist............................................................................87
Gestural Skills Checklist ........................................................................................88
Conversational Skills Checklist .............................................................................90
Evaluation Phase III: Analysis and Interpretation Forms ..................................................93
Language Evaluation Summary Form ...................................................................94
Initial Disability Determination Worksheet ...........................................................98
Re-Evaluation Form .........................................................................................................103
Re-Evaluation Disability Determination Worksheet:
Autism/Speech Impairment .................................................................................104
Dismissal Form ................................................................................................................111
Factors to Consider in Dismissal from SLP Therapy Services ........................................112
References ...................................................................................................................................113
Appendices ..................................................................................................................................119
Appendix A Classification System of Social Communication Disorder .....................120
Appendix B Core Characteristics of Social Communication Disorder ........................121
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 3
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix C Service Delivery Framework and Systems of Supports ..........................122
Appendix D Language Development Milestones to Consider .....................................125
Appendix E Speech Impairment Eligibility Flowchart when Considering Autism .....131
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 4
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
General Information

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 5
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Purpose and Intended Use of the Autism Companion to the SI Disability
Determination Guidelines for Language Disorder
The purpose of these Eligibility Guidelines is to provide a structure within which the
speech-language pathologist can participate as an integral member of the multidisciplinary
team in using consistent evaluation practices to describe the social communication impairment
that is present in children with autism, and to assist in the deliberation of eligibility for special
education on the basis of autism and/or speech impairment. As a member of the multi-
disciplinary team, the SLP may support the team in:
Completing a comprehensive evaluation of a student’s communication, language,
and learning profile;
Describing the nature of the social communication impairment that is present for
students identified with autism; and
Making recommendations to the Admission, Review, Dismissal (ARD) Committee
regarding eligibility for special education services and supports based on autism
and/or speech impairment.
The 2004 Individuals with Disabilities Education Act (IDEA) provides the following definitions:
Autism means a developmental disability significantly affecting verbal and nonverbal
communication and social interaction, generally evident before age 3, which adversely
affects a child’s educational performance. Other characteristics often associated with
autism are engagement in repetitive activities and stereotyped movements, resistance
to environmental change or change in daily routines, and unusual responses to sensory
experiences. The term does not apply if a child’s educational performance is adversely
affected primarily because the child has an emotional disturbance as defined by IDEA
criteria.
A child who manifests the characteristics of autism after age 3 could be diagnosed as
having autism if the criteria in the preceding paragraph are met (Code of Federal
Regulations [CFR], 2006; 34CFR § 300.7 (c) (1)).
Speech-Language Impairment means a communication disorder, such as stuttering,
impaired articulation, language impairment, or a voice impairment that adversely
affects a child’s educational performance (CFR, 2006; 34CFR § 300.101 (c) (11)).
The Texas Administrative Code (TAC) defines a student with autism as one who has
been determined to meet the criteria for autism as stated in (CFR, 2006; 34CFR, § 300.7 (c)
(1)). Students with pervasive developmental disorders are included under this category.
The team’s written report of evaluation shall include specific recommendations for
behavioral interventions and strategies (TAC, 2018; 19TAC § 89.1040 (c) (1)).

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 6
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
SLPs play a central role in the screening, assessment, diagnosis, and treatment of
persons with autism spectrum disorders (ASHA, Autism, 2016,). Individuals with autism have a
developmental disability that affects social communication skills, that is, use of language.
Regardless of the presence or absence of difficulties acquiring the form and content of
language, individuals with autism spectrum disorders may be eligible for speech-language
pathology services due to the varying levels of severity of their social communication
impairment.
SLPs provide evaluation and services to students with autism spectrum disorders
through an individualized educational program when the language disorder and social
communication disorder result in an adverse effect on educational performance. In order for a
student to meet the federal and state definition of Speech Impairment, the communication
disorder must result in an adverse effect on educational performance (academic achievement
and/or functional performance). The purpose of this manual is to provide guidance for the SLP
in describing and documenting the student’s communication profile whether or not there is an
educational need for speech-language pathology services.
Definitions
Autism
Autism is a neurodevelopmental disorder defined by impairments in social reciprocity
and lack of communicative competence and is accompanied by restricted, repetitive patterns of
behavior, interests and activities.
Communication Disorder
A communication disorder is an impairment in the ability to receive, send, process, and
comprehend concepts or verbal, nonverbal, and graphic symbol systems. A communication
disorder may be evident in the processes of hearing, language, and/or speech. A
communication disorder may range in severity from mild to profound. It may be developmental
or acquired.
Individuals may demonstrate one or any combination of communication disorders. A
communication disorder may result in a primary disability or it may be secondary to other
disabilities (ASHA, 1993).

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 7
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Language Disorder
A language disorder is an impairment in comprehension and/or use of a spoken, written,
and/or other communication symbol system (e.g., American Sign Language). The disorder may
involve the form of language (phonology, morphology, syntax), the content of language
(semantics), and/or the function of language in communication (pragmatics) in any combination
(ASHA, 1993). Language disorders may persist across the lifespan, and symptoms may change
over time (Bashir, 1989). Further, a language disorder can be a distinct diagnosis or may occur
within the context of other conditions.
A regional, social, or cultural/ethnic variation of a symbol system should not be considered
a disorder of speech or language (ASHA, 1993; ASHA, Language in Brief, n.d.).
Social Communication Disorder (SCD)
SCD includes individuals who have significant problems using verbal and nonverbal
communication for social purposes leading to impairments in their ability to effectively
communicate, participate socially, maintain social relationships, or otherwise perform
academically or occupationally, that is not otherwise explained by low cognitive ability. Notably,
it does not include the presence of restrictive or repetitive patterns of behavior. A robust
description, including the DSM-5 criteria, is included in Appendix A.
Speech-Language Impairment
This term is used in IDEA 2004 to mean a communication disorder, such as stuttering,
impaired articulation, language impairment, or voice impairment that adversely affects a child’s
educational performance (CFR, 2006; 34CFR § 300.101 (c) (11)).
Classification System for Autism
A multidisciplinary team (MDT) makes determinations using IDEA criteria in the
schools; however, medical diagnoses are established through DSM-5 criteria. A medical
diagnosis of autism is not sufficient to establish eligibility for special education services under
IDEA as other factors including educational need must be present.
The Diagnostic and Statistical Manual of Mental Health Disorders, Fifth Edition (DSM
5; APA, 2013) sets forth the most commonly used classification system for diagnostic criteria
for autism spectrum disorder. The DSM-5 has consolidated the previously categorized Pervasive
Developmental Disorder (PDD), which included five diagnoses under the autism spectrum:
autistic disorder, Asperger’s Syndrome, childhood disintegrative disorder, Rett’s Syndrome, and
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 8
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) into one umbrella
diagnosis of “Autism Spectrum Disorder” (ASD).
The DSM-5 states ASD is characterized by:
● Persistent deficits in social communication and social interaction across multiple
contexts, as manifested by the following currently or by history:
○ Deficits in social-emotional reciprocity, ranging, for example, from abnormal social
approach and failure of normal back-and-forth conversation; to reduced sharing of
interests, emotions, or affect; to failure to initiate or respond to social interactions.
○ Deficits in nonverbal communication behaviors used for social interaction, ranging,
for example, from poorly integrated verbal and nonverbal communication; to
abnormalities in eye contact and body language or deficits in understanding and use
of gestures; to a total lack of facial expressions and nonverbal communication.
○ Deficits in developing, maintaining, and understanding relationships, ranging, for
example, from difficulties adjusting behavior to suit various social contexts; to
difficulties in sharing imaginative play or in making friends; to absence of interest in
peers.
Specify current severity: Severity is based on social communication impairments and
restricted repetitive patterns of behavior. (See table below.)
● Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least
two of the following, currently or by history:
○ Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple
motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic
phrases).
○ Insistence on sameness, inflexible adherence to routines, or ritualized patterns or
verbal nonverbal behavior (e.g., extreme distress at small changes, difficulties with
transitions, rigid thinking patterns, greeting rituals, need to take the same route or eat
the same food every day).
○ Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong
attachment to or preoccupation with unusual objects, excessively circumscribed or
preservative interest).
○ Hyper- or hypo-reactivity to sensory input or unusual interests in sensory aspects of
the environment (e.g., apparent indifference to pain/temperature, adverse response to
specific sounds or textures, excessive smelling or touching of objects, visual
fascination with lights or movement).
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 9
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Specific current severity: Severity is based on social communication impairments and
restricted, repetitive patterns of behavior. (See table below).
● Symptoms must be present in the early developmental period (but may not become fully
manifest until social demands exceed limited capacities or may be masked by learning
strategies in later life).
● Symptoms cause clinically significant impairment in social, occupational, or other
important areas of current functioning.
● These disturbances are not better explained by intellectual disability (intellectual
development disorder) or global developmental delay. Intellectual disability and autism
spectrum disorder frequently co-occur; to make comorbid diagnosis of autism spectrum
disorder and intellectual disability, social communication should be below that expected
for general developmental level.
Note: Individuals with a well-established DSM-IV (APA, 1994) diagnosis of autistic
disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified
should be given the diagnosis of autism spectrum disorder. Individuals who have marked deficits
of social communication, but whose symptoms do not otherwise meet criteria for autism
spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Specify if:
● With or without accompanying intellectual impairment.
● With or without accompanying language impairment.
● Associated with a known medical or genetic condition or environmental factor (Coding
note: Use additional code to identify the associated medical or genetic condition.).
● Associated with another neurodevelopmental, mental, or behavioral disorder (Coding
note: Use additional code[s] to identify the associated neurodevelopmental, mental, or
behavioral disorder[s].).
● With catatonia.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 10
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Table 1
Severity Levels for Autism Spectrum Disorder
Severity Level Level 3
“Requiring very
substantial support”
Level 2
“Requiring substantial
support”
Level 1
“Requiring support”
Social
Communication
Severe deficits in
verbal and nonverbal
social communication
skills cause severe
impairments in
functioning, very
limited initiation of
social interactions,
and minimal response
to social overtures
from others. For
example, a person
with few words of
intelligible speech
who rarely initiates
interaction and, when
he or she does, makes
unusual approaches to
meet needs only and
responds to only very
direct social
approaches
Marked deficits in
verbal and nonverbal
social communication
skills; social
impairments apparent
even with supports in
place; limited initiation
of social interactions;
and reduced or
abnormal responses to
social overtures from
others. For example, a
person who speaks
simple sentences, whose
interaction is limited to
narrow special interests,
and who has markedly
odd nonverbal
communication.
Without supports in
place, deficits in social
communication cause
noticeable impairments.
Difficulty initiating
social interactions, and
clear examples of
atypical or unsuccessful
response to social
overtures of others.
May appear to have
decreased interest in
social interactions. For
example, a person who
is able to speak in full
sentences and engages
in communication but
whose to-and-fro
conversation with
others fails, and whose
attempts to make
friends are odd and
typically unsuccessful.
Restricted,
Repetitive
Behaviors
Inflexibility of
behavior, extreme
difficulty coping with
change, or other
restricted/repetitive
behaviors markedly
interfere with
functioning in all
spheres. Great
distress/difficulty
changing focus or
action.
Inflexibility of behavior,
difficulty coping with
change, or other
restricted/repetitive
behaviors appear
frequently enough to be
obvious to the casual
observer and interfere
with functioning in a
variety of contexts.
Distress and/or
difficulty changing
focus or action.
Inflexibility of behavior
causes significant
interference with
functioning in one or
more contexts.
Difficulty switching
between activities.
Problems of
organization and
planning hamper
independence

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 11
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Core Characteristics of Autism Spectrum Disorder
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by
deficits in social communication and social interaction and the presence of restricted, repetitive
behaviors. Social communication deficits include impairments in aspects of joint attention and
social reciprocity, as well as challenges in the use of verbal and nonverbal communicative
behaviors for social interaction. Restricted, repetitive behaviors, interests, or activities are
manifested by stereotyped, repetitive speech, motor movement, or use of objects; inflexible
adherence to routines; restricted interests; and hyper- and/or hypo-sensitivity to sensory input.
There is great heterogeneity in the population of individuals identified with ASD with a
wide range of cognitive, social communication, motor, and adaptive abilities. However,
noticeable difficulty in the area of social communication is the common characteristic integral
to the diagnostic criteria of ASD. Many students with ASD have difficulty acquiring the form
and content of language and/or augmentative and alternative communication systems; and all
the students with ASD have difficulty acquiring social use of communication.
Joint Attention
Joint attention includes social orienting, establishing shared attention, monitoring
emotional states, and considering another’s intentions. In typical development, infants
demonstrate predisposition to orient to social stimuli by focusing on a caregiver’s eyes and
direction of gaze, facial expressions, voice, and gestures. All of these behaviors support the
development of joint attention. With joint attention, a child recognizes another’s visual line of
regard, directs another person’s attention to objects or actions, determines another person’s
intentions, and in time, learns to modify language use based on knowledge of another person’s
experiences. Early joint attention routines are critical for developing the ability to share ideas,
internal states, and plans.
For individuals with ASD, challenges in acquiring joint attention skills inhibit
development of early communicative intent, social functions of communication, and language
acquisition. Young children with ASD may demonstrate limited ability to notice people in their
environment or respond to familiar voices. In addition, they often show limited ability to follow
another person’s focus of attention, shift gaze between people and objects, and follow gestures.
These early limitations in turn affect later social language use for commenting, requesting
information, and sharing experiences (Dawson et al., 2004; Wetherby et al., 1998).
Shared Enjoyment/Emotions
Sharing emotions and inferring the emotional state of others are important aspects of
social communication. Individuals with ASD tend to show less attention to emotional displays of
distress or discomfort than typically developing peers, and they tend to display less shared
positive affect and less emotional reciprocity following praise. As communicative intent

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 12
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
develops, children with ASD may communicate for requesting and protesting objects or
activities, but show restricted or delayed development of communicating functions of seeking
comfort, initiating social games, praising others, and commenting to share enjoyment and
interests (Wetherby, 1986; Wetherby et al., 1998; Wetherby & Prutting, 1984).
Social Reciprocity
Social reciprocity includes behaviors such as initiating bids for interaction, maintaining
interactions by taking turns, and providing contingent responses to bids for interaction initiated
by others. Children who both initiate and follow the attentional focus of communication partners
are most likely to develop sophisticated social communication and language (Carpenter &
Tomasello, 2000). Children with ASD often show a developmental history marked by a
decreased frequency of spontaneous bids for communication and a reliance on more structured
situations to engage in conversational exchanges (Landry & Loveland, 1989). This pattern of
development results in limited opportunities for children with ASD to initiate conventional
communication, respond to the model of others, and acquire more sophisticated language.
Early in development many children with ASD demonstrate limited gestures for
communication, limited back-and-forth communication exchanges, inattention to breakdowns in
communication, and a passive conversational style. Later in development, difficulty with social
reciprocity is marked by difficulty providing relevant remarks in response to topics initiated by
others, providing expansion comments, requesting information to maintain the conversational
exchange, and providing essential background information (Lord & Paul, 1997).
Nonverbal Communication
Using and understanding nonverbal communication, including facial expressions,
gestures, body language, proximity, and eye gaze are fundamental to successful social
communication. A meta-analysis of research related to recognition of emotions found there is
indeed a general impairment in emotion recognition in individuals with ASD. Individuals with
autism might be slower to recognize emotions, or might have more difficulty with dynamically
moving faces than with static photos. Tentative evidence for poorer recognition of negative
emotion was also provided (Uljarevic & Hamilton, 2012).
Behavior and Emotional Regulation
Behavior and emotional regulation involve effectively regulating one’s emotional state
and behavior while focusing attention on salient aspects of the environment and engaging in
social interaction. Typically developing children develop a range of strategies for self-regulation
(e.g., carrying a security blanket, playing with a preferred toy, retreating to one’s room when
overwhelmed). With the development of symbolic language, children begin to organize their
actions within an activity (e.g., first…then) and to prepare for upcoming activities during
transitions (Vygotsky, 1978). Language is used to request assistance or the need for breaks from
others. The ability to use language to express emotional states of self and others enables the

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 13
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
development of more advanced negotiation and or collaboration skills, leading to coping
strategies during interactions with peers (Prizant et al., 2003).
Children with ASD often continue to use early developing and idiosyncratic strategies for
self- regulation far beyond early childhood due to limited ability to benefit from models provided
by others. Immature patterns of behavior such as chewing on clothing, carrying/holding certain
objects, or rocking may be observed during situations causing mild emotional dysregulation.
Aggression, tantrums, or bolting from the social setting are examples of behavioral
strategies and emotional expressions that may be observed during periods of extreme emotional
dysregulation.
The compromised ability to benefit from models provided by others and reliance on early
developing strategies often result in the development of idiosyncratic language for self-
regulation (e.g., repetitively initiate a topic of special interest to cope with social anxiety; reciting
lines of a favorite movie or book when faced with stressful social circumstances; Rydell &
Prizant, 1995).
Restricted, Repetitive Behaviors, Interests, or Activities
Presence of restrictive and repetitive behaviors (RRBs), interests, and activities are a
defining characteristic of ASD. RRBs manifest in patterns specific to individuals. These
behaviors may include stereotyped and repetitive motor movements (e.g., hand flapping or lining
up items) or speech (e.g., echolalia). Individuals with ASD may demand sameness in their
routine, such as wearing the same clothing, taking the same daily route, or requiring activities to
be completed in the same order every time. RRBs can negatively affect individuals with ASD
when they interfere with the ability to engage in other activities or impact their relationships.
Those with ASD may experience anxiety when prevented from engaging in repetitive behaviors
or routines, which may result in problem behaviors such as emotional dysregulation, aggression
towards others or self-injurious behaviors. Evidence from research indicates that behavioral
interventions can decrease RRBs and improve coping (Kennedy Krieger Institute, n.d.).
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 14
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Data Collection for District Referral/RTI/MTSS Process

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 15
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Data Collection
The following data are considered essential to completing a comprehensive evaluation of
the student’s communication skills; however, the method in which the data are collected is
district specific and is therefore not included in this manual.
●
Parent data provides information on sociological factors, achievement of developmental
milestones, parent identified strengths and concerns for the student, information on
emotional/behavioral functioning, and functional skills.
●
Teacher data provides information on the educational impact of the student’s
communication difficulties as well as information related to the student’s performance
academically and behaviorally in the general education classroom as well as information
related to state/district assessments.
●
Health data provide information on recent hearing and vision screenings as well as any
other known health conditions.
●
Home language data provide information on the language(s) of the home and whether or
not the child is exposed to languages other than English.
●
Documentation of interventions provides information on the specific interventions
provided to the student and whether or not progress was made.
●
RTI/MTSS team deliberations provide information on the decisions made by the Student
Support Team as part of the Response to Intervention process.
Referral Considerations
If language, communication, or unusual behavior is indicated as a concern, the RTI/
MTSS members should review existing concerns with consideration of what may be atypical for
the student’s age/grade. See Appendix D Language Milestones to Consider.
1. For a non-identified student, teacher or parent brings learning and behavior concerns to
the Response to Intervention (RtI) Team/Multi-Tiered Systems of Support Team (MTSS). If
language, communication, or unusual behavior is indicated as a concern, the SLP along with
other Multidisciplinary team (MDT) members review existing data. Parent and teacher complete
information about the student to bring to the RTI/MTSS meeting, including vision and hearing
screening and Parent and Teacher Language Surveys. Please refer to the Guiding Questions form
(see Forms section) to assist the team in determining whether a referral is needed.
2. RTI/MTSS members discuss concerns of parent and teacher and
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 16
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
a. make recommendations for pre-referral intervention by teacher and parent,
OR
b. make a referral for autism evaluation if the student has an obvious disability and
the concerns expressed about the student are in the areas of social interaction,
communication, or unusual responses to the environment.
In the case of 2(a), the RTI/MTSS reconvenes after the recommended support and
intervention have been provided and determines from data collected if referral for a full and
individual evaluation is warranted or if interventions have been successful.
In the case of 2(b) or if classroom support and interventions have not been successful, the
RTI/MTSS makes a referral for a full and individual evaluation to address the areas of autism and
speech impairment.
3. In the case of a student already identified as having a disability but for whom ASD is
suspected in addition to the identified disability, the RTI/MTSS or the ARD Committee reviews
existing data including prior evaluations. Because autism includes qualitative impairment in
communication, the SLP participates in the review of existing data.
4. If a referral is initiated or additional evaluation is planned, the Guide to the Admission,
Review and Dismissal Process is given to parents along with Notice of Procedural Safeguards.
Notice and Consent for the Full and Individual Evaluation are provided and obtained.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 17
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Components of a Comprehensive Autism Evaluation
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 18
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Comprehensive Multidisciplinary Team Evaluations for
Autism Spectrum Disorder
IDEA 2004 requires the use of a multidisciplinary team (MDT) to determine eligibility
and to develop the IEP for students with disabilities. Required team members include “an
individual who can interpret the instructional implications of evaluation results …” and/or “other
individuals who have knowledge or special expertise regarding the child, including related
services personnel as appropriate” (CFR, 2006; 34CFR § 300.321; TAC, 2018; 19TAC §
89.1050 (c) (1)). For students with a suspected disability in the areas of autism spectrum
disorders or speech-language-communication disorders, this requirement is met with the
inclusion of an SLP on the multidisciplinary evaluation team.
Given the importance of social communication in the diagnosis of autism spectrum
disorder, as well as the complexity of the disorder, the SLP has an important role in the
interdisciplinary collaboration needed for evaluation, eligibility deliberation, planning, and
service delivery.
As the specialist in the area of social communication and communication disorders, the
SLP becomes an integral part of the MDT for:
● Defining the assessment question/s.
● Collecting data from multiple sources.
● Assessing communication competence, especially in the areas affected in ASD
○ Joint Attention
○ Reciprocal Social Interaction
○ Understanding and Using Verbal and Nonverbal Communication
○ Symbolic Play
○ Literacy Skills
○ Executive Functioning
○ Behavior and Emotional Regulation
● Determining the communication profile and social communication competence with a
variety of people and in a variety of contexts.
● Identifying the nature of the social communication disorder.
● Evaluating the impact of the communication disorder on academic achievement and
functional performance, if any.
● Developing an educational plan to address the student’s needs.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 19
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
SLPs have specialized training and are able to provide a thorough evaluation of students
with communication disorders. ASHA’s Scope and Practice in Speech Language Pathology
states, “SLPs are autonomous professionals who are the primary care providers of speech-
language pathology services. Speech-language pathology services are not prescribed or
supervised by another professional.” It is also stated, “Speech-language pathologists have
expertise in the differential diagnosis of disorders of communication and swallowing” (ASHA,
Scope of Practice, 2016).
In the school setting, the SLP is the most knowledgeable and highly skilled evaluation
team member to determine the presence of a speech impairment and make recommendations for
remediation and support. The SLP should be prepared to guide the ARD Committee in making
eligibility decisions.
Four Phases of the Language Evaluation
Components of a comprehensive language evaluation are outlined in the SI Disability
Determination Guidelines for Language Disorder. The SLP has an important role on the
multidisciplinary team addressing autism spectrum disorder and has the lead role in the disability
documentation of Speech Impairment with a language disorder. There are four phases in a
comprehensive evaluation of language.
Phase I – Assessment Plan
Review referral information and outside evaluations when available, collect information
from the parent and classroom teacher, and complete a criterion-referenced story retell task along
with a short conversational language sample. This information is used to determine language
areas of concern. Plan evaluation activities based on information gathered in Phase I.
Phase II – Data Collection
Administer criterion-referenced measures, language sample, checklists, questionnaires,
observations, and norm-referenced/standardized tests across school environments as outlined in
the Evaluation Plan.
Phase III – Analysis and Interpretation
Complete the Language Evaluation Summary Form and analyze results from Phase II –
Data Collection. Look for a pattern of performance that provides evidence of a language disorder
or no language disorder. Interpret results of tests and activities to answer these questions:
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 20
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
• Is there a language disorder?
• If so, is there an adverse effect on educational performance (academic achievement or
functional performance) resulting from the language disorder?
• When there is a documented language disorder with documentation of adverse effect on
educational performance, the conditions for disability determination have been met.
The final question to answer when giving recommendations to the ARD Committee
regarding eligibility for special education with a Speech Impairment is:
• Is specially designed instruction from the SLP needed to address the Speech Impairment
(disability condition)?
Phase IV – Evaluation Report
Complete a comprehensive Full Individual Evaluation report with results of formal and
informal tests/measures, description of the student’s language system, interpretation of results,
and clear description of disability determination. The Evaluation Report will include
recommendations to the ARD Committee about eligibility for services based on speech
impairment as well as recommendations about specially designed services from the SLP, or, if
there is no documented disability, recommendations to support the student based on referral
concerns.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 21
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Phase I of Evaluation:
Assessment Plan
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 22
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Assessment Planning Activities
The purpose of this phase of the language evaluation is to determine assessment
questions that will drive the selection of appropriate tools for further data collection. The
multidisciplinary team, with input from the SLP as a team member, will develop the assessment
plan to address autism spectrum disorders. The following planning activities may be useful for
the SLP when planning the language evaluation and can be summarized on the Assessment
Planning Worksheet.
Teacher Input
Teacher observations should be discussed and documented through the RTI/MTSS
process for concerns regarding autism. The Teacher Checklist: Initial Referral for Language
Concerns (see Forms Section) may provide useful information for planning the language portion
of the evaluation. If not completed during the RTI/MTSS process, have the teacher complete the
checklist during the Assessment Planning Phase, if needed.
Parent Input
Parent observations and concerns are documented on the Parent Information - Initial
Referral for Language Concerns form (see Forms Section) obtained by the teacher during the
referral process, or during the Assessment Planning Phase. This form may not be needed if the
parent has provided more complete information to plan the multidisciplinary team evaluation.
Other Significant Student Factors
If needed, summarize significant student factors on the Assessment Planning Worksheet
(see Forms Section):
• Excessive absences
• History of homelessness
• Instability at home
• Number of schools attended
• Discipline issues concerns or incidents.
• English Learner
• Recent Immigrant
• Poor academic progress in spite of intervention support.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 23
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Outside Reports
If any reports from an outside source regarding language are available, review and
include information you consider relevant on the Assessment Planning Worksheet.
Student Interaction
Meet with the child to complete a story retell screen and quick conversational language
sample. This should take no more than 10 minutes.
• Conversational language sample: Instructions and tips for obtaining a conversational
language sample during the assessment planning stage are included in the Forms Section.
• Narrative screen: The Story Retell Screener with instructions and scoring are included in
the Forms Section. This story retell task is scored as a criterion-referenced measure based
on developmental expectations for young children and grade-level expectations (Texas
Essential Knowledge and Skills) for school-age children. Select the Story Retell Screener
at the child’s grade level through fifth grade. Use the fifth-grade story for older students.
Complete the Assessment Planning Worksheet – Summary Section
Ask teacher for interventions provided and document response to intervention on
worksheet.
Assessment Questions
Autism Spectrum Disorder
1. The Multidisciplinary Team (MDT) examines the referral information collected by the
student support team/RTI/MTSS committee to determine the areas of concern. The MDT
considers the Guiding Questions to Assist in Determining Need for Referral found in the
Forms section of this manual. They can also develop additional assessment questions if
needed.
2. The MDT develops assessment questions that, when answered, provide sufficient
information about the student’s social communication and learning profile to deliberate
eligibility and guide instruction, intervention, and/or IEP decisions. MDT observations of
the student are advisable early in the process to help form these assessment questions.
3. The assessment questions determine which formal and informal tests and procedures are
selected for administration and by whom. When assessing for autism spectrum disorders,
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 24
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
the MDT poses questions about the deficit areas, and/or areas where the student seems to
be struggling to meet grade-level expectations. Practical and social adaptive skills
expected for age-level are also considered.
4. For three-year re-evaluations, the MDT uses the present levels of academic achievement
and functional performance as well as data about progress on IEP goals and information
from the student’s curriculum (general education and/or special education) to develop the
assessment questions.
5. For re-evaluations of students previously dismissed, the MDT should compare referral
data with information related to the previous dismissal from speech/language therapy.
The MDT must consider, on an individual basis, assessment questions for the student.
Language Disorder
Develop assessment questions based on the child’s weaknesses and areas of concern in
language form, content, and use in order to determine the tests and measures needed to fully
evaluate the child’s language system. Focused assessment activities allow the SLP to determine
if the child’s weaknesses and areas of concern are significant and interfere with the child’s
ability to be successful in school. The assessment questions guide the SLP’s selection of
assessments and evaluation activities to be administered. These include additional language
sampling, criterion referenced assessments, observations and norm-referenced tests or subtests.
Assessment Plan
Autism Spectrum Disorder
IDEA 2004 requires that the child is assessed in all areas related to the suspected
disability including, if appropriate CFR (2006; 34CFR §300.304 (c) (4)):
● Health
● Vision
● Hearing
● Social and Emotional
● General Intelligence
● Academic Performance
● Communicative Status
● Motor Abilities
The Assessment Plan allows the MDT to identify the areas that have been sufficiently
addressed with data in the referral information, and the areas that need further in-depth
assessment. The Assessment Planning Worksheet and Assessment Plan is then completed. MDT
members’ responsibilities are defined and a targeted completion date is given. The MDT should
allow time for analysis and interpretation of assessment data along with collaboration to
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 25
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
determine if the assessment data is comprehensive enough to determine eligibility and make
educational recommendations for the ARD Committee to consider. It is vital that the MDT
collaborate and communicate effectively during the evaluation process to produce a true, multi-
disciplinary evaluation.
The SLP’s role in planning the evaluation is to review the available information and
discuss the tests and subtests needed to address communication skills that may contribute to the
student’s struggle to meet grade-level expectations or make progress in their curriculum (general
education or special education). Consideration should also be given to planning assessment
activities that provide comprehensive information about the student’s communication profile and
adaptive functioning.
It is beneficial for the SLP to provide the MDT with examples of the student’s current
communication modes (e.g., nonverbal, Picture Exchange Communication System, pointing to
objects from a field of five). This will help determine if standardized tests are valid measures for
the student or if test(s) need to or can be modified.
Language Disorder
Compile information and develop the Assessment Plan (see Forms Section). When
evaluating a student’s language skills, complete a language sample, gather more specific teacher
and parent information if needed, observe the student across school environments when the
student is likely to use or attempt to use the language skills of concern, and administer norm-
referenced tests or subtests that provide information about the areas of concern identified in the
assessment planning phase of the evaluation.
When evaluating a student with possible ASD, the SLP should focus more on informal
measures than formal measures. Due to the social communication deficits of the student,
standardized scores typically do not yield complete information for describing or making
recommendations to improve the student’s communication skills. Formal testing may be used
for assessing the structure and form of language, but these evaluation tools may not
provide an accurate assessment of the student’s use of language. Standardized measures can
compensate and accommodate for social communication difficulties and provide extended
processing time not representative of real-life social situations (Ward & Jacobsen, 2014).
Determining the student’s social and communication competence necessitates evaluation across a
range of social settings using a variety of strategies for gathering information (ASHA, 2004).
Detailed information regarding various formal and informal assessment procedures is
included in the TSHA SI Disability Determination Guidelines for Language Disorder (2020).
Additional data collection tools are available in Forms Section of this manual.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 26
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Phase II of Language Evaluation:
Data Collection
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 27
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Step-By-Step for Disability Determination
1. The district’s MDT including an SLP, Psychologist (LSSP or Clinical Psychologist) and
diagnostician or other evaluation specialist trained in the assessment of autism complete the
autism evaluation. To prepare for the evaluation:
a. The MDT should observe the student in at least two different school environments,
preferably in one structured and one less structured context. The observations should be
completed in order to plan an individualized autism evaluation for the student (Phase I of
the Evaluation).
b. The MDT develops an Evaluation Plan for the student’s case (Phase I of the Evaluation).
c. The MDT completes the autism assessment using a variety of assessments and
procedures, including gathering information from parents and the teacher/s. Consider
collecting information from more than one teacher if the student presents differing
behavior in various environments (e.g., different teachers in rotations; PE teachers if the
student has more difficulty in less structured activities).
d. The SLP develops a plan of assessment for the student (Phase I of Evaluation) and
gathers assessment data as needed. Coordination between SLPs is needed when both the
campus SLP and a central Autism Assessment Team SLP are involved in the evaluation.
Each district may have its own strategy for SLP involvement in Autism evaluations.
Please refer to your district’s guidelines for planning in this area.
2. The MDT writes an integrated Full and Individual Evaluation (FIE) report that addresses all
areas of disability with recommendations for instruction. This includes:
a. Documentation of disability condition/s and recommendations to the ARD Committee
regarding eligibility conditions. Include information regarding the educational needs of
the student,
OR
b. Documentation that the conditions for disability determination are not met. When there is
lack of documentation of a disability condition, the ARD Committee documents that the
student does not meet eligibility for the disability condition. Include relevant information
that supports lack of documentation of the disorder and/or lack of documentation of
adverse effect on educational performance resulting from the disorder.
3. When a communication disorder is present, the SLP compiles documentation to address
whether there is an adverse effect on educational performance (i.e., academic achievement
and/or functional performance) resulting from the communication disorder. In this case, the
SLP should provide information to the ARD Committee about present levels of academic
achievement and functional performance (PLAAFP) related to communication, with
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 28
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
recommendations or suggestions for IEP goals and objectives in coordination with teachers
and other service providers.
4. The ARD meeting is scheduled to review the FIE to determine eligibility for special
education and related/supportive services.
5. If SI eligibility is determined, the SLP develops recommended service delivery plans,
including draft goals and objectives for ARD approval. Service delivery may be conducted
through:
a. Direct therapy services,
b. Indirect services and/or consultation,
c. A combination of these approaches.
6. If SI eligibility is not determined with direct services, the ARD Committee, with SLP input,
defines the indirect/consultation role of the SLP, if any.
7. If SI eligibility is not determined, the SLP may make recommendations for instructional
accommodations or modifications for the classroom teacher based on the evaluation data.
The communication related instructional recommendations should be incorporated in the
ARD/IEP.
Formal Assessment for Autism Spectrum Disorder
The following information should be gathered in a full and individual evaluation of
students at risk for ASD:
● Review of background information and referral concerns to complete the IEP; Parent/
caregiver interview to gather health, developmental, behavioral, and social
communication history of the child, and medical and mental health history of the family;
ASD is a retrospective diagnosis, and as such, the family information is a critical
component of differential diagnosis; and
● Parent interview to gather comprehensive information about current social
communication, functional communication, and speech and language skills; and
● Direct testing and diagnostic tools that confirm or rule out a diagnosis of ASD;
Direct/indirect testing and diagnostic tools that provide information about the student’s
social communication profile; and
● Direct behavior observation in multiple environments, with multiple communication
partners.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 29
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
A diagnostic evaluation to confirm or rule out ASD should be performed only by a
multidisciplinary team of professionals who have specific expertise in the evaluation and
treatment of autism (National Research Council, 2001). LSSPs and other team members may
also incorporate information from other rating scales and measures that may be helpful in
making final determinations. While this information may be considered, it should not serve as
the sole basis of information for identification of a pragmatic language impairment. The
following diagnostic tools for ASD have some published psychometric information including
evidence of reliability and validity:
● Autism Diagnostic Observation Schedule, Second Edition (ADOS-2; Lord et al., 2012)
The ADOS-2 is a semi-structured play and/or interview-based assessment that
includes activities designed to evaluate communication, reciprocal social interaction,
play, stereotypic behavior, restricted interests, and other abnormal behaviors in
individuals with ASD across the age range from preschool to adulthood. The ADOS-2
includes four test modules which have been developed for individuals with varying levels
of linguistic ability. Speech-Language Pathologists who have received formal training in
ADOS administration can administer this test as it is within their scope of practice.
● Autism Diagnostic Interview-Revised (ADI-R; Rutter et al., 2003)
The ADI-R is a standardized, semi-structured interview of 93 items for parents
that provides scores in three areas including quality of social interaction, communication
and language, and repetitive, restricted, and stereotyped interests and behaviors. It is used
for ages 2 and older.
● Childhood Autism Rating Scale, Second Edition (CARS-2; Schopler et al., 2010)
The CARS-2 is a 15-item rating scale completed by the clinician based on
observation of behaviors exhibited during other assessment activities and collected
parent/teacher information. It includes two protocols—high functioning (CARS2-HF)
and standard (CARS2-ST)—as well as an unscored Parent/Caregiver Questionnaire
(CARS2-QPC). Each of the 15 items uses a 4-point (with half steps) rating scale to
indicate the degree to which the child’s behavior deviates from age-appropriate norms. It
yields a standard score, percentile rank, and severity grouping. It is worth noting that the
CARS-2 was created with the framework of the DSM-IV (1994) definitions for Autism
and other related disorders, and also includes comparison tables to compare answer
profiles and scoring between students with different forms of Autism Spectrum Disorders
that are no longer recognized by the DSM-5 (2013).
● Gilliam Autism Rating Scale, Third Edition (GARS-3; Gilliam, 2013)
The GARS-3 is a rating scale consisting of 56 clearly stated items to be used by
parents, teachers, and professionals to help identify and estimate the severity of
symptoms of autism. Items are grouped into six areas including Restrictive/Repetitive
Behaviors, Social Interaction, Social Communication, Emotional Responses, Cognitive

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 30
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Style, and Maladaptive Speech. It yields standard scores, percentile ranks, severity levels,
and the probability of Autism.
● Monteiro Interview Guidelines for Diagnosing the Autism Spectrum, Second Edition
(MIGDAS-2; Monteiro & Stegall, 2018)
The MIGDAS-2 provides a way to organize a qualitative description of a
student’s language and communication, social relationships and emotional responses, and
sensory use and interests needed for diagnosing an autism spectrum disorder for toddlers,
children, adolescents, and adults. The MIGDAS-2 includes interviews and informal tasks
as well as suggestions for sensory-based toys and materials that must be purchased
separately. Two separate interview forms are available to use either for individuals with
limited to no verbal fluency or persons with verbal fluency.
● Parent Interview for Autism (PIA; Stone & Hogan, 1993)
The PIA is a structured interview designed to gather developmental information
and symptom severity information from parents of young children under age 6 years
suspected of having ASD. The PIA targets 11 areas including social behavior,
communication, repetitive activities, and sensory behaviors.
The measures most frequently used for the diagnosis of ASD in research protocols are the
ADI-R and the ADOS because of their strong psychometric features (Lord & Corsello, 2005).
In addition to formal measures specific to evaluation for Autism Spectrum Disorders, the
SLP should thoroughly investigate pragmatic language. It is important to consider that a single
pragmatic language test will not be appropriate to assess all students with social communication
concerns as these deficits exist on a continuum (Elleseff, 2015). Further information about
informal pragmatic language assessment can be found in the TSHA SI Disability Determination
Guidelines for Language Disorder, Phase II of Language Evaluation: Data Collection starting on
page 29.
Formal Assessment of Pragmatic Language
● Clinical Assessment of Pragmatics (CAPS, Lavi, 2019)
The CAPs is a video-based assessment of six subtests that provides information
on understanding and use of pragmatic language including nonverbal cues and overall
dynamics of social context in students ages 7:0 to 18:11. It yields scaled scores and
standard scores for three indexes.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 31
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
● Social Emotional Evaluation (SEE, Wiig, 2008)
The SEE includes five subtests to measure social language and higher-level
language needed to interact successfully in everyday social situations for students ages
6:0 to 12:11. It provides Z-scores.
● Social Language Development Test-Adolescent: Normative Update (SLDT-A:NU;
Bowers et al., 2017)
The SLDT-A:NU contains five subtests intended to measure a student’s ability to
make inferences and interpret and respond to social interactions in students ages 12:0 to
17:11. It provides standard scores and a Social Language Development Index.
● Social Language Development Test-Elementary: Normative Update (SLDT-E:NU
Bowers et al., 2016)
The SLDT-E:NU contains four subtests intended to measure language required to
appropriately infer and express what others are thinking and feeling, make multiple
interpretations, take mutual perspectives, and negotiate with/support their peers in
students ages 6:0 to 11:11. It provides standard scores and a composite Social Language
Development Index.
● Test of Narrative Language, Second Edition (TNL-2; Gillam & Pearson, 2017)
The TNL-2 measures the ability to understand and tell stories in children ages 4:0
to 15:11. It provides standard scores.
● Test of Pragmatic Language-2 (TOPL-2; Phelps-Teraski & Phelps-Gun, 2007)
The TOPL-2 includes six subtests intended to measure social skills and conflict
resolution for students ages 6:0 to 18:11. It provides standard scores.
Formal assessment related to pragmatic language: While not global assessments of pragmatic
language, aspects of these assessments provide information that could be useful in pragmatic
language assessment or be used for extension testing, if needed.
● Clinical Evaluation of Language Fundamentals, Fifth Edition-Metalinguistics (CELF-5
Metalinguistics; Wiig & Secord, 2014)
The CELF-5 Metalinguistics includes a metalinguistics profile that can be
completed by parents/teachers, two subtests in meta-pragmatics and two subtests in meta-
semantic skills. This assessment is for students aged 9:00 to 21:11 with subtle language
disorders or students identified with Autism that are lagging behind grade level peers. It
yields test and composite standard scores.
● Comprehensive Assessment of Spoken Language, Second Edition - (CASL-2; Carrow-
Woolfolk, 2017)
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 32
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
The CASL-2 Supralinguistic subtests include Non-literal language (ages 7-21),
Meaning from Context (7-21), Inference (3-21), and Double Meaning (9-21) that provide
a Supralinguistic Index in ages 7:0 and up. Additionally, the CASL-2 includes a
Pragmatic Language subtest for ages 3:0 and up. Each subtest yields a standard score.
● Test of Problem Solving Elementary-Third Edition Elementary: Normative Update
(TOPS-3E:NU; Bowers et al., 2018)
The TOPS-3E:NU is intended to measure how a student’s language skills impact
their ability to think, reason, problem solve, infer, classify, associate, predict, determine
cause, sequence, and understand directions in students 6:0 to 12:11 years. While not
primarily a test of pragmatic or social language skills, it yields information relevant to
pragmatic competence. It provides standard scores.
● Test of Problem Solving-2: Adolescent (TOPS-2:A; Bowers et al., 2007)
The TOPS-2:A is intended to measure five decision-making skill areas critical to
academic, problem-solving, and social success in students ages 12:0 to 17:11. While not
primarily a test of pragmatic or social language skills, it yields information relevant to
pragmatic competence. It provides standard scores.
When evaluating students with possible ASD, formal assessment procedures allow the
SLP to participate in the comprehensive multi-disciplinary team evaluation to confirm or rule out
the diagnosis of ASD, as well as to gather sufficient information to identify the student’s
communication profile and to describe the nature of their social communication skills. However,
the SLP should conduct informal measures in order to more fully describe the student’s present
levels of functional performance in the area of communication.
Indirect Formal Assessment of Pragmatic Language
These tools do not require direct elicitation of skills but are considered formal measures
as they provide standardized or scaled scores. They allow evaluators to gather data from sources
outside of direct contact with students in order to determine skills across settings but should not
be used solely to determine a disability.
● Children’s Communication Checklist (CCC-2; Bishop, 2006)
The CCC-2 is a parental questionnaire for ages 4:0 to 16:11 that includes 70
questions divided into 10 scales. Four of the scales are devoted to pragmatic aspects of
communication and two scales are specific to assess behaviors commonly impaired in
children with ASD.
● Clinical Evaluation of Language Fundamentals, Fifth Edition - Pragmatics Profile
(CELF-5; Wiig et al., 2013)
The CELF-5 - Pragmatics Profile is a subtest of the CELF-5 where information
provided to the SLP from parents and teachers is used to rate discrete social/pragmatic
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 33
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
language behaviors on a 1-4 Likert scale. It can be utilized for ages 5:0 to 21:11. It
provides a scaled score.
● Clinical Evaluation of Language Fundamentals - Preschool, Third Edition -
Descriptive Pragmatics Profile (CELF Preschool-3; Wiig et al., 2020)
The CELF Preschool-3 Descriptive Pragmatics Profile is a parental questionnaire
for ages 3:0 to 6:11 completed by a familiar adult that rates verbal and nonverbal
pragmatic skills necessary for expressing intentions and obtaining, responding to, and
giving information. It provides a scaled score.
● IMPACT Social Communication Rating Scale (IMPACT; Lavi, 2020)
The IMPACT is a norm-referenced pragmatic language rating scale of 35-40
questions to be completed digitally by parent, teacher, and clinician. It focuses on
pragmatic areas such as intent to socialize, nonverbal language, theory of mind, social
reasoning, and cognitive flexibility for ages 5:0 to 21:11. It provides standardized scores
and cut off scores.
● Language Use Inventory (LUI; O’Neill, 2009)
The LUI is a parental questionnaire for ages 1:6 to 3:11 that includes 180
questions divided into three areas including communication with gestures,
communication with words, and longer sentences. It has been recommended as an
evaluation for language acquisition in children with ASD (Tager-Flusberg et al., 2009).
● Pragmatic Language Skills Inventory (PLSI; Gilliam & Miller, 2006)
The PLSI is a 45-item rating scale for ages 5:0 to 12:11 that examines personal
interaction, social interaction, and classroom interaction skills that provides cut off scores
to indicate the need for further pragmatic language investigation. It utilizes cut off scores.
Criterion-Referenced and Informal Assessment
of Pragmatic Language
Informal data collection for students with possible ASD yields a qualitative description of
the student’s communication skills. Informal measures allow for an analysis of the student’s
communication strengths and challenges across communication environments and with a variety
of communication partners. Criterion-referenced measures can also be valuable in determining
how a student compares to same-aged peers.
Information about informal pragmatic language assessment can be found in the TSHA SI
Disability Determination Guidelines for Language Disorder, Phase II of Language Evaluation:
Data Collection starting on page 29.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 34
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Resources for informal measures of communication skills are included in the Forms
section of this manual:
● Parent/Teacher Communication Survey;
● Observation of Student Communication within School Environment;
● Observation of the School Environment to Facilitate Communication;
● Communicative Intent Checklist;
● Gestural Skills Checklist;
● Conversational Skills Checklist
● Play Based Skills Checklist
Informal data collection tools related to pragmatic language and social communication:
● Clinical Evaluation of Language Fundamentals, Fifth Edition (CELF-5; Wiig et al.,
2013)
The CELF-5 includes a Pragmatics Activities Checklist, which is a criterion
referenced measure that allows the evaluator to observe functional communication skills
during authentic, conversational interactions. It observes both verbal and non-verbal
communication skills.
● Clinical Evaluation of Language Fundamentals - Preschool, Third Edition (CELF
Preschool-3; Wiig et al., 2020)
The CELF Preschool-3 includes a Pragmatic Activities Checklist, which is a
criterion-referenced measure that allows the evaluator to observe functional
communication skills during authentic conversational interactions to identify verbal and
nonverbal behaviors that may negatively influence social and academic communication.
● Informal Social Thinking Dynamic Assessment Protocol, (ISTDAP; Winner, 2007)
The ISTDAP is a means of identifying and quantifying in real-time a student’s
social competencies and connecting student’s social learning abilities and related
academic strengths and challenges. The ISDTAP is not published as a diagnostic tool,
however, it can be valuable in determining areas of strength and challenge and degree of
impairment that will inform recommendations for intervention. The ISDTAP is
recommended for students aged 8 and older.
● Narrative Assessment
Analysis of narrative may reveal pragmatic deficits as it assesses the integration
of linguistic, cognitive, and social pragmatic abilities (Norbury, 2013). Elicitation of
narrative may occur with use of wordless picture books, immediate retelling of a story
just read with words occluded, or generation of a narrative given a prompt, stem, or
picture stimulus. Narrative assessment can be conducted with students preschool-aged
and older.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 35
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
● Natural Language Samples
Natural language samples collected in different communicative and social
contexts provide information about pragmatic skills that are difficult to measure using
other types of assessment. Natural Language Sampling should occur in a context that
aligns with the goals of assessment and should include adequate social presses. Ideally, a
sample of at least 30 minutes is collected for analysis (Tager-Flusberg et al., 2009).
● Observation
Observation is a useful assessment tool as it provides an opportunity to assess
difficult-to-test behaviors, validates information collected from formal testing sessions,
extends assessment activities to other settings, and can provide helpful information in
identifying the functional relationships between stimuli in the environment and a child’s
behavior. Some students with ASD perform within normal limits during formal testing,
even though they demonstrate functional communication deficits in other situations.
(Shipley & McAfee, 2008).
Observation in a variety of settings (e.g., structured and unstructured) provides an
opportunity to assess pragmatic language skills, both verbal and non-verbal, in real time,
applicable social and academic situations. Refer to the Forms section of this manual to
find observation forms that may be used in the classroom and in less structured
environments.
When writing about an observation, it is appropriate to include some
interpretation of what your observations mean in regards to the student’s strengths and
challenges in social communication. A brief narration of a student’s actions should be
supplemented with analysis that allows the reader to understand the underlying areas of
concern or strength that are impacting the student’s ability to interact with others in
various environments.
● Play-Based Assessment
Conducting a play-based assessment will allow the evaluator to observe the
student’s play skills, turn-taking and reciprocity in conversation and in games, as well as
providing opportunities to observe the student’s reactions to sabotage in play or
adjustment to another person’s verbal and nonverbal communication. This may be helpful
with younger students, as there are fewer standardized assessments that can be utilized in
this age range.
● SCERTS Assessment Process (SAP; Prizant et al., 2003)
The SAP is a criterion-referenced, curriculum-based tool that examines strengths
and weaknesses in social communication and emotional regulation. It provides
information across eight social-emotional growth indicators. The SAP is not a tool of
diagnosis, rather it is intended to be used to gather information for intervention and
educational planning.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 36
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Phase III of Evaluation:
Analysis and Interpretation

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 37
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Disability Determination
Autism Spectrum Disorder
The multidisciplinary team, including the SLP, conducts parent and teacher interviews,
formal and informal assessments and confirms or rules out ASD. The MDT provides
recommendations to the ARD Committee regarding eligibility for special education services
based on the presence of the disability and adverse effects on educational performance
(academic achievement and/or functional performance resulting from the disorder). The
disability and adverse effect of ASD is established with the following pattern and can be
documented utilizing the Adverse Effects on Educational Performance Chart within this section:
● Impairments in reciprocal social interaction;
● Impairments in verbal and nonverbal communication; AND
● Restricted, repetitive, and stereotyped patterns of behavior, interests, and activities.
The SLP may participate in a cross-battery analysis (XBA) in order to look at the
student’s cognitive abilities in Gc (Crystallized Intelligence) as related to overall cognitive
performance. Refer to the Language with Learning Disabilities Companion: TSHA SI Disability
Determination Guidelines for Language Disorder for more complete information on cross
battery analysis to aid in determining the presence of a language disorder.
Characteristics that overlap with other disability conditions (not exhaustive):
● Students who present with impairments in social communication, without evidence of
restricted, repetitive, and stereotyped patterns of behavior, interests, and activities should
be considered for Speech Impairment in the area of pragmatic language.
● Difficulty with social interactions is also observed in students with ADHD due to
impulsivity and disinhibition. Poor social interaction is also symptomatic in Emotional
Disturbance due to withdrawal from surroundings.
● Poor eye contact may be observed in students with ADHD who are hyperactive and/or
highly distractible and consequently they may not sustain attention or struggle to focus on
reciprocal social interactions. They may miss nonverbal social cues due to lack of
attention.
● Students with Emotional Disturbance also demonstrate difficulty establishing and
maintaining satisfactory interpersonal relationships with peers and teachers.
● Students with ADHD and Emotional Disturbance may have difficulty regulating their
emotions and communication to match the context due to executive functioning deficits,
limited self-control and sudden mood changes.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 38
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
● Anxiety and depression can be comorbid with Autism Spectrum Disorder. For example,
obsessive-compulsive behaviors, persistent irrational fears, low self-esteem, behavioral
outbursts, excessive dependence and poor personal boundaries may be observed in
students with either ASD or Emotional Disturbance. When these symptoms are observed,
the MDT should consider the presentation of the student as a whole and how these
characteristics manifest across all settings to assist with differentiating between eligibility
criteria.
These examples are not an exhaustive list, but highlight the importance of sharing
observations and data with your multidisciplinary team (particularly LSSP), so that a differential
diagnosis is considered. If the MDT suspects ADHD, documentation from a physician would be
required when recommending the eligibility code of Other Health Impairment, (Texas Education
Code, 34 CFR, § 300.8(c)(9)).
Autism with Intellectual Disability
The diagnostician/licensed specialist in school psychology and the MDT members
conduct formal and informal assessments and provide recommendations to the ARD Committee
regarding a possible intellectual disability co-occurring with ASD. An intellectual disability is
established when the answer is “yes” to the following two questions:
1. Does the student exhibit a significantly subaverage IQ: below 70 +/- the standard error
of measurement?
2. Does the student exhibit significant limitations in adaptive functioning in at least two
areas? (i.e., communication, self-care, home living, social/interpersonal skills, use of
community resources, self-direction, functional academic skills, work, leisure, health,
and safety)
However, when considering this identification in students with ASD, it is important for
the MDT to consider the overall specific areas of strength and challenges noted in the cognitive
profile for the student, as well as the impact of adaptive functioning deficits on the student.
Special Considerations for Autism in Girls
Symptomology of ASD is often notably different in girls. Differences in cultural
expectations for boys and girls impacts our perceptions of what is considered deviant behavior
(Shattuck, et al, 2009). Girls with ASD might appear more passive and better with social
communication skills, as in a stereotype of the “typical girl.” A girl’s passivity may not be
recognized as a social impairment at first glance, but may indicate deficits in social skills and
understanding of expectations of the group, as well as difficulty with expressing thoughts to
others. It is more socially acceptable for girls to be quiet and introverted or to be perceived as
shy, immature, or naive. Girls are generally more able to speak about their feelings and are less
prone to challenging behavior. Girls may not draw attention to themselves as boys with ASD are

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 39
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
likely to do, and may not cause disruptions in the classroom (Attwood, et al., 2006). Additional
research has corroborated these statements and also indicates that in instances when a girl
presents with no intellectual impairment or impacting behavior problem, identification is less
likely. Girls may be more difficult to recognize as they are more likely to have developed coping
mechanisms and strategies they can use to mirror the actions of others. Girls with ASD are often
identified later than their male counterparts, and the older they become, it is less likely
identification will occur.
The following are further differences in the presentation of ASD in girls:
● A preference for interactions with younger children (Kopp & Gillberg, 2011).
● The special or restricted interests of girls are more likely to be similar to those of any
other typically developing girl, and may be functional. (Attwood, 2006)
● May more often be “mothered” by other girls (Attwood, 2006).
● Repetitive or restrictive pretend play (e.g., may arrange their dolls in a particular, never
changing way and is unlikely to share them) (Attwood, 2006)
● Less obvious self-stimulation behavior, as the girl may have replaced her natural self-
stimulation with something more socially acceptable.
● Exhaustion after social stimulation (school, playgroups) (Attwood, 1998)
● “Jekyll & Hyde” behavior—following rules at school and being the “ideal student,” then
coming home and melting down in a “4 o’clock explosion” (Attwood, 1998)
SLPs should continue to use evidence-based practices and monitor current peer-reviewed
research in this area. Currently, international research is focused on the development of gender-
specific autism assessment tools to improve the early identification of ASDs.
Special Considerations for Autism in Gifted Students
A gifted/talented student is a child or youth who performs at or shows the potential for
performing at a remarkably high level of accomplishment when compared to others of the same
age, experience, or environment and who exhibits high performance capability in an intellectual,
creative, or artistic area; possesses an unusual capacity for leadership; or excels in a specific
academic field (Texas Education Code § 29.121).
Gifted students with a disability such as ASD or ADHD are referred to as twice-
exceptional children. While twice-exceptional students tend to be in the minority, accurately
identifying these students can pose a significant challenge in part due to the overlap of
characteristics of higher functioning ASDs and typical giftedness.
Gifted students, especially those that are in a classroom environment that do not meet
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 40
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
their educational needs, may demonstrate behaviors that are more likely to be viewed as different
or disruptive to their own or others’ learning. Amend et al. (2008) have developed a pre-referral
tool that organizes data in order to help develop appropriate interventions and aid in decision
making regarding referral for evaluation.
When evaluating for autism in students identified as gifted, careful consideration should
be given to the impact giftedness may have on memory and attention, speech and language (e.g.,
extensive and advanced vocabulary), social interactions, emotional regulation, and topics of
interest. As a part of the multidisciplinary team, the SLP can provide valuable information
regarding the subtle differences between speech and language comprehension and use between
students with ASD and those who are gifted, or those who are twice-exceptional.
Cultural and Linguistic Differences
Culture and cultural diversity can incorporate a variety of factors, including but not
limited to age, disability, ethnicity, gender identity (encompasses gender expression),
national origin (encompasses related aspects e.g., ancestry, culture, language, dialect,
citizenship, and immigration status), race, religion, sex, sexual orientation, and veteran
status. Linguistic diversity can accompany cultural diversity. (Keller-Bell, 2017)
The evaluating speech-language pathologist should consider how differences in cultural
expectations may influence a student’s presentation of pragmatic language abilities as well as
parent report of abilities across settings. Possible areas of difference may include: eye contact,
frequency of initiation, length of conversational turn, proximity, volume, body language, gesture
use, deference, tone of voice, facial expressions, etc. (Please note, this is not an exhaustive list)
Speech Impairment for Pragmatic Language without Autism
When data supports ONLY deficits in social communication, with NO current or historic
observation of restricted, repetitive patterns of behavior, interests, or activities, a code of Autism
would not be recommended. Students should continue to be considered for the code of Speech
Impairment in the area of pragmatic language using the staged eligibility process.
Pragmatic language concerns can arise outside of and without identification of Autism.
The DSM-5 (2013) has characterized a Social Communication Disorder, where pragmatic
language concerns present in the absence of repetitive and restrictive behaviors. Pragmatic
language concerns can also arise from other disability conditions as described above (e.g.,
Emotional Disturbance, ADHD, Intellectual Disability).
When significant deficits are noted in one or more of the areas of pragmatic language,
i.e., communicative intent, conversation, narrative, presupposition, and social register; the
evaluator should consider the impact of these areas of weakness and whether other factors may
be involved. For instance, for a student with deficits in only narrative skills, expressive and
receptive language skills should be considered in relation to these skills to determine how best to
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 41
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
characterize the cause of the deficit. For students with challenges with social register,
considering whether impulsiveness or attention difficulties are impeding the students’ ability to
control their statements, rather than a difficulty with understanding the different expectations for
social communication with different communication partners and in different settings.
Pragmatic language deficits should be addressed through a variety of service delivery
models provided either directly or indirectly by the SLP, with consideration of the natural
environment for the location of services, when an educational need is supported and specialized
instruction from a Speech Language Pathologist/Assistant is required (see next sections for Stage
II: Adverse Effects on Educational Performance and Stage III: Need for specially designed
instruction from an SLP/SLP-A).
Speech Impairment with Language Disorder
Use the Language Evaluation Summary Form (see Forms Section) to summarize data
collected during Language Evaluation – Phase II. Look for strengths and deficits in language
form, content, and use across the language modalities of listening, speaking, reading, and
writing.
Review the assessment questions developed based on the referral concerns and
information gathered from the parent, teachers, and student during the autism evaluation. Make
sure that sufficient data has been collected from a variety of sources to answer the questions.
Disability determination for Speech Impairment includes both the documentation of a
communication disorder and documentation of an adverse effect on educational performance
resulting from the communication disorder. When referral concerns include the student’s
language learning system, the questions that need to be answered are:
Stage I: Is there documentation of a language disorder?
Stage II: If so, is there evidence of an adverse effect on educational performance resulting
from the language disorder?
If the answer to both Stage I and Stage II questions is “yes,” a disability condition is
present.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 42
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage I: Evidence of a Language Disorder
Evidence of Language Disorder Yes No
Is there evidence of a language disorder based on test manual specifications from
a standardized language test?
Is there evidence of a language disorder based on analysis of a language sample?
Is there evidence of a language disorder based on analysis of other informal
criterion-referenced assessment measures?
Is the teacher concerned about the student’s use of language for academic
purposes?
Is the parent concerned about the student’s language and literacy achievement?
Is the student stimulable for expanded language use?
Does the professional judgment of the SLP support a concern?
Does the student lack confidence for language and learning tasks?
Total
Scoring: If the answer to at least four of the above questions is “yes,” it is likely that the student
presents with a language disorder.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 43
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage II: Adverse Effect on Educational Performance
Academic Achievement Yes No
There is a direct, noticeable relationship between the student’s communication
disorder and academic performance or achievement
The student’s communication disorder contributes to academic struggle or below
expected achievement on the IEP
The student’s communication disorder is out of proportion with overall
functioning level
Data indicates that the student’s performance in the academic curriculum will
require specially designed instruction from the SLP
The student with other disabilities needs speech-language therapy to benefit from
the special education program
Functional Performance Yes No
Communication skills limit participation in self-care, interpersonal, and daily
routines
Communication patterns disrupt and interfere with interaction and functional
performance
Social communication skills disrupt effective interpersonal interaction
Communication disorder is pervasive and noticeable across settings and interferes
with interaction
The student has no functional communication, limited means of expression, or
social/emotional adjustment is affected by the communication disorder
Total
Scoring: If the answer to at least three of the above questions is “yes,” it is likely that the
student’s language disorder results in an adverse effect on educational performance.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 44
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Sources of Documentation for Adverse Effect:
Grades Teacher/Parent Information
State, District, Local Assessments/Tests Student Self-Report
Student Work Other
Observation
Recommendations to Admission, Review, Dismissal Committee
When the student exhibits a language disorder that has been documented with informal
measures, and formal measures when appropriate, and there is evidence of an adverse effect on
educational performance resulting from the language disorder, the disability condition has been
established. The SLP’s recommendation to the ARD committee is for consideration of eligibility
for special education services on the basis of Speech Impairment.
When the ARD committee establishes Speech Impairment as an eligibility condition, the
Stage III question is addressed:
Stage III: Are specially designed SLP services needed for the student to make progress in
the curriculum?
Use the Language Evaluation Summary Form to document recommendations regarding
the need for specially designed SLP services that will support the student with a language
disorder (Speech Impairment).
The services of a speech-language pathologist should be considered to support the core
speech and language challenges observed in students with ASD, including (but not limited to):
● Phonology
● Fluency
● Voice
● Semantics
● Syntax
● Pragmatics
○ Joint attention
○ Communicative intent (forms of communication)
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 45
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
○ Conversation (Initiation, turn-taking, overlap, “sharing the floor”, topic maintenance,
repair, social register, etc.)
○ Presupposition
○ Narrative (personal, fictional, expository)
○ Understanding and use of nonverbal communication
○ Understanding and use of nonliteral language
○ Metalinguistics
When recommending whether support should be provided through social skills
instruction from Special Education staff other than the SLP, or if specially designed instruction is
required from a speech-language pathologist/assistant, the evaluators should determine the
underlying deficit. When language is the primary deficit affecting a skill, specially designed
instruction from the SLP should be considered. For example, if a student has difficulty with
emotional regulation, SLP support would be indicated when a student needs support acquiring
the language to request a soothing activity, break or assistance or being able to express their
emotional state. Choosing and using calming strategies in a variety of settings, in contrast, could
be supported by other instructional personnel.
Definition and separation of social skills from pragmatic language is a nebulous area
(Elleseff, 2015). Identifying and quantifying a student’s deficits in social interactions to
determine if specially designed instruction from an SLP are necessary to remediate social
difficulties can be challenging, especially in consideration of the multitude of variables that
influence overall social success aside from pragmatic language skills. While many resources may
use the terms “social skills” and “pragmatic language” interchangeably, ASHA provides some
clarification regarding the role of the SLP in remediation of social communication difficulties.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 46
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Phase IV of Evaluation:
Evaluation Report
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 47
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Report Writing Considerations
The evaluation report should provide a comprehensive picture of the child, with
information about the referral concern for autism spectrum disorder and also related to language
skills. In addition to charts and/or tables documenting language assessment results, a narrative
section should be included to adequately analyze the results of the assessment in the areas of the
qualitative impairment that is a component of autism spectrum disorder, in addition to language
form, content, and use. The narrative section should contain student specific information rather
than lengthy test descriptions followed by a score.
Sample Wording in Full Individual Evaluation Report
The FIE should contain a Summary/Conclusion section and a Recommendation section.
In the Summary/Conclusion section the MDT explains the conclusions regarding each of the
areas of disability, including Autism/ASD and Speech Impairment. If the MDT is also
considering an Intellectual Disability, the Speech Impairment conclusion must consider the
language skills in relation to intellectual abilities.
Example for Autism & Speech Impairment:
Summary/Conclusion
Autism. (The MDT defines the assessment results to determine autism.)
Speech/Language. As part of >>>>>’s evaluation, a qualified professional considered
existing evaluation data, information provided by the teacher and parent/s, and observations to
determine the presence or absence of a communication disorder which may be contributing to the
educational need. According to the speech impairment eligibility criteria and the federal
definition of speech-language impairment, a student must meet two prongs of eligibility in order
to be identified with speech impairment. The following are the two criteria stages and the
determination based on the evaluation results:
Stage I: Is there a communication disorder? (Answer the question and explain results.)
Stage II: Is there an adverse effect on educational performance (academic achievement or
functional performance) resulting from the communication disorder? (Answer the
question and explain results.)
The answer to both of these questions must be yes in order to make an eligibility
recommendation for Speech Impairment.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 48
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
• Based on test results and student data from a variety of sources, >>>>> meets/does not
meet eligibility criteria as a student with speech impairment.
• Based on the assessment data, the student’s language/communication skills indicate that
>>>.
It is the professional judgment of the speech-language pathologist/multidisciplinary team
that the student does/does not exhibit a communication disorder. Therefore, there are/are no
language/communication factors that directly affect the student’s ability to make progress in the
educational programming.
It is the responsibility of the ARD Committee to determine eligibility and educational
need for special education and related/supportive services.
Recommendations
This section includes recommendations that address all areas of concern. In regard to
speech-language, the recommendations in the FIE include an answer to the Stage III question for
SI:
Since the student meets the eligibility criteria for Speech Impairment, the third question is
addressed in order to make recommendations to the ARD Committee.
Stage III: Are specially designed services by a speech-language pathologist/assistant
needed in order for the student to benefit from a special education program?
Give specific examples of the recommended service delivery model/s and instructional
recommendations for the student.
Sample Wording for Does Not Qualify (DNQ) SI. One of the most challenging cases is
when the student meets criteria for Autism but does not meet criteria for SI. The following is an
example of some wording to consider as you think through the evaluation data.
Stage I – Is there a communication disorder?
Based on the formal assessment data, >>>>>’s language skills are within the average
range of functioning (give examples of strengths). During conversational or less
structured portions of the evaluation, >>>>> exhibited some deficits in the area of
social communication (give specific examples). The difficulties noted in the area of social
communication align with one of the core features of Autism and indicate a
communication disorder.
Stage II – Is there an adverse effect on educational performance in the current
curricular/classroom setting resulting from the communication disorder (academic
achievement and/or functional performance)?
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 49
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
While >>>>>’s social communication skills are mildly disordered, >>>>>'s overall
communication skills are considered functional. Any social communication difficulties
should be addressed within the context of the situation and/or curriculum by the
educational staff.
Based on test results and student data from a variety of sources, >>>>> does not meet
eligibility criteria as a student with speech impairment.
It is the responsibility of the ARD Committee to determine eligibility and educational
need for special education and related/supportive services.
Thoughts Regarding Autism, Intellectual Disability, and Speech Impairment
When considering Autism, Intellectual Disability, and Speech Impairment, the MDT
considers the student’s language and communication skills in relation to cognitive skills and
adaptive skills as well as ASD. The presence of a communication disorder will be evident.
Careful consideration of the functional and academic implications of the communication disorder
is important
Sample Intervention Goals Based on Core Challenges
in Autism Spectrum Disorder
The ASHA website has provided a link to Sample Intervention Goals Based on Core
Challenges in Autism Spectrum Disorder on the Practice Portal for Clinical Topics in Autism.
These sample goals address underlying language challenges observed in individuals with ASD.
For many students that have been identified with Autism in the school setting, there may
come a time when the student no longer presents with an educational need for specialized
instruction from a speech language pathologist. This may occur after years of intervention, or
after a short period of intervention, depending on that specific student’s progress and areas of
deficit.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 50
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Re-Evaluation
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 51
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Re-Evaluation Considerations
A re-evaluation must occur at least once every three years, unless the parent and the
school district agree that a re-evaluation is unnecessary after conducting a Review of Existing
Evaluation Data (REED; CFR, 2006; 34 CFR § 300.303). The school district must ensure that a
re-evaluation is conducted when the student’s needs warrant a re-evaluation, when the student’s
parents or teachers request a re-evaluation, or when the ARD committee is considering exiting
the student from special education services.
See the Disability Determination Guidelines for
Speech Impairment and follow district procedures for re-evaluation of students coded with
Speech Impairment.
Language re-evaluation processes and procedures mirror initial evaluation processes and
procedures with the added consideration of careful review of progress in therapy and analysis of
strengths and weaknesses in the student’s language learning system relative to the curriculum.
Refer to Phases I-IV of Evaluation.
One of the considerations during re-evaluation should be a need for continued services
based on educational need and need for specially designed instruction and whether dismissal
from special education is appropriate.
The Re-evaluation Disability Documentation Worksheet: Autism Spectrum Disorder may
be utilized to reconcile data between parent, teacher, and clinician observations. This worksheet
includes dismissal considerations.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 52
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Dismissal
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 53
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Dismissal Considerations
The goal of public-school speech-language pathology services is to remediate or improve
a student’s communication disorder such that it does not interfere with or deter academic
achievement and functional performance. The first step in the dismissal process should occur
when the student is first determined to be eligible for services through an IEP. There are three
goals of speech-language pathology services in schools:
● to determine if the student’s communication disorder is adversely affecting academic
achievement and functional performance;
● to provide intervention for those communication disorders that are adversely affecting
academic achievement and functional performance, specifying goals leading to specific
criteria for dismissal;
● to dismiss the student from speech-language pathology services once the criteria for
eligibility are no longer met (ASHA, Eligibility and Dismissal, n.d.).
ASHA’s Code of Ethics Principle of Ethics I, Rules K and L state:
● Individuals who hold the Certificate of Clinical Competence shall evaluate the
effectiveness of services provided, technology employed, and products dispensed, and
they shall provide services or dispense products only when benefit can reasonably be
expected.
● Individuals may make a reasonable statement of prognosis, but they shall not guarantee—
directly or by implication—the results of any treatment or procedure (ASHA, Code of
Ethics, 2016).
These rules should be taken into account when contemplating the initiation or
continuation of interventions.
A student may be considered for dismissal from speech-language therapy/IEP services,
based on a re-evaluation, when one or more of the following conditions exist:
● Based on re-evaluation (formal or informal) and therapy data, the student no longer
meets the district eligibility criteria for Speech-Language Impairment (document in
Eligibility Stage I and Stage II).
● The student’s speech/language/communication needs are being addressed through special
education services or by other service providers without the need of the SLP (document
in Eligibility Stage II as “no adverse effect on educational performance resulting from the
communication disorder”).
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 54
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
● The student’s speech/language/communication skills are commensurate with the level
of overall functioning, especially in adaptive skills and social communication skills
which allow for effective interpersonal communication (document in Eligibility Stages
I or II).
● The goals and objectives of treatment have been met and the educational need for
services has been mitigated (document in IEP).
● The student's communication abilities are comparable to those of the same chronological
age, gender, ethnicity, intellectual level, or cultural and linguistic background (document
in Eligibility Stage I).
● The student who uses an augmentative or alternative communication system has achieved
functional communication across environments and communication partners (document
in Eligibility Stage II).
Additional conditions may include:
● The student is unable to tolerate treatment because of a serious medical, psychological, or
other conditions. *
● The student demonstrates behavior that interferes with improvement or participation in
treatment (e.g., noncompliance, malingering), providing that efforts to address the
interfering behavior have been unsuccessful. *
● Speech-language therapy no longer affects change in the student’s communication skills.
There does not appear to be any reasonable prognosis for improvement with continued
treatment. *
* When using these as a basis for dismissal, the campus SLP should work with the MDT to
document minimal educational benefit from speech-language therapy services. The ARD
committee and MDT should review the Factors to Consider in Dismissal from Speech and
Language Therapy Services located in the Re-evaluation Eligibility Worksheet and document
their justification based on all applicable criteria (Arkansas Department of Education [ADOE],
Eligibility Criteria, n.d.).
For additional information regarding dismissal considerations, see the TSHA SI Disability
Determination Guidelines for Language Disorder.
Each program should have established policies and procedures for following the
individual after discharge. Follow-up is necessary because an individual’s circumstances may
change, new treatments may become available, or the individual may respond differently due to
maturational changes or new life transitions (ASHA, Decision Making in Termination of
Services, n.d.). If speech/language therapy services are discontinued, a student can be re-referred
at a later date until successful completion of an educational program or until reaching the age of
21. If a student is re-referred, the referral committee should compare the reason(s) for referral
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 55
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
with information on the previous termination of speech/language therapy services in order to
determine on an individual basis the appropriate course of action to be taken. This may result in
revaluation, a reinstatement of services, or a decision that no further consideration for services is
necessary (ADOE, Eligibility Criteria, n.d.).
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 56
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Forms

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 57
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Guiding Questions to Assist in Determining Need for Referral
Student:
Date Completed:
Individuals participating in questionnaire:
Parent:
Teacher:
Other:
1. Has the individual experienced any loss of previously acquired speech, babbling or social
skills? If so, is there any known cause (e.g., trauma, head injury)? Please explain:
2. Has the individual experienced any delay in language development? If so, what did previous
language testing indicate (receptive, expressive, pragmatic delay) and what was the outcome of
intervention?
3. Does the person avoid eye contact (take into account differences in cultural norms)? If so,
please describe:
4. Does the individual show a persistent preference for solitude? If so, what are some known
factors that could be contributing to this?
5. Does the individual demonstrate difficulty understanding the feelings of others? For older
children or adults, is it difficult for the person to understand when they are being teased or the
meaning of non-literal information including jokes? Does the older child, adolescent, or adult,
have difficulty considering the perspective of others? If so, please explain:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 58
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
6. Does the person exhibit persistent repetition of words or phrases (echolalia), or manner of
speaking that may be considered unusual for the individual’s age (e.g., a child who uses a more
advanced or formal style than others their age; a child who repeats learned phrases or scripts)?
Does the person show demonstrate any differences in the quality of their speech? For example,
do they speak in a monotone, or use a higher pitch? If so, please explain:
7. Does the person show resistance to minor changes to the environment or surroundings? How
does the individual respond to changes in their routine or to unexpected events? Does the person
show an insistence for things to happen just as expected? Please explain:
8. Does the individual have restricted interests, for example, an intense focus on certain topics?
For a younger child, are they only interested in playing with particular toys rather than showing
interest in a variety of toys or activities? For an older child or individual, this may be more
observable in topics discussed in conversation. The individual may frequently refer to the topic
in writing prompts or conversation when other conversational partners or audience are less
interested in the topic.
9. Does the individual exhibit any repetitive motor movements such as rocking, flapping,
spinning? If not currently, did the individual exhibit any such behaviors at a younger age? If so,
please describe:
10. Does the person show or have a history of displaying unusual and intense reactions to
sounds, smells, tastes, textures, lights and/or colors? If so, please explain:
Other questions to consider may include:
Does the individual show an interest in friendships and tries to interact with others, but struggles
with unwritten rules (e.g., knowing when to stop talking about a subject, knowing how to add
more comments in conversation)? Please explain:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 59
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Does the individual have difficulty with executive functioning such as planning and executing
tasks? Please describe:
Adapted from: Autism Speaks (n.d.). Learn the Signs. Available at
https://www.autismspeaks.org/learn-signs
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 60
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Evaluation Phase I: Assessment Plan
Assessment Planning Worksheet
RTI/MTSS Pre-Referral Intervention
Assessment Plan

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 61
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Assessment Planning Worksheet
Student: DOB: Date:
School: SLP:
Teacher: Grade:
Referral Concerns
Significant Student Factors No
Concern
Some
Concern
Significant
Concern
Attendance
Comments:
Discipline Incidents
Comments:
Instability at Home
Comments:
History of Homelessness
Comments:
Number of Schools Attended
Comments:
English Learner
Comments:
Recent Immigrant
Comments:
Poor Academic Progress in spite of intervention support
Comments:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 62
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Area Significant Information Obtained Completed
Teacher Input
Parent Input
Outside Reports
Story Retell Screener
Conversational Language
Sample – Low Structure
Other

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 63
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
RTI/MTSS Pre-Referral Intervention
Response to Intervention
Tier I Classroom Support
Tier II / Tier III Interventions
Phase I Summary: Strengths and Weaknesses
AREA DATA
Data Support
Concern?
YES NO
Morphology/Syntax
Semantics
Phonology – articulation of
speech sounds
Phonology –reading readiness/
understanding letter-sound
relationships
Pragmatics
Memory
Auditory processing
Social communication
Attention
Can communicate idea/ get point
across
Adult needs to ask questions to
clarify meaning
Other
Is diagnostician needed for additional evaluation? (IQ, adaptive, literacy,
achievement)
YES NO

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 64
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Assessment Plan
Assessment Questions:
Assessment Question Addressed Language Areas Assessed
Language Sample
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Teacher Information
In-depth probes
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Parent Information
In-depth probes
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Informal Criterion
Referenced Measures
Checklists, Interviews
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Norm-Referenced
Tests/Subtests
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Observation Across
School Environments
– Academic and
Nonacademic
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
Other:
__________________
__________________
__________________
__________________
Syntax & Morphology
Semantics
Pragmatics
Metalinguistics
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 65
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Evaluation Phase II: Data Collection Forms
Parent Teacher Communication Survey
Encuesta de Communicaciόn Entre Padres/Maestros
Observation of Student Communication within the School Environment
Observation of the School Environment to Facilitate Communication
Play Based Skills Assessment
Communicative Intent Checklist
Gestural Skills Checklist
Conversational Skills Checklist

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 66
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Parent/Teacher Communication Survey
Student:
Date Completed:
Informant:
Relationship:
Parent/ Teacher/ Other:
1. With whom does the student interact on a regular basis?
2. Where does the student go on a regular basis? (sports events, meetings, etc.)
3. What strategies are most helpful to encourage the student to communicate? (e.g., standing
close, pairing language & written cues, allowing frequent breaks)
4. List the student’s communication strengths:
5. List the student’s communication weaknesses:
6. Please check the student’s most frequent method of communication.
Oral Speech
Communication System:
____________________
Pictures
Signs
Gestures
7. Please check all the reasons the student communicates.
Request desired item or activity
Request help
Protest/refuse an undesired item or activity
Greet/ say good-bye
Request permission
Express empathy
Comment on immediate and past events
Request information regarding immediate and past events
Express feelings and opinions

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 67
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Please choose one:
Usually Rarely
1. Does the student consistently attempt to interact with others?
2. Is the student’s communication purpose easily understood
3. Does the student notice when his/her communication is being
misunderstood? If so, check the student’s most frequent responses to
being misunderstood:
Attempts to clarify/repeats
Becomes upset/frustrated
Gives up
Other:______________________
4. Does the student use and understand a variety of types of words?
(See the list below for examples of “types of words”)
Please indicate word types that the student is observed to understand and/or use:
Understands
Uses
Y N Y N Wh-words (e.g., what, where, who)
Y N Y N Words describing time (e.g., before, now, later)
Y N Y N Words describing size or number (e.g., small, many)
Y N Y N Words describing location (e.g., beside, between)
Y N Y N Pronouns (e.g., I/you, he/she, we/they)
Y N Y N Verbs (e.g., past, present, future tense)
Y N Y N Conjunctions that link (e.g., and, or)
Y N Y N Conjunctions that imply cause (e.g., but, so, because, if)
Y N Uses grammatically correct sentences

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 68
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Does the student: Usually Rarely
5. Initiate topics frequently?
6. Introduce a variety of topics?
7. Talk about things that are of interest to others?
8. Understand the meaning of what is said in conversation?
9. Talk turns as a speaker and listener?
10. Adjust conversation based on audience? (e.g., talking to a teacher
vs. talking to a peer)
11. Request relevant information?
12. Adjust length of turn based on partner’s behavior?
13. Shift topics smoothly?
14. End conversations politely?
15. Use and understand communication behaviors? (see the following
list)
Does the student: Usually Rarely
16. Adapt readily in new group situations
17. Express distress or boredom similar to peers of ability level?
18. Respond to feedback and guidance offered by others about
regulating emotion?
19. Speak fluently without repetitions or hesitations (stuttering)?
20. Use vocal quality that is consistent with age and gender? (e.g.,
hoarseness, harshness, breathiness, and pitch)
21. Recall words associated with specific situations or nouns? (e.g.,
salt and pepper, baseball and bat, bread and butter, garage and car)
22. Understand and use antonyms and synonyms?
23. Discuss the meaning of words/define words?
24. Understand more than one meaning for words? (e.g., bat, park,
foot)
25. Put ideas into words and explain ideas?
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 69
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
26. Understand subtleties in word and sentence meaning? (e.g.,
idioms, figurative language)
27. Distinguish fiction from non-fiction, including fact and fantasy?
28. Retell messages by summarizing or clarifying?
29. Use and understand negation? (e.g., I will go to the movies if it is
not too late.)
30. Generate ideas before telling a story?
31. Use suitable story structure?
32. Use story grammar?
33. Is the student’s speech easy to understand in conversation?
If the student is difficulty to understand, note the problem sounds
here:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 70
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Encuesta de Comunicaciόn Entre Padres/Maestros
El estudiante:
Fecha completada:
El informante:
Relación:
Padre / Maestro / Otro:
1. ¿Con quién interactúa el estudiante de forma regular?
2. ¿Dónde va el estudiante regularmente? (eventos deportivos, reuniones, etc.)
3. ¿Qué estrategias son más útiles para alentar al estudiante a comunicarse? (por ej., de pie
cerca, emparejó el lenguaje y las señales escritas, permitiendo descansos frecuentemente)
4. Enumere las fortalezas de comunicación del estudiante:
5. Enumere las debilidades de comunicación del estudiante:
6. Por favor, marca el método de comunicación más frecuente del estudiante.
Lenguaje oral
Sistema de comunicación:
____________
Dibujos
Señas
Gestos
8. Please check all the reasons the student communicates.
Solicitar el objeto o la actividad deseados
Solicitar ayuda
Protestar/rechazar un objeto o actividad no deseada
Saluda/digan adios
Solicitar permiso
Expresar empatía
Comentar sobre los eventos inmediatos y pasados
Solicitar información sobre eventos inmediatos y pasados
Expresar sentimientos y opiniones

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 71
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Por favor elija uno:
Usualmente
Raramente
1. ¿El estudiante constantemente intenta interactuar con otros?
2. ¿Se entiende fácilmente el propósito de comunicación del
estudiante?
3. ¿El estudiante se da cuenta cuando su comunicación está
siendo malentendida? Si es así, marca las respuestas más
frecuentes del estudiante a ser mal entendido:
Intenta aclarar/repetir
Se vuelve molesto/frustrado
Rendirse
Otro:__________
4. ¿El estudiante usa y entiende una variedad de tipos de
palabras? (Consulte la lista siguiente para ver ejemplos de
"tipos de palabras")
Por favor, indique los tipos de palabras que el estudiante observa para entender y/o
utilizar:
Entiende
Usa
Sí No
Sí No
Las palabras de pregunta (por ej., qué, dónde, quién)
Sí No
Sí No
Las palabras que describen el tiempo (por ej.,
antes, ahora, más tarde)
Sí No
Sí No
Las palabras que describen el tamaño o el número (por ej., pequeño, muchos)
Sí No
Sí No
Las palabras que describen el lugar (por ej., al lado, entre)
Sí No
Sí No
Pronombres (por ej., yo/tú, él/ella, nosotros/ellos)
Sí No
Sí No
Verbos (por ej., el pretérito, el presente, el futuro)
Sí No
Sí No
Conjunciones que conectan (p. ej., y, o)
Sí No
Sí No
Conjunciones que implican la causa (por ej., pero, por lo tanto, porque, si)
Sí No
Utiliza oraciones gramaticalmente correctas

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 72
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
¿El estudiante:
Usualmente
Raramente
5. ¿Iniciar temas con frecuencia?
6. ¿Presentar una variedad de temas?
7. ¿Hablar de cosas que son de interés para los demás?
8. ¿Entiende el significado de lo que se habla en la
conversación?
9. ¿Tomar turnos como orador y oyente?
10. ¿Ajusta la conversación basado en el público? (por ej.,
hablar con un maestro a lo contrario de hablar con un
compañero)
11. ¿Solicitar información relevante?
12. ¿Ajusta la duración del turno basado en el comportamiento
del pareja?
13. ¿Cambiar temas suavemente?
14. ¿Terminar las conversaciones cortésmente?
15. ¿Usa y entiende los comportamientos de comunicación?
(véase la siguiente lista)
Por favor, indique los comportamientos que el estudiante observa para entender y/o
utilizar:
Entiende Usa
Sí No Sí No Expresión de la cara
Sí No Sí No Los gestos
Sí No Sí No Postura del cuerpo
Sí No Sí No Proximidad o distancia física a la pareja
Sí No Sí No Volumen o sonoridad de la voz
Sí No Sí No Entonación de la melodía de la voz
Sí No Sí No
Indicadores de emoción (por ej., felicidad, tristeza, enojo/ira)
Sí No Sí No El humor

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 73
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Sí No Sí No Las burlas
Sí No Sí No El sarcasm
Sí No Sí No El engaño
¿El estudiante:
Usualmente
Raramente
16. ¿Adaptarse fácilmente en situaciones de grupos nuevos?
17. ¿Expresar angustia o aburrimiento similar a los compañeros
de mismo nivel de habilidad?
18. ¿Responde a las observaciones y orientación ofrecida por
otros acerca de la regulación de la emoción?
19. ¿Hablar fluidamente sin repeticiones o vacilaciones (el
tartamudeo)?
20. ¿Usar calidad vocal consistente con la edad y el sexo? (p.
ej., ronquera, aspereza, respiración y tono)
21. ¿Recuerda las palabras asociadas con situaciones o
sustantivos específicos? (p. ej., sal y pimienta, béisbol y bate,
pan y mantequilla, garaje y coche)
22. ¿Entiende y utiliza antónimos y sinónimos?
23. ¿Discutir el significado de las palabras/definir palabras?
24. ¿Entiende más de un significado para las palabras? (p. ej.,
“café” significa como el color y la bebida)
25. ¿Poner ideas en palabras y explicar ideas?
26. ¿Entiende las sutilezas en significado de palabra y oración?
(p. ej., modismos, lenguaje figurativo)
27. ¿Distinguir la ficción de la no ficción, incluyendo el hecho y
la fantasía?
28. ¿Volver a contar los mensajes resumiendo o aclarando?
29. ¿Usa y entiende la negación? (por ej., Voy a ir al cine si no
es demasiado tarde.)

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 74
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
30. ¿Generar ideas antes de contar una historia?
31. ¿Usar una estructura de historia apropiado?
32. ¿Usar gramática de la historia?
33. ¿Es fácil entender el discurso del estudiante en la
conversación?
Si el estudiante es difícil de entender, nota los sonidos de
problema aquí:
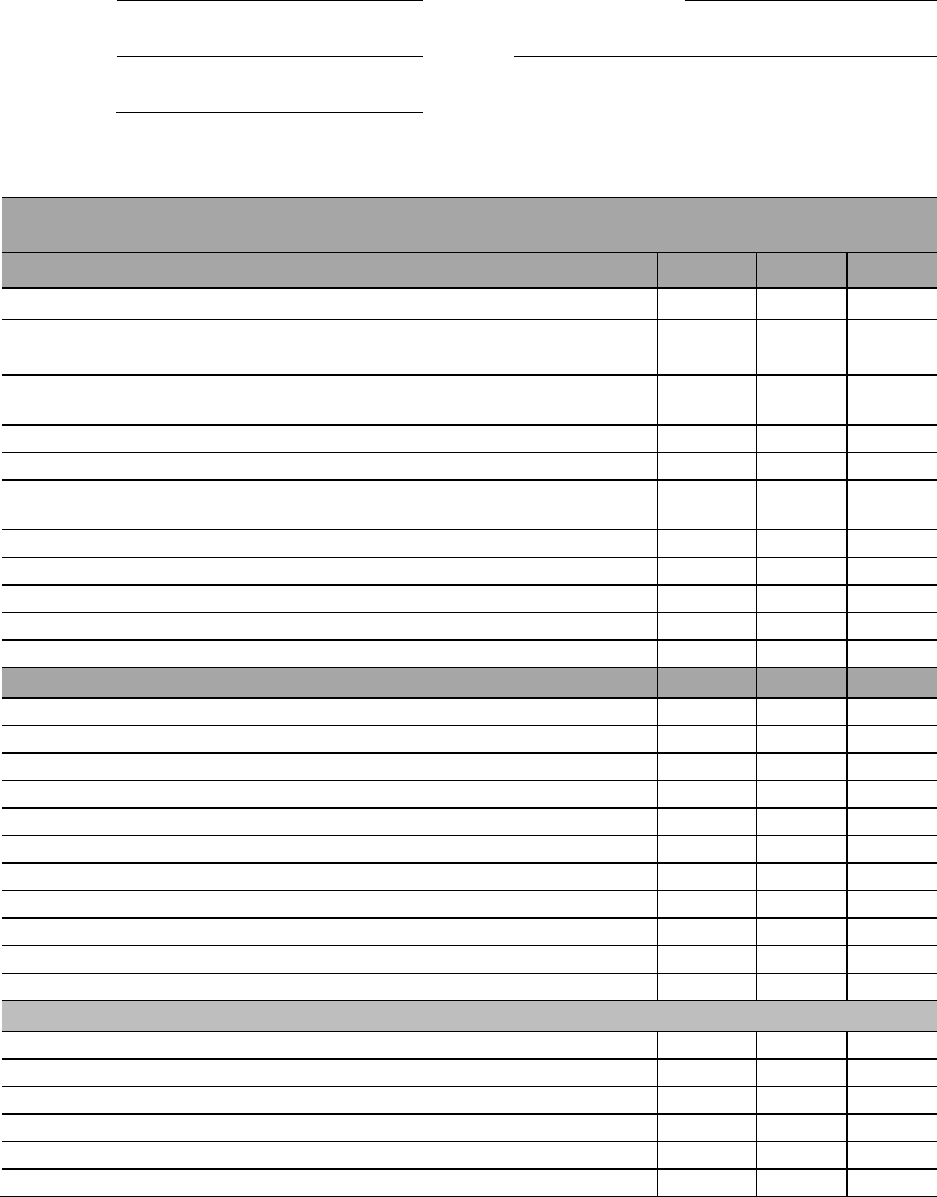
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 75
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Observation of Student Communication within the School Environment
Student: Date Completed:
School: DOB:
SLP:
Class/Subject Observed: (Observation should be in the area of suspected disability)
Communication
Behavior Regulation
Y N DNO
1. Respond to simple gestures used by adults when given directions
2. Independently carries out familiar, simple directions with minimal
repetition
3. Spontaneously communicates basic needs and desires clearly to
others
4. Asks for help by going to adult, raising hand, etc…
5. Shows approval or rejection in an appropriate way
6. Does not get upset when others are working or playing in close
proximity
7. Does not interrupt others
8. Reacts to changes in routine/environment
9. Insists on keeping certain objects with him/her
10. Engages in repetitive behaviors
11. Student appears to be in his/her “own world”
Social Interaction
Y N DNO
1. Seeks out and initiates contact with others
2. Interact with peers in routine structured work
3. Interacts with peers in play situations
4. Share and take turns with materials during group activities
5. Gain attention of others appropriately
6. Responds to others within environment by giving a response
7. Use and respond to greetings in familiar settings
8. Respond to own name
9. Acknowledge and respond to feelings by others
10. Use appropriate behavior to indicate desire to stop an activity
11. Ask to move from tasks to task as appropriate
Joint Attention
1. Comments on object held by others or in his sight
2. Adds new information to the topic of others
3. Responds to simple questions
4. Asks simple questions
5. Requests information
6. Clarifies

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 76
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Communication
Sensory
Y N DNO
1. Shows sensitivity to loud noises/lights
2. Engages in self-stimulatory behaviors (hand-flapping, rocking, spinning)
3. Resists being touched or held
4. Feels, smells and/or tastes objects in the environment
Communication Method Y N DNO
1. Understand and use gestures
2. Engage in echolalia
3. Display odd prosody or peculiar voice characteristics
4. Display adequate volume or rate of speech
5. Display scripted, stereotyped discourse
6. Display pedantic characteristics
7. Utilize idiosyncratic speech
8. Inappropriate use of pronouns
9. Use social rituals (please, thank you, excuse me)
10. Respond or reciprocate to greetings
Y = Yes, N = No, DNO = Did not observe
Comments:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 77
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Observation of the School Environment to Facilitate Communication
Student: Date
Completed:
School: SLP:
Class/Subject Observed: (Observation should be in the area of suspected
disability)
Observation of the School Environment to Facilitate Communication
(Curriculum Setting)
Area of Assessment Evidence/Examples
Yes No DNO
I. Classroom support of environmental events:
The classroom encourages
imitation
The classroom encourages
the child to comprehend
and use language
The classroom encourages play
The classroom provides
opportunities for peer
interaction.
II. Classroom support of functional skills:
Complying with adult requests
Turn taking
Responding to directions
across various proximities
Sitting quietly during activities
Participating during teacher
instruction
Walking in line
Using bathroom across settings

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 78
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
III. The environment fosters:
Independence
Initiative
Choice making
A variety of teaching
opportunities
The classroom supports teaching of:
Attention
Compliance
Imitation
Communication
Appropriate toy play

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 79
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Observation of the School Environment to Facilitate Communication
(Social Skills/Interactions)
Area of Assessment Evidence/Examples
Yes No DNO
I. The classroom maximizes learning through:
Repetition
Predictability
Classroom has a staff to child
ratio of _____ to _____
Student attends the program/school for an
average of ___ hours per day
Curriculum is integrated with
typical peers
Classroom uses a variety of
prompts
II. The classroom facilitates social interaction with:
Adults
Peers
Routines are evident
The student is motivated through a
variety of classroom activities
The classroom employs highly
preferred play materials or topics
III. Family involvement: (re-evaluations only)
Curriculum offers opportunities
for parents to be involved
Curriculum offers home visits
Curriculum offers the parents
behavioral strategies
Curriculum offers parent training
DNO - Did not observe
Adapted from: Dawson, G., & Osterling, J. (1997). Early intervention in autism: Effectiveness
and common elements of current approaches. In Guralnick, 1997.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 80
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Play-Based Skills Assessment
Speech
Articulation
Notes:
Fluency
Notes:
Voice
Notes:
Language: Form and Content
Cuing Codes: I: independent R: needs repetition P: needs pictures G: needs gestural cues M: needs model D: responds after a
delay
Column Codes: R: Receptive E: Expressive
Follow commands: Notes:
1 step
2 step
3+ step
Routine
Routine
Routine
Novel I R P
G M D
Novel I R P
G M D
Novel I R P
G M D
IDs/Names: objects/pictures from set of Notes:
R E
⃞
⃞
Colors I R P G M D
⃞ ⃞ Shapes I R P G M D
⃞ ⃞ Body parts I R P G M D
⃞ ⃞ Clothing I R P G M D
⃞ ⃞ Animals I R P G M D
⃞ ⃞ Food I R P G M D
⃞ ⃞ Transportation I R P G M D
⃞ ⃞ Family I R P G M D
⃞ ⃞ Other: I R P G M D
Student: Date
Completed:
School: SLP:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 81
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Pronouns:
R E
⃞ ⃞ I
⃞ ⃞ Me
⃞ ⃞ My
⃞ ⃞ Mine
⃞
⃞
Your
⃞
⃞
Gender
Notes:
Spatial/Prepositions:
R E
⃞ ⃞ In
⃞ ⃞ On
⃞ ⃞ Out
⃞ ⃞ Off
⃞ ⃞ Under
⃞ ⃞ Over
⃞ ⃞ Top
⃞ ⃞ Bottom
⃞ ⃞ Front
⃞ ⃞ Behind
⃞
⃞
Between
Notes:
Quantity/Size:
R E
⃞ ⃞ Big
⃞ ⃞ Little
⃞ ⃞ Tall
⃞ ⃞ Short
⃞ ⃞ Few
⃞ ⃞ Many
⃞
⃞
More
⃞
⃞
Less
Notes:
Descriptive Concepts:
R E
⃞ ⃞ Hot/Cold
⃞ ⃞ Fast/Slow
⃞ ⃞ Wet/Dry
⃞ ⃞ Sad/Happy
⃞ ⃞ Same/Different
⃞
⃞
Thirsty/Hungry
⃞
⃞
Other:
Notes:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 82
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Mode of Communication:
Limited verbal
Verbal, gestures/signs
AAC
Picture
Eye gaze
Body movements
Jargon
Notes:
Utterance Complexity:
Single words
words/ per phrase or sentence
Notes:
Uses:
Nouns
Plurals
Verbs
Progressive -ing
Past tense (regular)
Past tense (irregular)
Contractions
Conjunctions
Articles
Notes:
Asks and Answers Questions:
R E
⃞ ⃞ Yes/No
⃞ ⃞ What
⃞ ⃞ Where
⃞ ⃞ When
⃞ ⃞ Why
⃞ ⃞ How
Notes:
Language: Use (Pragmatic Language)
Cuing Codes: I: independent R: needs repetition P: needs pictures G: needs gestural cues M: needs model D: responds after a
delay

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 83
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Communicative Intent
Initiates to: Notes:
Greet
Respond
Comment
Request
Label
Protest
Converse
Verbal
Verbal
Verbal
Verbal
Verbal
Verbal
Verbal
Nonverbal
Nonverbal
Nonverbal
Nonverbal
Nonverbal
Nonverbal
Nonverbal
Social Interaction
Responds to:
Name I R P G M D
Noises I R P G M D
Questions I R P G M D
Notes:
Joint attention:
Sustained I R P G M D
Fleeting I R P G M D
Unable I R P G M D
Notes:
Social Games:
Participates for ____ turns
Resists
Ignores
Notes:
Shares items:
Appropriate
Minimally
With verbal prompts
With gestural prompts
Notes:
Play:
Spontaneous
Alone
Parallel
Imitates
Functional
(e.g. stacks blocks, pushes car)
Symbolic
Imaginary/pretend
Concrete
Sequenced
Interactive
Notes:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 84
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Follows another’s lead
Initiates themes in play
Nonverbal Communication
Eye Contact:
Appropriate
Checks in
Fleeting
None
Notes:
Body Position:
Appropriate
Turns body away
Difficulties with personal space
Notes:
Gestures:
Points
Waves
Nods
Grabs
Shrugs
Notes:
Response to Gestures:
Follows point with gaze
Does not notice
Notes:
Facial Expressions:
Appropriate
Neutral
Exaggerated
Minimal variation
Flat affect
Notes:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 85
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Restrictive and Repetitive Patterns of Behavior
Repetitive Speech, Motor, Object Use
Speech:
Echolalia
Delayed
Immediate
Jargon
Rote phrases
Pronoun reversals
Uses own name instead of I
Repetitive vocalizations
Notes:
Motor: Notes:
Hand:
Body:
Face:
Clapping
Flapping
Rocking
Spinning
Tensing
Teeth
grinding
Flicking
Finger
posturing
Toe walking
Body
posturing
Facial
grimacing
Other:
Object/Play:
Functional
Sensorimotor/exploration
(mouthing/rubbing)
Lines up
Drops intentionally/repetitively
Repetitive play
Opens/closes doors
Turns lights on/off
Notes:
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 86
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Routines/Resistance to Change
Transitions to and from testing:
Appropriately
Hesitant at first
Runs away/cries
Does not transition after time
Transitions between tasks:
Compliant
Persistent difficulties
Moving from preferred to non-preferred:
Difficulties with examiner led tasks
Easily transitions
Patterns of thinking:
Rule bound
Concrete
Flexible
Notes:
Interests/Focus
Plays with:
Wide variety
Narrow range
Carries object
Sensory interests:
Visual (light up)
Movement
Auditory
Focus on details/parts
Notes:
Sensory Input
Pain Response (parent report):
Typical
Hyper
Hypo
Describe any observations related to sensory
seeking or response behaviors to visual,
auditory, tactile, taste, or smell in notes.
Notes:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 87
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Communicative Intent Checklist
PV: Preverbal OW: One Word MW: Multiple Word
Skill PV OW MW
Behavioral Regulation
Request Object
Request Action
Protest
Social Interaction
Request Social Routine
Showing Off
Greeting
Calling
Acknowledgement
Request Permission
Joint Attention
Comment
Request Information
Clarification
Discourse Structure
Initiated
Respondent
Mode of Communication
Gestural
Vocal
Verbal
Gestural-Vocal
Gestural-Verbal
Adapted by Allan Bird from: Wetherby, 1988.
Student: Date
Completed:
School: SLP:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 88
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Gestural Skills Checklist
Student: Date Completed:
School: SLP:
The following checklist is designed to help the Speech-Language Pathologist assess the
development of communication in the very young child. It is designed to contain items which
are easily observed in normal interaction and can be scored with a minimum of interpretation
on the part of the examiner.
Skill: Present Not Present
Six to Nine Months
1. Extends arms when parents extend their arms to the child in
the gesture of picking them up.
2. Explores parent’s face, hair, person, but not other
individuals.
3. Selects and crawls toward parent, but not others.
4. Moves toward parents when alarmed.
5. Localizes the bell when rung laterally to the ear.
Nine to Twelve Months
1. Makes excursions from parent and returns.
2. Ceases activity when name is called or “no” is said.
3. Offers objects to another person.
4. Attends to adult when given simple command or gesture
5. Imitates gesture games such as the “Raspberry”
Twelve to Fifteen Months
1. Responds to request for a toy when given a gestural cue.
2. Pushes adult’s hand toward a toy which the child cannot
operate independently.
3. Tugs on parent when the child wants something.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 89
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
4. Localizes to sounds presented from below and above his field
of vision.
5. Waves bye-bye or plays peek-a-boo.
Fifteen to Eighteen Months
1. Hugs and kisses adults.
2. Points to an object which is out of his reach when he wants it.
3. Responds to request for a toy without a gesture.
4. Imitates simple motor activities such as patty-cake or others
very automatically.
5. Offers a toy to an adult and waits for the adult to activate the
toy. If no response will attempt again
Eighteen to Twenty One Months
1. Gives an object to the parent upon request.
2. Points and makes vocal/manual gesture towards an object to
call adults attention to it.
3. Imitates words.
4.Points to a familiar person when requested to do so.
5. Communicates “No” through some manner other than crying.
Twenty One to Twenty Four Months
1. Imitates pointing to 3-4 body parts or spontaneously points to
on body part upon request..
2. Responds to “Show me” by showing shoes or other clothing,
or own toys or other common objects.
3. Carries objects from one room to another when requested.
4. Gestures for someone to “Give me that” or uses other gestures
(other than pointing) to make wants known.
5. Identifies 7-10 pictures of common objects

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 90
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Conversational Skills Checklist
Student: Grade: Date:
Observer:
Position: (
Circle one)
Parent/ Teacher/ SLP
The Conversational Skills Checklist may be used as a Pre/Post Test to determine the following:
• A student’s strengths in using language skills in conversation
• A student’s needs for developing language skills in conversation
• A student’s progress towards proficiency of language skills in conversation
Directions for Observer: Mark (X) the student’s frequency of use or proficiency for each of the
skills listed on the chart. Base your responses on what has been observed at home (Parent), in the
classroom (Teacher), or during assessment and/or therapy sessions (SLP)
Conversational Skill Proficiency Codes
Opening Section: Not Yet Sometimes Proficient
Secures listener’s attention
Initiates topic of conversation
Asks permission before touching or borrowing other
people’s things
Makes eye contact with others
Uses friendly body language
Topic Selection: Not Yet Sometimes Proficient
Chooses topics that deal with “here and now”
Chooses topics that deal with the past
Chooses topics that deal with the future
Chooses interesting topics of conversation
Chooses topics appropriate for situation
Turn-Taking: Not Yet Sometimes Proficient
Overlap
Nature of Turn – Comment
Nature of Turn – Response
Nature of Turn – Directed
Takes turns in conversation
Waits to share at appropriate times
Invites others into conversation
Relinquishes turn to talk

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 91
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Topic Maintenance: Not Yet Sometimes Proficient
Maintained through repetition
Maintained through agreement
Maintained by adding information
Can sustain topic through several turns
Asks appropriate questions that are on topic
Topic Changing: Not Yet Sometimes Proficient
Introduces new topics
Reintroduces old topics
Shades topic of discussion
Can close or switch topics when appropriate
Repair: Not Yet Sometimes Proficient
Provides repairs when the listener doesn’t understand
Repeats what was said
Confirms what was said
Revises what was said
Adds additional information to what was said.
Provides cues
Inappropriate response
Seeks repairs when the speaker is not understood
Gives neutral-nonspecific message of lack of
understanding
Requests confirmation as to what was understood
Requests specific information to clarify
Quality: Not Yet Sometimes Proficient
A good listener when others are speaking
Remembers to thank others for help
Expresses sympathy when other people are hurting
Considers how words affect others before speaking
Manner: Not Yet Sometimes Proficient
Keeps messages of conversation organized (tells
things in order)
Focuses on most important details, clearly and
concisely
Uses cohesion (links ideas)
Relation: Not Yet Sometimes Proficient
Responds appropriately to others’ messages
Asks for clarification of messages from other people
Elaborates on a topic when appropriate
Disagrees without disrupting

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 92
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Assertiveness: Not Yet Sometimes Proficient
Asks question more than once if message
not understood
Continues to try to get messages across if listener
does not understand
Observer Comments:
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 93
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Evaluation Phase III: Analysis and Interpretation Form
Language Evaluation Summary Form
Initial Disability Determination Worksheet

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 94
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Language Evaluation Summary Form
Student:
Campus:
SLP:
Date of Birth:
Grade: Date Completed:
Assessment Questions:
Evaluation Tool
Results
Data Supports
Concern
Yes No
Teacher Checklist/
Interview
Parent Information/
Interview
Standardized
Test/Subtest
Results
Score/s:
Standard Deviation
Confidence Interval
Sensitivity
Specificity

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 95
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA). Please
note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the guidelines.
They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Evaluation Tool Results
Data
Supports
Concern
Informal Criterion-
Referenced Measures:
Language Sample
Checklists
Interviews/
Questionnaires
Skill Specific Probes
Language Skills:
Results/Comments:
Yes No
Syntax/ Morphology
Semantics
Metalinguistics
Phonology:
Speech Sounds
Reading/ Reading Readiness
Pragmatics:
Social Communication
Narrative Skills
Discourse Skills
Social Interaction:
Nonverbal Behaviors to Regulate
Interaction
Turn-Taking
Joint Attention
Shared Emotion
Use of Communication to
Regulate Interactions
Initiate/Sustain
Conversation
Intentionality
:
Request, Protest, Reject

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 96
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA). Please
note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the guidelines.
They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Interaction:
Initiate, Respond,
Maintain, Terminate,
Repair, Request, Greetings
Focused Observations
Other Assessment
Information

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 97
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA). Please
note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the guidelines.
They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Recommendations to the ARD
Committee
Yes No
Stage I:
Presence of a Language Disorder
Evidence:
Stage II:
Adverse Effect on Educational
Performance
Evidence (enter rating from Adverse
Effect Checklist):
Academic Achievement:
Functional Performance:
If yes to Stage I and II, the Disability Determination for Language Disorder has been met
Recommendation that ARD Committee consider eligibility for special education with a
Speech Impairment
Yes No
If ARD Committee determines SI eligibility, then address Stage III:
Are specialized services by an SLP needed to help the student with a language disorder
make progress in the curriculum?
Yes No
Recommendations for SLP services:

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 98
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Initial Disability Determination Worksheet
Autism/Speech Impairment
Student Name :
Age:
Data Reconciliation
Check areas where data supports concern in the listed areas.
Parent Teacher Evaluator
Persistent deficits in social communication and social interaction
Deficits in social-emotional reciprocity:
from abnormal social approach and failure of normal back-and-forth conversation; to
reduce sharing of interests, emotions, or affect; to failure to initiate or respond to social
interactions.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in nonverbal communication behaviors used for social
interaction:
f
rom poorly integrated verbal and nonverbal communication; to
abnormalities in eye contact and body language or deficits in understanding and use of
gestures; to a total lack of facial expressions and nonverbal communication.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in developing, maintaining, and understanding relationships:
from difficulties adjusting behavior to suit various social contexts; to difficulties in
sharing imaginative play or in making friends; to absence of interest in peers.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in understanding what is not explicitly stated
(e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g.,
idioms, humor, metaphors, multiple meanings that depend on the context for
interpretation).
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in ability to change communication to match context or the
needs of the listener, e.g. speaking differently in a classroom than on the
playground, talking differently to a child than to an adult, and avoiding the use of
overly formal language.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits reporting a personal experience in a logical sequence with
sufficient information for listener understanding.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Restricted, repetitive patterns of behavior, interests, or activities (currently or in history)
Stereotyped or repetitive motor movements, use of objects, or speech
e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia,
idiosyncratic phrases.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Insistence on sameness, inflexible adherence to routines, or ritualized
patterns or verbal nonverbal behavior
e.g., extreme distress at small changes, difficulties with transitions, rigid thinking
patterns, greeting rituals, need to take the same route or eat food every day.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Highly restricted, fixated interests abnormal in intensity or focus
e.g., strong attachment to or preoccupation with unusual objects, excessively
circumscribed or preservative interest.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 99
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Hyper- or hyporeactivity to sensory input or unusual interests in
sensory aspects of the environment
e.g., apparent indifference to pain/temperature, adverse response to specific sounds or
textures, excessive smelling or touching of objects, visual fascination with lights or
movement.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Parent Teacher Evaluator
Other Speech/Language Characteristics related to Autism:
Loss of previously acquired language skills
☐
☐☐
☐
Difficulty with pronouns
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Higher expressive language skills than receptive language skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Pedantic speech (overly formal; repetitive use of phrases (e.g. “well
actually”)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Characteristics of typical stuttering (initial position sound, syllable,
word repetitions; phrase repetitions; sound prolongations; blocks)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Characteristics of atypical stuttering observed in ASD
word-final disfluency (repetition of the last syllable in a word); word-
medial blocks (stopping of airflow or sound in the middle of a word);
mid-syllable insertion (inserting a syllable in a word); final sound
prolongation (final sound continues beyond typical length); final
phrase repetition (repeating the final phrase)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Atypical speech prosody (intonation, tone, stress, and rhythm)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Adaptive Behavior/Cognitive Observations
Deficits social adaptive skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Splinter skills observed in cognitive or academic skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in working memory
☐
☐☐
☐
Visual processing noted to be a relative strength
☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 100
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Executive Functioning
Deficits with planning and organization
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with initiation and sequencing of tasks
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with shifting between tasks
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with emotional regulation
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with problem solving
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Other Considerations
Family history of autism
☐
☐☐
☐
Family history of ADHD
☐
☐☐
☐
Family history of mental illness
☐
☐☐
☐
Family history of cognitive/learning disability
☐
☐☐
☐
Significant health concerns:
☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 101
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage I: Documentation of Disability
Yes No
Based on evaluation data (formal and/or informal), does the student demonstrate deficits in
social communication and social interaction?
Based on evaluation data (formal and/or informal), does the student demonstrate restricted,
repetitive patterns of behavior, interests, or activities (currently or in history)?
Are the student’s communication skills disproportionate with the level of overall functioning,
especially in adaptive skills and social communication skills which allow for effective
interpersonal communication?
Are the student’s communication abilities disproportionate to those of the same chronological
age, gender, intellectual level, or cultural and linguistic background?
Data supports BOTH deficits in social communication and social interaction and presence of restricted, repetitive
patterns of behavior, interests, or activities (currently or in history); AND results are not better explained by
Intellectual Disability or Emotional Disturbance AND communication skills are disproportionate with overall
functioning and to those of same age/gender/intellectual level/CLD background:
● IF YES: Team concludes the presence of disability of Autism and Communication Disorder
Data supports ONLY deficits in social communication, with NO current or historic observation of restricted, repetitive
patterns of behavior, interests, or activities AND communication skills are disproportionate with overall functioning
and to those of the same age/gender/intellectual level/CLD background:
● IF YES: Team concludes the presence of Social Communication Disorder/Pragmatic Language Disorder
Data supports BOTH deficits in social communication and social interaction and presence of restricted, repetitive
patterns of behavior, interests, or activities (currently or in history); AND results are not better explained by
Intellectual Disability or Emotional Disturbance BUT communication skills are NOT disproportionate with overall
functioning and to those of the same age/gender/intellectual level/CLD background OR social communication deficits
are mild in nature:
● IF YES: Team concludes the presence of disability of Autism

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 102
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage II: Adverse Effect on Educational Performance
Academic Achievement Yes No
There is a direct, noticeable relationship between the student’s communication disorder and
academic performance or achievement
The student’s communication disorder contributes to academic struggle or below expected
achievement on the IEP
The student’s communication disorder is out of proportion with overall functioning level
Data indicates that the student’s performance in the academic curriculum will require
specially designed instruction from the SLP
The student with other disabilities needs speech-language therapy to benefit from the special
education program
Functional Performance Yes No
Communication skills limit participation in self-care, interpersonal, and daily routines
Communication patterns disrupt and interfere with interaction and functional performance
Social communication skills disrupt effective interpersonal interaction
Communication disorder is pervasive and noticeable across settings and interferes with
interaction
The student has no functional communication, limited means of expression, or
social/emotional adjustment is affected by the communication disorder
Total
Scoring
If the answer to at least 4 of the statements is “yes”, it is likely that the student’s language
disorder results in an adverse effect on educational performance
Sources of Documentation of Adverse Effect
Grades
State, District, Local Assessments/Tests
Student Work
Observation
Teacher/Parent Information
Student Self-Report
Other
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 103
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Re-Evaluation Form
Re-Evaluation Disability Determination Worksheet

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 104
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Reevaluation Disability Determination Worksheet
Autism/Speech Impairment
Student Name :
Age:
;
Data Reconciliation
Parent Teacher Evaluator
Persistent deficits in social communication and social interaction
Deficits in social-emotional reciprocity:
from abnormal social approach and failure of normal back-and-forth conversation; to reduce
sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in nonverbal communicative behaviors used for social
interaction: from poorly integrated verbal and nonverbal communication; to
abnormalities in eye contact and body language or deficits in understanding and use of
gestures; to a total lack of facial expressions and nonverbal communication.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in developing, maintaining, and understanding relationships: from
difficulties adjusting behavior to suit various social contexts; to difficulties in sharing
imaginative play or in making friends; to absence of interest in peers.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in understanding what is not explicitly stated
(e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g., idioms,
humor, metaphors, multiple meanings that depend on the context for interpretation).
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits inability to change communication to match context or the needs
of the listener, e.g. speaking differently in a classroom than on the playground, talking
differently to a child than to an adult, and avoiding use of overly formal language.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Restricted, repetitive patterns of behavior, interests, or activities (currently or in history)
Stereotyped or repetitive motor movements, use of objects, or speech e.g.,
simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Insistence on sameness, inflexible adherence to routines, or ritualized
patterns or verbal-nonverbal behavior
e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns,
greeting rituals, need to take same route or eat food every day.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Highly restricted, fixated interests abnormal in intensity or focus
e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed
or preservative interest.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Hyper- or hyporeactivity to sensory input or unusual interests in sensory
aspects of the environment
e.g., apparent indifference to pain/temperature, adverse response to specific sounds or
textures, excessive smelling or touching of objects, visual fascination with lights or
movement.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 105
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Parent Teacher Evaluator
Persistent deficits in social communication and social interaction
Deficits in social-emotional reciprocity:
from abnormal social approach and failure of normal back-and-forth conversation; to reduce
sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in nonverbal communication behaviors used for social
interaction: from poorly integrated verbal and nonverbal communication; to
abnormalities in eye contact and body language or deficits in understanding and use of
gestures; to a total lack of facial expressions and nonverbal communication.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in developing, maintaining, and understanding relationships: from
difficulties adjusting behavior to suit various social contexts; to difficulties in sharing
imaginative play or in making friends; to absence of interest in peers.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in understanding what is not explicitly stated
(e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g., idioms,
humor, metaphors, multiple meanings that depend on the context for interpretation).
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in ability to change communication to match context or the needs
of the listener, e.g. speaking differently in a classroom than on the playground, talking
differently to a child than to an adult, and avoiding use of overly formal language.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits reporting a personal experience in a logical sequence with
sufficient information for listener understanding.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Restricted, repetitive patterns of behavior, interests, or activities (currently or in history)
Stereotyped or repetitive motor movements, use of objects, or speech e.g.,
simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Insistence on sameness, inflexible adherence to routines, or ritualized
patterns or verbal nonverbal behavior
e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns,
greeting rituals, need to take the same route or eat the same food every day.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Highly restricted, fixated interests abnormal in intensity or focus
e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed
or preservative interest.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Hyper- or hyporeactivity to sensory input or unusual interests in sensory
aspects of the environment
e.g., apparent indifference to pain/temperature, adverse response to specific sounds or
textures, excessive smelling or touching of objects, visual fascination with lights or
movement.
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 106
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Parent Teacher Evaluator
Other Speech/Language Characteristics related to Autism:
Loss of previously acquired language skills
☐
☐☐
☐
Difficulty with pronouns
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Higher expressive language skills than receptive language skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Pedantic speech (overly formal; repetitive use of phrases (e.g. “well
actually”)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Characteristics of typical stuttering (initial position sound, syllable, word
repetitions; phrase repetitions; sound prolongations; blocks)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Characteristics of atypical stuttering observed in ASD
word-final disfluency (repetition of the last syllable in a word); word-
medial blocks (stopping of airflow or sound in the middle of a word);
mid-syllable insertion (inserting a syllable in a word); final sound
prolongation (final sound continues beyond typical length); final phrase
repetition (repeating the final phrase)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Atypical speech prosody (intonation, tone, stress, and rhythm)
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Adaptive Behavior/Cognitive Observations
Deficits social adaptive skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Splinter skills observed in cognitive or academic skills
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Deficits in working memory
☐
☐☐
☐
Visual processing noted to be a relative strength
☐
☐☐
☐
Executive Functioning
Deficits with planning and organization
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
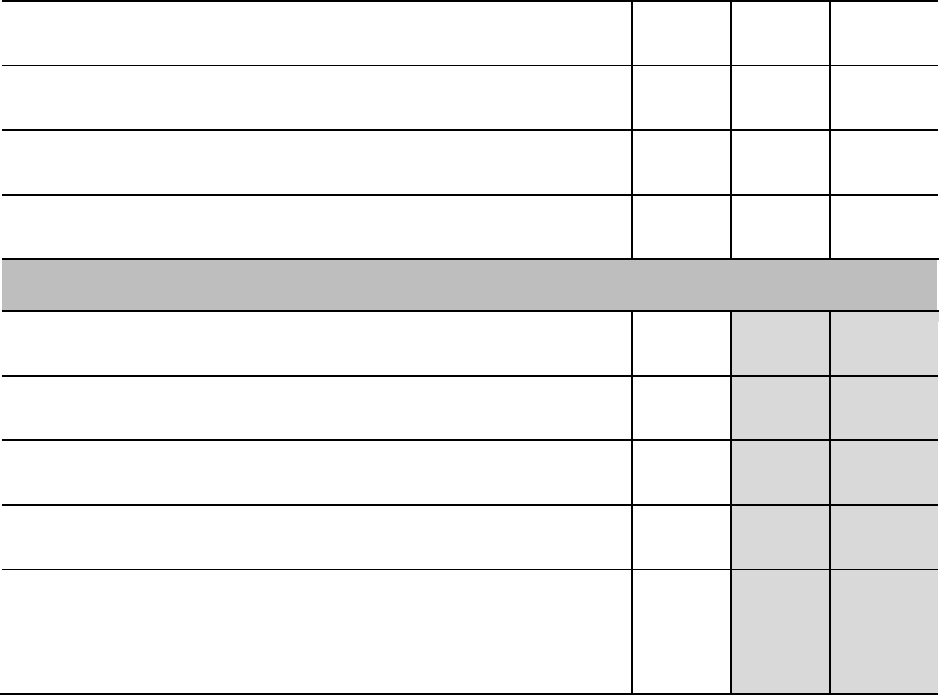
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 107
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Difficulty with initiation and sequencing of tasks
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with shifting between tasks
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with emotional regulation
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Difficulty with problem solving
☐
☐☐
☐ ☐
☐☐
☐ ☐
☐☐
☐
Other Considerations
Family history of autism
☐
☐☐
☐
Family history of ADHD
☐
☐☐
☐
Family history of mental illness
☐
☐☐
☐
Family history of cognitive/learning disability
☐
☐☐
☐
Significant health concerns:
☐
☐☐
☐

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 108
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage I: Documentation of Disability
Yes No
Based on evaluation data (formal and/or informal), does the student demonstrate deficits in
social communication and social interaction?
Based on evaluation data (formal and/or informal), does the student demonstrate restricted,
repetitive patterns of behavior, interests, or activities (currently or in history)?
Are the student’s communication skills disproportionate with the level of overall functioning,
especially in adaptive skills and social communication skills which allow for effective
interpersonal communication?
Are the student’s communication abilities disproportionate to those of the same chronological
age, gender, intellectual level, or cultural and linguistic background?
Data supports BOTH deficits in social communication and social interaction and presence of restricted, repetitive
patterns of behavior, interests, or activities (currently or in history); AND results are not better explained by
Intellectual Disability or Emotional Disturbance AND communication skills are disproportionate with overall
functioning and to those of same age/gender/intellectual level/CLD background:
IF YES: Team concludes presence of disability of Autism and Communication Disorder
Data supports ONLY deficits in social communication, with NO current or historic observation of restricted, repetitive
patterns of behavior, interests, or activities AND communication skills are disproportionate with overall functioning
and to those of the same age/gender/intellectual level/CLD background:
IF YES: Team concludes presence of disability of Social Communication Disorder (Pragmatic Language
Disorder)
Data supports BOTH deficits in social communication and social interaction and presence of restricted, repetitive
patterns of behavior, interests, or activities (currently or in history); AND results are not better explained by
Intellectual Disability or Emotional Disturbance BUT communication skills are NOT disproportionate with overall
functioning and to those of the same age/gender/intellectual level/CLD background OR social communication deficits
are mild:
IF YES: Team concludes presence of disability of Autism

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 109
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Stage II: Adverse Effect on Educational Performance
Academic Achievement Yes No
There is a direct, noticeable relationship between the student’s communication disorder and
academic performance or achievement
The student’s communication disorder contributes to academic struggle or below expected
achievement on the IEP
The student’s communication disorder is out of proportion with overall functioning level
Data indicates that the student’s performance in the academic curriculum will require
specially designed instruction from the SLP
The student with other disabilities needs speech-language therapy to benefit from the special
education program
Functional Performance Yes No
Communication skills limit participation in self-care, interpersonal, and daily routines
Communication patterns disrupt and interfere with interaction and functional performance
Social communication skills disrupt effective interpersonal interaction
Communication disorder is pervasive and noticeable across settings and interferes with
interaction
The student has no functional communication, limited means of expression, or
social/emotional adjustment is affected by the communication disorder
Total
Scoring
If the answer to at least 4 of the statements is “yes,” it is likely that the student’s language disorder results in an
adverse effect on educational performance
Sources of Documentation of Adverse Effect
Grades
State, District, Local Assessments/Tests
Student Work
Observation
Teacher/Parent Information
Student Self-Report
Other

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 110
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Potential Additional Dismissal Considerations
The student is unable to tolerate treatment because of a serious medical, psychological, or other condition?
The student demonstrates behavior that interferes with improvement or participation in treatment (e.g.,
noncompliance, malingering), providing that efforts to address the interfering behavior have been unsuccessful.
Speech-language therapy no longer affects change in the student’s communication skills. There does not appear
to be any reasonable prognosis for improvement with continued treatment.
When using these as a basis for dismissal, the campus SLP should work with the multidisciplinary
team to document minimal educational benefit from speech-language services.
The following factors should be considered:
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 111
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Dismissal Form
Factors to Consider in Dismissal from SLP Therapy Services

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 112
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Factors to Consider in Dismissal from SLP Therapy Services
DURATION, INTENSITY, & MODE OF SERVICE
What has been the duration of speech therapy services?
What has been the duration of therapy for current goals/objectives?
How frequently does the student receive such therapy?
Have alternative intensity levels of treatment been utilized?
Have alternative modes of service (individual therapy, group
therapy, integrated therapy, etc.) been utilized to stimulate
progress?
Have various models of service been used for a sufficient time
period?
FOCUS OF SERVICE
Have treatment methods been appropriate for the diagnosed
disorder?
Were appropriate goals/objectives established?
What has been the student’s level of response to treatment
method(s)?
Within the scope of the treatment program, has the student been
able to progress to the next level of the program or a branch of that
program?
Has treatment been at an appropriate level for the student?
Has the SLP truly individualized instruction for the student?
SETTING
What is the student missing in the regular classroom during speech
therapy?
Have alternative therapy times (different time of day, etc.) been
tried?
Is SLP working with regular and/or special education teachers to
assure curricular and/or instructional modifications are
implemented if they are needed?
PATTERN OF SERVICE DELIVERY
How has therapy been provided in the past?
What has been the focus of therapy in the past?
Have there been gaps in service (has child moved frequently or had
frequent absences)?
CAPACITY OF STUDENT FOR CHANGE
Has student been more responsive to therapy at times? Has there
been a pattern of regression and/or progression? When has he/she
been most responsive?
How do other service providers regard the child’s progress to date?
His/her responsiveness to therapy?
Does therapy and/or the IEP provide motivational incentives?
Has the SLP maximized therapy when progress is being achieved?
Adapted from: Texas Speech-Language Hearing Association. (2012). Language Eligibility Manual Companion III: Autism
Spectrum Disorders: Dismissal Considerations. Available from https://www.txsha.org/page/speech-impairment-eligibility-
guidelines and USA, Arkansas Department of Education, Special Education. (n.d.). Eligibility Criteria and Program Guidelines
for Children with Disabilities, Ages 3-21, PART III: Program Guidelines, Section 2: Use of Criteria for Dismissal from Speech
or Language Therapy Services. https://arksped.k12.ar.us/rules_regs_08/3. SPED ELIGIBILITY CRITERIA AND PROGRAM
GUIDELINES FOR CHILDREN/PART III PROGRAM GUIDELINES/2. USE OF CRITERIA FOR DISMISSAL FROM
SPEECH OR LANGUAGE THERAPY.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 113
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
References
Amend, E. R., Beaver-Gavin, K., Schuler, P., & Beights, R. (2008). Giftedness/ Asperger’s
Disorder Checklist (GADC) Pre-Referral Checklist. Lexington, KY: Amend
Psychological Services.
Amend, E., Schuler, P., Beaver-Gavin, K., & Beights, R. (2009). A unique challenge: Sorting out
the differences between giftedness and Asperger’s disorder. Gifted Child Today, 32(4),
57-63.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders
(4th ed.). Washington DC: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders
(5th ed.). Washington DC: American Psychiatric Publishing.
American Speech-Language-Hearing Association. (n.d.). Autism. https://www.asha.org/Practice-
Portal/Clinical-Topics/Autism/.
American Speech-Language-Hearing Association. (n.d.). Decision making in termination of
services. https://www.asha.org/NJC/Decision-Making-in-Termination-of-Services/
American Speech-Language-Hearing Association. (n.d.). Eligibility and dismissal in schools.
https://www.asha.org/slp/schools/prof-consult/eligibility/
American Speech-Language-Hearing Association. (n.d.). Language in brief. https://www.
asha.org/Practice-Portal/Clinical-Topics/Spoken-Language-Disorders/Language-In--
Brief/.
American Speech-Language-Hearing-Association. (n.d.). Social communication benchmarks.
https://www.asha.org/uploadedFiles/ASHA/Practice_Portal/Clinical_Topics/Social_Com
munication_Disorders_in_School-Age_Children/Social-Communication-Benchmarks.pdf.
American Speech-Language-Hearing Association. (n.d.) Social communication disorder.
https://www.asha.org/Practice-Portal/Clinical-Topics/Social-Communication-Disorder/
American Speech-Language-Hearing Association. (n.d.). Typical speech and language
development. https://www.asha.org/public/speech/development/.
American Speech-Language-Hearing Association. (1993). Definitions of communication
disorders and variations. www.asha.org/policy.
American Speech-Language-Hearing Association. (2004). Admission/Discharge criteria in
speech-language pathology: Ad hoc committee on admission/discharge criteria in
speech- language pathology. Rockville, MD: Author.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 114
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
American Speech-Language-Hearing Association. (2016). Autism, clinical practice, practice
portal. https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589935303&
section=Overview.
American Speech-Language-Hearing Association. (2016). Code of ethics. www.asha.org/policy.
American Speech-Language-Hearing Association. (2016). Scope of Practice in Speech-
Language Pathology. www.asha.org/policy.
Arkansas Department of Education (ADOE). (n.d.). Eligibility criteria and program guidelines
for children with disabilities, Ages 3-21, (Part III, Section 2 paragraph 6).
https://dese.ade.arkansas.gov/Offices/special-education/policy-regulations/eligibility-
criteria-program-guidelines
Attwood, T. (1998). Asperger’s syndrome: A guide for parents and professionals. London, UK:
Jessica Kingsley.
Attwood, T. (2006). Autism and Asperger syndrome: Preparing for adulthood, (2
nd
ed.). Journal
of Child Psychology and Psychiatry, 47(2), 223–224.
Attwood, T., et al., (2006). Asperger’s and girls. Arlington, TX: Future Horizons
Autism Speaks (n.d.). Learn the signs. https://www.autismspeaks.org/learn-signs.
Bishop, D., (2006). Children’s Communication Checklist, (2nd ed. – U.S. ed.). San Antonio, TX:
Pearson.
Bowers, L., Huisingh, R., & LoGuidice, C. (2007). Test of Problem Solving 2: Adolescent
(TOPS-2:A). Austin, TX: PRO-ED.
Bowers, L., Huisingh, R., & LoGuidice, C. (2016). Social Language Development Test -
Elementary: Normative Update (SLDT-E:NU). Austin, TX: PRO-ED.
Bowers, L., Huisingh, R., & LoGuidice, C. (2017). Social Language Development Test -
Adolescent: Normative Update (SLDT-A:NU). Austin, TX: PRO-ED.
Bowers, L., Huisingh, R., & LoGuidice, C. (2018). Test of Problem Solving 3 Elementary:
Normative Update (TOPS-3E:NU). Austin, TX: PRO-ED.
Campbell, R., et al. (1999). When does the inner face advantage in familiar face advantage
recognition arise – and why? Visual Cognition, 6, 197–216.
Carpenter, M., & Tomasello, M. (2000). Joint attention, cultural learning, and language
acquisition: Implications for children with autism. In A. M. Wetherby & B. M. Prizant
(Eds.) Communication and language issues in autism and pervasive developmental
disorder: A transactional developmental perspective. (pp. 31-54). Baltimore, MD:
Brookes.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 115
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Carrow-Woolfolk, E., (2017). Comprehensive assessment of spoken language, (2nd ed.). (CASL-
2). Torrance, CA: Western Psychological Services
Code of Federal Regulations, 34 C.F. R. § 300. (2006).
Curenton, S. M., & Justice, L. M. (2004). African American and Caucasian preschoolers' use of
decontextualized language: Literate language features in oral narratives. Language,
Speech, and Hearing Services in Schools, 35, 240–253.
Dawson, G., Toth, K., Abbott, R., Osterling, J., Munson, J., Estes, A., & Liaw, J. (2004). The
effectiveness of early intervention (pp. 307-326). Baltimore, MD: Brookes.
Elleseff, T. (2015). Assessing social communication abilities of school-aged children.
Perspectives on School-Based Issues, 16(3), 79. doi:10.1044/sbi16.3.79
Gillam, R., & Pearson, N., (2017). Test of Narrative Language, (2nd ed.). (TNL-2). Austin, TX:
PRO-ED.
Gilliam, J. (2013). Gilliam Autism Rating Scale, (3
rd
ed.). (GARS-3). pearsonassessments.com
Gilliam, J., & Miller, L., (2006). Pragmatic Language Skills Inventory (PLSI). Austin, TX; PRO-
ED.
Guralnick (Ed.). (1997). The effectiveness of early intervention: Second generation research.
(pp. 307-326). Baltimore, MD: Brookes.
Haute Autorité de la Santé. (2018). Autism spectrum disorder - warning signs, screening,
diagnosis and assessment in children and adolescents. https://www.asha.org/
articlesummary.aspx?id=8589979692
Iancommunity.org
Inglebret E., Jones, C., & Pavel, D. M. (2008). Integrating American Indian/Alaska Native
culture into shared storybook intervention. Language, Speech, and Hearing Services in
Schools, 39, 521–527.
Keller-Bell, Y. D. (2017). Disparities in the identification and diagnosis of autism spectrum
disorder in culturally and linguistically diverse populations. Perspectives of the ASHA
Special Interest Groups, 2(14), 68-81.
Kennedy Krieger Institute, Patient Care, Conditions. (n.d.). Restrictive and repetitive behavior.
https://www.kennedykrieger.org/patient-care/conditions/restrictive-and-repetitive-
behavior.
Kopp, S., & Gillberg, C., (2011). The autism screening questionnaire (ASSQ)-revised extended
version (ASSQ-REV): An instrument for better capturing the autism phenotype in girls?
A preliminary study involving 191 clinical cases and community controls. Research in
Developmental Disabilities, 32(6), 875-888.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 116
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Landry, S. H., & Loveland, K. A. (1989). The effect of social context on the functional
communication skills of autistic children. Journal of Autism and Developmental
Disorders, 19(2), 283-299.
Lavi, A., (2019). Clinical assessment of pragmatics (CAPs). Torrence, CA; Western
Psychological Services.
Lavi, A., (2020). IMPACT Social Communication Rating Scale. Lavi Institute.
https://videolearningsquad.com/wp-content/uploads/2020/10/IMPACT-Social-Rating-
Scale-manualupdated-by-charlotte.pdf
LeCouteur, A., Lord, C., & Rutter, M. (2003). Autism diagnostic interview-revised (ADI-R).
Torrance, CA: Western Psychological Services.
Linder, T., Tanni, A., Bundy, A., Charlifue-Smith, R., Hafer, J., Hancock, F., & Rooke, C.
(2008). Transdisciplinary play-based assessment, (2nd ed.). Baltimore, Maryland: Paul
H. Brooks.
Lord, C., & Corsello. C. (2005). Diagnostic instruments in autism spectrum disorders, in F.
Volkmer, R. Paul, A. Klin, & D. Cohen, Handbook of autism and pervasive
developmental disorders, (vol. 2, 3rd ed.). https://doi.org/10.1002/9780470939352.ch2
Lord, C., & Paul, R. (1997). Language and communication in autism. In D. J. Cohen & F. R.
Volkmar (Eds.), Handbook of autism and pervasive developmental disorders (2nd ed.,
pp. 195-225). New York, NY: Wiley.
Lord, C., et al. (2012). Patterns of developmental trajectories in toddlers with autism spectrum
disorder. Journal of Consulting and Clinical Psychology, 80(3), 477–
489. https://doi.org/10.1037/a0027214
Monteiro, M. D., & Stegall, S. (2018). Monteiro interview guidelines for diagnosing the autism
spectrum, (2nd ed.). (MIGDAS-2) Los Angeles, CA: Western Psychological Services
Mount, M. (2014). Facilitating cohesive service delivery through collaboration. Perspectives on
School-Based Issues, 15(1), 15. doi:10.1044/sbi15.1.15
National Research Council. (2001). Educating children with autism. Washington, DC: National
Academy Press, Committee on Educational Interventions for Children with Autism,
Division on Behavioral and Social Sciences and Education.
Norbury, C. F., & Sparks, A. (2013). Difference or disorder? Cultural issues in understanding
neurodevelopmental disorders. Developmental Psychology, 49(1):45-58.
Ohio Developmental Disabilities Council, Ohio Center for Autism and Low Incidence, et al.
(2011). Autism: Reaching for a Brighter Future. Service Guidelines for Individuals with
Autism Spectrum Disorder through the Lifespan, (2-143). Columbus, OH: Author.
https://www.asha.org/ArticleSummary.aspx?id=8589961619.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 117
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
O’Neill, D. (2009). Language Use Inventory. https://languageuseinventory.com
Phelps-Teraski, D., & Phelps-Gunn, T. (2007). Test of Pragmatic Language, (2nd ed.). (TOPL-
2). Torrance, CA: Western Psychological Services
Prizant, B. M., Wetherby, A. M., Rubin, E., & Laurent, A. C. (2003). The SCERTS Model: A
transactional, family-centered approach to enhancing communication and socioemotional
abilities of children with autism spectrum disorder. Infants and Young Children, 16, 296-
316.
Reed, V. A. (2016). Language impairment in adolescents: Impact, assessment, and intervention.
https://www.asha.org/Professional-Development/ASHA-Learning-Center/.
Rutter M., LcCouteur, A., & Lord, C. (2003). Autism diagnostic interview-revised. Los
Angeles, CA: Western Psychological Services.
Rydell, P. J., & Prizant, B. M. (1995). Assessment and intervention strategies for children who
use echolalia. In K. A. Quill (Ed.), Teaching children with autism: Strategies to enhance
communication and socialization (pp. 105-132). Albany, NY: Delmar.
Schopler, E., Van Bourgondien, M. E., Wellman, G. J., & Love, S. R. (2010). The Childhood
Autism Rating Scale (2nd ed.). (CARS2). Los Angeles, CA: Western Psychological
Services.
Shattuck, P. et al. (2009). Timing of identification among children with an autism spectrum
disorder: Findings from a population-based surveillance study. J Am Acad Child Adolesc
Psychiatry, 48(5), 474-483. doi: 10.1097/CHI.0b013e31819b3848.
Shipley, K., & McAfee, J. (2008). Assessment in speech language pathology: A resource
manual, (4th ed.). Boston, MA: Cengage Learning
Stone, W. L., & Hogan, K. L. (1993). A structured parent interview for identifying young
children with autism. J Autism Dev Disord 23, 639–652.
https://doi.org/10.1007/BF01046106
Tager-Flusberg, H., Rogers, S., Cooper, J., Landa, R., Lord, C., Paul, R., Rice, M., Stoel-
Gammon, C., Wetherby, A., & Yoder, P., (2009). Defining spoken language benchmarks
and selecting measures of expressive language development of young children with
autism spectrum disorders. Journal of Speech, Language, and Hearing Research, 52,
643-652.
Texas Administrative Code. 19 TAC § 89.1040 (c) (1) (2018).
Texas Education Agency. (n.d.). Texas essential knowledge and skills. https://tea.texas.gov/
curriculum/teks/

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 118
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Texas Education Agency. (2009). Related services for students with disabilities – questions and
answers. http://www.txspot.org/Documents/Related%20Services%20Q%20and%20A
%20Document.pdf.
Texas Speech-Language Hearing Association. (2011). Language eligibility manual:
Conversation development in children. https://www.txsha.org/d/do/871.
Texas Speech-Language Hearing Association. (2012). Language eligibility manual companion
III: Autism spectrum disorders: Dismissal considerations. https://www.txsha.org/page/
speech-impairment-eligibility-guidelines
Uljarevic, M., & Hamilton, A. (2012). Recognition of emotions in autism: A formal meta-
analysis. Journal of Autism and Developmental Disorders, 43(7), 1517-1526.
doi:10.1007/s10803-012-1695-5
Vygotsky, L. (1978). Interaction between learning and development in mind in society. (pp 79-
91). Cambridge, MA: Harvard University Press.
Ward, S., & Jacobsen, K. (2014). Executive function situational awareness observation tool.
Perspectives on School-Based Issues, 15(4), 164. doi:10.1044/sbi15.4.164
Wetherby, A. M. (1986). The ontogeny of communicative functions in autism. Journal of Autism
and Developmental Disorders, 16, 295-316.
Wetherby, A. M., Cain, D. H., Yonclas, D. G., & Walker, V. G. (1988). Analysis of intentional
communication of normal children from the prelinguistic to the multiword stage, Journal
of Speech and Hearing Research, 240-252.
Wetherby, A. M., Prizant, B. M., & Hutchinson, T. (1998). Communicative, social/affective, and
symbolic profiles of young children with autism and pervasive developmental disorders.
American Journal of Speech-Language Pathology, 7, 79-91.
Wetherby, A. M., & Prutting, C. (1984). Profiles of communicative and cognitive-social abilities
in autistic children. Journal of Speech and Hearing Research, 27, 364-377.
Wiig, E. (2008). Social emotional evaluation (SEE). Austin, TX: PRO-ED.
Wiig, E., & Secord, W., (2014). Clinical evaluation of language fundamentals, (5th ed.). (CELF-
5, Metalinguistics). Bloomington, MN: Pearson.
Wiig, E., Secord, W., & Semel, E., (2020). Clinical evaluation of language fundamentals
preschool, (3rd ed.). (CELF Preschool-3). Bloomington, MN: Pearson.
Wiig, E., Semel, E., & Secord, W., (2013). Clinical evaluation of language fundamentals, (5th
ed.). (CELF-5). Bloomington, MN: Pearson.
Winner, M. G., (2007). Thinking about you thinking about me, (2nd ed.). San Jose, CA: Think
Social Publications.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 119
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendices

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 120
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix A
Classification System of Social Communication Disorder
The Diagnostic and Statistical Manual of Mental Health Disorders, Fifth Edition (DSM 5;
APA, 2013) sets forth a classification system for diagnostic criteria for social communication
disorder (SCD).
The DSM-5 states SCD is characterized by:
● Persistent difficulties in the social use of verbal and nonverbal communication as
manifested by all of the following:
○ Deficits in using communication for social purposes, such as greeting and
sharing information, in a manner that is appropriate for the social context.
○ Impairment of the ability to change communication to match context or the
needs of the listener, such as speaking differently in a classroom than on the
playground, talking differently to a child than to an adult, and avoiding use of
overly formal language.
○ Difficulties following rules for conversation and storytelling, such as taking
turns in conversation, rephrasing when misunderstood, and knowing how to use
verbal and nonverbal signals to regulate interaction.
○ Difficulties understanding what is not explicitly stated (e.g., making inferences)
and nonliteral or ambiguous meanings of language (e.g., idioms, humor,
metaphors, multiple meanings that depend on the context for interpretation).
● The deficits result in functional limitations in effective communication, social
participation, social relationships, academic achievement, or occupational performance,
individually or in combination.
● The onset of the symptoms is in the early developmental period (but deficits may not
become fully manifest until social communication demands exceed limited capacities).
● The symptoms are not attributable to another medical or neurological condition or to
low abilities in the domains or word structure and grammar, and are not better explained
by autism spectrum disorder, intellectual disability (intellectual developmental
disorder), global developmental delay, or another mental disorder.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 121
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix B
Core Characteristics of Social Communication Disorder (SCD)
Social communication behaviors such as eye contact, facial expressions, and body language are
influenced by sociocultural and individual factors (Curenton & Justice, 2004; Inglebret, Jones, &
Pavel, 2008). There is a wide range of acceptable norms within and across individuals, families,
and cultures.
Social Communication Disorder
Social communication disorder is characterized by difficulties with the use of verbal and
nonverbal language for social purposes. Primary difficulties are in social interaction, social
cognition, and pragmatics. Specific deficits are evident in the individual’s ability to:
● communicate for social purposes in ways that are appropriate for the particular social
context;
● change communication to match the context or needs of the listener;
● follow rules for conversation and storytelling;
● understand nonliterate or ambiguous language; and
● understand what is not explicitly stated.
This definition is consistent with the diagnostic criteria for Social (Pragmatic) Communication
Disorder detailed in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition
(DSM-5; American Psychiatric Association [APA], 2013). Social communication disorder
includes difficulty participating in social settings, developing relationships, achieving academic
and vocational success. Social communication disorder may be a distinct diagnosis or may co-
occur with other conditions, such as
● intellectual disability
● developmental disabilities;
● learning disabilities;
● spoken language disorders
● written language disorders
● attention-deficit/hyperactivity disorder (ADHD);
● traumatic brain injury (pediatric and adult)
● aphasia
● dementia, and
● right-hemisphere damage.
In the case of Autism Spectrum Disorder (ASD), social communication problems are a defining
feature, along with restricted, repetitive patterns of behavior. Therefore, social communication
disorder cannot be diagnosed in conjunction with ASD.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 122
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix C
Service Delivery Framework and Systems of Supports
Speech-language pathologists have a critical role in ensuring that the communication
needs of persons with autism are met across the lifespan (ASHA, 2016). Specific to school
settings, SLPs provide direct and indirect services for students with communication disorders
when these services and supports are needed to assist students in making progress in the general
curriculum or benefitting from the specially designed instruction specified in the Individualized
Education Program (IEP). SLPs address communication skills that promote:
● Joint attention (e.g., social orienting, shared attention, monitoring emotional
state);
● Social reciprocity (e.g., initiation, turn taking, response to others);
● Language and related cognitive skills (e.g., symbolic play, literacy skills,
executive functioning); and
● Behavior and emotional regulation (e.g., maintaining social engagement,
regulating emotional state/behavior), (ASHA, 2016).
Purpose of SLP Services for Students with Autism
The Individuals with Disabilities Education Act (IDEA, 2004) describes speech-
language therapy as a related service, but gives states discretion to consider speech-language
therapy as an instructional service. Specifically, the IDEA defines related services as
transportation and such developmental, corrective, and other supportive services necessary for
a child with a disability to benefit from special education. “In Texas, speech-language therapy
is considered an instructional service. This means it can be a stand-alone service as well as a
supportive service” (Texas Education Agency, 2009). When speech impairment is the only
disability, speech-language therapy is considered an instructional service. Speech-language
therapy services are considered a related or supportive service when there are one or more
other disabilities.
When speech impairment is the only disability, the purpose of speech-language therapy
is to provide specially designed instruction outlined in the IEP that the student needs in order
to make progress in the general curriculum.
When speech impairment is present with autism, the purpose of speech-language therapy
is a supportive service to help the student benefit from the specially designed instruction
provided in special education. Speech, language, and communication skills are embedded in
state standards - the Texas Essential Knowledge and Skills (TEKS) and core curriculum for
each grade level and course. Speech, language, and communication skills are typically most

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 123
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
closely aligned with English Language Arts and Reading TEKS and should be addressed on a
daily basis by the classroom teacher. The SLP should consider the assistance and support the
teacher might need in order to address the speech, language, and communication skills that are
part of the curriculum. As a supportive service, speech-language therapy is provided to
enhance the student’s academic and functional communication abilities for independence, self-
advocacy, and to make progress through the curriculum.
Service Delivery Framework
The service delivery models used by SLPs for students with autism and communication
disorders are individualized on the basis of each student’s communication needs and the
supportive services needed to help them benefit from his/her special education program. The
dimensions of service delivery include the type of service: direct or indirect, where the services
are provided, by whom, and on what schedule. The student’s IEP must specify the frequency,
location, and duration of special education and related/support services. In addition, the IEP
should delineate the direct and/or indirect SLP services needed to support the student in his/her
special education program.
The ARD Committee should consider the various service delivery models for speech-
language services while considering that research emphasizes the need for speech-language
services that are connected with functional and meaningful outcomes. The natural setting is
critical when addressing the communication needs of students with autism. Pull-out services
should only be considered when repeated opportunities do not occur in the natural learning
environment. The ARD Committee determines the service delivery model or combination of
service delivery models most likely to result in progress for the student, keeping in mind the
overarching purpose of improving functional communication and supporting the student in
making progress in the specially designed instruction provided through special education.
"'Children [with autism spectrum disorder] should receive specialized instruction in settings in
which ongoing interactions occur with typically developing children'. Individual skills should
be targeted to provide optimum benefit from interactions with typically developing children
and to provide the foundation for success in natural or inclusive settings" (ODDC, 2011).
● Direct Services: Direct services for students with autism refer to direct interaction
between the SLP and the student. The location of the service may occur in a variety of
settings. The critical points to consider are the provision of speech-language services in
a natural learning environment and within the context of social communication with
various communication partners.
○ Classroom-Based Model: The SLP provides direct and indirect services within the
context of the classroom to support the communication skills needed to benefit from
instruction. The classroom-based model typically consists of co-teaching
approaches such as team teaching, station teaching, or parallel teaching provided by
the classroom teacher and the SLP. It is best practice for the classroom teacher and
paraprofessionals to remain in the classroom with the SLP in order to maximize
opportunities for them to learn communication strategies.
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 124
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
○ Non-Academic Setting (electives-music, PE, art, lunch, extra-curricular).
○ Pull-Out or Pull-Aside Model: The SLP typically works with a small group outside
of the classroom, often in a speech therapy room or pulled to the side within the
classroom. The rationale for this model is that it may be more effective and efficient
than other models for teaching specific skills that benefit from repeated trials (e.g.,
articulation training, picture exchange for requesting), for teaching new behaviors
(e.g., initial use of an augmentative alternative communication (ACC) device), for
structuring conversational exchanges, for minimizing auditory and visual
distractions, and for privacy. Despite these considerations, exclusive use of the pull-
out model for students with autism is rarely appropriate because of the compelling
need to provide services and opportunities to use communication skills in naturally
occurring contexts and environments.
● Indirect Services: Research supports that the greatest effect on the generalization of
communication skills results from working with classroom personnel and parents
(National Research Council, 2001). Collaboration in educational settings provides
opportunities to develop more coordinated approaches to service, learn from one
another, and ultimately, improve intervention outcomes for students. Intervention
provided through a collaborative approach has been shown to be more beneficial to
most students in terms of carryover of skills, generalization of new skills, and more
consistent progress over time (Campbell, 1999). In addition, it allows the SLP
numerous opportunities to train classroom teachers successfully on how to differentiate
instruction, utilize a variety of learning modalities, and increase the teacher’s resource
library. By providing collaborative service delivery within the least restrictive
environment, there is potential to have greater collaborative partnerships while
increasing team-building opportunities with colleagues as well as the ability to gain
valuable knowledge of the curriculum and the expectations for students within the
classroom (Mount, 2014).
The SLP provides indirect services to support communication skills in the classroom
and across multiple contexts and environments at school, home, and in the community.
Collaborative/consultation services are provided directly to the classroom teacher/s or
other service providers on behalf of the student in order for the IEP to be implemented.
These services may include (a) observations of the student, peers, and instructors in the
learning environment, (b) discussions with teachers, paraprofessionals, and other
service providers regarding methodology, and (c) strategies, or written
recommendations provided to the classroom teacher or other service provider.
o Collaborative Consultation Model
o Monitor
o Consultation
o Curriculum Support
o Contextual Support
o Instructional Support
o Assistive technology/alternative communication (AT/AC) Support

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 125
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix D
Language Development Milestones to Consider
If language, communication, or unusual behavior is indicated as a concern, the Student Support
team members should review existing concerns with consideration of what may be typical or not
for the student’s age.
*It is important to note that children develop at their own rate and may not meet milestones until
the end of the age range.
Early Childhood
Age Expected Skill
Birth to 3 months
May recognize caregiver’s voice
Quiets or smiles when caregiver talks
Coos
Cries will change for different needs
6 months
Responds to changes in caregiver’s tone
Moves eyes towards direction of noise/sounds
Smiles
Makes eye contact
Coos and babbles (e.g., ba, me)
Giggles
3-9 months
Exhibits exploratory/sensorimotor play (touching, mouthing objects;
repetitive play) *will likely continue to age 2 and older
At 9 months may start to exhibit relational/functional play (using
objects as intended)
12 months
Responds to name
Turns and looks towards source of sound
Starts to comply with simple commands (e.g., Don’t touch)
Looks when adult points
Listens to short songs
Imitates simple speech sounds
Babbles strings of sounds
Gestures (showing, pointing)
Says 1 or 2 words
Plays simple turn taking games (peekaboo)
16 months
Should be producing single words

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 126
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
18-24 months
Points to body parts
Follows one part directions
Points to pictures as parent names them
Has developed joint attention by looking back and forth between
objects and caregivers
Responds to simple questions (e.g., Who’s that?)
Has at least 50 words by age 2
Asks simple questions (e.g., Where’s dada?)
Uses 2 word phrases (e.g., more juice)
Uses pronouns (e.g., I, me, you, my, mine) by 24 months
May cling to parent in new situations and have temper tantrums
Develops relational or functional play (objects used for their purpose
(e.g., stacking blocks)
Plays alongside others
May pretend with objects (e.g., pretend to feed doll with spoon)
24- 36 months
Follows 2 step directions
Engages in short dialogues
Uses some politeness markers (e.g. please)
Relates own experiences
May show defiance
Introduces and changes topics
Uses two to three word combinations
Talks about things that are not in the immediate context
Asks why
May engage in pretend or dramatic play with sequences
Uses some objects symbolically (e.g., block used as a phone)
3-4 years
Answers simple who, what, where questions
Understands words for relatives (e.g., brother, aunt)
Engages in longer dialogues and anticipates next turn
Sustains topics at least 20% of the time
Repairs conversation when not understood with repetition
Uses more pronouns (e.g., I, me, you, we, they)
Uses 4 word phrases
Talks about what happened during the day
Shows emergence of constructive play (e.g., making and building)
May show emergence of more social pretend play with parents,
siblings and peers
4-5 years
Develops a basic understanding of Theory of Mind
Follows classroom directions
Produces four to five word sentences
Keeps a conversation going when explaining how something works;
more difficulty sustaining dialogue
May abruptly change topic
TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 127
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
By 5, topics may be maintained for 5 turns although some are
repetitions
By 5, responds to requests for clarification most of the time
Talks in different ways based on listener and place
Shows development in playing simple turn taking games
Rough and tumble play may peak
Continued more elaborate development of pretend play through age 6
Early Childhood Indicators for Concern:
At 6 months:
Few or no smiles or engaging expressions
Limited or no eye contact
At 9 months:
Limited or no back and forth interpersonal play with sharing of sounds, facial expressions and
smiles
At 12 months:
Limited or no babbling
Does not respond or limited response to name
Limited or no gestures such as pointing, showing, waving
By 16 months:
Very limited use or no words
By 24 months:
No or limited use of spontaneous meaningful two word phrases
Limited vocabulary, for example, fewer than 50 words
Between 2 and 3 years of age, difficulties in:
Communication:
Impairment and/or delay in language development, especially comprehension
Unusual use of language
Limited response to name
Reduced sharing of positive affect (e.g., failure to smile socially, to share enjoyment, and to
Respond to the smiling of others)
Lack of coordination of nonverbal communication including eye gaze
Limited use of gestures
Unusual prosody and atypical intonation
Lack of communicative vocalizations with consonants (e.g., ma, ba)

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 128
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Social impairments:
Limitation in, or lack of imitation of, actions (e.g., clapping) or use of use of toys or other
objects
Limited spontaneous showing
Lack of interest in other children or odd approaches to other children
Limited recognition or responsiveness to other people's emotions
Limited variety of symbolic and imaginative play, especially social imagination (i.e., not
joining with Others in shared imaginary games)
May seem as if they are “in his/her own world”
Failure to initiate simple play with others or participate in early social games
Preference for solitary play
Atypical or limited responses to interactions from others
Impairment of interests, activities, and other behaviors:
Unusual sensory responses (with touch, sound, light, taste, smell)
Motor mannerisms (rocking, hand flapping, etc.)
Sudden shifts in emotional states
Excessive reactions to removal of objects
Excessive pattern of tantrums that consistently involve aggression
Strong preference for sameness/inability to cope with change
Repetitive play with toys (e.g., lining up objects; repetitive routines of knocking toys off,
spinning wheels with close visual inspection)
School Aged
Age/Grade Level Expected Skill
By the end of
Kindergarten or age
6
Follows 1-2 step directions in order
Listens to and understands stories read
Follows a simple conversation
Shows interest by starting a conversation
Talks about something they did or about an activity
Works collaboratively with others including taking turns
Shows development in playing rule games
By the end of the 1st
Grade or age 7
Stays on topic
Starts conversations
Takes turns in conversation
Repairs conversation with more information but still uses repetition
most often to repair
Follows agreed-upon rules for discussion such as listening to others,
and speaking when recognized
Retells stories in a way the listener understands

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 129
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
By the end of the 2nd
Grade or age 8
Stays on topic
Selects topics that are concrete
Uses eye contact within conversation
Begins and ends conversations
By the end of the 3rd
grade or age 9
Is able to be a part of a group discussion
Stays on topic for 6 turns
Shows a reduction in abrupt topic changes
Turn takes in conversation and makes eye contact
Is able to understand where communication breakdown occurs and
repairs by adding more background and contextual information
Summarizes a story
By the end of the 4th
grade or age 10
Listens for different purposes (e.g., learning, enjoying)
Uses language for varied purposes such as inquiring, expressing
opinions, and joking
Demonstrates understanding of some figurative language
Participates in group discussions
Presents information in a clear and organized manner
By the end of the 5th
grade or age 11
Participates in student-led discussions and considers suggestions from
others in the group
Plans speeches that are appropriate for the audience
Presents a speech with appropriate eye contact, gestures, and volume
Writes for a variety of purposes
Discusses what poetry means
Shows emerging abstract discussion in conversation
Adolescent Years Continues to develop vocabulary with abstract meaning (e.g.,
oppression)
Continues to develop figurative language including idioms and
metaphors
Shows the ability to take perspective of the writer
Begins to code switch among different groups (e.g., between
acquaintances and peers)
Capable of using slang to identify with peer group
Expected to be active listeners
Consider taking perspective and turn taking in conversation as
important skills for their peers
Expected to form expository texts and to rely on metalinguistic skills
(Reed, 2016).
Elementary Indicators for Concern:
A history significant for any/all of the early childhood indicators as well as red flags for any
age listed below.

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 130
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Difficulties with subtleties of communication including interpreting tone of voice, facial
expressions, or body language.
Delays or differences in several expected skills seen across settings.
*For older students, signs may become more apparent as the social and academic demands are
greater and exceed the child’s ability to adapt (Haute Autorité de la Santé, 2018).
Secondary Ages/Adolescent Indicators for Concern:
A history significant for any/all of the early childhood indicators, anxiety in social situations,
as well as those listed below.
Delays or differences in several expected skills seen across settings.
Persistent difficulties in executive functioning and theory of mind. An older individual with
autism may continue to struggle with empathy.
Continued difficulties with social interactions, cognitive flexibility, and atypical
communication, as well as interpreting non-literal information (e.g., jokes, sarcasm).
*Signs may become more apparent as the social and academic demands are greater and exceed
the child’s ability to adapt (Haute Autorité de la Santé, 2018).
Possible Indicators for Concern at Any Age:
Loss or regression of previously acquired skills
Avoidance of eye contact (cultural norms should be considered)
Ongoing pattern of preference to be alone
Difficulty understanding how others are feeling
Delayed development of language
Use of echolalia
Ongoing resistance to change
Excessive restrictive interests
Repetitive behaviors such as flapping and rocking
Unusual responses to sensory input (sounds, smells, tastes, lights, colors)

TSHA: Autism Companion, Language Disorder Determination Guidelines, 2021 131
The SI Disability Determination Guidelines have been prepared by the Texas Speech-Language-Hearing Association (TSHA).
Please note that they are guidelines. TSHA has no regulatory or administrative authority and there is no requirement to use the
guidelines. They are provided by TSHA as a public service to enhance the quality of SLP services in public schools.
Appendix E
