
“What Matters” to
Older Adults?
A Toolkit for Health Systems to Design
Better Care with Older Adults
This content was created especially for:
TOOLKIT
An initiative of The John A. Hartford Foundation and
the Institute for Healthcare Improvement (IHI) in
partnership w ith the American Hospital Association
(AHA) and the Catholic Health Association of the
United States (CHA).

Authors:
Mara Laderman, MSPH: Director, IHI
Clark Jackson, MPH: Research Associate, IHI
Kevin Little, PhD: Principal, Informing Ecological Design, LLC, and IHI Faculty
Tam Duong, MSPH: Senior Project Manager and Research Associate, IHI
Leslie Pelton, MPA: Senior Director, IHI
Acknowledgments:
This work was supported by a grant from The SCAN Foundation. The SCAN Foundation works to
advance a coordinated and easily navigated system of high-quality services for older adults that
preserve dignity and independence. For more information, visit www.TheSCANFoundation.org.
This work was also made possible by The John A. Hartford Foundation, a private, nonpartisan,
national philanthropy dedicated to improving the care of older adults. For more information, visit
www.johnahartford.org.
IHI would like to thank our partners, the American Hospital Association (AHA) and the Catholic
Health Association of the United States (CHA), for their leadership and support of the Age-
Friendly Health Systems initiative. Learn more at ihi.org/AgeFriendly.
We would also like to thank the following individuals who provided guidance and critical review
through the development of this toolkit: Gretchen Alkema, Lil Banchero, Len Barry, Kevin Biese,
Maureen Bisognano, Susan Block, Joan Chaya, Lenise Cummings-Vaughn, Claire Curtis, Kate
DeBartolo, Susan Edgman-Levitan, Lindsay Gainer, Damara Gutnick, Daniela Lamas, Jennifer
Liu, Catherine Mather, Kelly McCutcheon Adams, VJ Periyakoil, Pat Rutherford, Lauge Sokol-
Hessner, Mary Tinetti, Matthew Tremblay, Erin Westphal, and Angela Zambeaux. Thank you to
the five prototype health systems — Anne Arundel Medical System, Ascension, Kaiser Permanente,
Providence St. Joseph, and Trinity — for stepping forward to learn what it takes to become an Age-
Friendly Health System. Finally, our deepest gratitude to Pat McTiernan and Val Weber of IHI for
their support in editing this toolkit. The authors assume full responsibility for any errors or
misrepresentations.
For more than 25 years, the Institute for Healthcare Improvement (IHI) has used improvement science to advance and sustain better outcomes in health
and health systems across the world. We bring awareness of safety and quality to millions, accelerate learning and the systematic improvement of care,
develop solutions to previously intractable challenges, and mobilize health systems, communities, regions, and nations to red uce harm and deaths. We
work in collaboration with the growing IHI community to spark bold, inventive ways to improve the health of individuals and populations. We generate
optimism, harvest fresh ideas, and support anyone, anywhere who wants to profoundly change health and health care for the bet ter. Learn more at ihi.org.
Copyright © 2019 Institute for Healthcare Improvement. All rights reserved. Individuals may photocopy these materials for educational, not -for-profit uses, provided that the
contents are not altered in any way and that proper attribution is given to IHI as the source of the content. These materials may not be reproduced for commercial, for -profit
use i n any form or by any means, or republished under any circumstances, without the written permission of the Institute for Healthcare Improvement.

Institute for Healthcare Improvement
•
ihi.org 3
Contents
“What Matters” to Older Adults: The Basis of Age-Friendly Health Care 4
The Age-Friendly Health Systems Initiative 6
Important Considerations for “What Matters” Conversations 8
Who Should Initiate a “What Matters” Conversation 11
What to Discuss in a “What Matters” Conversation 12
How to Prepare Older Adults and Caregivers for a “What Matters” Conversation 14
How to Conduct an Effective “What Matters” Conversation 15
Documenting “What Matters” Information 18
Incorporating “What Matters” Information into the Care Plan 21
Measuring “What Matters” 22
Conclusion 26
Case Examples 27
Appendix A: Resources to Support “What Matters” 29
Conversations with Older Adults
Appendix B: Examples of “What Matters” Conversations 31
Appendix C: Detailed Information on “What Matters” 32
Process and Outcome Measures
Appendix D: A Multicultural Tool for Getting to Know
You and What Matters to You 36
References 38

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 4
“What Matters” to Older Adults: The Basis
of Age-Friendly Health Care
In March 2012, Michael Barry, MD, and Susan Edgman-Levitan, PA, introduced the concept of
asking patients “What matters to you?” in addition to asking “What is the matter?” Their goal was
to increase providers’ awareness of critical issues in their patients’ lives that could drive
customized plans of care. Since then, the Institute for Healthcare Improvement (IHI) and other
organizations around the world have been encouraging providers and health care organizations to
ask patients and their caregivers about “What Matters” to them to inform their care.
1
IHI’s past work on The Conversation Project
2
and Conversation Ready
3
has sought to encourage
individuals, families, and health systems to have conversations about “What Matters” in the
context of end-of-life care. The Age-Friendly Health Systems initiative builds upon IHI’s previous
work in shared decision making, expanding the asking of “What Matters” beyond the context of
end-of-life care to all care with older adults across their lifespan. “What Matters” is the foundation
of the Age-Friendly Health Systems initiative, which in its entirety encompasses four evidence-
based elements of care for older adults — What Matters, Medication, Mentation, and Mobility.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 5
• The Age-Friendly Health Systems initiative defines “What Matters” as knowing and aligning
care with each older adult’s specific health outcome goals and care preferences including,
but not limited to, end-of-life care, and across settings of care.
• Health outcome goals relate to the values and activities that matter most to an individual,
help motivate the individual to sustain and improve health, and could be impacted by a
decline in health — for example, babysitting a grandchild, walking with friends in the
morning, or volunteering in the community. When identified in a specific, actionable, and
reliable manner, patients’ health outcome goals can guide decision making.
• Care preferences include the health care activities (e.g., medications, self-management tasks,
health care visits, testing, and procedures) that patients are willing and able (or not willing or
able) to do or receive.
The aim is to align care and decisions with the older adult’s health outcome goals.
Within the Age-Friendly Health Systems initiative, the “What Matters” element ensures ongoing
communication and relationship building with older adults and their caregivers. Instead of one-
time conversations between older adults and clinicians, “What Matters” conversations should take
place at multiple points of care (e.g., annual visits, major life events, or changes in health status)
and be coordinated among all members of the care team.
Operationalizing a system to understand, document, and act on “What Matters” to older adults in
health care organizations requires organizational culture change as well as clinician training and
specific changes to workflows and the electronic health record. “What Matters” is of great
importance to older adults, caregivers, and the health care workforce.
Note that aligning care to each patient is still a relatively new concept, particularly for patients who
are not seriously ill or near the end of life. This toolkit brings together the best available evidence
from health systems around the world to help guide the testing and implementation of this
important concept in your local health system.
The toolkit is intended to serve as a resource for multidisciplinary care teams, including, but
not limited to, physicians, nurses, physician assistants, medical assistants, social workers,
chaplains, nurse navigators, community health workers, and trained volunteers. The toolkit
provides actionable steps and guidance to ensure that every older adult’s health outcome goals
and care preferences are understood, documented, and integrated into their care by the entire
health care team.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 6
The Age-Friendly Health Systems Initiative
What Are Age-Friendly Health Systems and Why Are
They Important?
Three factors that impact caring for older adults in the United States today are occurring
simultaneously. Together, the factors make a compelling case for health systems to better support
the needs of older adults and caregivers:
• Demography: The number of adults over the age of 65 years is projected to double over the
next 25 years.
• Complexity: Approximately 80 percent of older adults have at least one chronic condition,
and 77 percent have at least two.
• Disproportionate Harm: Older adults have higher rates of health care utilization as
compared to other age groups and experience higher rates of health-care-related harm, delay,
and discoordination.
Becoming an Age-Friendly Health System entails reliably providing a set of specific, evidence-
based best practice interventions to all older adults, as needed, in your health system. This is
achieved primarily through redeploying existing health system resources to achieve:

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 7
• Better health outcomes for this population
• Reduced waste associated with low-quality, unwanted, or unneeded services
• Increased utilization of cost-effective services for older adults
• Improved reputation and market share with a rapidly growing population of older adults
The “4Ms” Framework of an Age-Friendly Health System
In 2017, The John A. Hartford Foundation and IHI, in partnership with the American Hospital
Association (AHA) and the Catholic Health Association of the United States (CHA), launched the
Age-Friendly Health Systems initiative, which set the bold aim that 20 percent of US hospitals and
health systems would be Age-Friendly Health Systems by December 2020.
The 4Ms Framework that emerged from the Age-Friendly Health Systems initiative is both
evidence-based and able to be put into practice reliably in the health care setting. The 4Ms are:
• What Matters: Know and align care with each older adult’s specific health outcome goals
and care preferences including, but not limited to, end-of-life care, and across settings of care.
• Medication: If medication is necessary, use age-friendly medication that does not interfere
with What Matters to the older adult, Mentation, or Mobility across settings of care.
• Mentation: Prevent, identify, treat, and manage dementia, depression, and delirium across
settings of care.
• Mobility: Ensure that older adults move safely every day in order to maintain function and
do What Matters.
The 4Ms are the essential elements of high-quality care for older adults and, when implemented
together, indicate a broad shift by health systems to focus on the needs of older adults. Reliable
implementation of the 4Ms is supported by board and executive commitment to becoming an Age-
Friendly Health System, engagement of older adults and caregivers, and community partnerships.
“What Matters” as the Basis of Age-Friendly Care
In the Age-Friendly Health Systems initiative, “What Matters” to the older adult is the basis for the
relationship with the care team and shapes the care that is provided. “What Matters” integrates
care and decision making across care settings. “What Matters” is not limited to end-of-life
planning. It is therefore essential to the older adult, the care team, and the health system that
“What Matters” to each older adult is identified, understood, and documented so it can be acted
upon, and updated across settings of care following changes in care or life events.
While fundamental to person-centered care, the practice of “What Matters” is the least developed
of the 4Ms. Because of its importance, and the need for further development in practice, this “What
Matters” to Older Adults Toolkit was developed by IHI with support from The SCAN Foundation.
Bringing together the best available evidence from health systems around the world, the toolkit is a
starting place and an invitation to learn together how to better understand and act upon “What
Matters” to older adults and measure progress in doing so.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 8
Important Considerations for “What Matters”
Conversations
Understanding “What Matters” is an ongoing process, built on strong relationships between care
team members and older adults. While there are some critical moments when an older adult’s
health and care goals and preferences may need to be elicited or redefined, understanding “What
Matters” requires a series of conversations over time that become the guide for how care is
delivered. There two considerations for “What Matters” conversations, as described below.
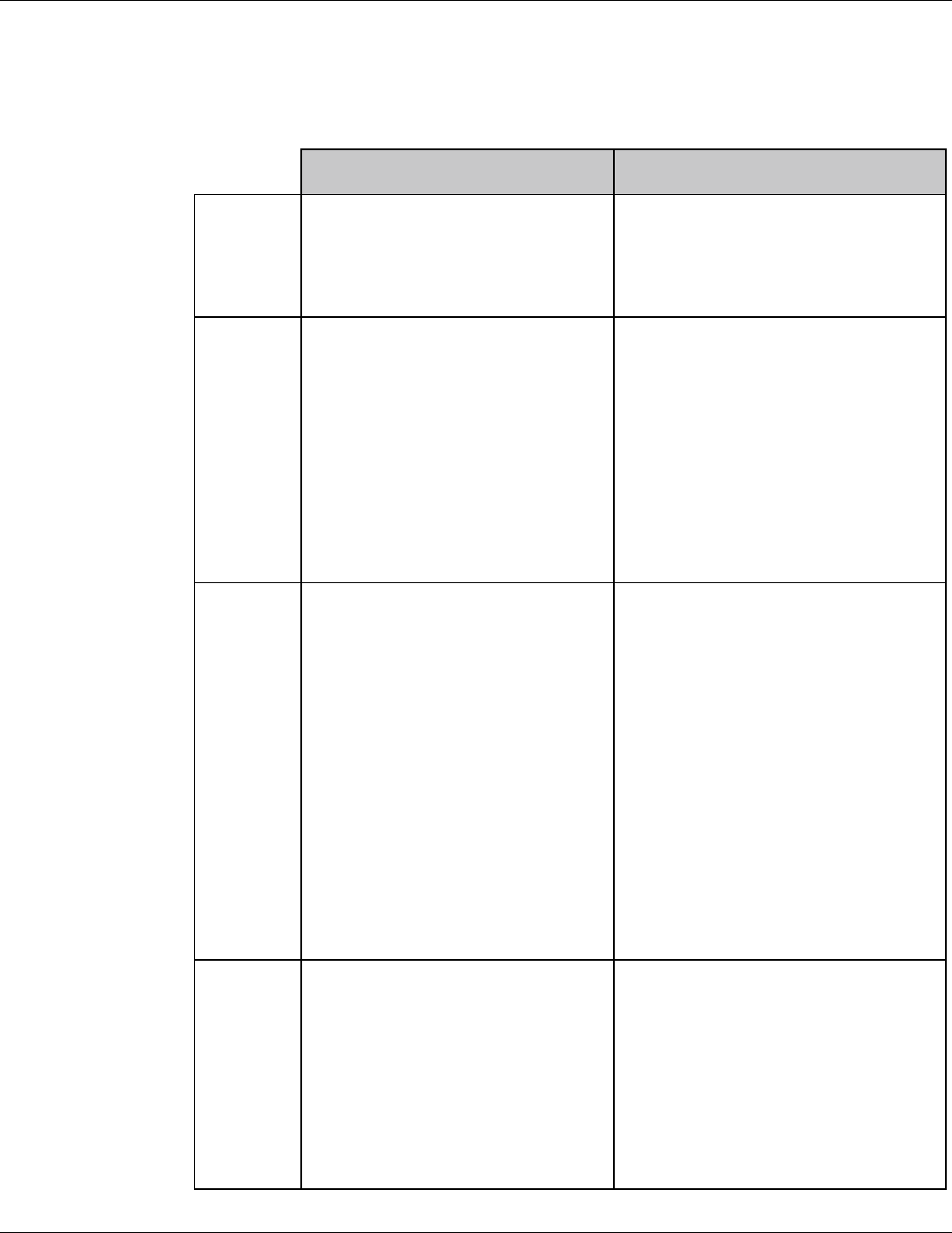
1. “What Matters” Conversations at Certain Care Touchpoints
Care touchpoints for older adults such as regular visits, annual wellness visits, a new diagnosis, a
life-stage change, ongoing chronic disease management, and inpatient visits present opportunities
for “What Matters” conversations (see Figure 1). These types of care interactions tend to be time
limited and specific to a clinical interaction. “What Matters” conversations can and should take
place in various settings, including inpatient hospital, primary care, cancer care, skilled nursing
facility or nursing home, home-based care, and specialty services such as rehabilitation.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 9
Figure 1. Care Touchpoints When “What Matters” Conversations Might Occur
Note that asking older adults about “What Matters” can be difficult in the emergency department
(ED), when decisions need to be made quickly to address the urgent issue at hand. Rather than
initiating “What Matters” conversations in the ED setting, ED care teams are more likely
“customers” of this information, using it to guide care decisions, particularly as patients in the ED
may not be able to communicate their goals and preferences during an emergency encounter.
Documenting “What Matters” information consistently and making it easily and clearly accessible
to clinicians in all settings are the most important factors in ensuring patients’ “What Matters”
preferences are known and respected in the ED.
2. “What Matters” Conversations as Part of Routine and
Recurring Care
Consistently incorporating “What Matters” as part of discussions between older adults and
clinicians is a key part of relationship-based care. These conversations might be broad (e.g., “My
grandchildren and knitting are important to me”) or specific (e.g., “I am worried I will be too weak
to attend a family reunion I’ve been looking forward to next month”).
“What Matters” conversations may be more effective and actionable if anchored to something
the older adult cares about, by connecting their goals and preferences to the impacts of care
and care decisions. “What Matters” conversations must also take into consideration cognition,
health status, and identity.
• A longer annual w ellness visit can be conducive to an initial “What Matters”
conversation. Regular w ellness visits are also an excellent opportunity to continue
“What Matters” conversations over time.
Regular and Annual Wellness Visits
• Schedule an initial “What Matters” conversation one w eek after the older adult has
received a new diagnosis or change in health status, and use this information w hen
planning a course of care.
New Diagnosis or Change in Health Status
• Initiate a “What Matters” conversation during a primary care appointment w ith an
older adult w ho has just entered retirement or enrolled in Medicare. Review “What
Matters” information at each visit follow ing the life-stage change for any updates on
the older adult’s care.
Life-Stage Change
• Discuss “What Matters” during primary care visits, revisiting past conversations and
discussing any changes or updates to the older adult’s goals and preferences.
Chronic Disease Management
• Ask older adults w hat is important to them at every hospitalization and document any
new information.
InpatientVisits (hospital, nursing home, skilled nursing facility)

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 10
Cognition
The care team must consider how older adults’ cognitive status does, and does not, impact their
ability to engage in meaningful conversations about their goals and preferences. Some clinicians
may think an older adult with cognitive impairment is not capable of a “What Matters”
conversation, and thus will not introduce the opportunity or will only speak with the family
or caregiver.
Older adults living with cognitive impairment and dementia are often capable of expressing their
goals and preferences and should participate in “What Matters” conversations to the degree
possible. It is the care team’s responsibility to get to know each older adult and engage with him or
her directly. Careful consideration should be given to the timing of “What Matters” conversations.
There may be times of the day when the older adult is more lucid (e.g., earlier in the day). If there
is significant cognitive impairment, the most important aspect of “What Matters” may be finding
out who the older adult relies most on to help make decisions. The guiding principle is to maximize
autonomy of cognitively impaired older adults and not diminish their self-image (e.g., “changes in
cognition” versus “cognitive impairment”).
4
Health Status
Older adults’ goals and preferences will likely change over time as health status changes. What
matters most to someone who is functionally independent and has few health problems will differ
from someone with functional disabilities and a heavy disease burden. Accordingly, the “What
Matters” conversations to understand older adults’ goals and preferences may need to vary based
on health status.
Identity
It is critical to consider the impact of race, ethnicity, language, religion, culture, and other
identities on how older adults view health and illness, and their preferences and willingness to
engage in conversations about “What Matters.” Issues of trust between some populations (e.g.,
communities of color, the LGBTQ+ community) and the health care system, borne of past
experiences and historic mistreatment, can affect “What Matters” conversations.
Clinicians are also at risk of expressing their own unconscious biases, which may manifest in subtle
verbal and nonverbal ways that can alienate patients. Without trust, it is challenging to truly
understand “What Matters” to inform a treatment plan that incorporates the older adult’s goals
and care preferences.
“What Matters” conversations can open the door to more culturally competent, affirming, and
humble care, as clinicians become better informed about the life and cultural contexts of each older
adult. We recommend that all clinicians undergo training on implicit bias as part of their
preparation for having “What Matters” conversations, using tools like the Project Implicit
assessments
5
and the National Standards for Culturally and Linguistically Appropriate Services
(CLAS) in Health and Health Care.
6
Guidelines from cross-cultural care can help the care team
hav e more successful conversations with older adults from different cultural backgrounds.
7

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 11
Checklist for Culturally Appropriate “What Matters” Conversations
Learn the older adult’s preferred term for his or her cultural identity.
Determine the appropriate degree of formality. Learn the older adult’s preference for how he
or she would like to be addressed and use this title and the surname (e.g., Mrs. Smith), unless
a less formal address is requested.
Determine the older adult’s preferred language. If the older adult has basic or below basic
literacy or English language proficiency, seek permission from the person to have a medical
interpreter assist in the “What Matters” conversation, or determine if a trusted individual
who is literate can be present during the “What Matters” conversation.
Be respectful of nonverbal communication. Watch for body language cues that might be
linked to cultural norms. Adopt conservative body language, use a calm demeanor, and avoid
expressive gestures.
Address issues linked to culture such as a lack of trust, fear of medical experimentation, fear
of side effects, and unfamiliarity with Western biomedical belief systems.
Rev iew the medical records to determine if there has been a history of trauma, including
refugee status, survivors of violence, genocide, and torture. These are v ery sensitive issues
and must be approached with caution. Reassure the older adult of the confidentiality of the
clinician–patient relationship.
Determine the level of acculturation and recognize that this is a factor for individuals who are
recent immigrants, as well as for those who are not recent immigrants.
Recognize health beliefs that include the use of alternative therapies.
Consider how gender or gender identity might affect decision making.
Consider an approach to decision making that recognizes family and community decisions
and does not automatically exclude them in favor of individual autonomy.
Who Should Initiate a “What Matters”
Conversation
Any member of the care team can initiate and document a conversation with an older adult about
their goals and preferences:
• While physicians may be the default care team member guiding care decisions based on an
older adult’s goals and preferences, they may not have time or the communication skills
necessary to engage in these conversations during a visit.
• Nurses, physician assistants, social workers, and medical assistants may have a close
relationship with the older adult and have more time for “What Matters” conversations.
Chaplains, nurse navigators, community health workers, or trained volunteers may also be
able to have meaningful conversations about goals and preferences and record that
information for clinicians to access.
• “What Matters” can also be elicited by self-report (for example, a form sent to an older adult
prior to the annual wellness v isit or filled out while in the waiting room).
Because “What Matters” conversations should be part of an ongoing dialogue, several members of
the interdisciplinary care team may have conversations with the older adult about his or her goals
and preferences at different times (for example, an older adult’s general values preferences may
remain relatively static over time, but specific goals may change from visit to visit). We recommend
that all members of the care team undergo training on motivational interviewing and shared

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 12
decision making prior to engaging in “What Matters” conversations (see Appendix A: Resources to
Support “What Matters” Conversations with Older Adults for additional resources).
Regardless of who on the care team conducts the “What Matters” conversation, there should be
a clear process for documenting and sharing this information. It is important to document and
communicate the older adult’s exact words, as these can be the most impactful. The documentation
process might include a write-in template (see Appendix D for one example), detailed notes in
the electronic health record (EHR) with information on health goals and care preferences, or
(for inpatients) a whiteboard in an older adult’s room that is updated with “What Matters” to
them daily. Whichever method is used, every care team member needs to be trained on where
to record their “What Matters” conversations, and where to find documentation of previous
“What Matters” conversations.
What to Discuss in a “What Matters”
Conversation
“What Matters” conversations are more effective and actionable if they: 1 ) explore the older adult’s
life context, priorities, and preferences and connect them to the impacts of care, self-management,
and care decisions; and 2) are anchored to tangible health or care events in an older adult’s life. It
may be appropriate to have an initial conversation in an outpatient setting that is focused on
understanding an individual older adult’s life context, then follow up with treatment-specific
questions or start a conversation from a diagnosis and specific treatment decisions, and then
broaden the discussion to the older adult’s life preferences.
8

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 13
Understanding Life Context and Priorities
These broad conversations explore what is important to older adults in their lives outside of their
health (e.g., children, family, pets, hobbies), both overall and on the day of the conversation.
Questions should ideally be asked by a variety of health care clinicians in their everyday
interactions with older adults in different settings.
Guiding Questions: Understanding Life Context and Priorities
• What is important to you today?
• What brings you joy? What makes you happy? What makes life worth living?
• What do you worry about?
• What are some goals you hope to achieve in the next six months or before your
next birthday?
• What would make tomorrow a really great day for you?
• What else would you like us to know about you?
• How do you learn best? For example, listening to someone, reading materials,
watching a video.
Anchoring Treatment in Goals and Preferences
“What Matters” conversations are anchored to an older adult’s health status and care needs and
may be most appropriate when there is a new diagnosis, treatment decision, or change in health
status. Questions need to focus on how treatment could facilitate or impede his or her ability to do
the things they enjoy (e.g., walking, cooking, everyday activities) or attain certain life goals (e.g.,
attending a meaningful event). Questions also should focus on a specific time frame, such as six
months or by the next birthday.
Guiding Questions: Anchoring Treatment in Goals and Preferences
• What is the one thing about your health care you most want to focus on so that you can
do [fill in desired activity] more often or more easily?
• What are your most important goals now and as you think about the future with
your health?
• What concerns you most when you think about your health and health care in the future?
• What are your fears or concerns for your family?
• What are your most important goals if your health situation worsens?
• What things about your health care do you think aren’t helping you and you find too
bothersome or difficult?
• Is there anyone who should be part of this conversation with us?

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 14
How to Prepare Older Adults and Caregivers
for a “What Matters” Conversation
Not all older adults are ready to engage in “What Matters” conversations. Most have never been
part of a discussion with a care team member beyond specific medical problems. Some older adults
and caregivers may be concerned that the questions, which are often associated with end-of-life
care, indicate a dire prognosis and spark concern that they may be terminally ill. Some may find
the questions intrusive or are reluctant, unprepared, or embarrassed to share details about their
liv es that they deem unrelated to their health care, or they are looking for more didactic
instructions. Others are willing and eager to guide clinical conversations with their nonclinical
goals. The success of being able to understand “What Matters” to each older adult will depend on
their (and their clinician’s) comfort, readiness, and expectation for incorporating their expressed
goals and preferences into care planning.
One way to prepare for “What Matters” conversations is to present the idea of identifying health
goals and care preferences prior to a face-to-face interaction with the health care system.
Conversations are likely to be more fruitful when older adults reflect in advance of a visit and have
a chance to prepare themselves to talk about their goals and priorities. Additionally, how older
adults respond to being asked depends on the framing, and the care team must be able to explain
why they are asking. Thus, setting the context for the conversation, before it happens, is critical.
Some ideas for how care team members can prepare older adults and their caregivers to have
“What Matters” conversations follow:
• Use a previsit survey, either paper or through a patient-facing EHR portal, to obtain
information about “What Matters” that is reviewed by clinicians prior to a visit.
• Meet with groups of older adults to encourage them to talk with each other about goals,
preferences, and common experiences.
• Utilize existing relationships with community-based organizations, such as faith
communities, to encourage more conversations about “What Matters.”
• Provide older adults with resources to prepare themselves to talk with their clinician, such as
the Prepare for Your Care, Stanford Medicine’s Bucket List Planner, or The Conversation
Project Starter Kits (see Appendix A for more resources).
• Include a “What Matters” brochure in waiting areas, similar to existing brochures on health
care proxies and advance care planning.
• Suggest that the older adult bring a family member, caregiver, or trusted friend to a
conversation about their goals and preferences.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 15
How to Conduct an Effective “What Matters”
Conversation
Below is a list of tasks to complete before, during, and after a “What Matters” conversation. The
guidance generally follows the framework described in the Serious Illness Conversation Guide
from Ariadne Labs: set up the conversation, assess understanding and preferences, share
prognosis, explore key topics, and close conversations.
9
See Appendix B for examples of “What
Matters” conversations.
Before the Conversation
Prepare the older adult for the conversation in advance.
Introduce the idea of talking about “What Matters,” and ask the older adult to do some reflection
prior to the visit, including with his or her family or caregiver, if appropriate. Let the person know
that they will be asked about their goals and preferences. The care team member should explain
why this information is being sought, namely to identify what matters most to the individual so
that care can be better aligned with “What Matters.” This preparation could take place during a
prior visit or as part of previsit paperwork. For specific ideas, see the section in this toolkit on
How to Prepare Older Adults and Caregivers for a “What Matters” Conversation.
Determine who on the care team will have the conversation.
The most appropriate person to conduct the conversation may depend on the care setting and the

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 16
relationship a given care team member has with the older adult. For example, if a physician will
be working closely with the older adult to design a care plan and he or she has the time and skills
to have the discussion, it is beneficial for the physician to facilitate the “What Matters”
conversation. Alternatively, if a nurse, care manager, or other care team member spends a
significant amount of time with the older adult, then one of these people may be better positioned
to facilitate the conversation and communicate the older adult’s needs to the rest of the team.
Time and availability are also factors, which is why training all members of the care team to
facilitate “What Matters” conversations is important to sustaining this work.
Decide on a setting for the conversation.
Hav ing a “What Matters” conversation in a meeting room, sitting around a table as equals, may be
more effective than having the discussion in an exam room, since the meeting room setting can
help reduce the perceived power dynamics between the older adult and clinician. If the
conversation must take place in an exam room, the older adult and care team member should sit
in chairs facing one another, with the older adult dressed in his or her own clothes rather than in
a patient gown, if possible. If the older adult uses a hearing aid, be sure it is turned on. Home is a
good location for the discussion, if feasible. For example, it can be done by a case manager, social
worker, or homecare nurse who already v isits the older adult’s home.
Rev iew the records of previous “What Matters” conversations.
Look over notes of previous conversations about the older adult’s goals and preferences, whether
documented in the EHR or elsewhere, as they may provide a good starting point for the current
conversation and the information may need updating.
Conduct a screen for cognitive impairment to inform approach for a “What
Matters” conversation.
This screening (which should occur routinely in an Age-Friendly Health System) is critical when
preparing for a “What Matters” conversation, given the burden of cognitive impairment among
many older adults. Some potential screening tools include Ultra-Brief 2-Item Bedside Test of
Delirium;
10
naming four legged animals in one minute;
11
drawing a clock face, either in isolation
or as part of the Mini-Cog;
12
and the Short Blessed Test Months Backward Timed.
13
It is important
to bear in mind that memory deficits do not preclude capacity to make decisions about what
matters. If there is cognitive impairment, consider how the older adult’s cognitive status does,
and does not, impact his or her ability to engage in a meaningful conversation about goals and
preferences. Ask the person who they rely on most to help them make decisions and consider
windows of lucidity and timing of these conversations.
Prepare for the conversation.
If y ou will be using any handouts, prompt cards, or education tools, line them up ahead of the
conversation. If the conversation will require an interpreter, include the interpreter in any pre-
meeting team conversations to ensure that they can translate questions in a way that will be
understood by the older adult.
During the Conversation
Invite the older adult to have a conversation.
The success of a “What Matters” conversation depends on having a strong relationship between
the older adult and their care team and both parties’ having similar expectations for incorporating
nonclinical goals in care planning. Begin by asking the older adult if they would like to talk about
their goals and preferences, and (if applicable) how involved they want others to be in the

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 17
conversation. If they are not comfortable or wish for additional people to attend the conversation
(e.g., family member, caregiver), ask what would make them more comfortable and offer the
option to have the conversation at a different time.
Start by asking one or more “What Matters” questions.
See the section What to Discuss in a “What Matters” Conversation for guiding questions on how
to start a conversation. Choosing an approach depends on the purpose of the conversation and
the level of comfort the care team member and the older adult have with talking about “What
Matters.” While scripts can be helpful, many trained staff report not needing a script and prefer
tailoring a conversation based on the older adult and the context. Rather than following a script,
think about the older adult’s health status (e.g., advanced illness, single condition, multiple
chronic conditions, or generally well) and life context. See Appendix A for additional tools
and resources.
Listen carefully and ask questions.
Giv e the older adult time to think and provide answers. Ask follow-up questions as needed, but
do not ask an overwhelming number of questions. Try to ask the fewest number of questions to
obtain the information.
Use training and health literacy tools to facilitate the conversation and provide
clarification.
Being able to successfully communicate health or clinical information is a critical component
of a successful “What Matters” conversation. Once the care team member identifies the
communication method that is most comfortable for the older adult, it may be helpful to use
health literacy tools such as education videos, flash cards, or pamphlets to communicate clinical
information. Asking the older adult to explain the clinical information in their own words (the
“Teach-Back” approach) will also help confirm that the information has been effectively
communicated. Note that “Teach-Back” may not be effective for those with executive dysfunction.
Affirm the conversation for the older adult.
Throughout the conversation, the care team member should take time to 1) acknowledge the older
adult’s thoughts and feelings; 2) confirm the older adult’s understanding of what they are
communicating; and 3) ask for clarification of anything that is unclear. If the older adult has
chosen to include other people in the conversation, this can also be a time to ask whether they
need any clarification from either the clinician or the older adult.
After the Conversation
Incorporate “What Matters” information into the care plan.
Once the care team has had the “What Matters” conversation with the older adult, the next step is
to incorporate their expressed goals and preferences into their care plan. By anchoring an initial
“What Matters” conversation around specific points in the care process during which decisions
about care are likely to be made (e.g., first v isit, new diagnosis, change in health status, or life
transition), the team may be in a better position to build a clinical care plan that reflects the older
adult’s goals.
If the conversation involves clinical decision making, we recommend the following steps:
• Present personalized evidence, considering all steps above, to help the older adult
reflect on and assess the impact of care decisions regarding their goals, preferences,
and lifestyle.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 18
• Identify choices the older adult can make and evaluate the clinical research in the
context of their life.
• Help the older adult reflect on the impact of different options on themselves and
their family.
• Come to a decision point with the older adult and family (when appropriate).
• Agree on next steps and plan for follow-up.
Document the “What Matters” conversation.
Document the conversation, ideally in the EHR, immediately following the conversation’s
conclusion, or within 24 hours. Use the person’s own words as much as possible (e.g., “Leslie
would like to be able to walk around the block” rather than “Patient wants to mobilize”) and use
tags to make preferences and goals readily searchable in the medical record (see section on
Documenting “What Matters” information for more guidance on incorporating “What Matters”
in the EHR).
Share information with the care team.
If appropriate, discuss conversation outcomes with the care team during regular team huddles.
If the team does not currently conduct regular team huddles, the Better Care Playbook provides
strategies for care teams to use huddles.
14
If any information requires immediate action, share
with appropriate care team members as soon as possible.
Continue the conversation.
During the next encounter with the older adult, revisit the previous “What Matters” conversation,
discuss any new or changing topics, and update the conversation documentation in the EHR or
the agreed upon location for storing documentation.
Documenting “What Matters” Information
Reliable and timely documentation of the older adult’s goals and preferences is a critical step in the
“What Matters” process. Documentation of the conversation should be easily accessible to the
older adult and all members of the care team so that it can be reviewed and referenced on a regular
basis and during care planning. All documented information should be clear, concise, reflective of
the older adult’s stated goals, and recorded using his or her own words as much as possible.
Where to Document “What Matters”: High-Tech and
Low-Tech Solutions
Where a care team chooses to document goals and preferences depends on available infrastructure
and care context. A whiteboard or construction paper poster can be a quick and highly visible way
to document and update “What Matters” for an older adult in an inpatient setting, but it is not
easily sharable across settings and not a practical method for documenting information in a
primary care or outpatient specialty care setting. Documenting “What Matters” in an EHR allows
clinicians to document conversations in more detail and allows the information to be reviewed over
time and by multiple members of the care team.
Both methods may be used in tandem to document both short- and long-term preferences and care
goals, depending on the care setting. Table 1 compares using physical versus electronic health
records for documentation.
TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 19
T able 1. Considerations for Documenting “What Matters” Conversations in Physical
v ersus Electronic Formats
Physical Record
Electronic Health Record (EHR)
Ideal for
• Inpatient/long-term care
• Recording small amount of
information quickly (e.g., one or
two sentences)
• Inpatient and outpatient care
• Long-term recording
• Recording detailed conversations
• Sharing information across care
settings
Pros
• Low cost
• Easy and quick to document
and update
• Easily visible to any member of
care team who enters older
adult’s room
• Does not require changes to
hospital information technology
(IT) infrastructure
• Does not require significant
training resources
• Readily accessible to all members
of the care team who have access
to the EHR, regardless of location
• Can document “What Matters”
conversations over time
• Can document conversations with
more detail
• All health-related information is
stored in one centralized location
• Can link older adult’s goals and
preferences with key documents
such as advance care plan
Cons
• Not shareable across different
care settings
• Not good for documenting large
quantities of or nuanced
information
• Not easily available to members
of the care team who do not
visit older adult’s room
• Not a viable method for long-
term recording
• Not effective for outpatient or
primary care setting where
exam rooms are used by
multiple patients throughout the
day
• Not private, which could make
some older adults
uncomfortable
• Requires significant initial
investment in EHR infrastructure
modifications
• Requires care team members to
take time to enter information
• Care team members must be
trained on new processes for
documenting “What Matters” in the
EHR
Examples
• Asking a hospitalized older
adult “What matters to you
today?” during daily rounds and
documenting responses on a
whiteboard in the patient’s room
• Paper “Patient Passport”
booklet that older adult is
responsible for carrying to and
from appointments
• Creating “tags” in the EHR for all
notes that contain information on
older adults’ goals and
preferences
• Creating “flags” to remind
clinicians to update “What Matters”
information
• Documenting the older adult’s
goals in Plan of Care section of
the electronic record

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 20
Documenting “What Matters” in the Electronic Health Record
If the organization’s EHR includes a patient portal, they may want to create a module for older
adults to enter and review relevant health care proxy information, advance directives, and
important notes on their care goals. Specific guidance for different EHR vendors is challenging
giv en variability between organizations and the newness of this work. While most examples are
from organizations using Epic, the guidance for Epic could contain some applicable lessons for
other EHRs. Some suggestions follow:
• Creating tags: Tags are keywords used to link notes in EHRs and can be used to indicate
that a note contains “What Matters” information or any record of a serious illness
conversation. Once a tag has been created, Epic can be configured so that notes with specific
labels appear first in the record. This can be used to ensure that “What Matters” information
is clearly available to whoever is checking the medical record.
• Using the “Longitudinal Plan of Care” or other care planning feature: These
provide a central location for documenting “What Matters” conversations.
• Using a patient-facing portal: Many EHRs have patient-facing portals that allow patients
to directly message their clinicians, attend e-visits, and complete questionnaires remotely.
15
This tool can be used to send questionnaires about “What Matters” to older adults prior to
visits. Clinicians can then use this information to facilitate further discussion.
• Requesting a custom build: Some organizations have worked with their EHR v endors to
build a template that works for their care team. A custom-built template may include the
following sections:
○ Self-perception of health status and trajectory
○ Health and health care concerns and fears
○ Values
○ Health goals
○ Care preferences

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 21
Incorporating “What Matters” Information
into the Care Plan
Once the care team has begun the process of talking with an older adult about “What Matters” to
them, the next step is to incorporate their expressed preferences and goals into their care plan. By
anchoring an initial “What Matters” conversation around specific points in the care process during
which decisions about care are likely to be made (e.g., first visit, new diagnosis, change in health
status, or life transition), the team may be in a better position to build a clinical care plan that
reflects the older adult’s goals.
Below are some key strategies to ensure that an older adult’s expressed goals and preferences are
incorporated into their plan of care.
• Patient education as part of care planning. Because most patients are not medical
professionals, they may not be as knowledgeable about the harms and benefits of various
treatment and care options. Applicable decision aids (e.g., patient education v ideos, flash
cards) may be used to educate them and support conversations about various options and
tradeoffs in some care decisions. While such aids can be useful for relevant decisions, they are
not a substitute for a conversation to elicit the issues that are most important to older adults.
Additionally, the uncertainty of benefits and harms of treatment options for older adults
makes the traditional approach of decision aids and shared decision making less effective.
16
It
is incumbent upon the clinicians to understand each patient’s goals and preferences and offer
treatment options within the context of those goals and preferences.
• When an older adult’s preferences conflict with clinical advice. Generally, an older
adult’s goals and preferences should be respected as much as possible when planning their
care with them. However, in some cases, an older adult may have preferences that are in
direct conflict with their clinician’s medical advice, or they may reject the advice of a clinician.
If this is the case, more communication about “What Matters” to them may lead to more
clarity about why they are rejecting certain options or plans. Both the older adult and the
clinician may need to re-evaluate their perspectives and work together to find alternatives.
• Leveraging interdisciplinary resources to address older adults’ needs. When
asking older adults about “What Matters” to them, many of their preferences or concerns may
inv olve social determinants of health on which a clinician is unable to have a direct impact
(e.g., housing, food, access to social services). This is where having an interdisciplinary care
team can be critical — a social worker or nurse navigator, for example, may be able to connect
people with additional resources outside of the clinical sphere. Some teams use regular (e.g.,
weekly) interdisciplinary team huddles to discuss the results of that week’s “What Matters”
conversations and share resources that can be used to address older adults’ concerns. Sharing
these stories and problem solving together also helps build will and improve satisfaction
among members of the care team.
• Engaging with community resources. In addition to the interdisciplinary care team,
community-based organizations can be excellent resources for addressing needs beyond the
health system. Maintaining a list of community organizations that can provide support for the
social determinants of health (e.g., housing, food assistance, transportation, financial
support, behavioral health) can facilitate the provision of referrals. Documenting any referrals
giv en to an older adult during a “What Matters” conversation in the EHR also allows
clinicians to follow up on these social determinants during subsequent v isits.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 22
Measuring “What Matters”
Why measure “What Matters”? The right measures can help improve how well the care team
understands, documents, and acts on “What Matters” to older adults. Measurement for
improvement relies on relatively frequent observations, tracked over time, to guide and maintain
changes to work.
T able 2. “What Matters” Measures
Process Measure: Documentation of “What Matters”
Why Measure Documentation of “What Matters”?
Documentation of “What Matters” signals that the care team has engaged the older adults they
serve in these conversations, and this documentation will guide the team as they develop and carry
out care plans aligned with “What Matters” for each older adult.
The process measure for “What Matters” documentation is the percent of patients served by the
relevant hospital unit or primary care team who have documentation of “What Matters” at the end
of each measurement period. Appendix C gives measurement details for inpatient and primary
care sites.
Tips for Getting Started with Measuring Documentation of “What Matters”
• Create examples. Have two care team members create or find at least three examples that
the team leaders consider to be acceptable documentation. What features do the examples
hav e that make them acceptable? Creating some good examples is a start to a formal
development of an “operational definition” to support consistent measurement.
• T est the measure.
○ Test 1: Have a care team member (a “tester”) who will be testing the measure review the
examples of good documentation. Look at one new instance of documentation. Can the
tester decide whether the documentation is acceptably aligned with the “What Matters”
questions and interaction proposed by the care team? If the tester cannot decide, what
features of documentation are missing that would enable a decision?
○ Test 2: Repeat Test 1 for five instances of documentation.
○ Test 3: Have two members of the care team assess the same three patient records for
quality of “What Matters” documentation. Compare their decisions. If two care team
members disagree on one or more decisions, discuss differences and propose changes to
the features (or criteria) that characterize good “What Matters” documentation.
Measure Type
Measure Name
Process
Documentation of “What Matters”
Outcome
Care Concordance with “What Matters”
Balancing
Impact on the Care Team

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 23
• A target goal for documentation of “What Matters” should be 95 percent or
greater. This means there is documentation showing the care team has engaged 95 percent
or more of older adults in their care in “What Matters” conversations. Remember that the
process should allow patients to decline to engage in “What Matters” conversations; an older
adult who declines to answer should be included in the numerator for this process measure.
The care team will have to assess whether the percent of older adults who decline to answer is
acceptable. If it is too high, this could be an area for study and improvement.
• Apply quality improvement methods to improve documentation. Directly observe
the documentation steps and have the care team member doing the documenting talk out
loud about the task, focusing on what is difficult or confusing. What can be changed to make
it easier to document “What Matters”? Another idea is to review 10 patient records that do
not meet the health system’s standard for documentation to identify features of poor
documentation. Then, identify one problem that can be mitigated or prevented. Test changes
to address this documentation problem.
Outcome Measure: Care Concordance with “What Matters”
Why Measure Care Concordance with “What Matters”?
While alignment between “What Matters” to older adults and the care they receive has been
studied for care at the end of life, understanding and aligning care with “What Matters” for all
older adults, regardless of life stage or prognosis, is critical.
There is currently no consensus or widely used approach to measure care concordance with “What
Matters,” though there is great interest in this topic and health systems will be actively testing and
learning how to measure concordance in the future. We know enough now to get started and learn
by doing.
The outcome measure tracks answers to closed-ended questions about care experience and “What
Matters” (see the table in Appendix C for details).
If the health system already asks specific populations about the concordance of care with “What
Matters,” then they should continue to use those tools. For example, a survey used for patients of
palliative care services at Trinity Health includes some questions that touch on concordance of care
with “What Matters,” ranked on a 1 -to-5 scale (very poor to very good). These include: 1) degree to
which the care team addressed the patient’s emotional needs; 2) the care team’s effort t o include
the patient in decisions about his or her treatment; 3) the care team’s respect of the patient’s
wishes regarding continuing or discontinuing statements.
Most hospital units and primary care practices will not yet measure care concordance with “What
Matters.” The next section introduces the collaboRATE™ tool to meet that need.
Introduction to the collaboRATE Tool
collaboRATE questions, developed by researchers at The Dartmouth Institute for Health Policy &
Clinical Practice, are appropriate after a specific clinic visit or during a hospital stay.
17
• For a clinic v isit, the questions should be asked before the patient leaves the clinic.
• For a hospital stay, the questions may be asked at any time after the first day of stay when the
patient is able to communicate with the care team. Integration of collaboRATE into the

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 24
course of care during the stay or at discharge increases the number of responses (rather than
sending a post-discharge questionnaire).
• For those patients unable to communicate, there is a version designed for individuals acting
on behalf of patients.
The wording of the three questions and the appearance of the scales have been tested and should
not be varied, though the opening statement can be varied to make it appropriate for the setting.
Note that the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)
guidelines may need to be reviewed prior to regular use of collaboRATE in hospital settings.
Getting Started with Measuring Care Concordance with “What Matters”
As collaboRATE will be a new measurement tool for most health systems, care teams will need to
figure out how to capture and summarize the question scores.
• Go to the collaboRATE Measurement Scales to find specific v ersions appropriate to your
populations (a Creative Commons license allows for free, noncommercial use).
• Consider joining the collaboRATE users group to learn more about practical use of the tool.
• Share the collaboRATE tool with relevant staff. Ask: What should we change so that almost
every patient will answer “9” to all three questions?
Outline a method to capture answers to collaboRATE and summarize top-box scores.
collaboRATE has been tested using different approaches; while response rates vary, researchers
found similar clinician performance across different data collection approaches.
18
Spreadsheet or
paper systems can suffice for initial testing and local application. REDCap software can also be
used to collect responses. Finally, health systems may want to investigate a third-party automated
solution, using existing patient portals or messaging systems, that maintains anonymity and helps
with clear reporting.
Learn about collaboRATE by testing to improve measurement. For example:
• Test collaboRATE with one patient. Ask: How will the care team member introduce the
questions? How will they record the answers?
• Test collaboRATE with five patients. What does this test indicate about collaboRATE’s
impact on workflow? What will it take to engage with patients and document answers
consistently?
• Repeat tests with older adults who prefer a language other than English.
Alternatives to Care Team Use of collaboRATE in a Hospital Setting
The collaboRATE questions and scale format, in principle, can be added to post-discharge patient
surveys administered after HCAHPS. This requires discussion with the hospital’s patient
experience survey vendor to determine if the collaboRATE questions can be included.
If it is not possible to use collaboRATE, hospitals can track the HCAHPS nurse communication
composite (HCAHPS questions 1, 2, 3) and physician communication composite (HCAHPS
questions 5, 6, 7) for patients 65 years and older who are treated in the relevant unit. Note that this

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 25
option will be of limited effectiveness if there are low counts of patients 65 years and older who are
surveyed and respond to the survey.
Additionally, hospitals can also conduct regular conversations with patients 65 years and older
about the alignment of their care with “What Matters.” A related project carried out by National
Health Service Scotland suggests five conversations a month provide a good basis to monitor
performance and provoke improvement ideas.
19
Some ideas for these conversations include:
• Ask two open-ended questions:
○ How well did we include “What Matters” to you in choosing what to do next?
○ What could we do better?
• Record the responses verbatim; don’t attempt to reword or analyze.
• Rev iew the verbatim responses with your team once a month. What ideas emerge that you
can test to improve alignment of “What Matters” with patient experience of care? Then, test
the ideas.
Balancing Measure: Impact on the Care Team
Balancing measures detect unintended consequences of a new intervention. This balancing
measure assesses the impact of “What Matters” efforts on the care team. Short term, the care team
needs to know if their approach to engaging patients and documenting “What Matters” is feasible.
Long term, the care team needs to know if engaging patients in “What Matters” conversations
causes stress, if the task of documentation creates a burden, or if follow-through into care planning
falls short. Too much stress or burden leads to inconsistent engagement in “What Matters” and can
contribute to staff burnout.
It is not necessary to create a formal survey or questionnaire to learn about work burden and
barriers to “What Matters” conversations, documentation, and use in care planning. Leaders
should instead commit to regularly asking care team members, once a month, two questions:
• What are we doing well in our “What Matters” conversations?
• What do we need to change to translate “What Matters” to our patients into more effective
care?
Tips for Getting Started
• To encourage care team members to continue to respond to the two questions, it is critical to
show that leaders are listening to their responses and acting on them. One approach is to
engage the team in testing one or more ideas and discuss together what was learned, with the
aim to make the “What Matters” work easier.
• If the question responses are collected during a team huddle or meeting and recorded on a
flipchart or whiteboard, take a digital photo so there is a time-stamped record.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 26
Conclusion
The practice of asking “What Matters” is gaining traction around the world. Still, there remains a
gap between what care team members know about what matters to their patients and what care
patients receive in accordance with their goals and preferences. This toolkit was designed to bring
together the best available current information about how clinicians and health care organizations
can ask and act upon “What Matters” to older adults and ensure that each older adult’s health
outcome goals and care preferences are understood, captured, and integrated into their care.
Even as the number of older adults who are engaged in “What Matters” conversations increases,
this remains an area in need of additional development and testing. This toolkit is a starting place
and an invitation to learn together how to better understand and act upon “What Matters” and
measure progress in doing so. We welcome feedback and shared learnings from organizations that
are undertaking the “What Matters” work as part of their efforts to provide age-friendly care. Email
us at: AFHS@IHI.org.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 27
Case Examples
Providence St. Joseph Health, Oregon Region
Providence St. Joseph Health, Oregon Region, began developing a process for operationalizing
“What Matters” conversations with older adults in February 2017. They initially formed an
exploratory workgroup, comprising a medical director, chaplain, physician, nurse, and social
worker. This workgroup shared their knowledge and experiences in asking “What Matters,” and
discussed what was needed to make this work valuable to patients and the organization. The
workgroup then used their shared knowledge, along with resources from the literature, “What
Matters” work at NHS Scotland, and the Serious Illness Conversation Guide to develop guidelines
for successful “What Matters” conversations.
After reviewing the first draft of the guidelines, frontline care team staff reported that the
guidelines did not provide specific enough guidance for structuring and conducting “What
Matters” conversations. The workgroup gathered comments and feedback from care teams
and created a list of suggested questions, introduced with the phrase “You can consider using the
following…” A second draft was developed and disseminated to frontline staff to begin testing
with older adults in two service lines: one primary medical home, and one elder at-home outreach
program.
Following a first round of testing with five patients, the frontline care teams debriefed their
experiences with the workgroup, who then used their feedback to revise the guidelines.
This cycle of testing is still ongoing, with the number of patients increasing each cycle. The
workgroup meets once every 2 to 3 weeks to review feedback from the frontline care teams
and revise the guidelines.
To date, the workgroup has noted the following learnings:
• Including an opening statement for clinicians to initiate “What Matters” conversations is
helpful in making clinicians and patients feel more comfortable with having a conversation.
• “What Matters” conversations have typically been shorter than clinicians anticipated.
• The guidelines have been modified to indicate that a family member or surrogate should
always be present during conversations with patients with dementia.
• Stories about rewarding experiences of “What Matters” conversations and how the
information from them is integrated into care planning is particularly motivating for frontline
team members.
Providence St. Joseph Health has also integrated “What Matters” information into their Epic EHR
sy stem using two custom-built modules (developed internally): one for advance care planning, and
one for goals.
Stanford Health Care, California
To better understand diverse patient perspectives, a team at Stanford Health Care conducted a
multisite, multilingual (English, Spanish, Burmese, Hindi, Mandarin, Tagalog, and Vietnamese)
study with the help of medical interpreters. All patients in the study uniformly reported that
discussing “What Matters” was very important to them, and a majority (60.6 percent) identified a
communication chasm between doctors and patients, and cultural/religious factors as barriers. All

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 28
were very open about expressing what mattered most to them and their goals and values if this
could be done in simple language.
In close partnership with numerous patients and family members, a simple letter template (in
a question-and-answer format) was written at a fifth-grade reading level in eight different
languages. This template was reviewed and refined based on input provided by Stanford’s Patient
Family Advisory Council (PFAC). By answering some simple questions, this template allowed
patients to share what matters most to them, their future life milestones, and wishes for care.
Patients could also choose to write a more personal “last letter” to their friends and family using
a second template.
Stanford Health Care formed an interdisciplinary team to implement the What Matters Most
(WMM) letter, including representatives from geriatrics and palliative care, blood and marrow
transplant, quality improvement, spiritual care service, nursing, patient advocacy, risk
management, legal counsel, information technology, social work, and patient care services.
A two-hour “train the trainer” training was conducted for a large group of volunteers from the
spiritual care service on how to answer questions from patients and families about the WMM letter
and how to complete the letter. Participants who attended the “train the trainer” workshop held
training sessions for multidisciplinary clinic staff, including physician assistants, advance practice
nurses, and social workers, to use the WMM letter to elicit what matters most to the patients and
to complete the letter advance directive.
A small cluster-randomized study was conducted in which the medicine ward teams were
randomized to the WMM letter arm or usual care arm. Patients admitted to the ward teams in the
WMM arm completed the letter. Patients in the usual care arm completed the traditional advance
directive. All ward care teams were given copies of their patients’ completed WMM letters (letter
arm) or advance directives (usual care arm).
For both study arms, clinician understanding of their patients’ goals of care and values was
assessed. Most clinicians preferred the WMM letter (92 percent), reporting that it: 1) improved
their understanding of the patient’s goals of care; 2) gave them more assurance in guiding the
proxy decision makers in making decisions on behalf of the patient; 3) captured end-of-life
preferences in the patient’s own words; and 4) helped clarify patient v alues and family dynamics.
Clinicians who had patients’ WMM letter (letter arm) were also more likely to know their patients’
preferred site of death (7 9 percent versus 20 percent of responses respectively, p<0.05) than
clinicians who got the advance directives (usual care arm). Clinicians reported that the WMM
letter helped them gain a better understanding of their patients’ preferences for care compared to
the traditional state-approved advance directives and the Provider Orders for Life-Sustaining
Treatment (POLST).
Patient groups have also been convened to help patients write their WMM letters in an informal
setting. One facilitator is typically needed for every 10 patients, and each session lasts
approximately 1 hour. Groups as large as 40 patients have been convened, with three to four
facilitators to help them. When conducting groups with patients with limited English proficiency, a
medical interpreter is present and sessions typically last 80 to 90 minutes.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 29
Appendix A: Resources to Support “What
Matters” Conversations with Older Adults
Online Tools
• Decision Worksheets (Health Decision Sciences Center, Massachusetts General Hospital):
Worksheets for diabetes, depression, high blood pressure, high cholesterol, and acute low
back pain, as well as guides for using the treatment worksheets during visits
• Geritalk: Communication Skills Training for Geriatrics and Palliative Medicine Fellows
20
• Hebrew Senior Life – Vitality 360 Program: Comprehensive wellness and exercise program
offered at Orchard Cove (part of Hebrew Senior Life)
• How’s Your Health? Patient Checkup Survey: Tool for assessing patient self-confidence in
health management
• Patient Priorities Care: Resources to support aligning care with what matters most to
patients. The Specific Ask (Matters Most) Conversation Guide and the Patient Priorities
identification conversation guide help identify the values, outcome goals, and care
preferences for older adults with multiple chronic conditions
• Person-Centred Health and Care Programme (Healthcare Improvement Scotland): Practical
guidelines for person-centered health care
• Preference Based Living and the Preference for Everyday Living Inventory: Tools and
resources for assessing individual preferences for “social contact, personal development,
leisure activities, living environment, and daily routine,” both at home and in nursing homes,
including the Preferences for Everyday Living Inventory (PELI)
21
• Project Implicit (Harvard University): Tests for identifying social attitudes and implicit
associations
• Shared Decision Making National Resource Center (Mayo Clinic): Tools and resources for
clinicians to use in practicing shared decision making with patients, including patient
decision aids, trainings, and workshops
• Stanford Medicine Bucket List Planner: Tool for reflecting on core values and goals through
“bucket list” planning
• Stanford School of Medicine Ethnogeriatrics Ethno Med Website: Resources for providing
high-quality geriatrics care to a multicultural population
• STEPS Forward: An online physician education module that guides physicians through how
to discuss end-of-life decisions with patients and caregivers
• Transforming Patient Experience, The Essential Guide (NHS Institute for Innovation and
Improvement) (Archived): Results from the UK National Health Service (NHS) on developing
an ev idence base on what matters to patients
Blog Posts
• Bisognano M. “Why ‘What Matters to You?’ Matters Around the World.” Institute for
Healthcare Improvement Blog. February 24, 2017.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 30
• Kassam-Adams N. “Asking (and Listening to) Pediatric Patients” Health Care Toolbox Blog.
May 16, 2016.
• Pickard L. “Asking Pediatric Patients, ‘What matters to you?’” Institute for Healthcare
Improvement Blog. March 18, 2016.
Conversation Guides
• Conversation Ready (IHI White Paper): Framework to help health care organizations become
“Conversation Ready” (i.e., reliably support clinicians and patients in having end-of-life
conversations, documenting these conversations, and providing concordant care)
• How to Talk to Your Doctor Starter Kit (The Conversation Project): Conversation guide for
individuals to use when having conversations to articulate end-of-life goals and care
preferences
• Y our Conversation Starter Kit for Families and Loved Ones of People with Alzheimer’s
Disease and Other Forms of Dementia (The Conversation Project): Conversation guide for
end-of-life care goals and preferences, with specific considerations for caregivers of
individuals with different forms of cognitive impairment
• Serious Illness Conversation Guide (Ariadne Labs): Conversation guide for clinicians that
outlines steps for having conversations with seriously ill patients about their goals and values
Books
• The Ethnogeriatrics Steering Committee of the American Geriatrics Society. Doorway
Thoughts: Cross-Cultural Health Care for Older Adults (volumes 1, 2, and 3). Sudbury, MA:
Jones & Bartlett Learning; 2008.
• Cruz-Oliver D. Hospice/Palliative Care: Concepts of Disease and Dy ing. In: Cummings-
Vaughn L, Cruz-Oliver DM (eds). Ethnogeriatrics: Healthcare Needs of Diverse Populations.
New York, NY: Springer Press; 2016.
• Schein EH. Humble Inquiry: The Gentle Art of Asking Instead of Telling. 2013.
Audio/Video
• WIHI: Realizing “What Matters” to Patients and Families (Podcast)
• “What Matters to Me” from Yorkhill Children’s Hospital (Video)
Commercial Tools and Trainings
• PatientWisdom: Online digital platform for connecting patients and clinicians
• Vitaltalk: Online faculty development courses on improving communication skills
• Motivational Interviewing Network of Trainers (MINT): Online network of trainers for
motivational interviewing, including a library of resources and event and training listings
• Cake App: Mobile app with end-of-life preference and planning tools
• PREPARE for Your Care: Online tools for advance care planning and advance directives
• Massachusetts General Hospital Health Decisions Science Center: Multidisciplinary research
group that provides tools and trainings on shared decision making and informed medical
decision making, including decision worksheets
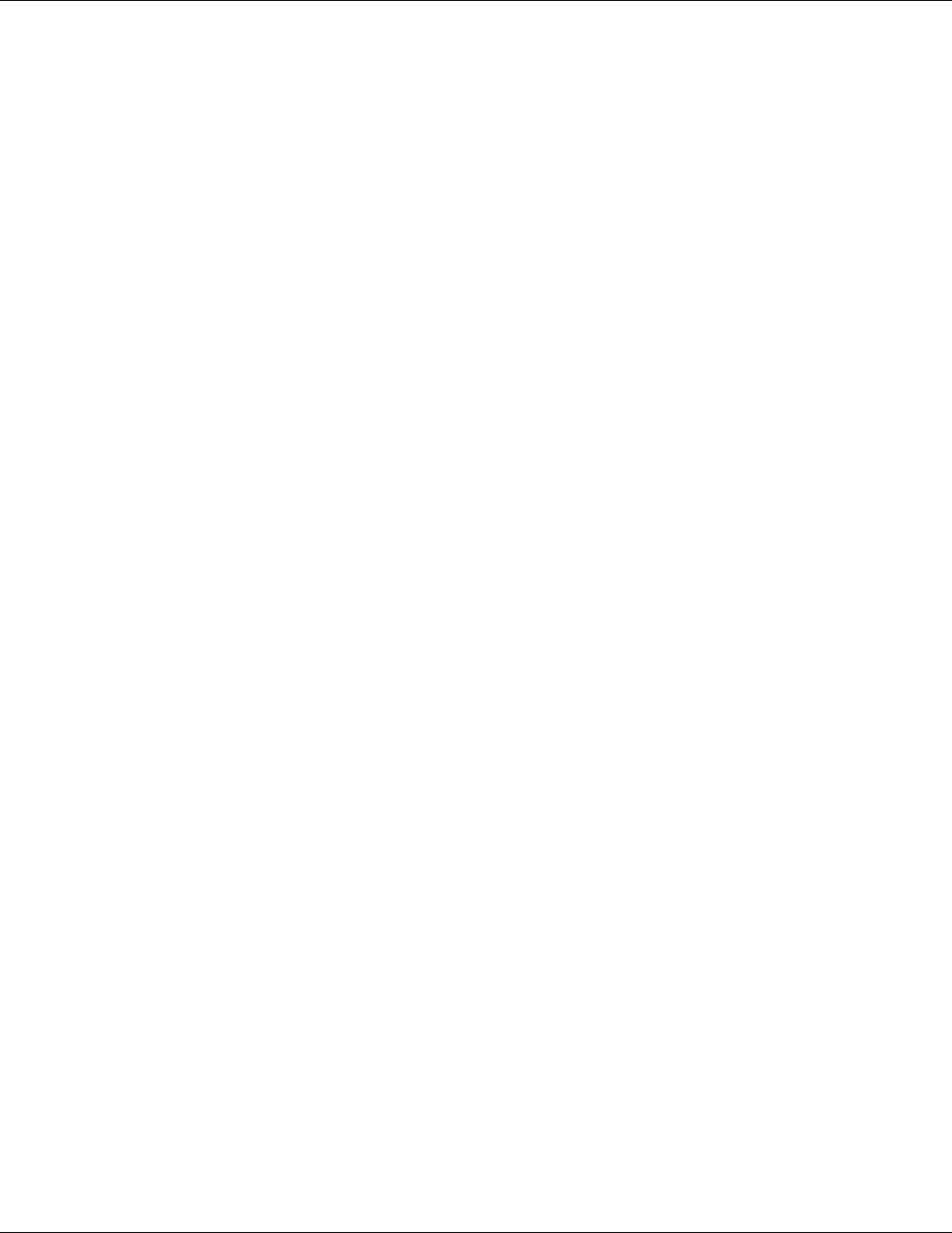
TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 31
Appendix B: Examples of “What Matters”
Conversations
Example: Newly Retired Man with Diabetes
Peter is 68 and has been managing his Type 2 diabetes and moderate hypertension for the past two
y ears. Peter is getting ready to retire and wants to spend more time gardening and traveling
around the country in an RV with his wife. His primary care physician (PCP) has prescribed
multiple medications to control his hypertension as well as regular appointments to monitor
Peter’s blood glucose, which has been difficult to get in control despite dietary changes.
At an annual wellness visit, the PCP asks about goals and preferences around Peter’s retirement.
Peter is nervous about bringing it up but mentions that he often feels lightheaded from the
hy pertension medication and, as a result, is not able to garden as much each day as he would like.
Peter also mentions that the weekly doctor’s appointments his doctor has requested will affect his
ability to go on longer trips. It’s important to him that his diabetes and hypertension are well
managed, but he worries that this management is making his life less enjoyable. This creates an
opportunity for Peter and his PCP to have a conversation about how to reconcile his physician’s
goals around hypertension and diabetes management with Peter’s goals for doing what he enjoys.
Example: New Diagnosis
Last week, Carol, age 81, was diagnosed with colon cancer. Four days after her diagnosis visit, a
nurse navigator called Carol to schedule an appointment to talk about “What Matters” to her and
treatment options. The nurse navigator sets up an hour-long appointment and arranges for Carol
to meet her in a small conference room rather than an exam room. The nurse navigator starts the
conversation by asking Carol specific questions about her health preferences and goals. He then
broadens the conversation to talk to Carol about what her hopes, fears, and concerns are for her
health as well as how her health could impact her ability to do what she enjoys. Carol notes that she
is not afraid of dying, but she is afraid of missing out on important time and events with her family,
and it is important to her that she be able to spend as much time with them as possible. Carol tells
the navigator that she wants to start treatment soon, but also wants to be able to attend her
granddaughter’s wedding in two months.
The nurse navigator shares this information with Carol’s oncologist, who then sits down with Carol
to talk about options for the timing of chemotherapy so that Carol will be able to see her
granddaughter get married. Carol and the oncologist also discuss how different treatment options
may affect her prognosis, her ability to stay at home, and other aspects that may impact her ability
to spend time with her family and attend important events. As Carol begins her course of
treatment, the nurse navigator checks in with her monthly by phone about how her treatment is
going and whether any of her preferences have changed. At the beginning of every appointment,
Carol’s oncologist reviews notes in the EHR from previous visits and calls with the nurse navigator,
and takes five minutes at the beginning of the appointment to follow up with Carol on any changes
or updates.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 32
Appendix C: Detailed Information on “What
Matters” Process and Outcome Measures
Process Measure: Document “What Matters”
Hospital Setting
Measure Name
Documentation of “What Matters”
Measure
Description
Percent of patients with documentation of “What Matters” conversations
(calculated as: numerator/denominator x 100)
Site
Inpatient unit
Population
Measured
Patients 65 years or older
Measurement
Period
Weekly or monthly
Weekly measurement will support faster testing and learning cycles but
has consequently higher measurement burden and may not be feasible.
Numerator
Inclusion: Patients in the denominator with documentation of “What
Matters,” per the unit's definition of “What Matters.” Your process should
allow patients to decline to engage in “What Matters” conversations — an
older adult who declines to answer and has “declined to answer”
documented should be included in the numerator.
Exclusions: None
Denominator
Inclusion: Patients with length of stay (LOS) >= 1 day present on the unit
between 12:01 AM on the first day of the measurement period and 11:59
PM on the last day of the measurement period.
Exclusions: None
Method Details
1. Asking “What Matters” is defined by the unit for the patients it serves.
At a minimum, asking “What Matters” involves: a) querying the medical
record for existing documentation of goals and preferences; and b)
engaging patients in discussion of “What Matters” to them as defined
by the unit.
2. Documentation standard is defined by the unit for the patients it
serves; standard describes the information that is recorded and the
method of recording that information.
3. If an automated report is possible, calculate denominator and
numerator.
4. If a complete manual tally is possible, calculate denominator and
numerator.
5. If neither an automated report nor a complete tally is possible, sample
records at the end of the measurement period and calculate numerator
and denominator. You can apply a stopping rule to reduce
measurement effort.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 33
Primary Care Setting
Measure Name
Documentation of “What Matters”
Measure
Description
Percent of patients with documentation of “What Matters” conversations
(calculated as: numerator/denominator x 100)
Site
Primary care
Population
Measured
Patients 65 years or older
Measurement
Period
Monthly
Numerator
Inclusion: Patients in the numerator with documentation of “What Matters”
within 12 months of the most recent office visit, home visit, or telemedicine
visit in the measurement month, per the primary care unit's definition of
“What Matters.” Your process should allow patients to decline to engage in
“What Matters” conversations — an older adult who declines to answer
and has “declined to answer” documented should be included in the
numerator.
Exclusions: None
Denominator
Inclusion: All patients in the population considered to be patients of the
primary care practice (e.g., patients assigned to a care team panel and
seen by the practice within the past three years) who have an office visit,
home visit, or telemedicine visit with the practice during the measurement
period.
Exclusions: None
Method Details
1. Asking “What Matters” is defined by the primary care practice for the
patients it serves. At a minimum, asking “What Matters” involves: a)
querying the medical record for existing documentation of goals and
preferences; and b) engaging patients in discussion of “What Matters”
to them as defined by the unit.
2. Documentation standard is defined by the primary care practice for
the patients it serves; standard describes the information that is
recorded and the method of recording that information.
3. If an automated report is possible, calculate denominator and
numerator.
4. If a complete manual tally is possible, calculate denominator and
numerator.
5. If neither an automated report nor a complete tally is possible, sample
records at the end of the measurement period and calculate
numerator and denominator. You can apply a stopping rule to reduce
measurement effort.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 34
Outcome Measure: Care Concordance with “What Matters”
Hospital Setting
Measure Name
Care Concordance with “What Matters”
Measure
Description
Percent collaboRATE “Top Box” score
Site
Inpatient unit
Population
Measured
Patients 65 years or older
Measurement
Period
Weekly or monthly
Weekly measurement will support faster testing and learning cycles, but
has consequently higher measurement burden and may not be feasible.
Numerator
Count of surveys with top-box answers to all three questions (“all-or-
nothing” score)
Exclusions: None
Denominator
Count of complete surveys returned from patients
Inclusion: Patients with LOS >= 1 day present on the unit between 12:01
AM on the first day of the measurement period and 11:59 PM on the last
day of the measurement period. For patients who are unable to respond to
the questions due to cognitive impairment, use the proxy version of
collaboRATE.
Exclusions: None
Method Details
1. Collect a minimum of 25 completed surveys to compute a top-box
percent (see http://www.glynelwyn.com/scoring-collaboRATE.html).
2. Recognize that if respondent confidentiality cannot be ensured, scores
may be biased upward.
3. To support informed analysis and interpretation, units should track
total number of patients approached to obtain the completed number
of surveys.
4. Paper/manual data tools will work for initial testing but may not scale
to additional units. Organizations will need to develop information
technology to allow patients to respond to the questions and to
summarize the measurement with low effort.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 35
Primary Care Setting
Measure Name
Care Concordance with “What Matters”
Measure
Description
Per cent collaboRATE “Top Box” score
Site
Primary care practice
Population
Measured
Patients 65 years or older
Measurement
Period
Weekly or monthly
Weekly measurement will support faster testing and learning cycles, but
has consequently higher measurement burden and may not be feasible.
Numerator
Count of surveys with top-box answers to all three questions (“all-or-
nothing” score)
Exclusions: None
Denominator
Number of surveys completed
Inclusions: Patients in the population seen for any reason by the primary
care practice during the measurement period
Exclusions: None
Method Details
1. Collect a minimum of 25 completed surveys to compute a top-box
percent (see http://www.glynelwyn.com/scoring-collaboRATE.html)
2. Recognize that if respondent confidentiality cannot be ensured, scores
may be biased upward.
3. To support informed analysis and interpretation, practices should track
total number of patients approached to obtain the completed number
of surveys.
4. Paper/manual data tools will work for initial testing but may not scale
to additional practices. Organizations will need to develop information
technology to allow patients to respond to the questions and to
summarize the measurement with low effort.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 36
Appendix D: A Multicultural Tool for Getting
to Know You and What Matters to You
This tool was developed by the Stanford Inreach for Successful Aging (iSAGE) for Diverse
Older Adults.
1. What matters most to you? (Examples: Being at home, gardening, going to church,
playing with my grandchildren)
2. Who are the people in your life you hold dear or care about? (Examples: My
friend Tom, my niece Maria)
Name
Relationship
When did you last see
this person
3. Name three treasured moments in your life? (Examples: Meeting the love of my
life, birth of my daughter, my graduation, getting my first car)
4. Name three life experiences you would like to have or tasks you would like to
complete in the next six months? (Examples: Travel to Europe, fishing trip, family
reunion, 50th wedding anniversary)
5. Name three activities you enjoy doing regularly? (Examples: Walking, reading,
cooking, hiking, dancing)
Activity
When was the last
time you did this
activity
What assistance do you need
to do this? (if no assistance
needed, say none)
1.
2.
3.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 37
6a. Describe what a good day looks like for you? (Example: I wake up at 7 and do
not have any pain. I have a hot breakfast with my family. Then go for a walk and meet
my friends. In the evening, I would watch football while eating chocolate ice cream.)
In the morning:
_____________________________________________________________________
In the afternoon:
_____________________________________________________________________
In the evening:
_____________________________________________________________________
Before bed:
_____________________________________________________________________
When was the last time you had a good day like this?
_____________________________________________________________________
7. In what languages are the TV programs you usually watch? (Examples: English
Spanish, Cantonese)
8. How confident are you with filling out medical forms by yourself?
1
2
3
4
5
Not confident
Very confident
Do you need help? Yes No
9. Who/what provides you with strength and hope? (Examples: Going to
church, meditation)
10. Do you have a community that supports you? Who are they and how
do they help?

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 38
References
1
Institute for Healthcare Improvement. “What Matters.”
www.ihi.org/Topics/WhatMatters/Pages/default.aspx
2
The Conversation Project. https://theconversationproject.org/
3
Sokol-Hessner L, Zambeaux A, Little K, Macy L, Lally K, McCutcheon Adams K. “Conversation
Ready”: A Framework for Improving End-of-Life Care (Second Edition). IHI White Paper.
Boston, Massachusetts: Institute for Healthcare Improvement; 2019.
www.ihi.org/resources/Pages/IHIWhitePapers/ConversationReadyEndofLifeCare.aspx
4
Fazio S, Pace D, Flinner J, Kallmyer B. The fundamentals of person-centered care for individuals
with dementia. The Gerontologist. 2018;58(suppl 1 );S10-S19.
5
Harvard University. Project Implicit. https://implicit.harvard.edu/implicit/
6
National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and
Health Care. US Department of Health and Human Services.
www.thinkculturalhealth.hhs.gov/clas
7
The Ethnogeriatrics Steering Committee of the American Geriatrics Society. Doorway Thoughts:
Cross-Cultural Health Care for Older Adults (volumes 1, 2, and 3). Sudbury, Massachusetts: Jones
& Bartlett Learning; 2008.
8
Naik AD, Dindo L, Van Liew J, et al. Development of a clinically-feasible process for identifying
patient health priorities. Journal of the American Geriatrics Society. [In press]
9
Serious Illness Conversation Guide. Boston, Massachusetts: Ariadne Labs; revised April 2017.
www.ariadnelabs.org/areas-of-work/serious-illness-care/resources/#Downloads& Tools
10
Fick DM, Inouye SK, Guess J, et al. Preliminary development of an ultrabrief two-item bedside
test for delirium. Journal of Hospital Medicine. 2015;10(10):645-650.
11
Howe E. Initial screening of patients for Alzheimer’s disease and minimal cognitive impairment.
Psychiatry (Edgmont). 2007;4(7):24-27.
12
Borson S, Scanlan J, Brush M, Vitallano P, Dokmak A. The Mini-Cog: A cognitive ‘vital signs’
measure for dementia screening in multi-lingual elderly. International Journal of Geriatric
Psychiatry. 2000;15(11):1021-1027.
13
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. V alidation of a short
orientation-memory concentration test of cognitive impairment. American Journal of Psychiatry.
1983;140:734-739.
14
Better Care Playbook. “Play: Manage Quality with Daily Huddles.”
www.bettercareplaybook.org/plays/play-manage-quality-daily-huddles
15
Epic. “Software: Patient Engagement.” www.epic.com/software#PatientEngagement
16
Fried TR. Shared decision making — finding the sweet spot. New England Journal of Medicine.
2016;374(2):104-106.

TOOLKIT: “What Matters” to Ol der Adults? A Tool kit for Health Systems to Design Better Care with Older Adults
Institute for Healthcare Improvement
•
ihi.org 39
17
Elwy n G. “collaboRATE™ 5-Point Anchor Scale.”
http://www.glynelwyn.com/uploads/2/4/0/4/24040341/collaborate_for_patients_5_anchor_po
int_scale.pdf
18
Barr P, Forcino R, Thompson R, et al. Evaluating collaboRATE in a clinical setting: analysis of
mode effects on scores, response rates and costs of data collection. BMJ Open. 2017;7:e014681.
19
Person-Centred Health and Care: Real-time and Right-time Care Experience Improvement
Models Evaluation Report. Healthcare Improvement Scotland. May 2018.
https://ihub.scot/person-centred-health-and-care-build/real-time-and-right-time-evaluation-
report/
