
Washington Apple Health (Medicaid)
ProviderOne
billing and
resource guide
June 2024

2 | PROVIDERONE BILLING AND RESOURCE GUIDE
Table of contents
About this guide ................................................................................................................................ 6
Current updates ............................................................................................................................. 6
Introduction ......................................................................................................................................... 7
Purpose ............................................................................................................................................. 7
Guide topics .................................................................................................................................... 8
Apple Health (Medicaid) overview ............................................................................................ 9
Apple Health ................................................................................................................................... 9
Washington Apple Health clients .......................................................................................... 9
Apple Health comparison ...................................................................................................... 10
Apple Health compared to Medicare ............................................................................... 10
Apple Health clients identified ............................................................................................ 10
Apple Health clients as consumers of healthcare services ..................................... 11
Provider enrollment ...................................................................................................................... 12
Benefits for enrolled providers ............................................................................................ 12
Enrolling as an Apple Health provider ............................................................................. 12
Requirements to enroll ........................................................................................................... 12
Eligible provider types ............................................................................................................. 13
Providers required to enroll .................................................................................................. 13
Provider enrollment policies................................................................................................. 13
Policies regarding documentation and paper claims ................................................ 14
Out-of-state bordering cities ............................................................................................... 14
Resources ...................................................................................................................................... 15
Important contacts.................................................................................................................... 18
Eligibility, Benefit Service Packages, and service limits ................................................ 19
Getting paid for eligible Apple Health services ........................................................... 19
Verifying Apple Health coverage ....................................................................................... 19
Verifying primary payer and program type ................................................................... 23
Client with managed care ...................................................................................................... 25
Integrated managed care ....................................................................................................... 25
Health Home program ............................................................................................................ 26
Behavioral health services ..................................................................................................... 27
State-only programs ................................................................................................................ 27
Primary Care Case Management (PCCM) ....................................................................... 27
Clients with Medicare .............................................................................................................. 28
Commercial insurance, Medicare Part C/D, or military benefits .......................... 28
3 | PROVIDERONE BILLING AND RESOURCE GUIDE
Restricted client information ................................................................................................ 31
Hospice services ......................................................................................................................... 31
Developmental Disabilities Administration (DDA) ..................................................... 32
Children with Special Health Care Needs (CSHCN).................................................... 32
Medicaid suspension ................................................................................................................ 32
Benefit Service Package .......................................................................................................... 33
Spenddown ................................................................................................................................... 33
Spenddown FAQ ........................................................................................................................ 33
Medical records for clients in Foster Care ...................................................................... 34
Covered services and prior authorization....................................................................... 38
Procedure codes and fee schedules .................................................................................. 39
Covered procedures ................................................................................................................. 39
Prior authorization requirement ......................................................................................... 40
Claim payments – professional services .......................................................................... 41
Claim payments – institutional services .......................................................................... 42
Claim payments – inpatient hospital services ............................................................... 42
Provider preventable conditions (PPCs) .......................................................................... 42
Client service limits ................................................................................................................... 44
Submitting fee for service claims ............................................................................................ 48
Timely and accurate payments ............................................................................................ 48
Claim submission method ..................................................................................................... 49
Claim backup ............................................................................................................................... 49
Submitting new claims and backup .................................................................................. 51
Direct Data Entry (DDE) .......................................................................................................... 52
Submitting backup for a DDE claim .................................................................................. 58
Submitting backup through a clearinghouse ............................................................... 61
Resolving DDE claim errors ................................................................................................... 61
Entering commercial insurance information ................................................................. 62
Saving a DDE claim ................................................................................................................... 64
Submitting online batch claims .......................................................................................... 65
Special Claim Indicators (SCI)............................................................................................... 66
Submitting Medicare crossover claims ............................................................................ 67
Overview of Medicare crossover process ....................................................................... 68
Medicare Part B professional services .............................................................................. 69
Part B only (no Part A), or Part A exhausted prior to stay ...................................... 70
Medicare begins during hospital stay, or Part A exhausts during stay............. 71
Medicare Advantage plans (Part C) ................................................................................... 72

4 | PROVIDERONE BILLING AND RESOURCE GUIDE
QMB – Medicare Only clients ............................................................................................... 74
Claim status .................................................................................................................................. 76
Timeliness ...................................................................................................................................... 77
Adjusting, resubmitting, or voiding a claim .................................................................. 77
Adjusting or Voiding DDE claims ....................................................................................... 80
Resubmitting denied or voided DDE claims .................................................................. 82
Claim templates .......................................................................................................................... 83
Submitting a template claim or batch of template claims ..................................... 86
The remittance advice .................................................................................................................. 89
Understanding claim status .................................................................................................. 89
Retrieving the RA ....................................................................................................................... 89
Adjustment types ....................................................................................................................... 91
Reviewing paid claims ............................................................................................................. 95
Reviewing denied claims ........................................................................................................ 96
Reviewing adjusted claims .................................................................................................... 97
Reviewing in process claims ................................................................................................. 98
Reviewing EOB codes ............................................................................................................... 98
Requesting prior authorization ................................................................................................ 99
The authorization intake process ....................................................................................... 99
DDE prior authorization intake process ........................................................................ 100
General Information for Authorization form, HCA 13-835 ................................... 100
Submitting backup for DDE authorizations ................................................................. 100
Submitting backup for faxed authorizations (no x-rays) ...................................... 101
Checking PA status ................................................................................................................. 101
Additional documentation requests ............................................................................... 102
Cover sheet tips ........................................................................................................................ 103
For more information ............................................................................................................ 103
Appendix A: Verify eligibility with IVR................................................................................ 105
Appendix B: Verify eligibility with magnetic card readers ........................................ 106
Appendix C: Managed care organizations ........................................................................ 107
Appendix D: Casualty and health insurance claims ...................................................... 108
Appendix E: Benefit service packages ................................................................................. 109
ACES program codes .............................................................................................................. 112
Appendix F: Prior authorization process ........................................................................... 118
Appendix G: Authorization status using the IVR ........................................................... 119
Checking authorization status using Interactive Voice Response (IVR) ......... 119
Checking authorization status using ProviderOne ................................................... 120

5 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix H: Cover sheets for backup documentation ............................................... 122
Appendix I: Taxonomy and ProviderOne .......................................................................... 124
Appendix J: Medicare crossover claim payment methodology .............................. 125
Professional services .............................................................................................................. 125
Institutional services ............................................................................................................... 126
Appendix K: Checking claim status using the IVR ......................................................... 127
Appendix L: Checking warrants using the IVR ................................................................ 129

6 | PROVIDERONE BILLING AND RESOURCE GUIDE
About this guide
This guide supersedes all previously published agency ProviderOne Billing and
Resource Guides.
Current updates
Reason for change
Page number
Subject
Change
New program
addition – Appendix
E
109, 112, and
115
Apple Health
Expansion (AHE)
AHE description
addition and 2 new
ACES program
codes
HCA accepts only electronic claims for Apple Health (Medicaid) services, except
under limited circumstances. Providers may seek approval to submit paper claims
if they are in a temporary or long-term situation outside of their control that
precludes submission of claims electronically. Go to the ProviderOne Billing and
Resource Guide webpage and go to paperless billing at HCA for more
information.

7 | PROVIDERONE BILLING AND RESOURCE GUIDE
Introduction
This guide provides a step-by-step resource to help providers and billing staff
understand the processes of ensuring clients are eligible for services and to
receive timely and accurate payments for covered services.
Disclaimer
A contract, known as the Core Provider Agreement (CPA), governs the
relationship between HCA and Apple Health (Medicaid) providers. The CPA’s
terms and conditions incorporate federal laws, rules and regulations, state law,
agency rules and regulations, and agency program policies, provider notices, and
provider guides, including this guide. Providers must submit a claim in
accordance with agency rules, policies, provider notices, and provider billing
guides in effect for the date of service.
HCA does not assume responsibility for informing providers of national coding
rules. ProviderOne will deny claims billed in conflict with national coding rules.
Consult the appropriate coding resources.
Purpose
This guide serves as a resource for providers and billing staff whose duties are to:
• Maintain provider records.
• Schedule client appointments or check in patients on the day they receive
services.
• Submit fee for service (FFS) claims to HCA.
• Post and reconcile payments.
This guide assumes familiarity with standard medical billing practices and coding.
Note: This guide does not include billing information for the
pharmacy point-of-sale (POS) system. See the Pharmacy
information webpage for more information on the POS system
or see the Prescription Drug Program provider guide for more
information. DSHS social service billers should refer to the
ProviderOne for social services webpage for training resources.

8 | PROVIDERONE BILLING AND RESOURCE GUIDE
Guide topics
This guide consists of the following six sections:
Apple Health (Medicaid) overview
This section explains the Apple Health (Medicaid) programs provided by HCA,
how Apple Health compares to other payers, how Medicaid differs from
Medicare, how to identify Apple Health clients, the ProviderOne services card,
requirements for becoming an Apple Health provider, and links to important
policy documents and resources.
Provider enrollment
This section is for general information about becoming an Apple Health provider.
Visit the Enroll as a provider webpage for more information.
Client eligibility, Benefit Service Packages, and coverage limits
This section explains how to determine if a client is eligible for Apple Health
(Medicaid) services using ProviderOne, if the service you plan to deliver is
covered under their Benefit Service Package (BSP), and when prior authorization
is needed.
This section also explains how to determine if a client:
• Has enrolled in a managed care plan.
• Has any restriction to a select number of health care providers.
• Has a spenddown balance that may affect eligibility.
Submitting fee for service (FFS) claims
This section prepares you to submit fee for service claims using the ProviderOne
Direct Data Entry (DDE) feature, submit electronic backup documentation, check
on the progress of a claim, and process Medicare crossover claims. This section
also outlines how to resolve errors, submit adjustments, resubmit denied claims,
or void a paid claim.
The Remittance Advice (RA)
This section explains how to obtain your Remittance Advice (RA), determine
which claims were paid or denied, review claims still in process, and determine
the reason for a claim denial.
Requesting prior authorization
This section explains how to determine if a procedure requires authorization and
what steps are needed to complete that process.

9 | PROVIDERONE BILLING AND RESOURCE GUIDE
Apple Health (Medicaid) overview
Apple Health
Medical assistance is the general name for Washington Apple Health programs
administered by the Health Care Authority (HCA).
Washington Apple Health includes Medicaid, mental health programs, chemical
dependency and prevention treatment programs, the Children’s Health Insurance
Program (CHIP), family planning programs, and other state-funded children’s
healthcare programs. Medicaid is the federal entitlement program financed and
operated jointly by the states and the federal government.
HCA provides healthcare coverage for low-income residents who meet certain
eligibility requirements. Examples of these requirements include age, pregnancy,
disability, and blindness. Special rules exist for those living in a nursing home or
for those who receive home and community-based services.
Clients receive healthcare services either through enrollment in a managed care
program or on a fee for service basis. For managed care, the agency contracts
with licensed health insurance carriers to provide a defined set of services to
enrolled members. Fee for service care is delivered by licensed or certified health
care providers who have a contract with the agency and receive payment through
ProviderOne.
Washington Apple Health clients
Washington’s Apple Health programs provide healthcare coverage for our most
vulnerable residents. Approximately 1.5 million Washington residents, nearly two-
thirds of them children, depend on Apple Health (Medicaid) programs for their
healthcare.
Apple Health covers one in three children living in Washington State including:
• Children enrolled in foster care.
• Children of working parents unable to afford health care coverage.
• Disabled children
Other clients also include:
• Nursing home residents
• Elderly or disabled individuals
• Low-income pregnant women
The Health Benefit Exchange (HBE), the HCA Medical Eligibility Determination
Services (MEDS), as well as the Department of Social and Health Services
determine eligibility for medical assistance depending on the client’s
circumstances.

10 | PROVIDERONE BILLING AND RESOURCE GUIDE
Apple Health comparison
Washington State has several programs dedicated to providing healthcare
coverage to low-income residents. Washington Apple Health is the largest single
source for this coverage. However, some Apple Health programs have limited
benefits compared to commercial carriers. See Appendix E for more details.
In many ways, Apple Health is like other payers. There are some distinct
differences between Apple Health and commercial insurance plans and Medicare.
These differences include:
Specific rules a contracted provider must follow regarding billing a client. See
WAC 182-502-0160 and form 13-879 for details.
Apple Health is almost always the payer of last resort, which means Medicare and
commercial private insurance companies are billed first. For more information on
general conditions of payment see WAC 182-502-0100.
Apple Health compared to Medicare
Apple Health and Medicare are very different programs. Medicare is an
entitlement program funded entirely at the federal level. It is a health insurance
program for people 65 or older, people 65 and younger with certain disabilities,
and people of all ages with end stage renal disease.
The Medicare Program provides:
• Medicare Part A, which covers inpatient hospital services.
• Medicare Part B, which covers professional, and vendor services.
• Medicare Part C, which is a managed care version of Medicare, also called a
Medicare Advantage Plan, and offered through private insurance companies.
• Medicare Part D, which covers prescription drugs.
Apple Health (Medicaid) is a needs-based program with eligibility determined by
income and covers a wider range of healthcare services than Medicare (i.e.,
dental). Some individuals are eligible for both Medicaid and Medicare. These
clients are referred to as “dual-eligible” clients.
For more information on Medicare, you can find extensive material at the Centers
for Medicare and Medicaid Services (CMS) website.
Apple Health clients identified
Each Apple Health client receives a plastic services card. The services card is
permanent, and each eligible family member receives a separate card with a
client identifier assigned for each client. The card contains only the following
information about the client:
• First name
• Last name
• ProviderOne client identification number (9 digits followed by WA)
• Date card was issued.
Using the ProviderOne client ID displayed on the front of the card is one way to
access a client’s eligibility information. The card also features a magnetic strip on

11 | PROVIDERONE BILLING AND RESOURCE GUIDE
the back and providers may use a magnetic swipe card reader to obtain the most
current eligibility information. There are many other ways to verify a client’s
eligibility if you do not have access to the client’s services card. See the eligibility,
benefit service packages, and coverage limits section for more information.
Example of a services card:
Apple Health clients as consumers of healthcare
services
The agency encourages Medicaid clients to be responsible consumers of
healthcare services. New clients receive information to use when obtaining
services that cover topics such as:
• Verifying if a provider is contracted to bill Apple Health before obtaining
services from a doctor, dentist, clinic, pharmacy, or other provider. Non-
contracted providers can bill clients directly.
• How to help the healthcare provider by bringing the services card to all
appointments. Clients should always carry the services card with them in case
of emergencies.
• Being courteous about appointments and call their provider’s office if an
appointment will be missed.
• Informing their provider if they have commercial or other medical insurance
besides Apple Health.

12 | PROVIDERONE BILLING AND RESOURCE GUIDE
Provider enrollment
Benefits for enrolled providers
Some benefits for Apple Health providers include:
• ProviderOne pays claims promptly when billed according to agency rules and
regulations.
• Providers may determine how many Apple Health patients to allow according
to their business needs.
• ProviderOne offers Electronic Funds Transfer (EFT) payments as a convenience.
• Enhanced payments are available for dental providers who provide Access to
Baby and Child Dentistry (ABCD) services.
• The satisfaction that Washington’s most vulnerable population is receiving
healthcare services.
Enrolling as an Apple Health provider
You can enroll as an Apple Health provider using the electronic enrollment
option in the ProviderOne system. See the Enroll as a provider webpage for more
information.
For enrollment questions contact the Provider Enrollment office at 1-800-562-
3022, extension 16137.
Requirements to enroll
To enroll as a provider with the agency, a healthcare professional, healthcare
entity, supplier or contractor of a service must, on the date of application:
• Be licensed, certified, accredited, or registered according to Washington State
laws and rules.
• Meet the conditions in Chapter 182-502 WAC and other chapters regulating
the specific type of provider, program, and/or service.
• To enroll, an eligible provider must sign a Core Provider Agreement (CPA)
with the agency according to WAC 182-502-0005.
• Enrollment of a provider applicant is effective no earlier than the date of
approval of the provider application.
• The agency does not pay for services provided to clients during the core
provider agreement (CPA) application process, regardless of whether the CPA
is later approved or denied.
Note: There is an application fee for institutional provider
enrollment applications. This fee does not apply to providers
enrolled with Apple Health prior to June 1, 2016. The provider
enrollment application fee is only required for provider types in
the institutional setting. Providers that are required to pay the
application fee will receive notification of the cost by mail.

13 | PROVIDERONE BILLING AND RESOURCE GUIDE
For additional information about federal and state regulations
related to the provider enrollment application fee, see 42 CFR
455, Subpart E, 42 CFR 455.460 and WAC 182-502-0010 (k).
For questions related to the enrollment application fee, email
providerenrollment@hca.wa.gov or call 800-562-3022 and use
extension 16137.
Eligible provider types
There are specific rules on who may enroll:
• All performing providers of services to an Apple Health client must be
enrolled under the billing provider’s CPA.
• The agency does not enroll licensed or unlicensed practitioners not specifically
addressed in WAC 182-502-0002, and ineligible providers as listed in WAC
182-502-0003.
• For a list of providers who are eligible to enroll with Apple Health, see WAC
182-502-0002.
• All dental servicing providers must be enrolled in ProviderOne under the
dental billing provider NPI (effective July 1, 2014).
Providers required to enroll
See 42 CFR 455.410:
• Any referring, ordering, or prescribing provider must be enrolled with HCA as
a fee for service provider.
• The National Provider Identifier (NPI) number of any referring, ordering, or
prescribing provider must be listed on any claims for services, supplies, tests,
etc. ordered, referred, or prescribed by that provider.
• To comply with the National Uniform Billing Committee (NUBC) guidelines all
NPI numbers of attending, operating, and “other” providers must be reported
on institutional claims.
• All providers reported on the institutional claim must be enrolled as a
Washington State Medicaid Provider.
Provider enrollment policies
Specific policies regarding provider enrollment include:
• You must notify HCA in writing within seven calendar days of ownership or
control changes of any kind (see WAC 182-502-0018).
• You may voluntarily terminate your provider agreement by contacting
Provider Enrollment at ProviderEnrollm[email protected] (see WAC 182-502-
0040).
• In some situations, the agency may immediately terminate your
enrollment/CPA (see WAC 182-502-0030).
• There are a few exceptions to the enrollment effective date (see WAC 182-
502-0005).

14 | PROVIDERONE BILLING AND RESOURCE GUIDE
• See the full text of Chapter 182-502 WAC for additional provider enrollment
information.
• To continue to provide services for eligible clients and be paid for services, a
provider must:
o Provide all services without discriminating on the grounds of race, creed,
color, age, sex, sexual orientation, religion, national origin, marital status,
the presence of any sensory, mental, or physical handicap, or the use of a
trained dog guide or service animal by a person with a disability.
o Provide all services according to federal and state laws and rules, Medicaid
agency billing instructions, numbered memoranda issued by the agency,
and other written directives from the agency.
o See the full text of Chapter 182-502-0016 for additional detail on these
requirements.
Policies regarding documentation and paper claims
Specific policies regarding documentation and paper claims include:
• The complete list of Healthcare Record Requirements can be found in WAC
182-502-0020.
• Charts and records must be available to the agency, its contractors or
designees, and the US Department of Health and Human Services upon
request for six years from the date of service, or longer if required specifically
by federal or state law regulation.
• As of October 1, 2016, the agency will only accept electronic claims for Apple
Health (Medicaid) services, except under limited circumstances. Providers may
seek approval to submit paper claims if they are in a temporary or long-term
situation outside of their control that precludes submission of claims
electronically. See the ProviderOne Billing and Resource Guide webpage for
more information.
Out-of-state bordering cities
WAC 182-501-0175
All eligible Washington residents may receive medical care in a recognized out-
of-state bordering city on the same basis as in-state care. The only Washington
recognized bordering cities are:
• Idaho: Coeur d’Alene, Lewiston, Priest River, Moscow, and Sandpoint
• Oregon: Astoria, Hermiston, Hood River, Milton-Freewater, Portland, Rainier,
and The Dalles
Note: Washington Apple Health does not cover services
provided outside Washington under the Involuntary Treatment
Act (ITA) (Chapter 71.05 RCW and Chapter 388-865 WAC),
including designated bordering cities.

15 | PROVIDERONE BILLING AND RESOURCE GUIDE
Out-of-state providers must have a contract with HCA for payment of out-of-
state emergency services and may request retroactive enrollment when
necessary.
For nonemergency services, use the Out of State Medical Services Request form,
HCA 13-787.
Resources
Topic
Contact or link
Where can I find provider guides
that explain program-specific
billing guidelines, coverage, and
limitations?
See the Provider billing guides and fee
schedules webpage.
Where can I find fee schedules?
See the Provider billing guides and fee
schedules webpage.
Where can I find hospital rates?
See the Hospital reimbursement webpage.
Who do I contact if I have
questions about payments,
denials, general questions
regarding claims processing, or
managed care plans?
The Medical Assistance Customer Service
Center (MACSC) provider line is available
Monday through Friday 7 a.m. to 4:30 p.m.
daily (claims line open 8 a.m. – noon, closed
noon – 1:30 p.m., and open 1:30 to 3:30 p.m.).
The interactive voice response (IVR) phone
system is available 24 hours a day, 7 days a
week.
• 1-800-562-3022
• Email MACSC using the Contact Us link.
Note: Providers may use HCA's toll free lines
for questions regarding its programs;
however, HCA's response is based solely on
the information provided to the
representative at the time of the call or
inquiry, and in no way exempts a provider
from following the rules and regulations that
govern HCA's programs (see Chapter 182-502
WAC).
Where can I get information
about becoming an Apple
Health provider, submitting a
change of address, submitting a
change of ownership, or to ask
questions about the status of an
application?
See the Enroll as a provider webpage.
Provider enrollment hours are 7 a.m. to 4:30
p.m. (closed noon to 1 p.m.) Tuesday and
Thursday.
Closed Mondays, Wednesdays, and Fridays.
• 1-800-562-3022 ext. 16137
• Fax: 360-725-2144

16 | PROVIDERONE BILLING AND RESOURCE GUIDE
Topic
Contact or link
• Email providerenrollme[email protected]
Where can I find information
about HCA’s current rule making
activity?
See HCA’s Rulemaking webpage.
Where do I find all Washington
Administrative Codes (WAC)?
See the Washington Administrative Code
(WAC) webpage.
What is the Apple Health web
address?
See the Washington Apple Health (Medicaid)
coverage webpage.
Where can I find the Washington
State Confidentiality Toolkit for
Providers?
See the Toolkit and webpage announcement.
Where can I ask questions about
private insurance or third-party
liability?
For private insurance claims, submit a Contact
us email. Choose Medical Provider and use
Private Commercial Insurance on the Select
Topic dropdown.
For casualty-related claims or third-party
liability, call the toll free number at 1-800-
562-3022 M – F from 8 a.m. – 4:30 p.m.
Where do I ask questions about
nonemergency transportation
services?
HCA provides access to nonemergency
transportation services for clients who need
help with transportation to and from their
healthcare appointments.
For more information, see the Transportation
services (nonemergency) webpage or email
HCA Transportation.
Where do I ask questions about
interpreter services?
For spoken language access providers (LAP),
register through Universal Language. Visit the
spoken language access provider webpage for
more details.
For sign language interpretation, visit the sign
language interpretation webpage for more
details.
E-mail: HCA Interpreter Services
Where do I obtain HCA’s forms?
See HCA’s forms and publications webpage.
Where can I find locations of
DSHS Community Service Offices
(CSO)?
For more information, see the Online
Community Services Office (CSO) webpage on
the DSHS website.

17 | PROVIDERONE BILLING AND RESOURCE GUIDE
Topic
Contact or link
Where do I find locations of
DSHS Home and Community
Services (HCS)?
For more information, see the Home and
Community Services Information for
Professionals webpage on the DSHS website.
How do I find out what is
included in the nursing facility
per diem or general rate?
Contact the DSHS Aging and Long Term
Support Administration (ALTSA) website or
call 1-800-422-3263.
How do I request authorization?
Visit the Prior authorization webpage for
complete step by step instructions on
entering prior authorization requests through
the direct data entry feature of ProviderOne.
Call 1-800-562-3022 using an extension listed
below:
• Durable medical equipment and supplies,
prosthetics and orthotics, and oxygen:
15466
• Dental: 15468
• Pharmacy: 15483
• Medical – Surgical: 52018
• All other medical services/enteral nutrition:
15471
See the program specific billing guide located
on the provider billing guides and fee
schedules webpage for information on
requesting authorization. See Appendix F for
instructions on completing the General
Authorization Request form, HCA 13-835.
• Authorization forms can only be sent by
fax to 1-866-668-1214
If you are faxing supporting documentation
without the original authorization request
form, a cover sheet is required. See Appendix
H for more information on cover sheets.
Where can I access provider
training materials?
See the ProviderOne resources webpage.
How do I submit backup
documentation for electronic
claims?
Heath Care Authority
RE: Cover sheets and backup documentation
PO Box 45535
Olympia, WA 98504-5535
Backup documentation must include a cover
sheet as the first page and can be faxed to 1-
866-668-1214.
See Appendix H for more information on
cover sheets.

18 | PROVIDERONE BILLING AND RESOURCE GUIDE
Important contacts
Section
Contact
Disability Insurance
1-800-562-6074
Fraud Hotline
1-833-794-2345
Home Health/Plan of Treatment
1-360-586-1471
Foster Care
1-800-562-3022 ext. 15480
Hospice Notification
1-360-725-1965 (fax only)
Medical Eligibility Determination
Services (MEDS)
1-800-562-3022
Medicare Unit Fax Line
1-360-664-2186
Patient Review and Coordination
1-800-562-3022 ext. 15606
TAKE CHARGE questions
1-800-562-3022
Telecommunication Relay Services
(TRS)
711
Managed care plan managers
HIPAA help desk

19 | PROVIDERONE BILLING AND RESOURCE GUIDE
Eligibility, Benefit Service Packages, and
service limits
Getting paid for eligible Apple Health services
HCA denies many claims because the client was not eligible for Apple Health on
the date of service. To prevent billing denials, always check the client’s eligibility
and confirm plan enrollment prior to providing any services. Checking eligibility
and coverage takes less time and effort than resolving a denied claim.
Some procedures may require the satisfaction of certain conditions before
reimbursement for a service, such as determining whether a service requires prior
authorization. Researching these requirements before providing a service will
help prevent denied claims.
If the service is not covered and the client chooses to receive and pay for a
specific service, providers may be able to bill the client. See the billing a client
WAC 182-502-0160 and Agreement to Pay for Healthcare Services form 13-879
for rules on billing a client. For training materials on this topic, see our webinars
page.
This section shows how to determine:
• If the client has Apple Health.
• If a service is covered under the client’s Benefit Service Package.
• If the client is enrolled in a managed care plan or if they are fee for service.
• If a client has commercial insurance as their primary payer.
• When prior authorization is required.
• When and if a waiver can be used to bill a client.
• If the client has a spenddown balance that may affect eligibility.
• Any special limitations or restrictions.
• If the client has reached their maximum for services with limitations.
Disclaimer
A contract, known as the Core Provider Agreement (CPA), governs the
relationship between HCA and Washington Apple Health providers. The CPA’s
terms and conditions incorporate federal laws, rules and regulations, state law,
HCA’s rules and regulations, and HCA’s program policies, provider notices, and
provider guides, including this guide. Providers must submit a claim in
accordance with HCA’s rules, policies, provider notices, and provider guides in
effect at the time they provided the service.
Verifying Apple Health coverage
It is your responsibility to verify whether the client has Apple Health coverage for
the date of service, and if so, to check the limitations of the client’s medical
program. Verification helps prevent providing a service that the agency will not
pay for. When making an appointment for a client it is important to check

20 | PROVIDERONE BILLING AND RESOURCE GUIDE
eligibility to determine if the client needs interpreter services for the
appointment.
There are many methods to check client eligibility. Most of these methods involve
using the ProviderOne system. Use ProviderOne to submit an eligibility inquiry
using one of these methods:
• Search for eligibility information using ProviderOne.
• Submit an electronic individual or batch 270/271 inquiry to ProviderOne.
• Swipe the client services card using a magnetic card reader (see Appendix B).
• Use a medical eligibility vendor to access information on your behalf (see
Appendix B).
• Call the interactive ProviderOne voice response (IVR) (see Appendix A).
• Submit a request through the Contact Us email link.
• If the client’s appointment is within 48 hours, call a customer service
representative at 1-800-562-3022.
To search for eligibility information in ProviderOne, log into ProviderOne and
select the EXT Provider Eligibility Checker or EXT Provider Super User profile to
verify client’s eligibility for Apple Health (Medicaid):
Select the Benefit Inquiry hyperlink from the provider portal home page menu:
Search by any one of the many combinations available. The inquiry start date will
default to the current date. When searching for other dates of service, make sure
to enter only the current date or previous dates as ProviderOne cannot search

21 | PROVIDERONE BILLING AND RESOURCE GUIDE
future eligibility. Information displayed is only valid for the inquiry start and end
date. A client’s eligibility segment may change if a different date of service is
used. The maximum date span for an eligibility inquiry is 2 years.
Note: If you aren’t sure how to spell the client’s name,
ProviderOne allows a client eligibility search by using the first 5
letters of the last name and the first 3 letters of the first name.
However, if using the name search feature, the date of birth or
SSN is required.
If your search was successful, the system then displays the selection criteria you
entered, followed by the demographic information. If the demographic
information is blank, review the System Response Information to see why
ProviderOne could not find the client.
Basic client detail is returned including client ID, gender, and DOB. The eligibility
information can be printed out using the Printer Friendly Version link in blue.

22 | PROVIDERONE BILLING AND RESOURCE GUIDE
Below the Client Demographic Information, successful client searches will display
the Client Eligibility Spans with detail on what kind of coverage the client has
during the date span you searched:
Each column is described below:
• Insurance type code – the type of coverage for the client
• Recipient aid category (RAC)
• Name of Benefit service package (BSP) acronym
• Eligibility start date - start date for this eligibility segment.
• Eligibility end date - if there is no end date, ProviderOne defaults to
12/31/2999.
• Review end date - the date a client may terminate if they don’t renew their
coverage (renewal notices are sent the month before). If there is no end date,
it does not apply to their coverage type.
• ACES coverage group - code assigned when eligibility is determined.
• ACES case number – case number assigned to client.
• Retro eligibility - this reflects the three calendar months before the month
the client applied for services (WAC 182-502-0150).
• Delayed certification - in some cases the determination of eligibility is
delayed. If approved, the delayed certification date will be displayed in this
location. The agency can accept claims up to one year past this date (WAC
182-502-0150).
Note: Some providers may need to use the Recipient aid
category (RAC) for specific billing purposes or to further
determine a client’s eligibility in a program. Please reference the
applicable program specific provider guide for further details.
If the eligibility inquiry is unsuccessful, the system will display an error message
under system response information:

23 | PROVIDERONE BILLING AND RESOURCE GUIDE
Note: If your search returns an error, check how you entered the
information and correct as needed.
Pitfalls:
• Relying on eligibility information obtained before the date of service. HCA
recommends that providers always verify eligibility the day the service occurs.
• Failing to verify the identity of the cardholder. Apple Health coverage is not
transferable. If you suspect that a client has presented a services card
belonging to someone else, request to see a photo ID or another form of
identification.
Verifying primary payer and program type
Apple Health is almost always the payer of last resort (for exceptions, see WAC
182-502-0100). The agency will not pay claims as primary if there is another payer
(such as Medicare or commercial insurance). Most Apple Health clients will be in
a managed care plan where the agency pays a monthly premium to that plan for
the client’s medical needs. If there is no managed care segment on the client’s
file, they are considered fee for service clients and all billing will be submitted
directly to ProviderOne, or through the agency’s pharmacy POS (point of sale)
system for prescription benefits.
Note: Effective for claims with dates of service on and after
January 1, 2017, the Health Care Authority changed the process
for managing Apple Health (Medicaid) benefits for clients with
other primary health insurance. See the Apple Health Medicaid
provider alert dated 11/16/2016 10:09 AM PST.
• Providers billing for fee for service clients with a private commercial insurance,
bill ProviderOne as secondary.
• Providers do not have to be part of the client’s MCO network to bill for
secondary coverage. However, to bill the client’s MCO, providers must follow
the MCO’s billing requirements.

24 | PROVIDERONE BILLING AND RESOURCE GUIDE
• After billing a client’s primary health insurance for a covered service, providers
must then bill the MCO or the MCO’s pharmacy benefit manager (PBM) to
coordinate benefits for copays, deductibles, or other remaining balances.
Providers must not bill copays, deductibles, or other remaining balances to
the client.
• If a provider bills the client’s MCO as a secondary payer, the MCO does not
require prior authorization. However, if the client’s primary health insurance
does not cover the service, the provider must follow the Apple Health MCO
requirements, including prior authorization if necessary.
To avoid turning away an individual at check-in, determine the client’s primary
payer when making an appointment. Some of the reasons a provider might turn
clients away include:
• The provider does not accept their managed care plan.
• The provider is not an enrolled Medicare provider.
• The provider is not an enrolled provider with their commercial private
insurance.
Client eligibility may change over time, and the primary payer may change as
well. For example, a client may enroll in an Apple Health managed care plan.
Nursing home providers must review the Institutional Award Letter. The award
letter explains client income and participation amount, medical care eligibility,
effective date for care, care level, and other information.
This does not apply to clients with Alternative benefits plan (ABP) benefits, as this
population has nursing home coverage without cost sharing, so the institutional
award letter is unnecessary.
All other providers that are not nursing homes can follow the instructions below.
This section covers the following:
• How to determine the client is enrolled in an Apple Health managed care
plan.
• How to determine the client is eligible for behavioral health services (mental
health and substance use disorders).
• Whether or not the client is enrolled with a Primary care case management
(PCCM) provider.
• Verifying the client is Medicare eligible.
• How to determine if the client has commercial private insurance, Medicare
Part C or D, or military.
• How to verify a client receives services from specific providers.
• Verifying a client is receiving services through a hospice agency.
• How to determine an individual is a client of the Developmental Disabilities
Administration (DDA).
• How to verify a client is participating with the Department of Health’s Children
with Special Health Care Needs (CSHCN) program.

25 | PROVIDERONE BILLING AND RESOURCE GUIDE
Client with managed care
If the client is enrolled in a Managed Care Organization (MCO), the following
segment will be displayed as part of the client benefit inquiry. HCA does not
process or pay claims for clients enrolled in an MCO for services provided under
the plan’s contract. If the service is covered by the MCO, do not bill HCA as a
secondary payer. If there is no managed care segment, or there are end dates
noted for the managed care plan and the dates you are billing for, the client is
fee for service, and you should bill ProviderOne directly.
Note: The benefit inquiry response does not return the primary
care provider (PCP) information but does return the PCP clinic
name when the information is available.
Contact the managed care plan with any questions regarding authorization and
billing. See Appendix C for MCO contact information.
Note: Already saw a client enrolled in an MCO and the provider
is not the assigned primary care provider (PCP), or the client
does not have a referral? Contact the PCP to get a referral and
then call the MCO to see if authorization is required or can be
obtained for the service provided. If the office is not contracted
with the MCO, call the MCO to see if they have an allowance for
a noncontracted provider treating the client.
When a client is enrolled in an MCO upon admit to a hospital stay, then disenrolls
from the plan and becomes fee for service (FFS) during the stay, the entire stay
and physician services are the responsibility of the plan until the client is
discharged.
Integrated managed care
Integrated managed care (IMC) was implemented in 2016 and includes physical
and mental health services, and drug and alcohol treatment, all in one health
plan. It is now available in all regions of the state with the remaining areas of
Thurston-Mason, Great Rivers, and Salish implemented January 1, 2020.
For more information, view a map of the integrated managed care plans available
in each region. IMC is represented as fully integrated managed care (FIMC) in
ProviderOne:

26 | PROVIDERONE BILLING AND RESOURCE GUIDE
Clients enrolled in Apple Health Core Connections (AHCC) will have a Healthy
Options Foster Care (HOFC) segment for Coordinated Care listed in the managed
care section:
Note: Effective for claims with dates of service on and after
January 1, 2017, clients with other primary health insurance may
be enrolled into an Apple Health managed care plan as a
secondary insurance. Remember to always check for other
primary payers when verifying eligibility in ProviderOne. See the
Apple Health Medicaid provider alert dated 11/16/2016 10:09
AM PST.
If a client has a managed care plan as their secondary
insurance, all updates related to their primary payer
(terminations, etc.) must be reported through the managed
care plan not through the agency’s Coordination of Benefits
Unit.
Health Home program
The Health Home (HH) program provides patient-centered care coordination
services to support Medicaid and dual Medicaid/Medicare eligible clients in
accessing appropriate medical and social services. Care Coordinators (CC) work
with clients to support their overall health, wellbeing, and self-care. Participation
is optional and does not affect Medicaid coverage or other health care benefits
the client is currently receiving.
FFS clients enrolled in the HH program will have a segment for “Health Home
Only” listed in the managed care section:
A managed care client enrolled in the HH program will have a Health Home
eligibility segment on the benefit inquiry screen in ProviderOne.

27 | PROVIDERONE BILLING AND RESOURCE GUIDE
Behavioral health services
As of January 1, 2020, the state has fully transitioned all behavioral health
organizations into the integrated managed care program (IMC). All behavioral
health services (including substance use disorder [SUD]) will go through the
client’s managed care plan.
Clients who are dual eligible (Medicare as primary) or some clients who are fee
for service, will receive behavioral health services through Behavioral Health
Services Only program (BHSO).
Clients enrolled in a BHSO will have the following display:
Apple Health clients who are in a program that is not eligible for a BHSO should
be referred to the appropriate community resource in their county to see if there
are available funds for services.
For more information on IMC and BHSO programs, please visit the Behavioral
Health Care and Recovery webpage page.
State-only programs
Some provider groups rely on the ACES program codes to help them determine if
the client is on a state only (fee for service) program. Review the ACES Program
Codes for assistance.
Primary Care Case Management (PCCM)
Primary Care Case Management (PCCM) is an Apple Health (Medicaid) program
where an Indian Health Service (IHS) or tribal clinic serves as the primary care
provider (PCP) and manages the client’s health care needs, including specialty
care. To support coordination of the health care services the client is receiving,
the agency requires a referral from the client’s assigned PCP.
Clients enrolled in a PCCM will have the following display in the Managed Care
Information section:
• Clients who have a PCCM have Apple Health (Medicaid) coverage without a
managed care plan and all claims are billed to ProviderOne fee for service.

28 | PROVIDERONE BILLING AND RESOURCE GUIDE
• All clients with a PCCM must have a referral from their PCCM for health care
services to be paid to an outside provider.
• Bill all services for PCCM clients covered by the referral to Apple Health and
indicate the PCCM referral number on the claim.
• Women who have a PCCM provider do not need a referral for OB/GYN, or
family planning services provided outside of the PCCM.
The current PCCMs are:
• Lake Roosevelt Community Health Centers
• Inchelium Clinic
• Lower Elwha Health Clinic
• Puyallup Tribal Health Authority
• Seattle Indian Health Board
• Lummi Tribal Health Center
• Roger Saux Health Center - Medical
• Native Project
• Nooksack Community Clinic
• Tulalip Tribes
• Yakama Health Center
• David C Wynecoop Memorial Clinic
• Colville Indian Health Clinic
• Shoalwater Bay Tribal Clinic
• Quileute Health Clinic
Clients with Medicare
The Medicare Eligibility Information screen displays the following segments for
clients eligible for Medicare Part A or Part B:
You must bill Medicare as the primary payer if Medicare covers the service. The
client’s Medicare Beneficiary Identifier (MBI) will be returned on a ProviderOne
benefit inquiry screen for billing purposes.
Commercial insurance, Medicare Part C/D, or military
benefits
If the client has other coverage, ProviderOne displays the following segments in
the Coordination of Benefits Information section of the eligibility results:

29 | PROVIDERONE BILLING AND RESOURCE GUIDE
Note: If you know an Apple Health client has a commercial
insurance and you do not see a Coordination of Benefits
Information segment on their eligibility file in ProviderOne, you
must complete a Contact Us email. Choose “I am an Apple
Health (Medicaid) biller or provider,” then choose the Medical
Provider button. On the select topic dropdown, choose Private
Commercial Insurance. Enter the client’s insurance information
in the Other Comments section. The agency’s Coordination of
Benefits unit will update the client’s file using this information.
Check eligibility again in ProviderOne in 3 – 5 business days to
verify the update has been made. Only after verification of this
information in ProviderOne should you bill the claim to the
system.
• You must bill the commercial private insurance as primary. ProviderOne
should be billed only after verification of commercial insurance on the client’s
file in ProviderOne, and all other commercial insurance claims have been
processed.
• The insurance carrier code displayed under the Carrier Code column must be
used on the direct data entry (DDE) secondary insurance claims billed to
ProviderOne as the insurance company ID number.
• If the private insurance does not cover the service or has denied the service,
expand the Other Insurance Information area in the DDE screen and complete
all required fields, entering zeros for COB Payer Paid Amount. If you do not
have a specific Claim Adjustment Reason Code (CARC) to enter in the Claim
Level Adjustment area, you must attach the letter or EOB from the primary
payer. By entering the Other Insurance Information, the claim will be manually
reviewed with the backup submitted. For assistance submitting backup with
your DDE claim, review the submitting backup documentation for a DDE claim
section of this guide.
• You must bill the Medicare Part C plan as primary. Bill a secondary crossover
claim to the agency after the claim is processed and payment is made by the
plan. If the Part C plan did not make a payment, these claims would not be
considered crossover claims and will be processed as a standard medical claim
in ProviderOne. Include a copy of the Medicare EOB with the denied claim.
• ProviderOne may pay the client liability amount (deductible, co-insurance, or
co-pay) according to the agency’s payment policy.
• If ProviderOne indicates Medicare Part D (prescription drug coverage) in the
Coordination of Benefits section, see the Prescription Drug Program provider
guide for specific details.

30 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Refer active-duty military clients who are eligible for benefits with the Civilian
Health and Medical Program of the Uniformed Services (CHAMPUS) to use
their local military facility. When a client is CHAMPUS eligible, the insurance
carrier code is either HI50 or HI00 (see example below).
• Individuals with Department of Veterans Affairs (VA) eligibility may seek care
through their VA primary insurance, but it is not required. When billing HCA
as secondary insurance, use the insurance carrier code VE02.
Note: If the client needs to locate a VA medical center, they may
call 1-800-827-1000 from any location in the United States and
the call routes automatically to the nearest VA regional office.
• Refer clients who have insurance through a commercial Health Maintenance
Organization (HMO) to their designated facility or provider. If a client’s
primary insurance is through an HMO, the insurance carrier code will be HM,
HI, or HO.
• Apple Health does not pay for services referred to a provider not contracted
with the primary HMO. This is the responsibility of the referring HMO. If the
HMO does not cover the service, the agency may be billed for those services if
they are covered by Apple Health.
Exception: If a client lives more than 25 miles or 45 minutes away from the
nearest primary HMO provider/facility, Apple Health will pay for nonemergency
services under the fee for service (per fee schedule) program. These cases are
generally determined on an individual basis.
You must complete a Contact Us email to our Coordination of Benefits Unit.
Choose the option “I am an Apple Health (Medicaid) biller or provider” and then
choose the Medical Provider button. On the select topic dropdown, choose
Private Commercial Insurance. Enter information relating to the issue in the
Other Comments section to include a reference to “out of area network review.”
The primary HMO may require notification of any emergency services before they
make any payment(s).
The Contact Us form can also be used to update a client’s file when the
commercial insurance is no longer active following the same steps as above. In
the Other Comments section enter the following detail:
• Termination date of the private insurance
• Date you spoke to the insurance agent to verify end date.

31 | PROVIDERONE BILLING AND RESOURCE GUIDE
The agency does not deny the following services for third party coverage unless
the third-party liability (TPL) carrier code is HM, HI, or HO:
• Outpatient preventative pediatric care
• Outpatient maternity-related services
• Accident-related claims, if the third party benefits are not available to pay the
claims at the time they are filed
Note: If it is determined that there is a possible casualty claim,
call the toll-free number at 1-800-562-3022 [e.g., motor vehicle
accident, Department of Labor and Industries (L&I) claim, injury
diagnosis]. See Appendix D for more information on casualty
claims.
Restricted client information
(WAC 182-501-0135)
Some clients are assigned to certain providers. ProviderOne displays the
following segment(s) in the Restricted Client Information screen when clients are
restricted to specific providers:
• The Patient Review and Coordination (PRC) program assists clients in using
medical services appropriately by assigning them a PCP, pharmacy, and/or a
hospital for nonemergency care. The PCP may make referrals for specialty
medical care. Some covered services that do not need a referral include, but
are not limited to, dental and medical equipment.
• Providers must bill PCP referred services with the PCP’s National Provider
Identifier (NPI) in the appropriate field on the claim. You may look up an NPI
at the National Plan & Provider Enumeration System (NPPES) Registry website.
For questions about the PRC program or to report a client for utilization
review, call 1-800-562-3022 ext. 15606.
Hospice services
(WAC 182-551-1210)
If the client receives services through a hospice agency, the following segment
will be displayed as part of the client benefit inquiry:
See the Hospice Services provider guide for more information.

32 | PROVIDERONE BILLING AND RESOURCE GUIDE
Developmental Disabilities Administration (DDA)
Clients of DDA will display the following segment in the Developmental Disability
Information section of the eligibility results:
Clients of DDA may be eligible for additional medical services. See the program
specific provider guides for those additional services.
Children with Special Health Care Needs (CSHCN)
If the client has special health care needs and is enrolled in the CSHCN program,
the system displays the following segment in the Children with Special Health
Care Needs Information section of the eligibility display:
Medicaid suspension
If an existing Apple Health client is incarcerated or committed to a state hospital,
their coverage with Apple Health will be suspended and no longer end dated in
ProviderOne. If you see the term “suspended when doing an eligibility check,
Apple Health would only be covering inpatient services for the time frame during
the suspension. All other services during the suspended timeframe would be
covered by the jail or state hospital. For more information, visit the Medicaid
Suspension webpage:
Pitfalls
• Failing to check the dates on a displayed segment. When reviewing the
eligibility record, always make sure the dates on a segment correspond with
the actual date of service.
• Billing the agency when there is a primary payer. This delays receipt of
payment increasing a provider’s workload. Commercial insurance must be
added to a client’s file prior to submitting a secondary claim to ProviderOne.
• Providing a service to a client who has chosen to obtain care with a PCCM
provider, and this provider is not the PCP, or the PCCM provider/PCP did not
refer the client. Contact the PCP for a referral.

33 | PROVIDERONE BILLING AND RESOURCE GUIDE
Benefit Service Package
Benefit Service Packages (BSP) do not cover all services and procedures. Providers
should always verify the service provided is a covered benefit under the client’s
BSP.
View additional information related to programs covered under a specific BSP
(e.g., physical therapy, dental, hospital) by clicking on the hyperlink under the
heading Benefit Service Package.
See Appendix E for an overview of Benefit Service Packages.
Spenddown
Spenddown is a type of client liability, like an insurance deductible. Spenddown
liability is the amount of medical expense a client must pay before Limited
Casualty Program/Medically Needy Program (LCP/MNP) coverage begins. When
the client has paid medical expenses equal to or greater than a predetermined
spenddown amount, the provider can submit a claim for the outstanding amount.
Medical coverage does not always begin on the first day of the month. A date of
service that is the same as the Medicaid eligibility start date may require the
claim to show a spenddown liability amount. See the Provider Spenddown step-
by-step fact sheet and Chapter 182-519 WAC for more information on
spenddown.
If the client has not accumulated enough financial obligation to obtain medical
benefits, the Benefit Service Package displays Pending Spenddown – No Medical:
Spenddown FAQ
Q - How do I find out if our claim was used to meet a client’s spenddown
liability? How do I find out how much of our claim was assigned to a client’s
spenddown liability?
A - Call the spenddown inquiry toll free number for providers 1-877-501-2233
and leave a message to request a call back from the specialized Spenddown Unit.
Q - How will my claim be processed if there is a spenddown amount applied to
my claim?
A - HCA will deduct the spenddown amount from HCA allowable amount. For
more information on provider payments, see WAC 182-519-0110.
Q - How do I know if a claim was denied for spenddown?
A - Check the remittance advice to find the denial code for the claim. Claims

34 | PROVIDERONE BILLING AND RESOURCE GUIDE
denied for spenddown will show adjustment reason code 125 and remark code
N58.
Q - What will happen if I submit a claim when ProviderOne indicates the client is
“pending spenddown”?
A - The claim will deny because the client is not eligible.
Q - Can I charge the client when some or my entire bill has been used to meet
the client’s spenddown liability?
A - Providers may charge the client no more than the spenddown amount that
was applied to the claim. See WAC 182-519-0110 for more information.
Q - How do I report spenddown on a claim?
A - See the Provider spenddown step-by-step fact sheet.
Q - What if I see an active Benefit Services Package, such as CNP effective for the
same date(s) as a pending spenddown segment?
A - Due to changes in the way eligibility is determined and displayed in
ProviderOne, some clients still show pending spenddown segments from the
benefit they had prior to Medicaid expansion on 1/1/14; these will not go away
until the end of their spenddown period, so until that happens providers will see
overlapping eligibility. It is important to note the active segment will always be
honored, so in these situations providers can ignore the pending spenddown
segment and bill according to the active segment.
Pitfalls
• Failing to check the client’s Benefit Service Package. This may result in
providing services that are not covered by HCA.
Medical records for clients in Foster Care
ProviderOne now gives the provider access to claims history for children in foster
care. The claims history (pharmacy, dental, medical, etc.) will be available when a
provider performs an eligibility check in ProviderOne.
Providers may benefit from knowing a foster care client’s claims history before
treating or prescribing medications for the client.
Log into ProviderOne and select the Benefit Inquiry hyperlink to conduct an
eligibility check for the client.
Enter the appropriate search criteria to locate the client’s eligibility information. If
the selected client’s medical records are available when the eligibility page
displays in ProviderOne, the following “Medical Records” button appears
at the top left of the screen:

35 | PROVIDERONE BILLING AND RESOURCE GUIDE
Note: The placement code (indicated by the arrow in the image
above) may allow an enhanced payment to providers for certain
E&M codes. See the EPSDT provider guide for the placement
code table, plus detailed information about how to bill for the
enhancement.
Select Medical Records to open the next screen which contains claims
information in three separate sections. These sections contain information about
paid claims obtained from the ProviderOne claims history database. Two years of
data will be returned by default, regardless of the eligibility search begin or end
dates.
The three sections include:
• Pharmacy services claims
• Medical services claims (including dental)
• Hospital services claims
The overall screen looks like the example below. Providers may need to use the
scroll bar on the right side of the page to see the bottom portion of the screen.
This is a “Printer Friendly Version”, so the content of this screen is printable by
clicking on the blue “Printer Friendly Version” hyperlink at the top center of the
screen.

36 | PROVIDERONE BILLING AND RESOURCE GUIDE
The first section contains the Pharmacy claim information:
Some fields could be empty or contain “zero (0)” as a value for the different
pharmacy claims if that information is not available for viewing.
Providers have the option to search the pharmacy list for specific dates of service
by using the “Filter By Period” option as seen in the segment below.
1. Pick the filter value name (all or a date range) using the drop-down
option.
2. If using a date range, in the next box indicate the filter value “from” date
of service.
3. Next in the date range, use the second filter box to enter the “to” date of
service (all dates entered in ProviderOne must be formatted as
mm/dd/ccyy).

37 | PROVIDERONE BILLING AND RESOURCE GUIDE
4. Click the Go button.
ProviderOne will return the paid claim(s) found for those filter values based on
the “from” date. Providers can sort the list of pharmacy claims using the up/down
triangles located under each blue column heading.
The system only sorts by one column heading at a time; however, it will sort the
whole list based on the column heading chosen.
• Clicking on the triangle (caret) on the left causes ProviderOne to sort the list
by the oldest, smallest, or in alphabetical order, according to the column
specified.
• Clicking on the caret on the right causes ProviderOne to sort the list by the
latest, largest, or in reverse alphabetical order, according to the column
specified.
Note: The search (Filter By) option and the column sort
functions work the same for each specific claim section on this
screen.
Providers should keep in mind that each claim history section may have multiple
pages. The buttons at the bottom of the page provide the ability to move to the
next page if they have black text. If there are no more pages to review, the Next
button will be greyed out. In the following screen example, the Next button
indicates that more than one page of claims is available to view.
The medical, including dental, services section look like the following segment:

38 | PROVIDERONE BILLING AND RESOURCE GUIDE
Some fields could be empty when viewing the different professional and dental
services because the information did not apply to the service indicated, or the
data may not be available. The “filter by” (search) and the column sort features
described above work the same on this screen.
The hospital care screen looks like this and is the last section on the page:
When viewing the hospital claims in this section, some fields may be empty
because the information does not apply, or the data is not available. The “filter
by” (search feature) and the column sort features work the same as described in
the previous section.
Note: If any one of the screens return the message No Records
Found! the client does not have any claims history for that
section.
Covered services and prior authorization
Apple Health does not cover all medical services and some covered services
require Prior Authorization (PA). The agency will not pay a claim if a provider fails
to obtain a required prior authorization. For additional information on prior
authorization, visit the Prior Authorization webpage.
This section describes how to identify a procedure code, how to use that
procedure code to determine if Apple Health covers the service, and how to
determine if PA is required (as identified in Apple Health’s program specific
provider guides).
PA indicates providers must obtain prior authorization before providing certain
healthcare services, equipment, or supplies to clients. Before approval of a prior
authorization request, the provider must prove the service is medically necessary.
For more information, see WAC 182-501-0165, Expedited Prior Authorization
(EPA) WAC 182-531-0200, Exception to Rule (ETR) WAC 182-501-0160, and
Limitation Extensions (LE) WAC 182-501-0169.
Identify the procedure code which best describes the service provided to the
client. Use the following types of codes when billing in ProviderOne:
• American Dental Association (ADA) Current Dental Terminology (CDT)
procedure codes
• American Medical Association (AMA) Current Procedural Terminology (CPT)
procedure codes (CPT® is a registered trademark of the American Medical
Association)

39 | PROVIDERONE BILLING AND RESOURCE GUIDE
• U.S. Department of Health & Human Services ICD-10 diagnosis codes
• Level II Healthcare Common Procedure Coding System (HCPCS) procedure
codes
• National Drug Code (NDC)
• Revenue codes - the National Uniform Billing Committee (NUBC) assigned
coding system for billing inpatient and outpatient hospital services, home
health services, and hospice services.
Procedures performed must match the descriptions and guidelines from the most
current CPT, HCPCS, CDT, and ICD-10 manuals for all Apple Health covered
services. HCA publishes only the short descriptions of procedure codes due to
copyright restrictions. Consult the current manual for full descriptions.
Procedure codes and fee schedules
The fee schedules will provide information about the procedure code and
payment rate. HCA updates fee schedules as updates to national codes occur and
HCA is notified of the changes.
Covered procedures
Procedure codes that are not listed in the fee schedule for a specific program are
not a covered service under that program.
Also review the maximum allowable columns:
• If there is an NC noted, it is a non-covered service.
• If there is a DC noted, a different service code should be billed.
• Consult the legend for each fee schedule for specific detail.
Note: You can request an “Exception to Rule” (ETR) authorization
for a non-covered service. For more information about ETR, see
WAC 182-501-0160.

40 | PROVIDERONE BILLING AND RESOURCE GUIDE
Prior authorization requirement
The fee schedule may indicate that PA is required.
If this is the case, you have two options to submit your prior authorization
request:
• Enter the prior authorization request through the direct data entry (DDE)
feature in the ProviderOne portal.
o For complete self-service training materials, click one of the following links
depending on your provider type:
▪ Medical providers
▪ DME providers
▪ Dental providers
• Complete the General Information for Authorization form, HCA 13-835. To
ensure that the form will be scanned correctly, see the instructions about
completing this form in Appendix F and the back of the form.
o If a provider is faxing supporting documentation without the original
authorization request form, print the required cover sheet to ensure
association with the correct authorization. For more information see the
document submission cover sheets webpage and Appendix H.
• Once a provider has submitted the PA request, check the status using
ProviderOne or the IVR. For more information, see Appendix G.
When Medicare is the primary payer and denies a service that is covered by the
agency with a prior authorization requirement, the agency waives the “prior”
requirement in this circumstance. Submit a request for authorization. Attach the
Explanation of Benefits (EOB) to the request for services denied by Medicare.
Note: If the client has TPL, also known as commercial or private
insurance, and the service you are billing for requires prior
authorization (PA) from the agency, the agency waives the “prior”
requirement in this instance. If the commercial insurance denies
payment for the service that required the authorization, you
must then request authorization and include a copy of the
insurance denial EOB with the request. See the Requesting prior
authorization section for more information on submitting an
authorization request.
For some programs PA is required before providing services regardless of which
payer is considered primary. Examples of this are DME supplies,
dental/orthodontia, and inpatient hospital stays that require authorization.

41 | PROVIDERONE BILLING AND RESOURCE GUIDE
If the primary pays the service, then authorization is not required for the
secondary claim. Refer to the program specific provider guide applicable to the
service provided.
Note: When billing HCA using a “By-Report” (BR) CPT or HCPCS
code that requires authorization and the authorization has been
approved, a provider must:
- Bill HCA with the amount requested on the authorization
form.
- Do not bill HCA the allowed amount for the (BR) CPT or
HCPCS code.
- Do not include sales tax in the billed amount for the (BR) CPT
or HCPCS code.
The fee schedule may indicate “EPA” for expedited prior authorization. The EPA
process eliminates the need for prior authorization for selected procedures. The
intent is to establish authorization criteria and identify these criteria with specific
codes, enabling providers to create an EPA number when appropriate. Refer to
the program specific provider guide for the EPA criteria for specific supplies or
services.
EPA guidelines
• Medical justification (criteria) - all medical justification must come from the
client’s prescribing physician or physical/occupational/speech therapist. HCA
does not accept information obtained from the client or from someone on
behalf of the client (e.g., family).
• Documentation - the billing provider must keep documentation of the criteria
in the client’s file. Upon request, a provider must provide documentation to
HCA showing how the client’s condition met the criteria for EPA. Keep
documentation on file for six (6) years.
• Providers must follow EPA criteria exactly. If the exact EPA criteria outlined in
the provider guide is not met, the formal PA process must be followed.
Note: HCA may recoup any payment made to a provider if the
criteria do not meet the requirements or the wrong code was
used on the claim.
For more information on prior authorization and expedited prior authorization, visit the Prior
authorization webpage.
Claim payments – professional services
Apple Health publishes fee schedules to communicate to providers the maximum
allowed amount for a health care service.
• Use the fee schedule to determine the payment rate for the procedure.
o Facility setting maximum allowable fee (FS fee) is paid when the provider
performs the services in a facility setting (e.g., a hospital or ambulatory

42 | PROVIDERONE BILLING AND RESOURCE GUIDE
surgery center) and the cost of the resources are the responsibility of the
facility.
o Non-facility setting maximum allowable fee (NFS fee) is paid when the
provider performs the service in a non-facility setting (e.g., office or clinic)
and typically bears the cost of facility space and resources, such as labor,
medical supplies, and medical equipment associated with the service
performed.
• Use the fee schedule that covers the date of service on the claim.
Note: HCA does not pay more than the billed amount on a claim
regardless of the allowed fee listed in any of the fee schedules.
HCA recommends that providers bill their usual and customary
charges on their claims. Claims that are underpaid will have to be
adjusted by the provider to capture the under billed but allowed
amount. (Exceptions are for trauma claims and services that pay
a sales tax.)
Claim payments – institutional services
Providers billing on an institutional claim have various payment methods that are
much too detailed to cover in this publication. Please see the appropriate fee
schedule or provider guide for detailed information about payments.
Claim payments – inpatient hospital services
For payment information on inpatient hospital services, please see the Inpatient
hospital services billing guide.
Provider preventable conditions (PPCs)
The agency has established a policy for services provided to Medicaid clients,
both FFS and for those enrolled in one of HCA’s MCO plans that result in provider
preventable conditions. The rule applies to all health care professionals and
inpatient hospitals.
Provider preventable conditions is a term used for hospital and non-hospital
acquired conditions that are included in two distinct categories:
• Health care-acquired condition (HCAC) is a condition occurring in any
inpatient hospital setting (identified as a hospital acquired condition by
Medicare). Examples include a foreign object retained after surgery to certain
surgical site infections, etc. See the Medicare Hospital-Acquired Conditions
HAC list and WAC 182-502-0022.
• Other provider preventable conditions (OPPCs) are an adverse health event
that could have been prevented through the application of nationally
recognized evidence-based guidelines. Examples of PPCs include surgery on
the wrong patient, or medication errors, etc. Also see adverse health events
identified by the Department of Health in WAC 246-302-030.
Under the policy, HCA will deny or recoup payments to health care professionals
and inpatient hospitals for care related only to the treatment of consequences for
HCAC and OPPC conditions.

43 | PROVIDERONE BILLING AND RESOURCE GUIDE
All hospitals are required to include the present on admission (POA) indicator
when submitting inpatient claims for payment. The POA indicator may prompt a
claim review when billed with an HCAC diagnosis code according to CMS
guidelines. Professional claims will be identified using this claim information.
For professional services performed during an inpatient hospital stay, insert one
of the following modifiers to all lines related to the surgical error:
• MX – wrong surgery on patient
• MY – surgery on wrong body part
• MZ – surgery on wrong patient
CMS has created three new HCPCS Level II modifiers for practitioners, ambulatory
surgical centers (ASCs), and hospital outpatient facilities to use to report
erroneous surgeries. Add one of the following HCPCS Level II modifiers to all
lines related to the surgical error:
• PA – surgery wrong body part
• PB – surgery wrong patient
• PC – wrong surgery on patient
Providers must report confirmed PPCs to HCA within 45 calendar days of the
incident. Notification must be in writing, addressed to HCA’s Chief Medical
Officer (CMO) and include the PPC, date of service, client identifier, and the claim
number (TCN) for claims submitted in ProviderOne. Hospitals and health care
professionals must complete their portion of the “Other provider preventable
conditions (OPPC) notification form” 12-200 and send with the notification.
The complete text and details covering a PPC, ProviderOne payment, reporting a
PPC, and a provider dispute process can be located in WAC 182-502-0022.
Pitfalls
• Using outdated coding books. This can result in a claim denial.
• Using a procedure code and diagnosis code that do not correspond with each
other. This can result in a claim denial.
• Not confirming eligibility on the day of service. PA does not override
eligibility.
• Failing to obtain authorization when required will result in a claim denial.
• Handwriting the PA request form. If the PA request is not typed, it will be
returned to the provider because it cannot be scanned using “optical
character recognition.”
• Trying to request authorization without the client ID. If the client ID is
unknown, providers can do a client search in ProviderOne.
• Billing claims without the proper PPC modifier or POA indicator could result in
a claim review and possible recoupment of the payment.

44 | PROVIDERONE BILLING AND RESOURCE GUIDE
Client service limits
Apple Health limits certain covered services with respect to quantity, frequency,
or duration. For example, HCA covers a routine eye exam for an adult client every
two years, or some DME supplies, and dental services may have quantity and
frequency limits.
Determine the service needed. Then look in the program specific provider guides
to find the quantity, frequency, or duration service limitations. Providers can
check client service limits by:
• Using the Client Limit Inquiry feature of ProviderOne, or
• Use the secure contact us form, or
• If the date of service is within 48 hours, call the Customer Service line at 1-
800-562-3022 and follow the prompts for provider services. All other requests
must utilize the contact us web form.
ProviderOne allows providers to check service limits using claim data stored in
ProviderOne. This system functionality is limited to claims previously paid by
ProviderOne and does not account for claims received in the system but are still
in process or have denied. There is also the possibility that billing has not
occurred for provided services.
Check for service limits by logging into ProviderOne and selecting one of the
following profiles:
• EXT Provider Super User
• EXT Provider Claims Submitter
• EXT Provider Eligibility Checker
• EXT Provider Eligibility Checker-Claims Submitter
Select the Client Limit Inquiry hyperlink on the provider portal:
At the Client Limit Inquiry screen fill in the required fields numbered below:

45 | PROVIDERONE BILLING AND RESOURCE GUIDE
1. Client ID number
2. Date of service (when you are planning a visit/service; future dates accepted)
3. Taxonomy code of the billing provider
4. Requested unit(s) - requires at least one or enter the amount to be supplied.
5. Procedure code
6. Primary diagnosis code (if required) - no decimal point should be used here.
7. Invoice type (claim type)
o D = dental
o P = professional
o I = institutional
8. Provider NPI (pre-populated)
9. Facility type (place of service if procedure code requires)
10. Modifiers (if the service has a specific modifier)
11. Tooth number (if dental service requires a tooth)
Example request with completed form:
Click the Submit button after completing all the required fields. The system
clears the data boxes and displays the information entered in the form at the
bottom of the client limit inquiry screen.

46 | PROVIDERONE BILLING AND RESOURCE GUIDE
The limit inquiry is processing in the background, so the Available unit(s) box is
still empty. Wait a short time then click the Get Results button to see the
response to the limit inquiry.
Note: If the Available unit(s) box remains empty click on the Get
Results button again as it may take ProviderOne a few seconds
to complete the database inquiry.
Once the inquiry is complete, ProviderOne will display this screen with a value
populated in the Available unit (s) field:
If there are available units, the system will display the number of units available.
Note: The available unit(s) does not account for services
incurred but not yet billed or reported. The information returned
does not imply a service authorization or guarantee of payment.
Both ProviderOne and the HCA toll free phone line rely on the submission of
claims for services paid in ProviderOne. If the system finds claims for the service
performed within the timeframe of the service limit, it will return a zero value for
the Available unit(s) field.

47 | PROVIDERONE BILLING AND RESOURCE GUIDE
In these cases, the billing provider should review the program specific provider
guide to see how to proceed with treatment and check for any PA requirements.
Note for vision providers: Use one of the exam codes or fitting
fee codes as the search criteria rather than one of the hardware
codes. ProviderOne will not have a record of the history of these
codes since hardware is not billed directly to HCA. For questions
about hardware benefits, contact Airway Optical at 888-606-
7788.
Other reasons ProviderOne may return a zero
• The client is enrolled in a managed care plan, is QMB-Only or covered by
Medicare, etc. which may mean that no units are available through Medicaid
fee for service.
• The client is currently ineligible.
• The billing provider taxonomy is incorrect for the procedure code and/or the
taxonomy used is not listed on the provider’s file in ProviderOne.
• The diagnosis code used is incorrect for the procedure (if applicable).
• The modifier used is incorrect for the procedure (if applicable).
ProviderOne will retain the Client Limit Inquiry data line you entered if
completing additional limit checks for other codes during the same session.
Pitfalls
• Not checking for service limits. By not checking client eligibility for services
that have quantity, frequency, or duration limits of the services, providers risk
denial of a claim.
• The results of the search are separate from checking a client’s eligibility for
any service. It is the responsibility of the provider to verify eligibility for the
estimated date of service, in addition to checking service limits.
• Not checking eligibility to verify enrollment of the client in a managed care
plan that pays for services outside ProviderOne.

48 | PROVIDERONE BILLING AND RESOURCE GUIDE
Submitting fee for service claims
Timely and accurate payments
This section shows how to submit claims using the following methods:
• Direct data entry into ProviderOne
• Process online batch submissions (837)
And to perform the following:
• Submit electronic and paper backup documentation on individual claims
• Resolve errors during a claim submission
• Submit commercial insurance secondary claims
• Save claims
• Submit Medicare crossover claims
• Check claim status
• Submit claim adjustments
• Resubmit denied claims
• Void paid claims
• Create template claims
• Submit a template claim or a batch of template claims
When you determine that the client is eligible for Apple Health, the service is
covered, Apple Health is the primary payer, and any authorization requirements
have been fulfilled (if required), you may bill ProviderOne after rendering the
service.
Disclaimer
A contract, known as the Core Provider Agreement (CPA), governs the
relationship between HCA and Apple Health providers. The CPA’s terms and
conditions incorporate federal laws, rules and regulations, state law, HCA rules
and regulations, and HCA program policies, numbered memoranda, and provider
guides, including this guide. Providers must submit a claim in accordance with
HCA rules, policies, provider notices, and provider guides in effect at the time
they provided the service.
HCA does not assume responsibility for informing you of national coding rules.
ProviderOne denies claims billed in conflict with national coding rules. To correct
such errors, consult your coding resources.

49 | PROVIDERONE BILLING AND RESOURCE GUIDE
Claim submission method
HCA wants you to receive timely payments. Providers usually base their claim
submission method decision in part on the volume of claims billed and the level
of technology they have available.
Select one of the methods below:
• Direct data entry of individual claims using the ProviderOne portal -
ProviderOne enables you to submit new claims, check claim status, submit
adjustment claims, correct, and resubmit denied claims, and attach electronic
backup documentation to claims. Updates to ProviderOne claim options
enable you to create and save template claims, create a claim from the
template, and create batches of claims using saved templates.
• Electronic batch claim self-submission - electronic claims you submit directly
in ProviderOne using a companion guide to keep your software up to date
[electronic batch submitters are required to pass testing with ProviderOne and
have a Trading Partner Agreement (TPA)].
• Electronic batch claim submission using a billing agent or clearinghouse -
electronically submitted claims to ProviderOne through a billing agent or
clearinghouse, who use a companion guide to keep their software up to date
[electronic batch submitters are required to pass testing with ProviderOne and
have a Trading Partner Agreement (TPA)].
For more information on trading partner agreements, see the HIPAA Electronic
Data Interchange (EDI) webpage.
Claim backup
Claims billed in ProviderOne may need backup documents if the client has:
• Commercial private insurance
• Medicare
• A Medicare Advantage plan
You must attach backup documentation to DDE or electronic claims when a
specific type of service requires additional information. Examples of these backup
documents include:
• Invoices for Acquisition Costs (AC)
• By Report (BR) services
• Operative reports or other documents, if required or requested by HCA
An Explanation of Benefits (EOB) may be needed if there is a primary payer.
• If you are submitting an EOB with a claim, the information on the claim must
match the line information billed to the primary payer as reflected on the EOB.
Documentation is needed for some services such as the following:
• Acquisition Cost (AC) and By Report (BR) services are listed in the fee
schedules. Review the fee schedules on the fee schedule webpage.

50 | PROVIDERONE BILLING AND RESOURCE GUIDE
See below for an example from the professionally administered drugs fee
schedule, J7699, which has the AC (acquisition cost) indicator in the allowable fee
field. Refer to the provider guides to verify if an invoice will be required as
backup.
Acquisition Cost (AC) indicators
Claims for drugs with an AC indicator in the fee schedule with billed charges of
$1,100.00 or greater or claims for supplies with billed charges of $50.00 or
greater, require a manufacturer’s invoice to be paid. Submit a copy of the invoice
by attaching it to the claim and note the quantity given to the client in the
comments or billing note section of the claim.
It is not necessary to attach an invoice with claims when procedure codes have an
AC indicator in the fee schedule for drugs with billed charges less than $1,100.00,
or supplies with billed charges less than $50.00, unless requested by HCA. For
claims of this type, bill only one unit of service. See acquisition cost (AC) on the
introduction page of the Physician-Related Services/HealthCare Professional
Services provider guide for additional information.
By Report (BR) indicators
Services with a BR indicator in the fee schedule with billed charges of $1,100.00
or greater require a detailed report to be paid. Attach the required report
describing the nature, extent, time, effort, and/or equipment necessary to deliver
the service to the claim.
When the fee schedule contains a BR indicator it is not necessary to attach a
report to the claim for services when charges are less than $1,100.00 unless
requested by HCA. See the Physician-Related Services/HealthCare Professional
Services provider guide for additional information.
ProviderOne may deny a claim and request an operative report to justify medical
necessity for services.
Pitfalls
• Failing to include required backup information with the claim. This will result
in claim denial.
• Billing services not billed to the primary payer. This will cause the claim to be
denied.
• Failing to check eligibility to determine if another payer exists.

51 | PROVIDERONE BILLING AND RESOURCE GUIDE
Submitting new claims and backup
ProviderOne accepts the following methods for you to submit claims and backup
documents:
• Direct data entry into ProviderOne
• Direct data entry commercial insurance secondary professional claim
• Saving a direct data entry claim
• Online batch claims submission
ProviderOne offers several free methods to submit claims to pay for services
provided to our clients. HCA encourages billing using electronic methods
provided in ProviderOne to optimize payment receipts and to improve
resubmission turnaround time in case a claim is denied for a billing error.
This section covers in detail the billing methods available.
Initial claims
Submit claims in the ProviderOne system for assignment of a transaction control
number (TCN) within 365 days from any of the following:
• The date the service was furnished to the eligible client.
• The date a final fair hearing decision is entered that impacts a particular claim.
• The date a court orders HCA to cover the service.
• The date HCA certifies a client eligible under delayed certification criteria.
For more information, see WAC 182-502-0150 (3) (4).
HCA may grant exceptions to the timely filing limit when either of the following
cause billing delays:
• The client receives retroactive Apple Health coverage, which displays in the
eligibility results. The agency allows one year from the date of retroactive
eligibility award.
• For various reasons, ProviderOne may recoup premiums to a client’s managed
care plan, causing the plan to recover payments. Those bills would then need
to be submitted fee for service. ProviderOne will allow one year from the date
the plan recouped the payment for a given claim if you enter “Managed care
recoupment [date]” in the remarks or comments field.
o Follow the same steps to submit the claim to ProviderOne if a managed
care plan paid in error when the service should have been billed fee for
service originally.
• The commercial payer recouped their payment as primary. You have one year
from the date of the takeback to submit the claim to ProviderOne. Enter the
“primary payer” and “recoupment [date]” in the remarks or comments field.
• Providers can prove to the agency that there are extenuating circumstances.
To appeal a timely claim denial made by HCA, contact the customer service
center by phone.
ProviderOne follows National Correct Coding Initiative (NCCI) policy. The Centers
for Medicare and Medicaid Services (CMS) created this policy to promote

52 | PROVIDERONE BILLING AND RESOURCE GUIDE
national correct coding methods. NCCI assists the HCA in controlling improper
coding that may lead to inappropriate payment.
HCA coding policies are based on:
• The American Medical Association’s (AMA) Current Procedural Terminology
(CPT®) manual
• National and local policies and edits
• Coding guidelines developed by national professional societies
• The analysis and review of standard medical and surgical practices
• Review of current coding practices
Direct Data Entry (DDE)
It is extremely important before claims submission to disable any popup blockers
on your web browser. The ProviderOne system uses popup windows during the
claims process.
Log into ProviderOne and choose the EXT Provider Claims Submitter or EXT
Provider Super User profile.
From the Provider Portal, select On-line Claims Entry:
To create a new claim, select the appropriate claim type hyperlink in blue. The
below information is based on choosing the Submit Professional.
Note: For more assistance with DDE for all claim types, visit the
ProviderOne resources webinars webpage.
Complete the required data fields marked with a red asterisk and add any
optional information needed for ProviderOne to process the claim. If you have
questions regarding billing policies, please refer to the appropriate provider
specific provider guide for the claim type.
Enter the billing Provider NPI number and Taxonomy Code. For more
information on taxonomy codes, please see Appendix I for more information.

53 | PROVIDERONE BILLING AND RESOURCE GUIDE
Answering the “yes/no” questions
There are several routine yes/no questions you need to answer on any DDE claim:
• For a solo practice office, the billing provider is also the rendering provider.
• For a clinic or group practice, the billing provider would not be the rendering
provider. Check No to this question and fill in the NPI and taxonomy for the
provider who rendered the service.
• If the service provided is the result of a referral from another provider, check
Yes and enter the referring provider’s NPI (taxonomy codes are not required
for referring providers).
Client information
Enter the ProviderOne Client ID and expand the box by selecting the red plus
sign to enter the client’s name, birthdate, and gender. The client’s last name,
birth date, and gender are required on all claims. While the first name is optional,
if entered the first name also appears on the RA. When billing for a newborn
claim using the birthing parent’s id, enter the baby’s name, baby’s birthdate, and
the baby’s gender in the boxes instead of the birthing parent’s information.
Check Yes if indicating the claim is for a baby using the birthing parent’s ID:
The next data element is a question about Medicare; check Yes if indicating this
is a Medicare crossover:

54 | PROVIDERONE BILLING AND RESOURCE GUIDE
If the claim requires authorization, select the red plus sign to expand the prior
authorization number area, and enter the authorization number:
Sometimes a claim needs a claim note added to the claim so that it processes
correctly. To add a note, click the red plus sign to expand the note option, and
then type in the note information keeping it short.
Some of the reasons to add a note or claim indicator are:
• SCI=B for baby on birthing parent’s ID (can only be used the first 60 days of
baby’s life)
o For multiple births use the following:
▪ SCI=BA for twin/triplet A
▪ SCI=BB for twin/triplet B
▪ SCI=BC for triplet C
• SCI=F for enteral nutrition – client not eligible for WIC
• SCI=I for Involuntary Treatment Act (ITA)
• SCI=V for voluntary (psych) treatment
Other examples of claim notes needed to enter on a claim can be found in the
agency’s program related billing guides.
Note: When using Special Claims Indicator (SCI) entries,
everything following the “=” symbol will be read as part of your
indicator, so do not enter spaces before or after the =.
Always check No for the next question, claim adjudication does not use this
information:
Use the Patient Account No field to enter any internal patient account numbers
used. This information appears on the remittance advice for your convenience.
Enter the Place of Service code number using the drop-down option.

55 | PROVIDERONE BILLING AND RESOURCE GUIDE
If the client has a spenddown amount, report this on the claim by selecting the
red plus sign to expand the Additional Claim Data field and enter the
spenddown amount into Patient Paid Amount.
Now enter the Diagnosis Codes without the decimal point. ProviderOne adds
the decimal point where needed once the claim is submitted. HIPAA allows up to
12 fields for diagnosis codes. Later ProviderOne uses a pointer to indicate which
diagnosis code applies to the service line.
Note: When entering diagnosis codes, do not enter the decimal
point. ProviderOne will add the decimal automatically when the
claim is submitted.
Next enter the basic line item information for the first service line of the claim:
• Enter the Service Date From and To date(s) of service using date spans for
equipment rental, etc.
• Use the dropdown menu to indicate the Place of Service (optional as the place
of service has already been entered at the claim level).
• Enter the Procedure Code being billed on this service line.
• Enter the Modifier(s) if appropriate, then tab through the other boxes.

56 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Enter the Submitted Charges (whole dollar amounts do not need a decimal
point).
• Use the Diagnosis Pointers dropdown to indicate which diagnosis code(s)
from the previous section above will apply to this line.
• Enter the number of Units used - at least one unit must be indicated.
• Enter a National Drug Code (NDC) only if you are billing a code that requires
the NDC in the NDC field. Do not enter the NDC in the Drug Identification
section. Skip that area.
• If you have more than one authorization number, expand the Prior
Authorization section, and enter the PA number for that service line.
• Skip the additional service line Information section.
Next, click the Add Service Line Item button:
The entered line information will appear under the Previously Entered Line Item
Information section. Make sure every line has the correct information and
appears under this section before submitting the claim.
Editing lines due to keying errors or coding mistakes
Select the line number of the line to correct and the system will repopulate the
service line item boxes. Make the changes as necessary and select the Update
Service Line Item button:
The system will change the original information to the corrected information.
You can use a shortcut when adding more lines to the claim. Use the edit feature
of the system to quickly add more lines. Select the line number to repopulate the
service line item boxes. Now add the information for the next line by overwriting
what is there, only changing what is different. Usually only the procedure code
and the billed amount would change, or in some cases the codes are the same,
but the date of service has changed. After adding the updated information, select
the Add Service Line Item button to add the new line. Repeat this process to
add line 3 and 4, etc.
Continuous hospital stay information (only if applies)
Clients that are fee for service (FFS) when admitted to a hospital and then later
enrolled in a managed care plan during the hospital stay, the entire stay for

57 | PROVIDERONE BILLING AND RESOURCE GUIDE
physician services is paid FFS until the client is discharged. Fill out the claim as
normal and before submitting a claim for a continuous hospital stay enter the
initial hospital admit date and discharge date following the instructions below.
Select Other Claim Info at the top of the page:
Then select the Relevant Dates expander:
Enter the Admission Date and Discharge Date for the hospital stay. Select Basic
Claim Info at the top of the page to get back to the first page of the claim
screen, and after entering all the claim information, select Submit Claim at the
top of the screen.
The following popup window message will appear:
If no backup is being submitted, select Cancel and the following window appears:
Select Submit to send the claim to ProviderOne for processing. The system will
return you to a blank claim form ready for your next claim submission.

58 | PROVIDERONE BILLING AND RESOURCE GUIDE
Submitting backup for a DDE claim
ProviderOne allows the biller to submit backup two ways to a DDE claim:
• Browse files on your computer to attach an electronic file
• Submit paper backup with a cover sheet (by fax or mail)
HCA policy specifies how long to hold a claim waiting for backup documentation
as follows:
• DDE – held for 3 days
• HIPAA/EDI – held for 21 days
After selecting Submit Claim, a popup will appear asking if you want to submit
backup documentation:
Select OK to proceed with attaching backup, if/when necessary.
The backup documentation screen tells us about the backup:
Fill in the following fields:
A. Pick the Attachment Type from the drop-down list.
B. The Transmission Code is By Mail (BM), Fax (FX), or Electronic (EL).
C. The Line No field is not required.
D. Add an electronic attachment using the Filename field. Use the choose
file button to find the file on your computer to attach to your claim.
If you receive an error when attaching a file, try changing the name of the
document. Do not use special characters or start file names with a number.
Select OK when completed.

59 | PROVIDERONE BILLING AND RESOURCE GUIDE
Attaching electronic backup
Electronic backup image files are limited to 2 megabytes in size. The below
screenshot shows a sample of an electronic file attached to a claim. Select
Submit to send your claim to ProviderOne for processing.
Attaching paper backup using mail or fax
Attach paper backup to a DDE claim in two different ways, by mail (BM) or by fax
(FX). Write down the TCN number and select Print Cover Page:
Below is an example of the cover sheet. Enter in the TCN number captured on the
confirmation screen when you submitted the claim. The barcode expands to
reflect the data entered once the data field is completed by clicking the enter key
or clicking outside the TCN box.

60 | PROVIDERONE BILLING AND RESOURCE GUIDE
All supporting documentation requires a ProviderOne cover sheet. For more
information on cover sheets, see Appendix H. There is one cover sheet for use
with claims submitted through ProviderOne regardless of claim type. This cover
sheet can be accessed on the document submission cover sheets webpage under
claim attachment.
When filling out the cover sheet, only add in the numeric TCN. Do not add a zero,
an extra space, or any other characters. Do not save the cover sheet for reuse, as
the cover sheet is specific to the claim TCN only. Do not use any software other
than Adobe for opening and generating the cover sheet. The barcode used to
link documents will not work properly using other software.
When finished attaching backup, select Submit to send your claim to
ProviderOne for processing.
To send your paper backup for claims entered by DDE, attach a ProviderOne
cover sheet to the backup documents and either fax to 1-866-668-1214 or mail
using the following address:
Heath Care Authority
RE: Cover sheets and backup documentation
PO Box 45535
Olympia, WA 98504-5535

61 | PROVIDERONE BILLING AND RESOURCE GUIDE
HCA accepts large amounts of backup by mail only. Mail to the above address
and be sure to use a cover sheet for each claim.
Submitting backup through a clearinghouse
You can also easily submit your claims through your clearinghouse, then fax in
your backup documents.
Follow these steps:
• Prepare the claim as normal and submit the claim to the clearinghouse.
(Reminder: the HIPAA file transaction must include the “Claim Supplemental
Information” to notify ProviderOne that backup is being sent. If you have
questions on how to include this detail, please discuss with your software
vendor or clearinghouse, or have them contact HCA HIPAA staff at HIPAA-
• Wait 48-72 hours to allow the claim to process in ProviderOne and for
ProviderOne to assign a TCN number to the claim.
There are two options to get the TCN number for the claim(s):
• Log into the provider portal and select Claim Inquiry, then enter the client ID
and the date of service. The system will return all the TCNs that meet the
search criteria. Find the newest TCN for your claim (the larger the TCN number
the newer the claim).
• Submit a 276 HIPAA transaction and the system will return a 277 transaction
with the TCNs for the claims needed. Work with your technical staff for
completions of these transactions.
After receiving the TCN number for the claim, go to the document submission
cover sheets webpage and select the claim attachment cover sheet. Complete
the cover sheet (as first page) by entering the TCN and fax it to the number on
the cover sheet. An EDI claim will be held for 21 days waiting for any backup
submitted.
Resolving DDE claim errors
During the process of submitting a DDE claim, ProviderOne does a data check
prior to submission to verify the following required entries:
• Fields contain valid entries.
• Fields are completed.
• Questions are answered.
Errors can come in two formats. A popup window:
Or a red text message at the top of the claim screen:

62 | PROVIDERONE BILLING AND RESOURCE GUIDE
To correct such errors, review the red warnings and review the data previously
keyed in for corrections.
Entering commercial insurance information
Expand the Other Insurance Information section using the red plus sign. Then
expand the Other Payer Insurance Information section for the first insurance.
ProviderOne allows you to enter information for more than one insurance
company – note the 1 before Other Payer Insurance Information which
indicates the first commercial carrier data entered.
Do not enter Medicare or Managed Medicare (Medicare Part C) information here.
HCA does not consider them commercial insurance.
When the Other Insurance Information screen opens, skip directly to the Other
Payer Information section, and enter the name of the insurance company.
Then select the red plus expander to open the Additional Other Payer
Information section.
Enter the following:
• Enter the ID number as the Carrier Code
• Payer ID Type from the ID Type dropdown (always choose PI-Payor Identification)

63 | PROVIDERONE BILLING AND RESOURCE GUIDE
Finding the commercial insurance carrier code
ProviderOne requires use of the insurance carrier code found on the client’s
eligibility file under the Coordination of Benefits section. The carrier code in the
example below is BX08.
Then scroll down to COB Monetary Amounts field and enter the amount paid
by the insurance:
Note: If you are attaching the EOB to your claim or mailing or
faxing in the backup using the following methods, stop here.
Avoid sending in the insurance EOB with your claim
Expand the Claim Level Adjustments section:
Enter the HIPAA adjustment reason code information from the insurance EOB:
• Group Code (choose from the options)
• Claim Adjustment Reason Code (CARC - only the HIPAA reason code
number is required)
• Amount (enter a zero if billing services denied by the insurance company)
Finish filling in the rest of the claim data and submit the claim as outlined above.
You can use this process to submit services denied or paid by the primary
insurance company. ProviderOne can process the claims with these data
elements:
• The name and carrier code of the insurance company.

64 | PROVIDERONE BILLING AND RESOURCE GUIDE
• The amount paid by the insurance company (enter zero if no payment).
• The HIPAA adjustment reason codes for non-payment or denials.
The agency is requesting that providers submit both paid and denied lines on the
same claim, which can result in more efficient processing. Line level entries of TPL
payments and adjustment reason codes can be billed for more accurate payment
of commercial insurance claims via DDE. The agency will provide a resource for
line level billing through direct data entry if provider’s request assistance. For
assistance with line level HIPAA/EDI billing for third party claims, please see the
Reporting Medicare/Managed Medicare and commercial payer data on an 837
transaction fact sheet.
FQHC’s, RHC’s, and tribal billers should submit TPL amounts at header only to
correctly receive encounter payments.
For more information on billing Medicaid secondary to a commercial insurance,
see the “Billing with commercial insurance or Medicare as primary” section on the
fact sheets webpage.
Third-Party Liability (TPL) and Prior Authorization
If the client has TPL, also known as commercial insurance or private insurance,
and the service you are billing for requires prior authorization (PA) from the
agency, the agency waives the “prior” requirement in this instance. However, if
the commercial insurance denies payment for the service that required the
authorization, you must then request authorization and include a copy of the
insurance denial EOB with the request. See Completing the authorization intake
process for submitting a request.
For some programs PA is required prior to providing services regardless of the
primary payer. Examples of this could be DME supplies, dental/orthodontia, and
inpatient hospital stays. Review the specific provider guide for more details. If the
primary pays the service, then authorization is not required for the secondary
claim.
Saving a DDE claim
If interrupted during the process of entering a claim, ProviderOne allows you to
save the claim, and later retrieve the saved claim to finish and submit the claim.
Make sure to complete the following data elements before trying to save the
claim:
Provider Information
• Billing provider NPI
• Billing provider taxonomy
• Question: Is the billing provider also the rendering provider?
• Question: Is this service the result of a referral?
Subscriber/Client Information
• Client ID number
• Question: Is this a Medicare crossover claim?

65 | PROVIDERONE BILLING AND RESOURCE GUIDE
Claim Information
• Question: Is this claim accident related?
Basic service line items are not required before saving a claim.
Once all the minimum necessary data fields are completed, select Save Claim:
ProviderOne will display the following confirmation box:
Select OK to proceed or Cancel to return to the claim. When you select OK,
ProviderOne will check the claim to ensure the minimum data fields are
completed, and if so will save and close the claim.
Retrieving a saved claim
On the provider portal, select Retrieve Saved Claims:
When ProviderOne displays the Saved Claims List, select the Link icon to retrieve
a claim:
The system loads the saved claim in the professional DDE screens. Continue to
complete any required fields and submit the claim.
Once a saved claim is retrieved and submitted, the claim no longer appears in the
saved claim list.
Submitting online batch claims
From the homepage, select Online Batch Claims Submission. On the provider
portal, select Submit HIPAA Batch Transaction (837):

66 | PROVIDERONE BILLING AND RESOURCE GUIDE
Select the Upload button on the next screen:
Select the Choose File button and locate the batch file on your computer.
When the file name displays, select OK.
If the upload was successful, ProviderOne displays a confirmation page, which
you should print out and use for a reference when checking on the batch
response (997).
If sending backup documentation for a claim in the batch (a TCN is required to
do this) a completed and printed cover sheet is required. Several different types
of cover sheets are available on the document submission cover sheets webpage.
For more information on cover sheets, see Appendix H.
Special Claim Indicators (SCI)
ProviderOne has a feature that allows scanning of certain routine comments
directly into the system, without the need for manual review. To make any of the
following comments, enter “SCI=” and the corresponding letter on the list below:
• B – baby on birthing parent’s client id (can only be used the first 60 days of
baby’s life)
• F – enteral nutrition – client not eligible for WIC
• H – children with special healthcare needs
• I – involuntary treatment act (ITA) (legal status)
• K – not related to terminal illness (hospice client)
• V – voluntary treatment (legal status)
When billing Medicaid as the secondary payer using HIPAA batch files, use an
837 transaction to electronically submit the primary payer insurance information
to ProviderOne. Please follow the guidelines within the ProviderOne 837
Professional, Institutional and Dental ProviderOne 5010 companion guides.
If you are sending in backup documentation for an EDI claim, HCA holds the
claim(s) for 21 days after receiving the electronic file.

67 | PROVIDERONE BILLING AND RESOURCE GUIDE
Pitfalls
• Failing to use the National Provider Identifier (NPI) that ProviderOne has on
file.
• Failure to use a proper taxonomy code.
• Failure to include gender on the claim.
• Failing to indicate the baby’s name, birth date and gender on a newborn claim
using birthing parent’s ID.
• Forgetting to click submit on the bottom of the last popup on the DDE
screens, even if a TCN is displayed (the TCN will become invalid if you do not
submit it).
• Failure to turn off the popup blocker when using ProviderOne, which is
necessary for you to get to the final popup to select submit.
• Forgetting to click the enter key or to click outside any field when filling out
the cover sheet, as the cover sheet will not then contain the proper barcodes
and the backup will not be attached to the DDE claim in ProviderOne.
• Reusing or saving cover sheets, as each cover sheet has unique coding for the
claim the backup document is attached to.
Submitting Medicare crossover claims
Medicare crossover claims are claims for the client’s Medicare cost sharing
liability (deductible, coinsurance, or copay). This does not apply to claims denied
by Medicare, as these are not considered crossover claims.
In most cases, after processing the claim for payment, Medicare will forward the
claim electronically to ProviderOne and include a message on the Medicare
Explanation of Medicare Benefits (EOMB) stating: “This information is being sent
to either a private insurer or Medicaid.” In these cases, ProviderOne processes
crossover claims without any action on your part.
There are instances where Medicare may not forward claims to ProviderOne (i.e.,
Managed Medicare) so you may need to bill the crossover claim directly to
ProviderOne. HCA recommends billing claims electronically or using ProviderOne
DDE for faster processing. If Medicare paid, complete the Medicare fields as
shown in this section. If Medicare denied, it would require attaching a copy of the
EOMB to the claim.
You will know that Medicare has not forwarded the crossover claim to
ProviderOne if:
• It does not show up on the remittance advice (RA).
• The message “This information is being sent to either a private insurer or
Medicaid” does not show up on the EOMB from Medicare.
Reasons Medicare may not forward a crossover claim directly to ProviderOne
include:
• The patient may be a new Medicare/Medicaid enrollee and Medicare does not
yet list them as having Medicaid coverage.
• The provider billed Medicare with an NPI number ProviderOne does not have
in the system.

68 | PROVIDERONE BILLING AND RESOURCE GUIDE
• There are electronic file corruption issues.
• Managed Medicare (Medicare Part C or Medicare Advantage plans) may not
forward claims directly to ProviderOne.
See Appendix J for payment methodology information on crossover claims.
Overview of Medicare crossover process
The next section explains how each type of Medicare crossover claim is submitted
to the agency if the claim is not automatically forwarded by Medicare. Please see
Appendix J for crossover payment methodologies.

69 | PROVIDERONE BILLING AND RESOURCE GUIDE
Medicare Part B professional services
To submit crossover claims for professional services:
• If Medicare has paid all lines on the claim, submit the crossover claim to
ProviderOne.
• If Medicare has allowed and denied service lines on the claim, do not submit
paid lines with denied lines on the same claim form. This could cause a delay
in processing the claim. Submit two claims, one crossover for services
Medicare paid on and one professional claim for services Medicare denied:
o If Medicare bundled the service into another paid service line, do not split
out or unbundle to bill Medicaid.
o Attach the EOMB to the claim for services denied by Medicare.
• When Medicare is the primary payer and denies a service that is covered by
the agency with a prior authorization requirement, the agency waives the
“prior” requirement in this circumstance. Submit a request for authorization.
Attach the explanation of benefits (EOB) to the request for services denied by
Medicare.
• If Medicare applies to the deductible or makes payment on a service that
required PA, then authorization is not required for the service.
• Bill the agency on the same claim format billed to Medicare with the same
services and billed amounts.
• Bill Medicare with the appropriate taxonomy code for the claim according to
Medicare guidelines. Medicare will then forward the taxonomy on the claim
to ProviderOne.
• If billing DME rental codes that require a date span, bill Medicare with the
appropriate date span. Medicare will then forward the date span on the claim.
When submitting a DDE professional services crossover claim in ProviderOne, fill
out the additional Medicare information at the line level for each service line:
• Select the Medicare Crossover Items expander.
• Fill in the required Medicare information.
• The rest of the claim is filled out as normal.
If the Medicare Advantage or Part C Plan indicates an allowed amount for the
service but does not make a payment on the service, enter the copayment,
coinsurance, or patient responsibility as the deductible if the plan EOB indicates a
remark code of copayment for the service. ProviderOne requires a deductible
amount in this case to process the claim.

70 | PROVIDERONE BILLING AND RESOURCE GUIDE
If you bill a crossover electronically or DDE, ProviderOne does not require the
EOMB to be uploaded or sent as an attachment, unless Medicare denies the
service.
Medicare Part A institutional services
When submitting a DDE institutional crossover claim in ProviderOne, fill out the
additional Medicare information at the claim level. DDE claims do not require the
EOB.
Select Yes to indicate this claim is a crossover:
• Fill in the required Medicare information in the fields with asterisks indicated.
• The rest of the claim is filled out normally.
While claims for clients that do not have Medicare Part A or Part A benefits are
exhausted are not considered crossover claims, we have included how to bill
these claims in this section.
Part B only (no Part A), or Part A exhausted prior to
stay
Description
DRG
Per
diem
RCC
CPE
CAH
Bill Medicare Part B for qualifying services delivered
during the hospital stay
Yes
Yes
Yes
Yes
Yes
Bill ProviderOne as primary for hospital stay
Yes
Yes
Yes
Yes
Yes
Show as non-covered in ProviderOne and bill what
was billed to Medicare under Part B
No
No
Yes
Yes
Yes
Expect ProviderOne to reduce payment for the
hospital stay by what Medicare paid on the Part B bill
Yes
Yes
No
No
No

71 | PROVIDERONE BILLING AND RESOURCE GUIDE
Description
DRG
Per
diem
RCC
CPE
CAH
Expect ProviderOne to recoup payment as secondary
on Medicare Part B bill*
Yes
Yes
No*
No*
No*
Report the Part B payment on the claim in the other
payer field “Medicare Part B”
Yes
Yes
Yes
Yes
Yes
Attach Medicare Part A & B EOB to claim
Yes
Yes
Yes
Yes
Yes
Include a claim note**
Yes
Yes
Yes
Yes
Yes
ProviderOne pays by the stay (DRG claims) or the day (per diem) on other claims.
ProviderOne calculates the payment and then subtracts what Medicare has
already paid and recoups what it paid as secondary on the Medicare claim.
* ProviderOne pays line item by line item on some claims (RCC, CPE, and CAH).
ProviderOne does not pay for line items that Medicare has already paid.
**The claim note should be one of the following:
• No Part A benefits; or
• Part A benefits exhausted prior to stay
What does the agency pay the hospital?
DRG paid claims pay the allowed amount minus what Medicare paid under Part
B. When billing, enter the Part B payment amount in the TPL commercial
insurance field and indicate the primary payer as Medicare Part B.
Per Diem paid claims pay the allowed amount minus what Medicare paid under
Part B. When billing, enter the Part B payment amount in the TPL commercial
insurance field and indicate the primary payer as Medicare Part B.
RCC, CPE and CAH claims pay the allowed amount for line items covered by
Apple Health (line items usually covered by Medicare under Part A, if client were
eligible).
Medicare begins during hospital stay, or Part A
exhausts during stay
To submit a claim in situations where a client’s Medicare coverage began during
an inpatient stay, or exhausts the Part A benefit during an inpatient stay:
• Bill Medicare - per Medicare PPS Payment Manual, Chapter 3, Section 40A,
bullet 3: “The beneficiary becomes entitled after admission. The hospital may
not bill the beneficiary or other persons for days of care preceding entitlement
except for days in excess of the outlier payment.”
• ProviderOne must have a paid/billed inpatient crossover claim in the system.
• After the inpatient crossover claim is paid, bill ProviderOne the primary claim
for the entire stay:
o If billing RCC, CPE or are a CAH, list the Medicare covered day’s charges as
non-covered.

72 | PROVIDERONE BILLING AND RESOURCE GUIDE
o If billing DRG or per diem, list all services (no non-covered).
• If Part A exhausts during the stay, you must still bill Medicare for the Part B
charges.
• ProviderOne may pay something using the following formula:
o HCA allowed amount for the entire stay, minus Medicare paid, minus HCA
crossover payments
• Add the following claim note:
o “Part A benefits exhausted during stay;” or
o “Medicare Part A coverage began during the stay;” or
o Enter the Part A start date, or the date benefits were exhausted in the
occurrence fields using occurrence code A3.
• Attach Part A and Part B EOMB.
These claims can be very complex and are addressed on a case-by-case basis and
sometimes it is necessary for HCA to contact the biller for additional information.
Medicare Advantage plans (Part C)
Some Medicare clients have elected to enroll in a Medicare HMO plan called a
Medicare Advantage Plan (Part C) and you are required to bill these Medicare
Advantage Plans instead of FFS Medicare. The Managed Medicare – Medicare
Advantage Plan is the primary payer and HCA does not consider this as
commercial insurance.
• To receive payment, it is necessary to follow the billing guidelines established
by the Managed Medicare – Medicare Advantage (Part C) plans prior to billing
ProviderOne.
• After the Medicare Advantage plan processes the claim, submit the claim to
ProviderOne as a Medicare crossover claim.
o Use the same claim format used to bill the Medicare Advantage plan,
unless billing a crossover for an FQHC or RHC, in which case the claim
format to use is the institutional format.
o Make sure the services and billed amounts match what was billed to the
Medicare Advantage plan (DDE claims do not require the EOB to be sent
with the claim).
• You must submit the Medicare Advantage claim within six months of the
Medicare Advantage payment date.
• If Medicare Advantage is the primary payer and denies a service that is
covered by the agency with a prior authorization requirement, the agency
waives the “prior” requirement in this circumstance. Submit a request for
authorization. Attach the EOB to the request for services denied by Medicare.
• If the Medicare Advantage Plan pays the service, then PA is not required.

73 | PROVIDERONE BILLING AND RESOURCE GUIDE
Billing for managed Medicare – Medicare Advantage (Part C) plans
Providers must submit claims for capitated copayments for the Medicare Part C
plan as a crossover claim type (both professional and institutional claims).
If there is not a Medicare (plan) allowed amount, enter the sum of payment +
copayment + coinsurance + deductible as the Medicare Allowed Amount.
• If there is no amount for an entry, just add together the entries that do have
an amount.
• Finish filling in the other amounts (even if these amounts were used to
calculate an allowed amount).
• Enter a zero (0) in any other fields without a value.
• If the user entered a zero (0) in the Medicare Paid field, then enter either the
Medicare Co-payment or Medicare Deductible amount (whichever is
applicable).
• “Managed Medicare” comments are not required on the claim.
Claims with a coinsurance, deductible, or a non-capitated copayment balance
due on a claim must be billed as follows:
• Professional services
o Bill the claim paid by the Part C plan as a crossover claim.
o If the Part C plan lists a copay amount but no coinsurance amount, enter
the copay amount in the coinsurance field on the crossover claim
submitted to ProviderOne.
o If the Medicare Advantage or Part C plan indicates an allowed amount for
the service but does not make a payment on the service, enter the
copayment, coinsurance, or patient responsibility as the deductible if the
plan EOB indicates a remark code of copayment for the service.
▪ ProviderOne requires a deductible amount in this case to process the
claim.
▪ If the Medicare Advantage claim includes both allowed and denied
service lines on the claim, do not submit paid lines with denied lines to
ProviderOne on the same claim; you must submit a crossover claim for
services Medicare paid, and a separate claim for services Medicare
denied attaching the EOMB to the claim.
o If Medicare bundled the service into another paid service line, do not split
out or unbundle to bill Medicaid.
o If Medicare Advantage denies a service on a claim, ProviderOne may or
may not make a payment on the service, depending on the reason for the
Medicare Advantage plan denial.

74 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Institutional Services:
o Follow the directions above for sending a Part C plan institutional
crossover claim, except you cannot split out specific lines denied by the
Part C plan to bill a separate claim. Institutional claims are processed as
one entire claim.
QMB – Medicare Only clients
QMB – Medicare Only clients have a limited Benefit Service Package which only
pays secondary to Medicare and has no independent scope of care.
QMB-only payment methodology is as follows:
• If Medicare or the Medicare Advantage plan and ProviderOne cover the
service, ProviderOne pays only the client’s cost sharing liability (deductible,
and/or coinsurance, and/or copayment) up to the Apple Health allowed
amount.
• Payment is based on the ProviderOne allowed amounts minus any prior
payment made by Medicare or the Medicare Advantage plan. In these cases,
ProviderOne considers the crossover claim paid in full.
• If Apple Health does not cover a service, ProviderOne will use a CMS
approved negotiated rate or Medicare’s allowed amount in the place of HCA’s
allowed amount.
Discrepancies, disputes, protests, or justifications for a higher fee or payment for
any claim should be directed to Medicare or the Medicare Advantage plan. If
Medicare or the Medicare Advantage plan adjusts the payment and the claim has
previously been paid, submit an adjustment request to ProviderOne. Submit a
new claim if the original claim was denied.
Backup documentation for Medicare crossover claims
For crossover claim billing clarification, HCA has specific requirements for the
EOMB submitted with the claim.
Header (claim) level information on the EOMB must include all the following:
• Medicare (or the Part C plan) as the clearly identified payer
• The Medicare claim paid or process date
• The client’s name (if not in the column level)
• Medicare reason codes with descriptions
• Text in font size 11 or greater
Column level labels on the EOMB for professional claims must include all the
following:
• Client name
• Date of service
• Number of service units (whole numbers only)
• Procedure codes
• Modifiers

75 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Billed amount
• Allowed amount
• Deductible
• Amount paid by Medicare
• Medicare reason codes with descriptions
• Text that is font size 11 or greater
Column level labels on the EOMB for the institutional claim must include all the
following:
• Client name
• From and through dates of service
• Billed amount
• Deductible
• Co-insurance
• Amount paid by Medicare
• Medicare reason codes with descriptions
• Text that is font size 11 or greater
• Rural Health Center (RHC) and Federally Qualified Health Center (FQHC)
providers must include their per diem rate
Claims for services denied by Medicare with backup
When Medicare or the Part C plan denies services that can be billed to Medicaid,
the above criteria apply to the required EOB sent with the claim.
Medicare Prescription Drug Program
For more information on the Medicare Prescription Drug Program, review the
Prescription Drug Program provider guide.
Pitfalls
• Billing Medicare with an NPI that has not been reported to the agency.
ProviderOne cannot identify the provider when these claims are forwarded by
Medicare.
• The claim billed to Medicare does not match the claim billed to ProviderOne.
• If a Medicare exhaust issue, failing to indicate when the benefit exhausted in
the claim note or occurrence code.
• The coding and dollar amount billed on the claim to Medicare does not match
the coding and dollar amount on the claim billed to ProviderOne.
• Failing to bill the paid Part C plan claim as a crossover claim type.
• If Medicare denies a service, failing to submit the claim to ProviderOne
without the Medicare EOB.

76 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Sending an EOB with the claim that does not indicate Medicare (or a Part C
plan) as the payer or other missing required information.
Claim status
ProviderOne allows several options to search for a claim’s status. You may want
to check a claim because:
• A claim has been submitted and ProviderOne has not responded.
• You are trying to rebill some older claims and need the Transaction Control
Number (TCN) to prove timely submission of the original claim.
• You are searching for a claim because your accounts receivable system does
not yet show a posted payment.
The easiest method to find claims in ProviderOne is to use the claim inquiry
option in the ProviderOne portal.
Select the EXT Provider Claims/Payment Status Checker or EXT Provider Super
User profile, and select Claim Inquiry on the provider portal:
Select the appropriate NPI from the dropdown box and enter available
information in the remaining fields before selecting Submit. The bullets at the
top left of the box describe the various combinations of search criteria you can
use to find a claim. The easiest method is to search by TCN.
You may want to record each TCN generated when submitting claims in case you
have a need to check the claim using Claim Inquiry later.
• You may request status for claims processed within the past four years.
• The claim service period from and to date range cannot be greater than three
months.
To find a claim (or a list of claims) use the client ID and the oldest from date of
service on the claim. ProviderOne will display a list of all claims for that date of
service.

77 | PROVIDERONE BILLING AND RESOURCE GUIDE
After selecting Submit, select the blue Transaction Control Number (TCN)
hyperlink to view the claim:
See Appendix K for instructions on checking claim status via the Interactive Voice
Response (IVR).
Pitfalls
• Calling the HCA Customer Service Center to check on the status of a claim.
Providers can easily check on a claim status using ProviderOne or the
Interactive Voice Response (IVR) without assistance.
Timeliness
The initial timely filing deadline is 365 days from the date of service, but you may
resubmit, modify, or adjust any timely initial claim (except prescription drug
claims) for a period of 24 months from the date of service.
Exceptions to this rule are:
• Medicare crossover claims must be submitted initially within six months of the
Medicare processing date, and for resubmissions, voids, or adjustments within
two years from the “from” date of service.
• Prescription drug claims must be resubmitted, modified, or adjusted within 15
months from the date of service.
For more information, see WAC 182-502-0150.
Adjusting, resubmitting, or voiding a claim
ProviderOne does not process claim appeals. If a claim has any paid amount (i.e.,
is not in denied status) you must submit an adjustment. If a claim was denied,
verify the denial reason(s), and correct the claim for resubmission.
Adjust a paid claim when:
• A billing error was made (e.g., wrong client, billed amount, tooth number, etc.).
• The claim contained multiple surgical procedure codes, and one of the
procedure codes denied or paid incorrectly.
• The claim was overpaid (this may be a void claim).
Denied claims can be resubmitted using the ProviderOne resubmit feature and
correcting the error that caused your claim to deny. ProviderOne does not post
duplicate denials against previously denied claims. ProviderOne will not allow
adjusting or voiding of a denied claim.
There are various methods to modify, adjust, or void claims depending on the
billing format. If the claim was paid (or partially paid) then you must submit an

78 | PROVIDERONE BILLING AND RESOURCE GUIDE
adjustment to make any corrections or modifications using the following
guidelines:
• For DDE adjustments (regardless of submission method used for the original
claim), log into ProviderOne using either the EXT Provider Claims Submitter or
EXT Provider Super User profile and use the online Claim Adjustment/Void
option.
• For electronic claims, submit a HIPAA batch transaction claim using a
frequency 7 to adjust/replace the original claim or a frequency 8 to void the
original claim. Follow the ProviderOne companion guide rules for submitting
frequency 7 (adjustment) or 8 (void) transactions.
When an adjustment and resubmission of a claim is required after the one-year
timely filing rule, ProviderOne requires proof of timely filing to resubmit your
claim.
Locate the timely Transaction Control Number (TCN) using the ProviderOne
“claim status” search option or the remittance advice, and follow these guidelines:
• For a DDE claim denial, resubmit the original claim using the Resubmit
Denied/Voided Claim, which will automatically link the old claim to your new
claim to prove timeliness without the need for you to enter a timely TCN.
• For DDE adjustments on paid claims, use the Claim Adjustment/Void function
and ProviderOne will similarly link the original timely TCN to your adjustment
without the need for you to enter a timely TCN.
• For HIPAA batch claim transactions, see ProviderOne 5010 companion guides
for entering the timely TCN number.
If an original claim was adjusted or replaced and it is necessary to adjust or
replace it again, you must use the most recent TCN number in the claim trail.
ProviderOne will only allow one adjustment for each TCN. Once a claim has been
adjusted or resubmitted, it cannot be adjusted or resubmitted again.
The general adjustment process
The ProviderOne system assigns an 18-digit Transaction Control Number (TCN),
also referred to as a claim number, to each claim received. The TCN will also
appear on your remittance advice (RA).

79 | PROVIDERONE BILLING AND RESOURCE GUIDE
Reading the TCN
Each of the 18 digits in the claim number (TCN) has a reserved meaning. The
table below describes each (e.g., 202318400000001000):
2
A
0
B
23184
C
0
D
0000001
E
000
F
A: Claim medium indicator
• 0 – Not used
• 1 – Paper
• 2 – Direct data entry (DDE web submission)
• 3 –Electronic (X12)
• 4 – System generated
• 5 – DDE social service claims
• 6 – Non-HIPAA compliant social service
electronic batch submission (includes
template).
• 7 – Social service repetitive/client
payment/adjustments or void
• 8 – Reserved for future use.
• 9 – Represents a claim billed in the legacy (old)
payment system (21 digits long).
B: Type of claim
Placeholder number that could be one of the
following:
• 0 – Medical
• 1 – Pharmacy
• 2 – Crossover or medical
• 3 – Medical encounter
• 4 – Pharmacy encounter
• 5 – Social services
• 6 – Social service shadow claim type. System
generated daily/removed nightly from system.
Does not produce payable claim. Provider and
staff, please disregard.
• 7 – 9 Reserved for future use.
C: Batch date
• First two digits are the year (23).
• The next 3 numbers are the Julian day of the
year with 184 being July 2nd. ProviderOne uses
the Julian calendar to record dates claims were
received. The Julian calendar is simply a
continuous counting of the days of the year
from 1 to 365. Leap years add an additional
day and use 1-366.
D: Adjustment indicator
• 0 – Original claim
• 1 – Adjustment credit
• 2 – Adjustment debit
E: Claim sequence number
• Sequential counting of claims each day starting
with 0000001.
• Allows claim counting to reach almost 10
million (9,999,999) claims daily.
F: Line number
• The claim level number will be 000.
• Each claim line also has a TCN number. The
line number will start with 001 sequentially
(e.g., 002 for line 2, etc.) for each new claim line
(HIPAA Transactions can have up to 999 lines).

80 | PROVIDERONE BILLING AND RESOURCE GUIDE
Adjusting or Voiding DDE claims
Select Claim Adjustment/Void from the Provider Portal:
At the search screen enter the required information to find the claim to adjust or
void and select Submit:
Note: Per WAC 182-502-0150 claims can only be
adjusted/voided in ProviderOne 24 months from the date of
service. Prescription drug claims have only 15 months.
The system will then display claim(s) based on the search criteria.
To adjust a paid claim, select the box next to the TCN and click the Adjust button
in the upper left hand corner. The claim will display in the DDE screen with the
values of the selected claim populated. Make the necessary changes then
resubmit the adjustment request to ProviderOne for processing. The system will
go through the same final steps of a claim submission and will ask if you need to
attach backup information.

81 | PROVIDERONE BILLING AND RESOURCE GUIDE
Remember to select Submit on the Submitted Claim Details screen to finish
sending in the resubmitted claim. ProviderOne assigns a new TCN to the claim
after resubmission. There will be two TCN’s associated to the adjustment:
• A TCN with a negative amount representing the takeback of the original
payment (credit), and
• A TCN representing the new corrected claim (debit).
The HIPAA adjustment reason code of 129 will appear in the last column on the
remittance advice associated with the credit transaction.
ProviderOne allows you to give a payment back by simply voiding a claim. To
void a claim, click the Void Claim button in the upper left-hand corner of the
screen.
ProviderOne displays the claim data on the DDE screen, but all the values are
grayed out in the display, meaning no changes can be made.
Select Submit and the void will be sent to ProviderOne for processing. The claim
will appear as a credit on the remittance advice. There will be one TCN associated
to a void – a TCN with a negative amount representing the takeback of the
original payment (credit). The HIPAA adjustment reason code of 129 will appear
in the last column on the remittance advice associated with the credit transaction.
If a provider is voiding/canceling a claim for an overpayment, there are two
options available:
1. Void the claim and the agency will recoup the claim and deduct the excess
amount from future payments until the overpayment is satisfied.
2. Issue a refund check payable to the Health Care Authority, attach a copy of
the RA showing the paid claim and include a brief explanation for the refund.
Mail to:
THE HEALTH CARE AUTHORITY
FINANCE DIVISION
PO BOX 9501
OLYMPIA WA 98507-9501
The billing time periods do not apply to overpayments that the provider must
refund to the agency. After the allotted time periods, a provider may not refund
overpayments to the agency by claim adjustment. The provider must refund
overpayments to the agency by a negotiable financial instrument such as a bank
check (see WAC 182-502-0150 (8)).
The adjusted/replaced claim will appear on the RA in the adjustment claim
section as two transactions:
1. The original claim; and
2. The replacement claim
The claim paid amount is adjusted based on the adjustment request and the
adjusted amount is reflected in the total payment. See the section on the
remittance advice for a complete explanation about the RA.

82 | PROVIDERONE BILLING AND RESOURCE GUIDE
Note: When a claim is voided, the agency will recover
the amount originally paid from the next total payment
and the voided claim will appear on the RA as only one
transaction. Voided claims can be resubmitted by using
the credit TCN.
Resubmitting denied or voided DDE claims
Select Resubmit Denied/Voided Claim from the provider portal:
Search for the claim by entering the appropriate information then select Submit:
ProviderOne will display the claim list screen. Select the box next to the TCN of
the claim to be resubmitted then select Retrieve in the upper left-hand corner.
The claim will display in the DDE screen with the values of the selected claim in
the fields and will indicate the type of claim.
Make any necessary changes to the claim using the same procedure as described
above in the Adjusting a Claim section. Upon completing the changes, submit the
claim to ProviderOne for processing. The system will go through the same final
steps of a claim submission asking if you want to send backup documentation,
etc.

83 | PROVIDERONE BILLING AND RESOURCE GUIDE
Pitfalls
• Adjusting the wrong claim or claim line, which may result in unexpected
results with the claim and payment.
• Failing to select Submit on the Submitted Claim Details screen will result in
the claim not being sent to ProviderOne for processing.
Claim templates
ProviderOne allows you to create and save a template of a claim for services that
you may be billing for a client on a weekly, bi-weekly, or monthly basis. When
creating a DDE template, you can add as much claim information to the template
as needed, however the system does require a minimum of information to be
able to save the template.
The minimum required information is:
• A template name
• Answers to the questions on the DDE screen; and
• If a data field or section is open or expanded, then additional information may
be required.
You can use templates repeatedly to create claims. The template can be edited,
resaved, or deleted if no longer useful. You can create and save as many
templates as needed.
Creating a template
Log into ProviderOne with the EXT Provider Claims Submitter or EXT Provider
Super User profile and select Manage Templates which will open the following
screen:
First, start building a template by choosing which type of template is desired then
select Add.
Create a name for the template. Use a name that describes a service or use the
client’s name. It is best not to use a template name that uses alpha/numeric
characters that are common to all templates, which would make the template
difficult to sort from a list of many templates.

84 | PROVIDERONE BILLING AND RESOURCE GUIDE
Fill in as many data fields as possible. If the template is for a client that receives
specific services monthly, then fill in all fields except the dates of service. If the
template is service-specific, then fill in all the service information and leave off
the client information and dates of service. When building and saving a template,
ProviderOne will ignore some of the system rules (i.e., not all required fields need
data).
Once the template is complete and ready to save, select Save Template.
The system will ask to verify saving the template:
ProviderOne may return the message, “Warning: Template Name Already Exists,
please enter a unique name”. Two things may cause this warning:
• A template has already been created with this name under your domain; or
• ProviderOne found the template name already existed in history.
If the template is truly a new one for the domain, add a number to the end of the
template name and attempt to save again.
After selecting OK, ProviderOne returns to the Create a Claim Template screen
adding the template to the list:

85 | PROVIDERONE BILLING AND RESOURCE GUIDE
Add as many templates as necessary, either by creating new ones using the
above method, or copying and editing a saved template.
Copying a template
To copy a template, click on the check box next to the template name and click
on Save As/Copy:
The system now displays the DDE screen with all the template information except
the template name. Name this template and change any data as needed then
save the template. Build as many templates as required using this method.
Viewing a template
To view a template, click on the check box next to the template name and click
the View button:
The system now displays the DDE screen with the template information and all
the template data will be grayed out and cannot be edited.
Deleting a template
To delete a template, click on the check box next to the template name click the
Delete button:
A popup will appear asking if you are sure you want to delete the selected
record. Click OK to delete the template.
Editing a template
To edit a template, click on the check box next to the template name and click
the Edit button:

86 | PROVIDERONE BILLING AND RESOURCE GUIDE
The system now displays the DDE screen with the template information available
to edit with changes or updates as needed.
Pitfalls
• Choosing the wrong profile after logging into ProviderOne.
• Choosing the wrong claim type for the template.
• Using common starting characters in naming the template. Makes it difficult
to sort and find a template on a large list.
Submitting a template claim or batch of template
claims
Providers that bill reoccurring services for a client or clients may want to use a
claim template to create and submit those claims.
ProviderOne also allows institutional providers to build batches of templates into
a batch of claims instead of submitting a single claim template one at a time.
Submitting a single claim from a template
Log in to ProviderOne using either the EXT Provider Claims Submitter or EXT
Provider Super User profile.
From the provider portal, select Create Claims from Saved Templates:
ProviderOne will display the Create Claim from Saved Templates List screen.
Click on the template name to load the template into the DDE screen.
• If there are several templates listed, use the Filter By boxes to find a specific
template, or
• Use the sort tools (little diamonds/carets) under each column heading
which sorts from top to bottom or bottom to top.

87 | PROVIDERONE BILLING AND RESOURCE GUIDE
At the DDE screen finish filling in the claim data. When the data entry is
completed, save the claim, or submit the claim to ProviderOne. If submitting the
claim, ProviderOne will ask if backup is being sent. Attach backup, if necessary, by
clicking Ok, or Cancel if no backup is needed.
Click the Submit button to submit the claim.
Go back to the Create Claim from Saved Templates List screen if you want to
submit another claim using a template.
Submitting a batch of template claims
ProviderOne can identify and gather a group of claim templates together to
create a batch of templates for submission into the system as a batch of claims.
This process has these basic requirements:
• All claim types must be the same in the batch (i.e., professional, dental, or
institutional).
• All batch templates will be for the same date of service (or date span).
• The billed amount could be the same on each claim template [based on the
date(s) of service].
• Each claim template units will be the same [calculated based on the date(s) of
service].
A detailed explanation of the process is beyond the capacity of this publication;
however the ProviderOne Managing Claims system manual has a complete
overview of the process. Nursing Home providers submitting institutional claims
have a detailed webinar and presentation slide show demonstrating the complete
process. Other provider types wanting to use the process would follow the same
steps; however, they may be using a different claim format.
To submit a batch of template claims, log into ProviderOne and click on Manage
Templates.
At the Claims Template List screen there are three options to create a batch of
claim templates:
• Create Batch
• Create Batch All
• Auto Batch

88 | PROVIDERONE BILLING AND RESOURCE GUIDE
At the Batch Claim Attributes screen assign the from and to dates of service then
build the batch.
Each batch is assigned a batch number.
At the portal page switch to the Manage Batch Claim Submission hyperlink.
At the Batch Claim Submission Status List page, check the status of a batch. The
status can be:
• Waiting
• In Process
• Failed in Validation
• Passed Validation
• Submitted for Claims Loading
Only template batches that have passed validation can be submitted. Submitted
batches are now in Submitted for Claims Loading status. Claims are assigned a
TCN and begin processing in ProviderOne. This template batch will be auto
purged from the list page.
Pitfalls
• Forgetting to change a data element that needed changing on a template.
This could result in a denied claim or an overpaid claim.
• Trying to submit a batch of templates that are different claim types.
• Not keeping track of the batch number for a specific template batch service.
• Trying to submit a batch of templates that have not passed validation.

89 | PROVIDERONE BILLING AND RESOURCE GUIDE
The remittance advice
Understanding claim status
The Remittance Advice (RA) provides detail about paid, denied, adjusted and in-
process claims submitted to ProviderOne.
ProviderOne makes weekly payments every Monday. Claim submission cutoff in
the payment system is Tuesday at 5 p.m. Pacific Time to make payment the
following Monday for a “clean” claim. Clean claims submitted after cutoff will be
paid the following payment cycle on the following Monday. The agency sends
out the RA weekly and always follows Monday’s payment cycle.
Clean claims are claims that have all the required data elements and do not
conflict with Apple Health program policies.
Claims may arrive in the payment system before 5:00 PM on Tuesday but may not
process until after the cutoff time. These claims will miss the next Monday
payment and be paid the following payment cycle on the following Monday.
The RA is broken down into the following sections:
• RA newsletter
• RA summary
• Paid claims
• Denied claims
• In-process claims
• Adjusted claims
Disclaimer
A contract, known as the Core Provider Agreement (CPA), governs the
relationship between HCA and Apple Health providers. The CPA’s terms and
conditions incorporate federal laws, rules and regulations, state law, Apple Health
rules and regulations, and HCA program policies, numbered memoranda, and
provider guides, including this guide. You must submit a claim in accordance with
HCA rules, policies, numbered memoranda, and provider guides in effect at the
time you provided the service.
Retrieving the RA
There are two ways to obtain the Remittance Advice (RA). You will want to select
which of the two methods that bests suits your business needs, PDF file or
electronic 835. This guide only covers processes related to using the ProviderOne
portal, not HIPAA EDI transactions. Please review the HIPAA webpage for the 835
Companion Guide and/or HIPAA help desk contact information.
To retrieve the RA through the ProviderOne portal, log in to ProviderOne and
choose the EXT Provider Claims/Payment Status Checker or EXT Provider Super
User profile. Select View Payment (RHCs and FQHCs select View Capitation
Payment to view enhancement/managed care RAs):

90 | PROVIDERONE BILLING AND RESOURCE GUIDE
The segment below will be displayed.
Select the RA/ETRR Number in the first column to review a PDF of the RA.
ProviderOne will hold four years of RAs generated in ProviderOne.
Pitfalls
• Failing to use the correct user profile. This may result in not being able to
retrieve the RA in ProviderOne.
• Logging into the wrong domain. This may result in not finding the RA
matching your payment.
Reviewing updates and key messages
ProviderOne uses the RA newsletter to communicate changes and new
information. Taking the time to review this section will ensure you see the most
current and important changes or messages.
Viewing the first page of the RA:

91 | PROVIDERONE BILLING AND RESOURCE GUIDE
The following information displays:
A. Provider demographic information
B. The number assigned to the RA.
C. The NPI provider number used in billing ProviderOne.
D. The payment date and the date this RA was prepared.
E. The main body of this RA page is our newsletter with important provider
update information (sometimes specific to certain provider groups).
You can call the IVR to check your warrant (check) amount (see Appendix L).
Reviewing the summary page
The summary page lists all claim payments by sections and all other payment and
adjustment amounts.
You can find out the total amount of your Electronic Funds Transfer (EFT) or
warrant (check) and how ProviderOne determined that amount.
The following information displays:
A. Check number and date of payment.
B. Total payment received on the check (warrant) or EFT.
C. Total of the paid claims on this RA
D. Deduction due to a claim adjustment from the total paid amount.
E. Deduction due to an overpayment (NOC Referred to CARS)
F. Deduction due to a provider adjustment (P1OFF Recoupment)
Adjustment types
The summary page of the RA can show several different adjustment type codes.
The adjustment type is a result of your actions on a claim(s), or an action initiated
by the ProviderOne system. The following table indicates the adjustment type
and explains what they are:

92 | PROVIDERONE BILLING AND RESOURCE GUIDE
Adjustment type
Definition
P1Off invoice
This occurs when you owe HCA payment due
to adjustments exceeding payments. In these
cases, HCA creates an account receivable,
which is satisfied by either:
• Taking payment from a future paid claim,
or
• Through a receivable sent to CARS
(Collections and Accounts Receivable
System) to initiate the recovery.
The latter only happens if the P1OFF is not
satisfied after six months, at which point it
becomes an ATC Referred to CARS (see
below).
P1Off recoupment
This identifies the payments used to satisfy
HCA’s accounts receivable. This typically posts
immediately following a P1OFF invoice line.
NOC invoice
A Non-Offset receivable is created for transfer
to CARS. The creation of this receivable can be
a result of voiding a claim or net negatively
adjusting a claim. These are caused by:
• Adjusting an old claim
• Payment Review Program (PRP)
recoupment of an old claim
• HCA doing a mass adjustment which
affects old claims
NOC referred to CARS
A claim is adjusted but ProviderOne will not
use paid claims to satisfy the amount owed.
Instead, these amounts are referred directly to
OFR for recovery.
CASH RECEIVED invoice
HCA has received a check from you and now
the claims are adjusted to account for the
cash received.
CASH RECEIVED cash application
You sent HCA a check for money owed to the
agency which was applied to the receivable in
the accounting system.
ATC referred to CARS
ProviderOne tried to recover money you owed
HCA but did not have a sufficient total of
claim payments post in the last six months to
satisfy the debt. At this point the remaining
balance is submitted to the OFR for collection.

93 | PROVIDERONE BILLING AND RESOURCE GUIDE
Adjustment type
Definition
COFF invoice
CARS creates a CARS Offset Invoice in OFIN
for each request sent to ProviderOne from
CARS. Direct all questions about COFF offsets
to OFR at 1-800-562-6114.
COFF recoupment
OFR accepts a receivable to collect, and OFR
sends back a request to take other payments
for paid claims from you to satisfy the
receivable. There should be other paid claims
on the RA, and some of those payments go to
OFR to help satisfy the debt.
COFF referred to CARS
ProviderOne tried to recover a dollar amount
you owed HCA but did not have a sufficient
total of claim payments post in the last six
months to satisfy the debt. The balance owed
is sent to the OFR for collection.
Legend for above acronyms:
• OFR: Office of Financial Recovery
• OFIN: Oracle Financial System
• CARS: Collections and Accounts Receivable System (OFR recovery)
• NOC: Non-Offset to CARS
• ATC: Automatic Transfer to CARS
• COFF: CARS Offset (lien)
• P1OFF: ProviderOne Offset (claim adjustment)
FIN invoice number
Each adjustment type displayed on the RA generates an invoice account.
ProviderOne assigns a Financial Invoice Number (FIN) to each account that
displays on the RA. Only finance staff have access to these account numbers in the
system. Updates to ProviderOne now provide the original TCN/claim number
along with the invoice number to help identify the original payment involved in
the adjustment. Use this TCN to determine the client ID and the date of service the
adjustment occurred on.
Most common adjustment types
The most common adjustment type is the P1OFF which is an offset resulting from
a claim (or several claims) being net negatively adjusted or voided.
• A net negative adjustment is when a claim is originally paid then adjusted and
the adjusted claim gets denied.
• Adjusting a claim usually creates a “credit,” then a “debit” repays the amount
on the same RA and the system does not generate a P1OFF. ProviderOne is

94 | PROVIDERONE BILLING AND RESOURCE GUIDE
supposed to credit, and debit adjusted claims on the same RA in order not to
create unnecessary P1OFF accounts.
• A voided claim will create a P1OFF which may or may not be recouped on the
same RA.
Finding P1OFF invoice claim(s)
The original claim number that was involved in the adjustment appears in the FIN
Invoice Number column related to the P1OFF. Use this claim number to
determine the client and date of service for this adjustment. If there are multiple
P1OFFs listed, there is a possibility that they could carry over onto the
subsequent weeks’ RA, until the debt(s) owed is satisfied.
Satisfying P1OFF adjustments
P1OFF invoices are cleared when enough new claim payments are generated for
the RA reporting period. Clearing a P1OFF invoice requires that two transactions
display on the summary page:
• The P1OFF – Invoice which is the amount owed the state; and
• The P1OFF – Recoupment which is the amount taken from the new claim
payments to satisfy the offset amount.
The RA will display the total recoupment amount as the total adjustment amount
at the bottom of the adjustment type list side of the summary page.
Calculating the P1OFF dollar amount
Sometimes the P1OFF recoupment amount is not fully satisfied by the new claim
payment amounts so ProviderOne carries the balance forward to the next RA as a
new P1OFF invoice amount. The new P1OFF invoice amount does not match any
claim paid amount, but the FIN Invoice Number and the associated TCN can be
used to track the client and date of service the adjustment is for. This new P1OFF
invoice amount will be satisfied with new claim payments generated in the
ProviderOne system.
What to do if the dollar amounts still do not match
It can be difficult to track claim payments, P1OFF recoupments, and the actual
check generated for the week. If there were a large amount of P1OFF invoices,
they could carry over onto several RAs and all those RA summary pages are
needed to balance actual payments. All the figures should eventually balance out:
• Claim payment(s) plus
• Positive or negative adjusted claim amounts, total then minus
• Total adjustment amount, equals
• Actual check amount
Cash refunds
You can refund overpaid claims by sending in a check. These show up on the RA
as CASH RECEIVED adjustment types.
Other adjustment types
Other adjustment types may occur when ProviderOne recoups claims:
• For non-compliance to program rules

95 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Overpayments
• A P1OFF – invoice over 6 months old; or
• COFF invoice
• Other adjustment reasons
A letter requesting payment from you usually accompanies these other
adjustment types.
Failing to review any payment adjustments, which could be mistaken as an
underpayment or an overpayment by the agency.
Pitfalls
Failing to review any payment adjustments, which could be mistaken as an
underpayment or an overpayment by the agency.
Reviewing paid claims
The remittance advice shows all claims generated or in process during the
previous week, divided into paid, denied, adjusted, and in process claims.
Review the paid claims section(s):
• There may be more than one paid claim section depending upon what
services were provided and have been paid. For example, if there were billings
for children’s Early and Periodic Screening, Diagnosis and Treatment exams
(EPSDT) there would be a “Paid claims – EPSDT claims” section that is separate
from the “Paid claims – professional claims” section.
• Be aware of the possibility of multiple paid claim sections to ensure that
account payments for all paid claims listed on the RA get posted.
Example of professional (physician) paid services:
Some paid claims may also contain denied service lines. These will also be
displayed in the paid claims section within the specific claim that was paid but
will have the same remark codes and adjustment reason codes as denials in the
denied section.

96 | PROVIDERONE BILLING AND RESOURCE GUIDE
Pitfalls
• Missing a paid claim section. This may result in an unnecessary call to the
Medical Assistance Customer Service Center (MACSC), or a claim rebill that
causes extra work for both you and HCA.
Reviewing denied claims
Locate the denied claims section on the RA:
Look for the HIPAA adjustment reason and remark codes to determine why the
claims denied. Every denied claim will have a claim adjustment reason code.
Some will also have a remittance advice remark code for further information. If
you are unable to understand the reasons a claim denied, a customer service
representative can assist at the Medical Assistance Customer Service Center
(MACSC) at 1-800-562-3022. They can assist in reprocessing your claim if
ProviderOne denied the claim in error. You can also submit a Contact Us email for
assistance on denied claims.
After reviewing the adjustment reason codes and remark codes, determine the
denial reason and if the claim can be corrected. Resubmit the claim when:
• The entire claim is denied.
• An individual line on a professional/dental service multiple line claim is
denied. This line can usually be rebilled as a new claim.
• The paid professional/dental claim can be adjusted to correct an error on the
denied line of a multiple line claim.
You have two years to get the claim rebilled or resubmitted, referencing the
original claim number. Medicare crossover claims must be submitted initially
within six months of Medicare’s process date, with two years from Medicare’s
“from” date of service for resubmissions.
Pitfalls
• Missing a denied claim section on the RA.
• Overlooking a claim or line that needs to be rebilled or resubmitted and delay
payment.
• Overlooking rebilling or resubmitting a claim or line until it is past the timely
billing period.
• Overlooking rebilling or resubmitting a claim until it is past the primary
payer’s timely billing period.
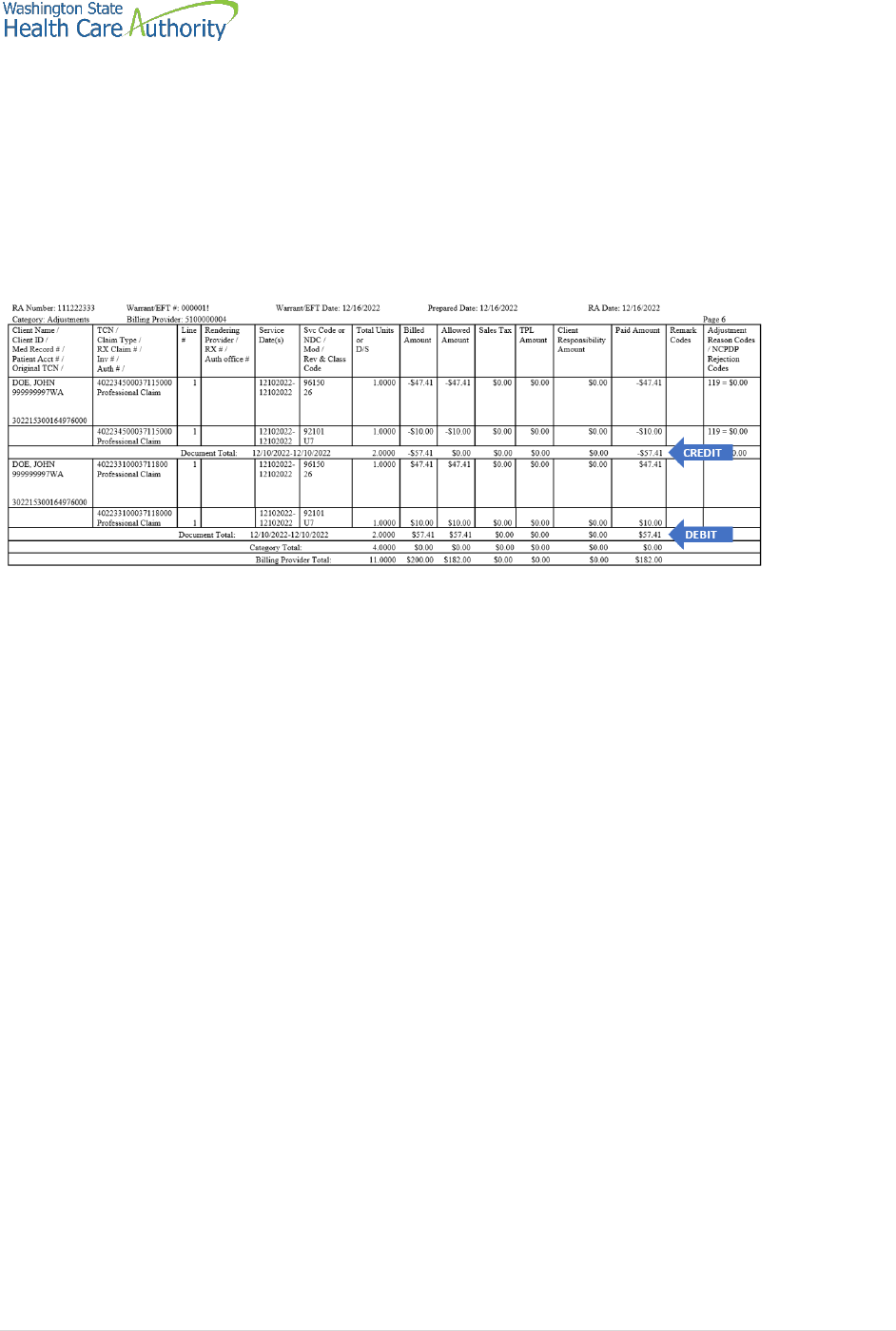
97 | PROVIDERONE BILLING AND RESOURCE GUIDE
Reviewing adjusted claims
This section of the RA lists claims that have been adjusted or modified after the
original submission. You may have sent in an adjustment request to correct a
paid claim or ProviderOne initiated an adjustment. Adjusted claims may or may
not affect the amount of the payment for services, depending on the changes
made.
Page through the RA until the section category labeled “adjustments” is found:
• Adjustments to modify or correct claim billing errors utilize these basic
accounting principles and will have two transactions displayed on the RA:
o The Credit transaction is a copy of the original claim with dollar amounts
listed as a negative.
o The Debit transaction is a repayment that displays the modification or
corrections made to the original claim and the associated repayment dollar
amounts.
o ProviderOne will then subtract the original payment amount from the
adjusted claim payment amount and include this difference in the current
payment amount.
The adjustment to the original claim may reduce the adjusted claim payment
resulting in a subtraction in the current payment amount. If you owe more money
from adjustments to claims than they earned from other paid claims on the
current RA, you may be in a “credit balance” situation. HCA will wait until you
have been paid enough through subsequent billings to satisfy the “credit
balance” before making an actual payment. An RA will be made available weekly
in any case.
Pitfalls
• Not reviewing the adjustment section, as there may be paid and denied claims
in this section.
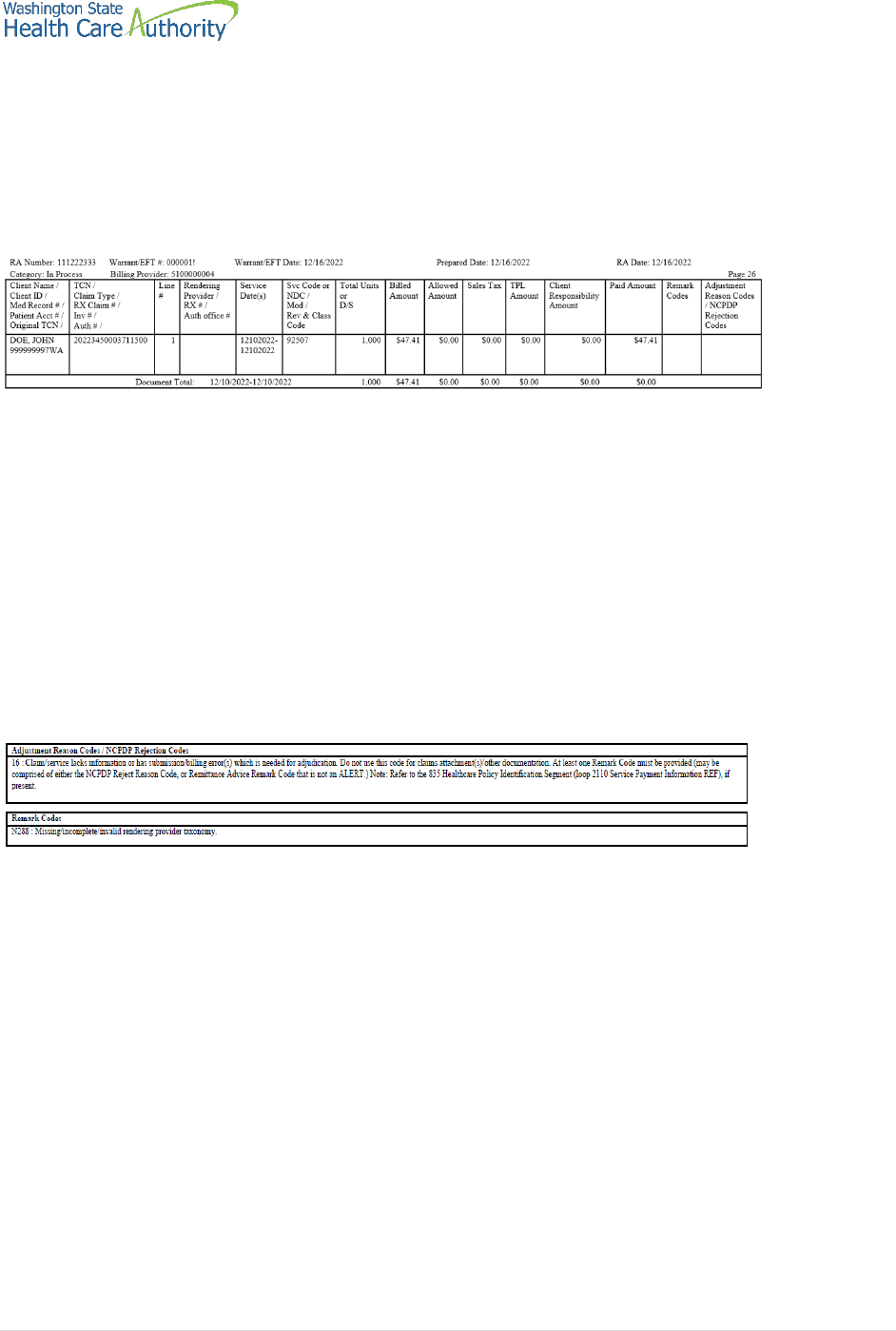
98 | PROVIDERONE BILLING AND RESOURCE GUIDE
Reviewing in process claims
This section of the RA displays claims that are currently in process. These claims
are in the payment system but are usually pending review by claims processing
staff and will show up on a future RA as a paid or denied claim.
Review the section under the “in process” claims category:
Pitfalls
• Rebilling claims because you do not see them in the other sections of the RA;
make sure to review the claims “in process” section.
Reviewing EOB codes
There could be many reasons a claim may have denied, or additional information
was added to a processed claim. You can find these HIPAA adjustment reason
codes and remark codes on the last page of your RA.
Download the PDF file of the remittance advice, locate the claim denial code, and
then scroll down to the last page of the RA to find the code and code definition.
The complete list of standardized adjustment reason and remark codes are
located on the X12 organization’s website.
Pitfalls
• Not downloading the RA to find the denial codes.
• Not reviewing the adjustment reason code and the remark code if both are
on the denied claim.

99 | PROVIDERONE BILLING AND RESOURCE GUIDE
Requesting prior authorization
The authorization intake process
New functionality was implemented in 2018 to allow providers to enter
authorization requests through the direct data entry (DDE) feature in the
ProviderOne portal. Since the COVID-19 pandemic, mailed requests will no
longer be supported.
The DDE prior authorization process is the agency’s preferred method. The
requests are received directly in ProviderOne and allow uploading of photos, x-
rays, and/or chart notes to support the authorization request. Authorization
requests submitted without supporting documentation for medical necessity can
cause delays in processing.
Any information related to mailing authorization requests or using the mail for
submitting required backup for authorization requests has been removed from
this section of the guide.
This section shows how to:
Locate the training materials for entering authorization requests through the
DDE process.
• Locate the General Information for Authorization HCA form, 13-835, for fax
submission only.
• Fill out the authorization form with the required information.
• Navigate the ProviderOne fax intake process.
• Check the status of your authorization request, using the DDE process.
• Submit additional supporting documentation with HCA cover sheets or the
DDE process when needed.
This section does not apply to pharmacy authorization, Long Term Acute Care
(LTAC), or Physical Medicine and Rehabilitation (PM&R) admissions. For more
information on the prior authorization process and for self-service training
materials on entering prior authorizations through the ProviderOne portal, visit
the Prior Authorization webpage.
Why is requesting authorization important?
Some Medicaid-covered procedures require prior authorization. If you need to
determine if the service requires authorization, please review the section titled
Determine if Apple Health covers the service and if so, is prior authorization (PA)
required.
Authorization for a service does not guarantee payment. You must meet
administrative requirements (e.g., client eligibility, claim timeliness, third party
insurance, etc.) before ProviderOne pays for services.
This section will discuss how to submit your authorization request. Doing so
according to agency’s guidelines will help expedite the authorization process.

100 | PROVIDERONE BILLING AND RESOURCE GUIDE
DDE prior authorization intake process
There are three resources for step-by-step instructions on submitting
authorization requests using the ProviderOne provider portal depending on the
type of service you are requesting:
• DDE authorization submission for medical providers
• DDE authorization submission for dental providers
• DDE authorization submission for DME providers
General Information for Authorization form, HCA 13-
835
Beginning the authorization process requires downloading and completing the
General Information for Authorization form, HCA 13-835. Once completed, fax to
1-866-668-1214.
Note: Always go to HCA forms website to ensure use of the most
current form. Do not print the form to copy and use later.
• Find information specific to the most common service types on the back of
the General Information for Authorization form, HCA 13-835.
• The General Information for Authorization form 13-835 must be the first page
of the fax.
• Do not use a cover sheet when faxing an authorization request.
• A confirmation fax will be returned to the sending fax if the fax number can be
identified by caller ID. This fax confirmation does not guarantee that the
request has been entered into the ProviderOne system; it just means that HCA
has received the fax.
Pitfalls
• Handwriting the authorization request form. Forms that are handwritten will
be returned to you.
• Using a cover sheet when faxing in an authorization request; the authorization
form must be the first page of the fax, or it will be returned to you.
• Using an NPI that is not on your ProviderOne account (you can confirm you
are using the correct NPI by checking Step 1 in your ProviderOne file).
• Using an NPI for a servicing provider in field nine instead of the “pay-to
provider”. Always use the NPI of the entity that will be paid for the service.
Submitting backup for DDE authorizations
Follow the steps in the linked processes on the Prior Authorization webpage (or
links above sorted by category of service) to submit any photos, x-rays, or chart
notes required for review of a prior authorization request.

101 | PROVIDERONE BILLING AND RESOURCE GUIDE
Submitting backup for faxed authorizations (no x-
rays)
Prior authorization requests can be faxed to 1-866-668-1214. If the forms are
sent correctly, they can be processed and loaded into ProviderOne with very little
human intervention. Please follow these instructions when submitting the
request:
• Place the General Information for Authorization form, HCA 13-835 as the first
page of your fax.
• Do not use your own cover sheets. The first page of the fax must be the
General Information for Authorization form 13-835.
• Please make sure the settings on your fax machine are for 8½ x 11 size and
photo quality.
Another option for sending dental photos or x-rays for prior authorization is the
FastLook and FastAttach services provided by the National Electronic Attachment,
Inc. (NEA) (no affiliation with ProviderOne/HCA). You may register with NEA by
visiting the NEA website. Contact the NEA at 800-782-5150 extension 1 for
questions. Choosing this option, you can fax your request to HCA and indicate
the NEA# in the NEA field on the authorization request form.
Pitfalls
• Handwriting the authorization form. Forms that are handwritten cannot be
scanned and will be returned to you.
• Using a cover sheet when faxing the authorization form to HCA. The first page
of the fax must be the General Information for Authorization form, HCA 13-
835.
• Using automated outbound fax technology that has altered the paper size to
less than 8 ½ x 11.
• Not having the date stamp on your fax machine current.
• Not setting your fax machine to photo quality images.
Checking PA status
You can verify receipt of your request by HCA using self-service options. You can
also check the status of the authorization to see where it is in the review process.
There are two ways you can verify the status of your request, Check the status of
an authorization using the ProviderOne provider portal, or using the Medical
Assistance Customer Service Center (MACSC) interactive voice response (IVR)
system.
Review Appendix G for instructions on using the IVR to check status, using
ProviderOne to verify status, and for definitions of the different types of
authorization statuses used in processing authorization requests.

102 | PROVIDERONE BILLING AND RESOURCE GUIDE
Pitfalls
• Calling the Medical Assistance Customer Service Center and waiting on hold
to talk with an agent to check status. You can check the status of your request
without having to wait to speak with a customer service representative.
Additional documentation requests
Once HCA receives your authorization request, it will proceed through the review
process. We may request additional information to process the authorization.
If you receive a request for supporting documentation and your authorization
request was submitted through the DDE submission process using the provider
portal, follow the instructions for ProviderOne DDE PA pend process to submit
the information requested by the agency. You may only submit additional
documentation to your online request if the status is “pending”.
Use a cover sheet if you are faxing supporting documentation or responding to a
request from HCA for additional information.
Cover sheets for many different tasks are available on this webpage. Please use
the “Prior Authorization Pend Forms” cover sheet for submitting additional
information to an existing authorization request. You will need to know the
authorization number to use this cover sheet.
After selecting this form, you will be asked to fill in the “Authorization Reference
# field” which is the prior authorization number. Make sure you key in the nine-
digit number. Do not copy and paste the PA number into the authorization
reference number field.
Once you enter in the number and click enter, a barcode generates on the cover
sheet. This bar code enables our scanning system to read the number so that
ProviderOne can electronically attach the documentation to your prior
authorization request. Print out the completed form and attach it to the
supporting documentation.

103 | PROVIDERONE BILLING AND RESOURCE GUIDE
Cover sheet tips
• Always use the PA pend form when submitting additional information to
attach to an existing authorization as requested by the agency.
• Click the enter key or click outside the field after typing in the complete
authorization number so the barcode is created. Cover sheets without
completed barcodes will be returned to you.
• You must submit a separate cover sheet for each authorization you are
submitting backup documentation for.
• You can save the link to the cover sheets webpage as a “Favorite,” but do not
save completed forms for re-use on future authorization requests.
• If you are creating multiple cover sheets, make sure to select Clear Fields
before entering the next authorization number.
Non-scannable cover sheets
It is important that the ProviderOne scanning technology reads the barcode on
the cover sheet to properly attach the documentation to your authorization
request. If the fax quality is poor or the barcode is incomplete, it will not scan
correctly into ProviderOne.
• Avoid handwriting the authorization number.
• Avoid submitting poor quality images with black dots or smudges.
• Set your fax to “photo quality” images to improve readability.
• Cover sheets with incomplete barcodes cannot be scanned.
Pitfalls:
• Not completing the barcode. If you do not click outside the field or press
enter after you type in the Authorization Reference #, the barcode will not be
created.
• Using the Client ID instead of the authorization reference number. You must
enter the prior authorization number on the cover sheet.
• Sending a cover sheet that is a poor quality image; barcodes must be readable
by the ProviderOne scanning system.
• Sending an original authorization request form 13-835 when sending in
additional information to attach to an existing record.
For more information
• Webinars
• Fact sheets
• Billers and providers webpage
• Health Insurance Portability and Accountability Act (HIPAA) homepage
• Provider guides and fee schedules
• Hospital Finance Rates and Contact Us webpage
• Claims and billing resources

105 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix A: Verify eligibility with IVR
Client eligibility – use keypad only
Dial 1-800-562-3022
Select 1 for English or stay on the line
“If you have an extension, press 1 now.”
Select 2 for self-service provider menu
Select 4 for client eligibility
Enter NPI when prompted
Enter client id – numbers only
What will I hear?
The IVR will play only the information specific to the client. The types of
information available are:
• Services card ID number
• Program medical coverage (i.e., CNP)
• Managed care plan name
• Medicare Parts A-D
• Private insurance
• Hospice
• Long term care
• Provider restrictions
More details are available for each of the above options such as beginning
and end dates, as well as contact names and phone numbers. After hearing
the list, enter the number noted for that selection:
• Medicaid – 1
• Managed care – 2
• Medicare - 3
• Insurance coverage – 4
• Hospice – 5
• Long term care – 6
• Restrictions – 7
• Check coverage for another person - 8

106 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix B: Verify eligibility with
magnetic card readers
Magnetic card reader
The option is available to use a magnetic card reader to access eligibility
information for clients using the services card. HCA will not provide or sell
readers. While swipe card technology gives providers an easy and immediate way
to check eligibility, there are other low or no-cost inquiry methods.
• Mini magnetic card readers attach to PC screen and UB connection
o Provider “swipes” services card
o Eligibility information is displayed on the PC screen
o Providers can print the screen
• Desktop magnetic card readers connect directly to the internet
o Provider “swipes” services card
o Eligibility information is printed line by line
The Health Care Authority – Washington Apple Health does not favor, endorse, or
recommend magnetic card readers over any other inquiry method, and does not
favor, endorse, or recommend any magnetic card reader model or vendor over
any other model or vendor. HCA and its employees have neither a financial
interest, nor any other type of interest, in which inquiry method you choose.
For providers choosing the card reader option, you will need a card reader that is
configured appropriately, and you will be subject to a monthly subscription fee to
access the secure network that connects to ProviderOne eligibility data. Providers
are encouraged to shop for the model and vendor that best meets their needs.
For additional information and configuration questions or assistance, please
submit a ticket to HIPAA-Help@hca.wa.gov.

107 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix C: Managed care organizations
Send all claims for services covered under the client’s managed care plan to that
plan for payment. Managed care plans cover a range of services depending on
the program type. For more information about the range of services or covered
services in each contract see the Apple Health (managed care) medical programs
webpage.
The following are subject to change:
• Wellpoint, Washington (WLP, formerly Amerigroup)
1-833-731-2274
https://www.provider.wellpoint.com/
• Community Health Plan of Washington (CHPW)
1-800-440-1561
http://www.chpw.org
• Coordinated Care of Washington (CCW)
1-877-644-4613
http://www.coordinatedcarehealth.com
• Molina Healthcare of Washington (MHC)
1-800-869-7175
http://www.molinahealthcare.com
• United Healthcare Community Plan
1-877-542-9231
http://www.uhccommunityplan.com/health-professionals/wa.html
• Beacon Health Options
1-855-228-6502
https://www.beaconhealthoptions.com

108 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix D: Casualty and health
insurance claims
Casualty claims routinely investigated for possible third-party coverage are:
• Motor vehicle accidents
• Accidents occurring in a place of business, public building, in the home or on
the property of another person.
• Litigation involving a malpractice claim.
• Department of Labor and Industries claims.
• Injury diagnoses and services performed in a hospital or physician’s office.
While a provider’s Apple Health casualty claim is pending investigation, the
provider must call HCA using the toll-free number 1-800-562-3022 only if the
provider has additional insurance information. When the investigation is
completed, HCA makes payment or gives the provider the name and address of
the party responsible for payment. If the provider receives payment from an
insurance company for services that have been paid by HCA, the provider must
immediately refund to HCA either HCA’s payment or the insurance payment,
whichever is less. If the refund is not made within 30 days, HCA recovers the
lesser payment.
Mail refund checks to:
THE HEALTH CARE AUTHORITY
COB CASUALTY UNIT
PO BOX 45561
OLYMPIA WA 98504-5561
Health insurance claims
Third party liability claims other than those for trauma-related injuries are
considered health insurance claims. These claims are routinely held for Third
Party Resources (TPR) investigation when:
• HCA’s records indicate insurance benefits are available through a third party.
• Other resources are indicated on the claim or attachment (name of insurance
company, insurance pending, etc.).

109 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix E: Benefit service packages
Categorically Needy Program (CNP)
This program has the largest scope of care. A few of the services
are doctors, dentists, physical therapy, eye exams, eyeglasses
(children only), mental health, prescriptions, hospitals, and family
planning for men, women, and teens. There is limited coverage
for maternity case management, orthodontia, private duty
nursing, and psychological evaluations. Chiropractic care and
nutrition therapy are limited to the Healthy Kids program.
Alternative Benefits Plan (ABP)
This program is available to persons eligible to receive health
care coverage under Washington Medicaid’s Modified Adjusted
Gross Income (MAGI)-based adult coverage. The scope of
services available is equivalent to that available to CNP-covered
clients with the addition of a benefit for habilitative services.
Washington Administrative Code (WAC) program policies are
applicable to this new eligibility group, as are the instructions in
the ProviderOne Billing & Resource Guide and program-specific
provider guides. This client population does not include those
eligible for Medicare.
Apple Health Expansion (AHE)
This program covers many of the basic services such as doctor
and dental visits, prescriptions, behavioral health, and
hospitalizations. However, some services such as long-term care
are not included in this coverage. This client population does not
include those eligible for federally funded programs.
Emergency Related Services Only (ERSO) – PA may be required
This program has coverage for only specific medical conditions: a
qualifying emergency, end stage renal disease on dialysis, cancer
actively receiving treatment, or post-transplant status on anti-
rejection medications. Prior authorization for some services may
be required. Services not related to the medical condition are not
covered. HCA determines if the client has a qualifying condition
for any of these programs in accordance with the Washington
Administrate Code (WAC) criteria. For specific details please see
Chapter 182-507 WAC.

110 | PROVIDERONE BILLING AND RESOURCE GUIDE
Take Charge – Family Planning Service Only (TCFPO)
This program is for both women and men. It covers family
planning services such as annual examinations, family planning
education and risk reduction counseling, FDA approved
contraceptive methods such as birth control pills and IUDs,
emergency contraception, and sterilization procedures.
Family Planning Services Only (FPSO)
This program is for women. Services include coverage for all birth
control methods, sterilization, OB-GYN exams, and counseling to
help with family planning.
Medical Care Services (MCS) - no out of state care
This program covers many of the most basic services such as
doctor and dental visits, prescriptions, and hospitalizations.
However, some services such as mental health treatment may
have restrictions that require prior authorization or may not be
covered. This benefit was previously known as General Assistance
(GA) and Disability Lifeline (DL).
Alcoholism and Drug Addiction Treatment and Support Act (ADATSA) - no
out of state care
This program covered many of the most basic services such as
doctor's visits, prescriptions, and hospitalizations. However, some
services, such as dental and mental health treatment may have
restrictions that require prior authorization or may not be
covered. Coverage is equivalent to Medical Care Services (MCS)
below, with the addition of treatment for alcohol and drug
addiction.
Limited Casualty Program – Medically Needy Program (LCP-MNP)
This program covers many medical services. A few of the services
are doctors, dentists, eye exams, eyeglasses (children only),
mental health, prescriptions, and hospitals, family planning for
men, women, and teens. There are some services that are not
covered, such as physical therapy. There are also limited
services: maternity case management is one example.
Chiropractic care and nutrition therapy are limited to the Healthy
Kids program.

111 | PROVIDERONE BILLING AND RESOURCE GUIDE
Qualified Medicare Beneficiary (QMB) – Medicare Only
This Medicare Savings Program pays for Medicare Part A and B
premiums and pays for deductibles, coinsurance, and
copayments according to Medicaid rules.
Specified Low-Income Medicare Beneficiary (SLMB)
This Medicare Savings Program only pays for Medicare Part B
premiums. Health coverage through Apple Health Medicaid is
not covered.
Qualified Individual 1 (QI-1)
This Medicare Savings Program only pays for Medicare Part B
premiums. Health coverage through Apple Health Medicaid is
not covered.
Qualified Disabled Working Individual (QDWI)
This Medicare Savings Program only pays for Medicare Part A
premiums. Health coverage through Apple Health Medicaid is
not covered.
Inpatient Psychiatric Care Only (IPCO)
This program covers services given in a psychiatric
institution/hospital. Other services are not covered.
For more information, please submit questions to Contact Us.

112 | PROVIDERONE BILLING AND RESOURCE GUIDE
ACES program codes
Some provider groups rely on the ACES program codes to help them determine if
the client is on a state-only program or is on an Apple Health (Medicaid) program
to identify their funding sources. The following table lists these program codes.
Category
ACES
Description
BSP
SSI and SSI related, also called
Aged/Blind/Disabled (ABD);
disability is determined by SSA or
by NGMA referral to DDDS
S01
SSI recipients
CNP
S02
ABD categorically needed
CNP
S03
QMB Medicare savings program (MSP)
Medicare premium and copays
MSP
S04
QDWI Medicare savings program
MSP
S05
SLMB Medicare savings program - Medicare
premium only
MSP
S06
QI-1 (SLMB) Medicare savings program
MSP
S07
Undocumented alien - Emergency related
service only
ERSO
S20
Apple health expansion (AHE)
AHE
S95
Medically needy no spenddown
MNP
S99
Medically needy with spenddown
MNP
SSI related healthcare for workers
with disability
S08
Healthcare for workers with disability CNP
premium based program - substantial
gainful activity (SGA) not a factor in
disability determination
CNP
SSI related living in an alternate
living facility (nonmedical
institution), adult family home,
boarding home, or DDD group
home
G03
Non institutional medical in ALF CNP
income under the SIL plus under state rate x
31 days + 38.84
CNP
G95
Medically needy non-institutional in ALF no
spenddown
MNP
G99
Medically needy non-institutional in ALF
with Spenddown
MNP
Institutional HCBS waivers
(HCS/DDD) and hospice
SSI and SSI related
L21
DDD/HCS waiver on SSI
CNP
L22
DDD/HCS waiver – gross income under the
SIL
CNP

113 | PROVIDERONE BILLING AND RESOURCE GUIDE
Category
ACES
Description
BSP
L24
Undocumented alien/non-citizen LTC –
residential placement; must be preapproved
by ADSA program manager; Emergency
related service only (45 slots)
ERSO
-
CNP
L31
PACE or hospice on SSI (effective
10/1/2015)
CNP
L32
PACE or hospice – SSI-related (effective
10/1/2015)
CNP
L41
Roads to community living on SSI (effective
10/1/2015)
CNP
L99
Roads to community living – SSI related
(effective 10/1/2015)
CNP
Non-institutional community first
choice
Personal care services in the
community
L51
Community first choice (CFC) on SSI
(effective 10/1/2015)
CNP
L52
Community first choice (CFC) – SSI related at
home or in an ALF (effective 10/1/2015)
CNP
Institutional SSI - related
Residing in a medical institution 30
days or more
L01
SSI recipient in a medical institution -
residing in a medical institution 30 days or
more
CNP
L02
SSI related CNP in a medical institution
income under the SIL
CNP
L04
Undocumented alien/non-citizen LTC must
be pre-approved by ADSA program
manager; Emergency related service only
(45 slots)
ERSO -
CNP
L95
SSI related Medically needy no spenddown
Income over the SIL; Income under the state
rate
MNP
L99
SSI related Medically needy with
spenddown; income over the SIL; income
over the state rate but under the private
rate; locks into state NF rate
MNP
Institutional family/children TANF
related income/resource rules
K01
Categorically needy family in medical
institution
CNP

114 | PROVIDERONE BILLING AND RESOURCE GUIDE
Category
ACES
Description
BSP
K03
Undocumented alien family in medical
institution - Emergency related service only
ERSO
K95
Family LTC Medically needy no spenddown
in medical institution
MNP
K99
Family LTC Medically needy with
spenddown - in medical institution
MNP
Pregnancy
P02
Pregnant 185% of FPL & postpartum
extension
CNP
P04
Undocumented alien pregnant woman
CNP
P05
Family planning service only
Family
planning
P06
Take charge family planning only
P99
Medically needy pregnant spenddown
MNP
Refugee medical assistance
R02
Transitional 4 month extension
CNP
R03
Refugee Categorically needy
CNP
DCFS/JRA medical foster care
D01
SSI recipient FC/AS/JRA Categorically needy
CNP
D02
FC/AS/JRA Categorically needy
CNP
D26
Title IV-E Federal foster care
CNP
Family related medical assistance
F01
TANF cash and Medicaid (ended 9/30/2013)
CNP
F02
Transitional Medicaid
CNP
F03
Post TANF child/spousal support (4 months
max - ended 12/31/2013)
CNP
F04
TANF related
CNP
F05
Newborn
CNP
F06
Categorically needy medical children
(effective 1/1/2009, this may be CNP
Medicaid children or CNP State funded
children)
CNP
F07
Children’s health insurance program
CNP

115 | PROVIDERONE BILLING AND RESOURCE GUIDE
Category
ACES
Description
BSP
F08
Undocumented alien children (this coverage
group ended 12/31/2008 and is merged
with the F06 group)
CNP
F09
Undocumented alien – Emergency related
service only
ERSO
F10
Interim Categorically needy (2 months max -
ended 12/31/2014)
CNP
F99
Medically needy children spenddown
MNP
MAGI family related medical
assistance
N01
MAGI parent/caretaker Medicaid; adult
CNP
N02
12-month transitional MAGI
parent/caretaker Medicaid; adult
CNP
N03
MAGI pregnancy
CNP
N04
After pregnancy
CNP/ABP
N05
MAGI adult Medicaid; income =<133%
(Medicaid expansion)
ABP
N07
After pregnancy; not Medicaid eligible
during pregnancy
CNP
N10
MAGI newborn medical/birth to one year
CNP
N11
MAGI children's Medicaid/age under 19
CNP
N13
MAGI Children's health insurance program
(CHIP) children under 19; premium payment
program
CNP
N20
Apple health expansion (AHE)
AHE
N21
MAGI parents/caretaker; Emergency only;
AEM
ERSO
N23
MAGI pregnancy; not lawfully present
CNP
N24
After pregnancy; not lawfully present
CNP
N25
MAGI adult Medicaid; non-citizen - income
=<133% (Medicaid expansion) AEM
ERSO

116 | PROVIDERONE BILLING AND RESOURCE GUIDE
Category
ACES
Description
BSP
N27
After pregnancy; not lawfully present; not
Medicaid eligible during pregnancy
CNP
N31
MAGI Children's medical; under 19; non-
citizen
State
funded
CNP
N33
MAGI Children's health insurance program
(CHIP): under 19; premium payment
program, non-citizen
State
funded
CNP
ADATSA State program drug &
alcohol TX program
W01
ADATSA Medical state funded (ended
12/31/2013)
State
funded
W02
ADATSA Medical state funded (ended
12/31/2013)
State
funded
W03
Detox medical state funded (ended
12/31/2013)
State
funded
Medical care services and ABD
cash with CN Medicaid
G01
MCS Medical care services (ended
8/31/2014)
State
funded
A01
MCS Medical care services – non-citizen
(Aged/Blind/Disabled)
State
funded
A05
MCS Medical care services – non-citizen
(under 65, incapacitated)
State
funded
A24
MCS Medical care services – non-citizen SFA
for Survivors of certain crimes
State
funded
G02
ABD cash plus either:
ABD-X Presumptive SSI Federally funded CN
Medicaid (ended 12/31/2013)
ABD-A Federally funded CNP - AGED
(ended 8/31/2014)
ABD-D Federally funded CNP- NGMA
disability determination (ended 8/31/2014)
CNP
Mental health institutional
I01
Inpatient psychiatric (mental health - ended
12/31/2013)
CNP
Breast and cervical cancer program
S30
Breast and cervical cancer (Health
Department approval)
CNP

117 | PROVIDERONE BILLING AND RESOURCE GUIDE
Category
ACES
Description
BSP
Take charge
P06
Family planning (Take charge)
Family
planning
Psychiatric inpatient
M99
Psychiatric indigent inpatient spenddown
(MI prior to 7/2003)
Mental health ONLY (ended 12/31/2013)
Inpatient
psychiatric
hospital
only
Tailored supports for older adults
(TSOA)
HCS maintains TSOA cases
T02
TSOA-No medical benefits and no
Medicaid services card issued
Pre-Medicaid benefit for the caregiver of a
person 55 or older to support the caregiver.
For those not eligible for a CN or ABP
Medicaid program and not needing or
eligible for other LTSS services because of
resources. Must meet NFLOC.
No
medical
benefits
For a high-level scope of care table for services covered by these programs see
Health Care Coverage Program Benefit Packages and Scope of Service
Categories.

118 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix F: Prior authorization process
Authorization for services does not guarantee payment. Providers must meet
administrative requirements (client eligibility, claim timeliness, third-party
insurance, etc.) before HCA pays for services. For more information on prior
authorization and for self-service training materials on entering prior
authorization requests through the ProviderOne portal, visit the Prior
Authorization webpage.
Download the General Information for Authorization form, HCA 13-835.
Note: See page two of the General Information for Authorization
form, HCA 13-835, for complete instructions about completing
the authorization form.
When faxing the General Information for Authorization form, HCA 13-835:
• Do not use a cover sheet when faxing an authorization request.
• Make the General Information for Authorization form, HCA 13-835 the first
page of the fax.
• Only send one request form at a time.
• Disable the “bundle” setting for multiple fax transmissions when sending to a
single fax number. If this function is not disabled, the entire bundle of faxes
will be sent under the first cover sheet and cannot be scanned correctly.
A confirmation fax will be returned to the provider if the sending fax number can
be identified by caller ID.

119 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix G: Authorization status using
the IVR
There are two ways to check the status of a ProviderOne authorization request:
using the Interactive Voice Response (IVR) and using the ProviderOne portal.
Checking authorization status using Interactive Voice
Response (IVR)
Authorization status – use keypad only
Dial 1-800-562-3022
Select 1 for English or stay on the line
“If you have an extension, press 1 now.”
Select 2 for self-service provider menu
Select 1 for authorization
Select 1 for pharmacy authorizations
Select 2 for medical, dental, or other authorizations
Enter NPI when prompted
Select 2 for get status
Choose option 1 to search by authorization number
Choose option 2 to search by client ID/date of birth
What will I hear?
The IVR will play the information only to the provider(s) identified on the
authorization. Search by the client’s services card number and date of birth, or by
the authorization number. If multiple authorization numbers are found, narrow
the search with an NDC or service code, as well as an expected date of service.
The types of information available are:
• Authorization number
• Status date
• Status, such as:
• Approved
• In review
• Denied

120 | PROVIDERONE BILLING AND RESOURCE GUIDE
• Referred
• Pending
• Cancelled
Checking authorization status using ProviderOne
Select Provider Authorization Inquiry from the provider home page:
Enter the search criteria using one of the three inquiry options and click on the
submit button:
The system will return the authorization status:
Any one of the following may appear in the authorization status field:
Status
Meaning
Error
There is an error in ProviderOne that will be
cleared once the request is worked. No action
is needed by the provider.

121 | PROVIDERONE BILLING AND RESOURCE GUIDE
Status
Meaning
Requested
HCA received the requested authorization.
In review
The authorization is in review.
Canceled
The authorization request is canceled.
Pended
Requires additional information to decide on
the request.
Referred
Request has been forwarded to a second
level reviewer.
Approved/hold
Request approved, but additional information is
necessary before the release of authorization for
billing.
Approved/denied
Partially approved and some services have
been denied.
Rejected
Returned to the provider as incomplete.
Approved
HCA has approved the request.
Denied
HCA has denied the request.

122 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix H: Cover sheets for backup
documentation
Use a cover sheet when submitting backup documentation to a claim or an
authorization. Cover sheets help HCA quickly match backup documents to claims
submitted using Direct Data Entry (DDE) or by batch submission. Backup
documentation for claims can be faxed or mailed, however supporting
documentation for prior authorization requests must be faxed.
These cover sheets are necessary when submitting backup documentation
without the original claim or prior authorization form.
While performing tasks in ProviderOne, the system will sometimes prompt the
user to print a cover sheet. For example, when clicking the “submit claim” button
while entering a DDE claim, the system will display a popup box asking if you
want to send backup documentation. By clicking on the “OK” button,
ProviderOne will go directly to the document submission cover sheet page.
On the document submission cover sheet webpage, click on the document
hyperlink for the cover sheet you want to use. Below is a list of forms to use and a
description of their purpose (forms that apply to pharmacies only are not listed).
Cover sheet name
When would it be used?
Claim attachments
Use this cover sheet when mailing or
faxing backup documentation required
for a dental, institutional, or professional
claim. The TCN from the claim is required
to use this form.
Prior authorization pend forms
Use this cover sheet when submitting
the supporting documentation for a
prior authorization (PA) request in
pended status. You must use the
authorization number to use this cover
sheet. Backup information to support
prior authorization requests must be
faxed.
After choosing the appropriate cover sheet, the provider must fill in pertinent
information such as TCN. Once the required information is entered into the form,
click “enter” or click outside of the field, and a barcode will be generated. Then
print the completed form by clicking on the PRINT button (NOT: File/Print). Do
not make any modifications to these forms other than filling out the required
information and generating the barcodes. The barcode contains critical
information that helps HCA link the supporting documents to the claim or PA
request in ProviderOne.
After printing the completed form, attach it to the supporting documentation
and submit by fax (only option for prior authorization requests) to 1-866-668-
1214 or by mail to:

123 | PROVIDERONE BILLING AND RESOURCE GUIDE
Heath Care Authority
RE: Cover sheets and backup documentation
PO Box 45535
Olympia, WA 98504-5535
A few tips about cover sheets:
• Submit a separate cover sheet for each claim number (TCN) or client
authorization that requires backup.
• If faxing multiple requests, make sure each request has its own cover sheet.
• When mailing multiple sets of documentation for claims, mail in a single
envelope with a cover sheet for each.
• Save the link to the cover sheets webpage as a “Favorite”, but always use
cover sheets printed from the website to make sure you have the most current
version. Do not save and re-use them. Each cover sheet has barcodes
generated specific to each claim or request.
• Do not use a cover sheet when submitting an initial prior authorization
request, if submitting using the 13-835 General Information for Authorization.
Note: When filling out the cover sheet, be sure to fill in all the
fields with information:
- Do not add a zero to any field if the information for that field
is not available when filling out the cover sheet. Obtain the
information, then fill in the fields and print.
- Do not hand write on the cover sheet after printing.
- Do not save the cover sheet for reuse. Each cover sheet is
specific to each document sent to the agency.
- Do not use any software other than Adobe for opening and
generating the cover sheet. The barcode used to link
documents will not work properly using other software.

124 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix I: Taxonomy and ProviderOne
A taxonomy code indicates provider type, specialty, and subspecialty. You will
need to use a taxonomy for billing and servicing (if applicable) providers on all
claims submitted in ProviderOne.
The general term “taxonomy” refers to a classification system. For medical billing
and payment, “provider taxonomy” refers to the national provider classification
system defined by the Centers for Medicare and Medicaid Services (CMS). This
national classification system is part of the National Provider Identification (NPI)
rule of the Health Insurance Portability and Accountability Act (HIPAA).
Apple Health requires taxonomy on Medicare crossovers. You must include
taxonomy on Medicare claims when the client is also eligible for Medicaid as a
secondary payer. Medicare will pass the taxonomy on these claims to Apple
Health. If the taxonomy is missing on Medicare claims passed to Apple Health,
these claims will deny. In addition, Apple Health does not receive TPL claims
directly from other payers (other than Medicare). When billing the agency directly
for TPL coverage, follow Apple Health rules about taxonomy (i.e., make sure the
taxonomy is associated with the provider and that the taxonomy description
aligns with the service).
There are three steps to using taxonomy in ProviderOne:
1. Verify the taxonomy to be billed is loaded in your ProviderOne account:
o This information can be found under Manage Provider Information on the
Provider Portal.
o On the Business Process Wizard (BPW) page, taxonomy is referred to as
Specializations.
o There are 2 profiles in ProviderOne that allow the user to edit or add to
your account: EXT Provider File Maintenance and EXT Provider Super User
(other profiles may only allow viewing of the file).
o ProviderOne uses subsets of the national taxonomies; there are many more
taxonomies available that are not used by the ProviderOne system. Only
those taxonomies shown in the drop down list in the provider file are
being used.
2. Use the verified taxonomy for billing and rendering/servicing (if applicable)
providers on the claim (this is not necessary for referring providers).
3. Make sure the service billed is allowed by the taxonomy:
o The service on the billed claim must be associated with the taxonomy and
be within the scope of licensure for the provider supplying or performing
the service. For example, oxygen services require oxygen taxonomy;
Durable Medical Equipment (DME) billings require DME taxonomy; dental
services require a dental taxonomy, etc.

125 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix J: Medicare crossover claim
payment methodology
Professional services
Refer to WAC 182-502-0110 for full details; this guide provides a summary of
these rules as follows:
• ProviderOne compares Apple Health’s allowed amount to Medicare's allowed
amount for the service, selects the lesser amount of the two, and then deducts
Medicare's payment from the amount selected.
• If there is a balance due, ProviderOne pays the client’s cost sharing liability
(deductible, coinsurance, or co-pay) up to the lesser of the allowed amounts.
• If there is no balance due, ProviderOne does not make any crossover claim
payment because Medicare's payment exceeds Apple Health’s calculated
allowed amount.
o As of 12/20/2015, for QMB clients ProviderOne began paying such claims at
$0.00 instead of denying with CARC 23.
• When Apple Health does not cover the service, pricing on QMB clients will use
either Medicare's allowed or a Medicaid State Plan rate appropriate to the
service, whichever is less; HCA has the option to use a CMS approved
negotiated rate instead and will pursue this option over time.
ProviderOne cannot make direct payments to clients to cover the client’s cost
sharing liability (deductible, coinsurance, or co-pay) amount of a Part B Medicare
claim. ProviderOne can pay these costs to you on behalf of the client when:
• You accept assignment; and
• Total reimbursement to you from Medicare and ProviderOne does not exceed
the rate in Apple Health’s fee schedule.
HCA has revised procedure codes that may be non-covered by Apple Health, but
the services are covered. If the service is covered by Apple Health, but the code is
not, ProviderOne may pay as follows:
Medicare allowed – Medicare paid = agency payment
ProviderOne payment on crossover claims equals the lesser of the Apple Health
allowed amount minus the Medicare or Part C plan payment toward the client’s
cost sharing liability. Payment from Medicare or the Part C plan and ProviderOne
cannot exceed Apple Health’s allowed amount for the service.
• The crossover claim payment cannot exceed the client’s cost sharing liability.
• No payment will be made if the Medicare or Part C plan payment exceeds
Apple Health’s allowed amount for the service.

126 | PROVIDERONE BILLING AND RESOURCE GUIDE
Institutional services
Outpatient hospital
Payment equals the lesser of the Apple Health allowed amount minus the
Medicare paid amount up to the client’s cost sharing liability (deductible,
coinsurance, or co-pay). Total payment to you from Medicare and the agency
does not exceed Apple Health’s allowed amount.
RHC-Rural health clinic
For RHCs who bill for Medicare encounter services, payment equals the RHC per
diem rate on file with the agency, minus the Medicare paid amount. These RHC
claims are submitted using type of bill (TOB) 71x and billing provider taxonomy
261QR1300X.
FQHC-Federally Qualified Health Clinic
For Federally Qualified Health Centers (FQHCs) who bill for FQHC Services,
payment equals the Medicare coinsurance amount. These FQHCs bill crossover
claims using TOB 77x and billing provider taxonomy 261QF0400X.
Inpatient hospital for client with both Medicare Part A and Part B coverage
Payment equals the lesser of the Apple Health allowed amount minus the
Medicare paid amount, up to the client’s cost sharing liability (deductible,
coinsurance, or co-pay).
Dual-eligible clients with a commercial Medicare supplement
ProviderOne will adjust any payment amounts if the client has a commercial
Medicare supplement policy and that entity makes a payment after Medicare. In
that case the formula is:
Medicare payment + commercial insurance payment – total
Medicaid allowed amount = agency payment

127 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix K: Checking claim status using
the IVR
Check claim status – use keypad only
Dial 1-800-562-3022
Select 1 for English or stay on the line
“If you have an extension, press 1 now.”
Select 2 for self-service provider menu
Select 2 for claims
Enter NPI when prompted
Enter 1 to search by TCN
Enter 2 to search by client ID
Enter 3 to search by prescription number
What will I hear?
The IVR will play only the information specific to your claims. The type of
information available is dependent on the status. In addition to the claim
number (TCN), you can also check the following:
• Status of paid:
o Date paid
o RA date
o Amount paid
o Warrant amount
o Warrant number
o RA number
o Services dates
• Status of denied:
o Date denied
o Denial reasons (limited to 5)
• Status of in process:
o Date received

128 | PROVIDERONE BILLING AND RESOURCE GUIDE
o Message if more than 30 days
• Provider menu choices:
o Authorizations – 1
o Check claims – 2
o Check warrants – 3
o Client eligibility – 4
Searching with data other than the TCN will generate additional questions:
• Client ID:
o Date of birth
o Search by specific date or range
• Prescription:
o Claim more than 2 days old
o Prescription number
o Fill date

129 | PROVIDERONE BILLING AND RESOURCE GUIDE
Appendix L: Checking warrants using the
IVR
Check warrants – use keypad only
Dial 1-800-562-3022
Select 1 for English or stay on the line
“If you have an extension, press 1 now.”
Select 2 for self-service provider menu
Select 3 for check warrants
Enter NPI when prompted
Enter 1 to search by most recent
Enter 2 to search by a specific date
What will I hear?
The IVR will play only the information specific to the associated provider. The
types of information available are:
• Paid date
• Warrant amount (check amount)
• Warrant number (check number)
• RA number
Provider menu choices:
• Authorizations – 1
• Check claims – 2
• Check warrants – 3
• Client eligibility – 4

