
Stte of Helth n the EU
The Netherlnds
Countr Helth Profle 2021

2
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
The Countr Helth Profle seres
The Stte of Helth n the EU’s Countr Helth Profles
provde concse nd polc-relevnt overvew of
helth nd helth sstems n the EU/Europen Economc
Are The emphsse the prtculr chrcterstcs nd
chllenes n ech countr nst bcdrop of cross-
countr comprsons The m s to support polcmers
nd nfluencers wth mens for mutul lernn nd
voluntr exchne
The profles re the ont wor of the OECD nd the
Europen Observtor on Helth Sstems nd Polces,
n cooperton wth the Europen Commsson The tem
s rteful for the vluble comments nd suestons
provded b the Helth Sstems nd Polc Montor
networ, the OECD Helth Commttee nd the EU Expert
Group on Helth Sstems Performnce Assessment (HSPA)
Contents
1 3
2 4
3 7
4 8
5 11
51 Effectveness 11
52 Accessblt 14
53 Reslence 17
6 22
Dt nd nformton sources
The dt nd nformton n the Countr Helth Profles
re bsed mnl on ntonl offcl sttstcs provded
to Eurostt nd the OECD, whch were vldted to
ensure the hhest stndrds of dt comprblt
The sources nd methods underln these dt re
vlble n the Eurostt dtbse nd the OECD helth
dtbse Some ddtonl dt lso come from the
Insttute for Helth Metrcs nd Evluton (IHME), the
Europen Centre for Dsese Preventon nd Control
(ECDC), the Helth Behvour n School-Aed Chldren
(HBSC) surves nd the World Helth Ornzton
(WHO), s well s other ntonl sources
The clculted EU veres re wehted veres of
the 27 Member Sttes unless otherwse noted These EU
veres do not nclude Icelnd nd Norw
Ths profle ws completed n September 2021, bsed on
dt vlble t the end of Auust 2021
Demographic factors The Netherlands EU
Populton sze (md-er estmtes) 17 407 585 447 319 916
Shre of populton over e 65 (%) 195 206
Fertlt rte (2019) 16 15
Socioeconomic factors
GDP per cpt (EUR PPP) 39 641 29 801
Reltve povert rte (%, 2019) 132 165
Unemploment rte (%) 38 71
1 Numbr of chldrn born pr womn gd 15-49 2 Purchsng powr prt (PPP) s dfnd s th rt of currnc convrson tht qulss th
purchsng powr of dffrnt currncs b lmntng th dffrncs n prc lvls btwn countrs 3 Prcntg of prsons lvng wth lss thn 60 %
of mdn quvlsd dsposbl ncom Sourc Eurostt dtbs
Dsclmer The opnons expressed nd ruments emploed heren re solel those of the uthors nd do not necessrl reflect the offcl vews of
the OECD or of ts member countres, or of the Europen Observtor on Helth Sstems nd Polces or n of ts Prtners The vews expressed heren
cn n no w be ten to reflect the offcl opnon of the Europen Unon
Ths document, s well s n dt nd mp ncluded heren, re wthout preudce to the sttus of or soverent over n terrtor, to the delmtton
of nterntonl fronters nd boundres nd to the nme of n terrtor, ct or re
Addtonl dsclmers for WHO ppl
© OECD nd World Helth Ornzton (ctn s the host ornston for, nd secretrt of, the Europen Observtor on Helth Sstems nd
Polces) 2021
Demographic and socioeconomic context in The Netherlands, 2020

3
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
1 Hhlhts
Three coverage schemes provide broad health coverage to nearly all the Dutch population. These include a
competitive social health insurance system for curative care, a single-payer system for long-term care and
municipal systems for social care. Like the rest of Europe, the Netherlands faced high pressures from the
COVID-19 pandemic, and experienced a temporary drop in life expectancy in 2020. The unprecedented strain
caused by COVID-19 posed a clear challenge at all levels of the Dutch health system.
Health Status
Life expectancy in the Netherlands is higher than the EU average by about
one year, but gains have slowed over the past decade. As a result of the
COVID-19 pandemic, life expectancy fell by 0.7 years between 2019 and
2020 – the same as the EU average. Lung cancer, stroke and ischaemic
heart disease made up the highest share of mortality in 2019. In 2020, 1 in
15 deaths were attributed to COVID-19.
Risk factors
Behavioural risk factors in the Netherlands account for a lower share of
deaths than the EU average. Smoking and obesity rates are both below the
EU averages. However, one in five deaths in 2019 resulted from tobacco
consumption – a higher share than in the EU – and obesity levels among
adults have increased over the last two decades. Dutch adults and
adolescents are more physically active than those in most other EU countries.
Health system
The Netherlands spends more per capita (EUR3967) on health than the EU
average (EUR3523), with a considerable share dedicated to long-term care.
Expenditure on outpatient pharmaceuticals and medical devices is kept
low, aided by volume and price control policies and well-established health
technology assessment processes. Public sources cover a high percentage of
health expenditure, resulting in a lower share of out-of-pocket spending for
health care than the EU average.
Effectiveness
The Netherlands has among
the lowest mortality rates from
preventable and treatable causes
in the EU. Most preventable
deaths are from lung cancer,
while colorectal cancer and breast
cancer account for 40% of deaths
from treatable causes. Mortality
rates from ischaemic heart
disease, stroke and pneumonia
are among the lowest in the EU.
Accessibility
The Dutch population has
historically reported low unmet
needs for medical treatment, but
this changed during the COVID-19
pandemic when many non-urgent
services were cancelled or
postponed. Evidence suggests that
15% of people had to forgo care
during the first 12 months of the
pandemic. Teleconsultations were
used to help maintain access to
services.
Resilience
The health system response to
COVID-19 encountered obstacles,
including fragmentation in
testing, contact tracing and
vaccination efforts. After a slow
start, the vaccination campaign
accelerated, and 63% of the
population had received two
doses (or equivalent) by the end of
August 2021.
NL EU
Option 1: Life expectancy - trendline Select a country:
Option 2: Gains and losses in life expectancy
Netherlands
81
2010 2015 2019 2020
Lf xpctnc gns, rs
NL EU Lowest Hhest
Obesity
Physical
Inactivity
Smoking
0 10 20 30
70 80 90 100
0 20 40
Physical Inactivity
% of 15-yea r-olds
Obesity
% of adults
Smoking
% of adults
1
Pr cpt spndng (EUR PPP)
NL EU
Netherlands EU
€ 4 500
€
3 000
€ 1 500
€ 0
Ag-stndrdsd mortlt rt
pr 100 000 populton, 2018
Preventble
mortlt
Tretble
mortlt
Effect veness - Prevent ble nd tre t ble mort l t
AT 157 75
BE 146 71
BG 226 188
HR 239 133
CY 104 79
For tr nsl tors O
CZ 195 124
152 73
EE 253 133
FI 159 71
FR 134
63
DE 156 85
GR Greece 139 90
HU 326 176
IS 115 64
IE 132 76
IT 104 65
LV 326 196
LT 293 186
LU 130 68
MT 111 92
NL 129 65
NO 120 59
PL 222 133
PT 138 83
92
160
65
129
Netherlands EU
-
NL
EU
Shr of totl populton vccntd gnst
COVID-19 up to th nd of August 2021
SShhaarree ooff ttoottaall ppooppuullaattiioonn vvaacccciinnaatteedd aaggaaiinnsstt CCOOVVIIDD--1199
Note: Up to end of August 2021
Source: Our World in Data.
Note for authors: EU average is unweighted (the number of countries included in the average varies depending on the week). Data extracted on 06/09/2021.
54%
63%
62%
70%
0%10%20%30%40%50%60%70%80%90%100%
EU
Netherlands
Two doses (or equivalent) One dose
NL
EU
0% 50% 100%
Two doses (or equvlent) One dose
Accessibility - Unmet needs and use of teleconsultations during COVID-19
Option 1:
Netherlands
Option 2:
39%
42%
% using
teleconsultation
during first 12 months
of pandemic
21%
15%
Netherlands EU
% reporting forgone
medical care during
first 12 months of
pandemic
15
21
0
10
20
30
42
39
0
20
40
60
% reporting forgone medical
care during first 12 months
of pandemic
% using teleconsultation
during first 12 months of
pandemic
39%
42%
% using
teleconsultation
during first 12 months
of pandemic
21%
15%
Netherlands EU
% reporting forgone
medical care during
first 12 months of
pandemic
% reporting forgone
medical care during first
12 months of pandemic
% using teleconsultation
during first 12 months of
pandemic
% reporting forgone medical
care during first 12 months
of pandemic
% using teleconsultation
during first 12 months of
pandemic
NL EU27

4
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
2 Helth n the Netherlnds
Life expectancy temporarily dropped by
0.7 years in 2020 during the COVID-19
pandemic
In 2020, life expectancy at birth for the Dutch
population was 81.5 years, almost one year higher
than the average in the EU as a whole (80.6 years),
but lower than many of the top performing countries
(Figure 1). Men in the Netherlands live almost two
years longer than the EU average, while Dutch women
live almost five months less. This comparatively weak
performance for women reflects the legacy of high
smoking rates in previous generations (see Section 3)
and which has increased the number of women with
lung cancer.
Progress in life expectancy in the previous two
decades was significant, but between 2010 and 2019,
women only gained 0.7 years in life expectancy, while
men gained 1.7 years, a slowdown that is not unique
to the Netherlands. Owing to the COVID-19 pandemic,
overall life expectancy fell temporarily from 82.2 years
in 2019 to 81.5 years in 2020, representing a decline of
nearly 8.5 months.
Figure 1. Dutch life expectancy is 1.3 years below the best performing EU country but higher than the EU
average
Not Th EU vrg s wghtd Dt for Irlnd rfr to 2019
Sourc Eurostt Dtbs
COVID-19 accounted for a large number of
deaths in the Netherlands in 2020
In 2019, the leading causes of death in the
Netherlands were lung cancer, stroke and ischaemic
heart disease (Figure 2). Mortality rates from lung
cancer and chronic obstructive pulmonary disease
(COPD) continue to be among the highest in the EU,
despite some reductions over the years. In contrast,
mortality rates from stroke and ischaemic heart
disease remain among the lowest in the EU (see
Section 5.1).
In 2020, COVID-19 accounted for about 11600 deaths
in the Netherlands – almost 7% of all deaths –
while an additional 6400 deaths were attributed to
COVID-19 by the end of August 2021. The majority of
deaths were among people aged 60 and over. Overall,
the mortality rate from COVID-19 up to the end of
August 2021 was about 35% lower in the Netherlands
than the average across EU countries (approximately
1035 per million population compared with about
1590 for the EU average). However, the broader
indicator of excess mortality suggests that the direct
and indirect death toll related to COVID-19 in 2020
may have been higher (Box 1).
LLiiffee eexxppeeccttaannccyy aatt bbiirrtthh,, 22000000,, 22001100 aanndd 22002200
Select a country:
GEO/TIME 2000 2010 2020
22000000 22001100 22002200
Norway 78.8 81.2 83.3 0 #N/A #N/A #N/A
Iceland 79.7 81.9 83.1 0 #N/A #N/A #N/A
Ireland 76.6 80.8 82.8 0 #N/A #N/A #N/A
Malta 78.5 81.5 82.6 0 #N/A #N/A #N/A
Italy 79.9 82.2 82.4 0 #N/A #N/A #N/A
Spain 79.3 82.4 82.4 0 #N/A #N/A #N/A
Sweden 79.8 81.6 82.4 0 #N/A #N/A #N/A
Cyprus 77.7 81.5 82.3 0 #N/A #N/A #N/A
France 79.2 81.8 82.3 0 #N/A #N/A #N/A
Finland 77.8 80.2 82.2 0 #N/A #N/A #N/A
Netherlands
83.3
83.1
82.8
82.6
82.4
82.4
82.4
82.3
82.3
82.2
81.8
81.6
81.5
81.3
81.2
81.1
81.1
80.9
80.6
80.6
78.6
78.3
77.8
76.9
76.6
75.7
75.7
75.1
74.2
73.6
65
70
75
80
85
90
2000 2010
Years
2020
Netherlands
EU
81.0
81.6
82.2
81.5
2010 2015 2019 2020
Years
Life expectancy at birth

5
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 2. Lung cancer, stroke and ischaemic heart disease are the leading causes of death in the Netherlands
Not Th numbr nd shr of COVID-19 dths rfr to 2020, whl th numbr nd shr of othr cuss rfr to 2019 Th sz of th COVID-19 box s
proportonl to th sz of th othr mn cuss of dth n 2019
Sourcs Eurostt (for cuss of dth n 2019) ECDC (for COVID-19 dths n 2020, up to w 53)
Box 1. Some gaps between COVID-19 deaths and excess mortality in 2020 are evident in the Netherlands
In the Netherlnds, s n mn other countres, the
ctul number of deths from COVID-19 s lel
to be hher thn the number of reported deths,
especll becuse there s no oblton to report
COVID-19 s cuse of deth untl t ppers on
deth certfctes, whch re onl vlble severl
months lter The number of COVID-19 deths
reported lso does not te nto ccount the possble
ncrese n deths from other cuses tht m rse
durn or fter the pndemc These m be due,
for exmple, to reduced ccess to helth servces
for non-COVID-19 ptents or fewer people seen
tretment becuse of fer of ctchn the vrus
(ndrect deths) The ndctor of excess mortlt
(defned s the number of deths from ll cuses
over nd bove wht would hve been normll
expected, bsed on bselne dt from the prevous
fve ers) cn provde broder mesure of the
drect nd ndrect mpct of COVID-19 on mortlt
tht s not ffected b ssues relted to testn nd
cuse-of-deth restrton prctces
In the Netherlnds, between Mrch nd December
2020, trends for excess deths nd reported COVID-19
deths were enerll consstent, but wth some
ncreses n the p between the two n Aprl nd
from md-October 2020 (Fure 3) A hetwve n
Auust 2020 ws probbl the cuse of reltvel
steep rse n excess deths t tht tme, nd ws not
connected wth COVID-19 Overll, excess mortlt
ccounted for bout 20 000 deths between Mrch
nd December 2020
Figure 3. COVID-19 and excess deaths peaked in spring 2020 in the Netherlands
Not Th clculton of xcss dths s bsd on th vrg for th prvous fv rs (2015-2019)
Sourcs ECDC (for COVID-19 dths) OECD bsd on Eurostt dt (for xcss dths)
- 500
0
500
1 000
1 500
2 000
2 500
COVID-19 deaths Excess deaths
Weekly number of deaths
COVID-19
11 598 (68%)
Lun cncer
10 262 (68%)
Stroe
9368 (62%)
Ischemc hert dsese
8 370 (55%)
Colorectl cncer
4 857 (32%)
Pneumon
3 374 (22%)
Brest
cncer
3 089 (20%)
Pncretc
cncer
3 024 (20%)
Alzhemer’s
dsese
4 116 (27%)
Chronc obstructve pulmonr
dsese
6984 (46%)

6
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Most Dutch people report good health, but
sizeable disparities exist across income groups
In 2019, about 75% of Dutch people reported that
they were in good health – a greater share than in the
EU as a whole (69%). However, as in other countries,
people on lower incomes are less likely to report
good health; only 60% of those in the lowest income
quintile reported good health compared to 87% of
those in the highest (Figure 4).
The burden of cancer in the Netherlands is
considerable
According to estimates from the Joint Research
Centre based on incidence trends from previous years,
around 110000 new cases of cancer were expected in
the Netherlands in 2020. However, fewer people were
newly diagnosed with cancer than in previous years,
probably as a result of the pause in cancer screening
programmes in spring 2020 during the pandemic.
Prostate cancer is the main cancer among men, while
breast cancer is the leading cancer among women.
Colorectal and lung cancers are the second and third
leading cause of cancer among both sexes (Figure 5).
Despite having a substantial disease burden, with over
45000 deaths from cancer in 2019, cancer survival
rates in the Netherlands are higher than the EU
average (see Section 5.1).
Figure 4. Inequalities in self-reported health by
income level are relatively large in the Netherlands
Not 1 Th shrs for th totl populton nd th populton on low
ncoms r roughl th sm
Sourc Eurostt Dtbs, bsd on EU-SILC (dt rfr to 2019)
Figure 5. An estimated 110000 people in the Netherlands were expected to be diagnosed with cancer in 2020
Not Non-mlnom sn cncr s xcludd Utrus cncr dos not nclud cncr of th crvx
Sourc ECIS – Europn Cncr Informton Sstm
Others
Kidney
Non-Hodgkin
lymphoma
Skin melanoma
Bladder Lung
Colorectal
Prostate
After new data, select all and change font to 7 pt.
Adjust right and left alignment on callouts.
Enter data in BOTH layers.
Others
Non-Hodgkin
lymphoma
Bladder
Uterus
Skin melanoma
Lung
Colorectal
Breast
26%
3%
4%
7%
9% 11%
16%
24%
26%
3%
3%
4%
8%
12%
14%
30%
Men
61 755 new cases
Age-standardised rate (all cancer)
NL 759 per 100 000 populton
EU 686 per 100 000 populton
Age-standardised rate (all cancer)
NL 577 per 100 000 populton
EU 484 per 100 000 populton
Women
52 846 new cases
FFoorr ttrraannssllaattoorrss OONNLLYY::
0 20 40 60 80 100
Ireland
Greece
Cyprus
Iceland
Sweden
Spain
Netherlands
Norway
Belgium
Malta
Italy
Luxembourg
Austria
Romania
Denmark
EU
Finland
Bulgaria
France
Slovenia
Germany
Slovakia
Czechia
Croatia
Poland
Hungary
Estonia
Portugal
Latvia
Lithuania
High incomeTotal populationLow income
% of adults who report being in good health
Hh ncome Totl populton Low ncome
1
1
% of dults who report ben n ood helth

7
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
3 Rs fctors
Behavioural risk factors account for more than
one third of all deaths
More than one third (35%) of all deaths in the
Netherlands can be attributed to behavioural
risk factors – below the EU average of 39%. These
behaviours include smoking, dietary risks, alcohol
consumption and low physical activity (Figure 6). One
in five deaths in 2019 could be attributed to tobacco
consumption (including direct and second-hand
smoking), which is higher than the EU average (21%
compared to 17%). The second major risk factor is
dietary risks (including low fruit and vegetable intake,
and high sugar and salt consumption), which were
responsible for an estimated 11% of deaths in 2019 –
well below the EU average (17%). About 5% of deaths
that year were associated with alcohol consumption,
which is close to the EU average (6%). Environmental
factors such as air pollution, in the form of fine
particulate matter (PM
2.5
) and ozone exposure alone
accounted for nearly 5000 deaths in the Netherlands
in 2019 (or 3% of all deaths, compared to 4% in the
EU).
Figure 6. Tobacco consumption is the leading behavioural risk factor contributing to mortality in the Netherlands
Not Th ovrll numbr of dths rltd to ths rs fctors s lowr thn th sum of ch on tn ndvdull, bcus th sm dth cn b
ttrbutd to mor thn on rs fctor Dtr rss nclud 14 componnts such s low frut nd vgtbl nt, nd hgh sugr-swtnd bvrg
consumpton Ar polluton rfrs to xposur to PM
25
nd ozon
Sourcs IHME (2020), Globl Hlth Dt Exchng (stmts rfr to 2019)
Smoking and drinking rates in both adults and
adolescents have decreased
Adult smoking rates have declined following the
introduction of smoke-free working environments and
other policy changes (see Section 5.1), and are below
the EU average. In 2018, about one in eight 15-year-
olds in the Netherlands reported smoking cigarettes
in the past month – a substantial decline from 2014,
when it was one in five.
Overall consumption of alcohol among adults has
declined by about 20% since 2000, and is now
lower than in most other EU countries. Repeated
drunkenness among 15-year-olds is also slightly less
widespread in the Netherlands than across the EU,
with 19% of 15-year-olds reporting having been drunk
more than once in their life in 2018, compared with a
22% EU average.
Overweight and obesity rates are rising
The overweight and obesity rate among Dutch
teenagers and adults is lower than in most EU
countries (Figure 7). More than one in eight adults
(14%) in the country were obese in 2019, up from 10%
in 2002. These trends are a cause for concern, given
that obesity carries a significant risk for diabetes,
cardiovascular diseases and several different cancers.
This highlights the need to increase efforts to change
dietary habits among both children and adults.
Adults in the Netherlands have among the lowest
fruit and vegetable consumption in the EU, with
around 6 out of 10 reporting that they do not eat
at least one portion per day. A higher proportion
of adolescents report eating at least one vegetable
each day compared with the EU average, but it is
the opposite for fruit consumption: only about one
quarter (27%) of 15-year-olds reported eating at least
one fruit per day in 2018 – a lower proportion than the
EU average (31%).
Dietary risks
NL: 11%
EU: 17%
Tobacco
NL: 21%
EU: 17%
Alcohol
NL: 5%
EU: 6%
Air pollution
NL: 3%
EU: 4%
Low physical activity –
NL: 1% EU: 2%
8
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Fewer than one in five teenagers engage in
moderate physical activity every day
While most adults in the Netherlands report at least
150 minutes of moderate physical activity per week,
this is not the case among 15-year-olds. Only 18%
of Dutch teenagers reported engaging in moderate
physical activity on a daily basis in 2018, with a lower
rate among girls: only 14% of girls reported doing at
least moderate activity each day, compared to 21%
of boys. While this exceeds the EU averages of 10%
of girls and 18% of boys, low physical activity can
affect other health outcomes and increases the risk of
overweight and obesity.
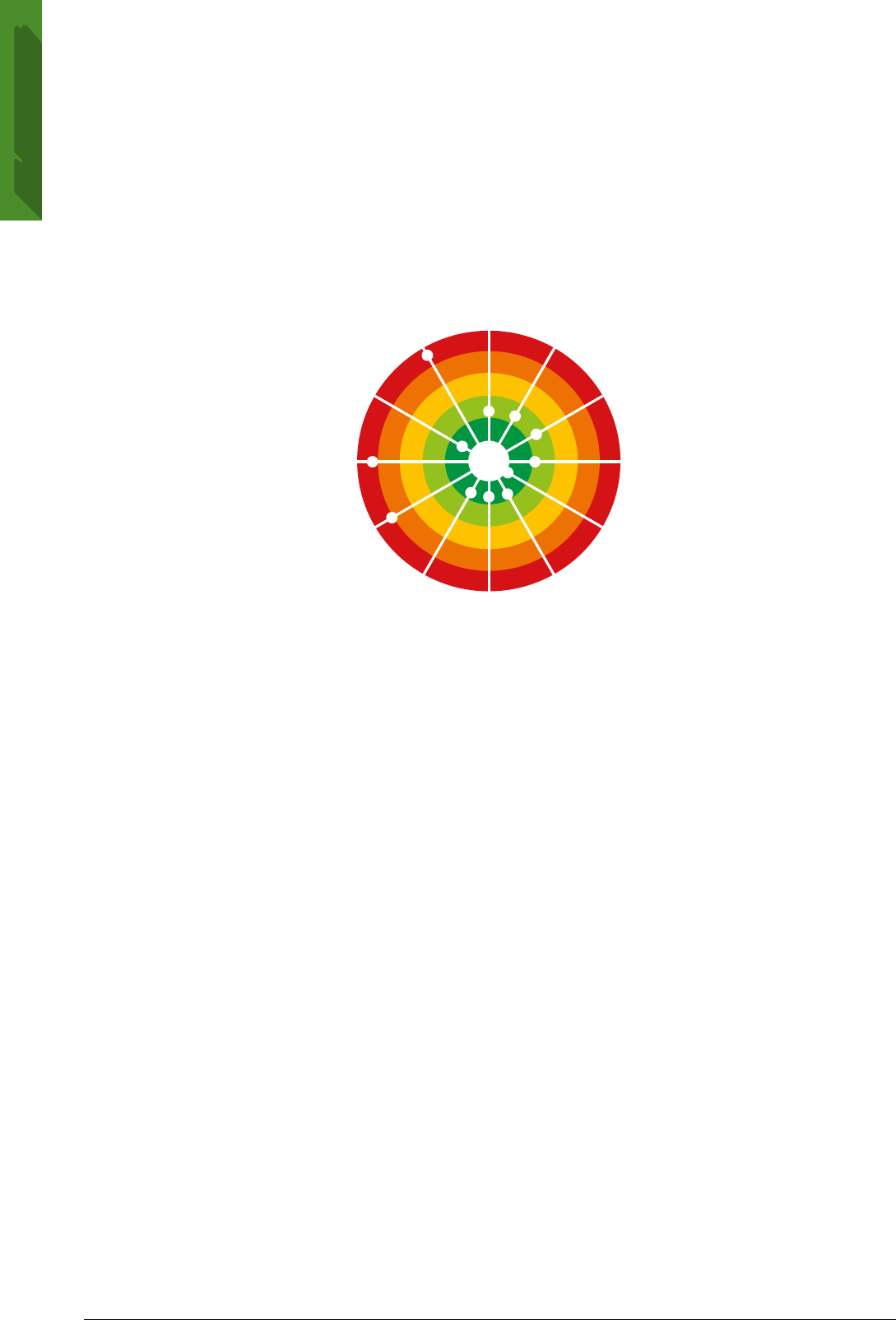
Figure 7. The Netherlands performs better than most other EU countries on many risk factors
Not Th closr th dot s to th cntr, th bttr th countr prforms comprd to othr EU countrs No countr s n th wht “trgt r” s thr s
room for progrss n ll countrs n ll rs
Sourcs OECD clcultons bsd on HBSC surv 2017-18 for dolscnts ndctors nd EHIS 2019 nd Dutch HIS for dults ndctors
4 The helth sstem
Three separate coverage schemes form the
basis of the Dutch health system
The Dutch government regulates and oversees three
schemes that together provide broad universal
health coverage. First, competing health insurers
administer a social health insurance (SHI) system
for curative care. The system, introduced in 2006,
mandates all residents to purchase insurance policies
that cover a defined benefits package set by the
government. Insurers must accept all applicants,
and they negotiate and contract with providers
based on quality and price. The SHI scheme covers
all specialist care, primary care, pharmaceuticals
and medical devices, adult mental health care, some
allied care services and community nursing. The
second scheme is a single-payer social insurance
system for long-term care, which is carried out by
the regionally dominant health insurer, and which
was the subject of a large reform in 2015 to rein in
the scope of the scheme and spending. The third is
a tax-funded social care scheme implemented by
the municipalities. The National Institute for Public
Health and the Environment (RIVM) provides guidance
for public health services at the national level, while
municipalities cover most services such as screening,
vaccination and health promotion (Box 2).
Spending on health as a share of GDP is slightly
above the EU average
In 2019, the Netherlands spent 10.2% of GDP in
health – slightly above the EU average of 9.9%.
This translates to EUR3967 per capita (adjusted
for differences in purchasing power), which is well
above the EU average of EUR3523. Expenditure
growth between 2013 and 2017 only increased by
1.0% on average per year, following the introduction
of a reform package that increased financial risk
6
Vegetable consumption (adults)
Vegetable consumption (adolescents)
Fruit consumption (adults)
Fruit consumption (adolescents)
Physical activity (adults)
Physical activity (adolescents)
Obesity (adults)
Overweight and obesity (adolescents)
Alcohol consumption (adults)
Drunkenness (adolescents)
Smoking (adults)
Smoking (adolescents)
Select dots + Effect > Transform scale 130%
OR Select dots + 3 pt white outline (rounded corners)

9
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
for insurers and providers and increased the
share of out-of-pocket (OOP) health expenditure.
In addition, the Dutch Ministry of Health signed
several agreements with stakeholders that aim
to keep spending growth within predefined levels.
However, between 2017 and 2019, annual health
expenditure growth rose to 2.3% per year. During the
COVID-19 pandemic, insurers and providers agreed
on measures to compensate revenue losses and extra
spending due to COVID-19. The government allocated
additional tax revenues for 2020 and 2021 to the
health sector, including for testing and contact tracing
(EUR476million in 2020 and EUR450million in 2021)
and intensive care unit (ICU) beds (EUR80.1million
and EUR93.9million).
A relatively large voluntary health insurance
sector contributes to low OOP payments
Following the abolition of the private insurance
scheme in 2006, public expenditure (government
spending and compulsory insurance) increased from
about two thirds (68.4%) of health spending in 2005 to
83.8% in 2006, before falling slightly to 82.6% in 2019.
This remains slightly above the EU average of 79.7%
(Figure 8).
OOP spending as a share of current health
expenditure was about two thirds of the EU-wide
average in 2019, at 10.6% in the Netherlands
compared to 15.4% in the EU. Around 57% of OOP
payments are due to cost-sharing, although general
practitioner (GP) care, maternal care and care from
district nurses remain free at the point of delivery. In
the Netherlands, health insurers may offer voluntary
health insurance (VHI) policies to cover services
outside the benefits package. This contributes to a
relatively large VHI sector (6.8% of health spending
compared to 4.9% in the EU in 2019), as individuals
who expect to incur high OOP payments usually take
out VHI (see Section 5.2).
Figure 8. Health spending per capita is above the EU average
Not Th EU vrg s wghtd
Sourc OECD Hlth Sttstcs 2021 (dt rfr to 2019, xcpt for Mlt 2018)
Box 2. The Netherlands took steps to implement a national-level response to the COVID-19 crisis
In ccordnce wth the ntonl pndemc response
pln n plce before the COVID-19 outbre, the
frst response focused on the reonl level n the
provnce of Noord-Brbnt, where the frst COVID-19
outbre occurred Soon, the response ws scled
up to the ntonl level under the mnement of
the RIVM (see Secton 53), whch coordntes the
reonll conducted testn, contct trcn nd
reportn of cses The RIVM lso hosts the Outbre
Mnement Tem, whch dvses the Prme
Mnster nd the Cbnet on necessr mesures, nd
conssts of medcl speclsts, vrolosts, medcl
mcrobolosts nd representtves of the ntonl
reference lbortor Throuhout the utumn of 2020,
the Netherlnds dd not pss n ntonl emerenc
leslton, nd muncpl uthortes could determne
whether to mplement emerenc decrees However,
the countr ntroduced the COVID-19 Temporr
Mesures Act on 1 December 2020, whch enbles
ntonl decson mn The Act cn be extended
nd stopped t n tme wth the reement of the
prlment
Sourc COVID-19 Hlth Sstms Rspons Montor
CCoouunnttrryy
GGoovveerrnnmmeenntt && ccoommppuullssoorryy iinnssuurraannccee sscchheemmeess VVoolluunnttaarryy iinnssuurraannccee && oouutt--ooff--ppoocckkeett ppaayymmeennttss TToottaall EExxpp.. SShhaarree ooff GGDDPP
Norway 4000 661 4661 10.5
Germany 3811 694 4505 11.7
Netherlands 3278 689 3967 10.2
Austria 2966 977 3943 10.4
Sweden 3257 580 3837 10.9
Denmark 3153 633 3786 10.0
Belgium 2898 875 3773 10.7
Luxembourg 3179 513 3742 5.4
France 3051 594 3645 11.1
EU27 22880099 771144 3521 9.9
Ireland 2620 893 3513 6.7
Finland 2454 699 3153 9.2
Iceland 2601 537 3138 8.5
Malta 1679 966 2646 8.8
Italy 1866 659 2525 8.7
Spain 1757 731 2488 9.1
Czechia 1932 430 2362 7.8
Portugal 1411 903 2314 9.5
Slovenia 1662 621 2283 8.5
Lithuania 1251 633 1885 7.0
Cyprus 1063 819 1881 7.0
2019
0.0
2.5
5.0
7.5
10.0
12.5
0
1 000
2 000
3 000
4 000
5 000
Government & compulsory insurance Voluntary insurance & out-of-pocket payments Share of GDP
% GDP
EUR PPP per capita
0.0
2.5
5.0
7.5
10.0
12.5
0
1 000
2 000
3 000
4 000
5 000
Government & compulsory insurance Voluntary insurance & out-of-pocket payments Share of GDP
% GDP
EUR PPP per capita

10
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
The Netherlands has the second highest share
of spending on long-term care in the EU
When measured in per capita terms, health spending
in the Netherlands is above the EU average for
outpatient care, long-term care and prevention,
and is below the average on inpatient care, retail
pharmaceuticals and medical devices (Figure 9). A
large long-term care sector, which covers elderly care,
care for disabled people and long-term mental care,
contributes to the relatively high overall spending
on health. Spending on retail pharmaceuticals and
medical devices is well below the EU average and
even decreased from 13.9% of total health spending
in 2010 to 11.2% in 2019. The Netherlands has among
the highest levels of spending on prevention, at
EUR131 per person, compared to an EU average of
EUR102, but this amount has not increased over time.
Between 2010 and 2019, the share of spending on
prevention dropped from 4.3% to 3.3% of total health
spending.
Figure 9. Long-term care expenditure exceeds that of most other EU countries
Not Th cost of hlth sstm dmnstrton s not ncludd 1 Includs hom cr nd ncllr srvcs (g ptnt trnsportton) 2 Includs onl th
hlth componnt 3 Includs curtv-rhblttv cr n hosptl nd othr sttngs 4 Includs onl th outptnt mrt 5 Includs onl spndng for
orgnsd prvnton progrmms Th EU vrg s wghtd
Sourcs OECD Hlth Sttstcs 2021, Eurostt Dtbs (dt rfr to 2019)
Nursing attracts more people to the profession
than in many other EU countries
In the last 10 years, the ratio of doctors to population
has increased from 3.4 to 3.7 per 1000 population,
close to the EU average of 3.9. The ratio of nurses
grew from 8.7 to 10.7 per 1000 population, which
is well above the EU average of 8.4. In 2019, 60%
more nurses graduated than in 2009, while doctors’
graduation rates rose by a more modest 26%. Nurses
in the Netherlands participate in task-shifting and
advanced nursing practices, creating a more attractive
work environment. Nurse specialists were granted
the authority to practise independently in 2012, and
this was codified in law in 2018. They are empowered
to prescribe all medicines within their competence
and to perform endoscopies, among other specified
services. However, the nursing workforce is
overburdened in hospitals, and nursing and home
care personnel also face shortages, which became
more pronounced during the COVID-19 pandemic (see
Section 5.3). An above-average share of doctors work
as GPs – 24% of all physicians compared with 21%
across the EU.
Strong primary care and gatekeeping contribute
to low hospital admission rates
Health services are overwhelmingly provided by
private non-profit providers, and most physicians
are self-employed. The Netherlands operates a strict
gatekeeper system. Patients require a referral from a
GP to visit hospital and specialist care, including for
COVID-19 (see Section 5.3). Although the Netherlands
reports comparatively high numbers of outpatient
contacts, it also has relatively low rates of hospital
discharges, suggesting that strong primary care and
outpatient specialist treatment manage to keep
people out of hospitals (Figure 10). Both long-term
care and mental health care reforms were designed
for delivery in outpatient settings to respond to
historically high institutionalisation rates (Kroneman
et al., 2016).
1 022
617
1 010
630
102
0
0
0
0
0
1 128
1 112
961
445
131
Netherlnds
Preventon Phrmceutcls
nd medcl devces
Inptent cre Lon-term cre Outptent cre
0
200
400
600
800
1 000
1 200
1 400
EU27EUR PPP per cpt
29%
of totl
spendn
28%
of totl
spendn
24%
of totl
spendn
11%
of totl
spendn
3%
of totl
spendn

11
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 10. The Netherlands has the lowest inpatient use in the EU
Not Th EU vrg s unwghtd
Sourc OECD Hlth Sttstcs nd Eurostt Dtbs (dt rfr to 2019 or nrst r)
5 Performnce of the helth sstem
51 Effectiveness
Low mortality from preventable and treatable
causes point to effective health interventions
Mortality from preventable causes in the Netherlands
compares favourably with the rate across the EU as
a whole, at 129 deaths compared to 160 per 100000
population (Figure 11), reflecting both a lower
prevalence of risk factors and a lower incidence
of many of these health issues compared to most
other EU countries. Lung cancer accounts for 30% of
preventable deaths in the Netherlands, making it the
largest contributor to preventable mortality. Since the
early 2000s, the government has implemented several
public health policies aiming to minimise the impact
of behavioural risk factors and social determinants of
health. Smoking was banned in workplaces in 2004,
and in cafés and restaurants in 2008, while alcohol
control measures implemented in 2013 focused on
reducing alcohol use among teenagers. The National
Prevention Agreement concluded in 2018 prompts
municipalities to implement regional and local
agreements to improve health outcomes and reduce
health inequalities in their populations. So far,
14 initiatives with an average of 41 participating
organisations have been developed, working
towards the 2040 targets to have a smoke-free
generation, reduce the share of the overweight and
obese population from 50% to 38% and decrease
problematic alcohol abuse.
The Netherlands reports one of the lowest mortality
rates from treatable causes – that is, deaths that
could have been avoided through effective health
care interventions (Figure 11). These rates remain low
compared to the rest of the EU in spite of the above-
average mortality from colorectal and breast cancer
in the Netherlands, which accounted for more than
40% of treatable deaths in 2018. Mortality rates from
other treatable causes – such as ischaemic heart
disease, stroke and pneumonia – were among the
lowest in the EU.
50 200 250 350300150100
0
2
4
6
8
10
12
Number of doctor consultations per individual
Discharges per 1 000 population
EU average: 6.7
EU average: 172
High inpatient use
Low outpatient use
High inpatient use
High outpatient use
Low inpatient use
Low outpatient use
Low inpatient use
High outpatient use
NO
DK
CZ
MT
LT
LU
IE
FR
SI
RO
PL
SK
IT
ES
CY
BG
SE
DE
EL
IS
AT
PT
FI
BE
HR
EU
NL
EE
HU
LV

12
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 11. Deaths from preventable and treatable causes are lower than in most EU countries
Not Prvntbl mortlt s dfnd s dth tht cn b mnl vodd through publc hlth nd prmr prvnton ntrvntons Trtbl mortlt
s dfnd s dth tht cn b mnl vodd through hlth cr ntrvntons, ncludng scrnng nd trtmnt Hlf of ll dths for som dsss
(g schmc hrt dss nd crbrovsculr dss) r ttrbutd to prvntbl mortlt th othr hlf r ttrbutd to trtbl cuss Both
ndctors rfr to prmtur mortlt (undr g 75) Th dt r bsd on th rvsd OECD/Eurostt lsts
Sourc Eurostt Dtbs (dt rfr to 2018, xcpt for Frnc 2016)
The Netherlands faces increasing numbers of
avoidable admissions for chronic conditions
While the Netherlands reports an overall low number
of avoidable hospitalisations, avoidable admissions
for asthma and COPD have increased between 2007
and 2019 from 182 to 208 avoidable admissions per
100000 population. The Netherlands has responded
to this with information campaigns and several
policy actions over the past decade. Initial results
bode well for the effect of these policies, as avoidable
admissions for COPD dropped from 213 to 200
avoidable hospitalisations per 100000 population
between 2015 and 2016. Additional measures
implemented in 2020 introduced neutral packaging
for cigarettes, a ban on flavoured e-cigarettes, a
prohibition of smoking in schoolyards, a ban on
displays of tobacco products in supermarkets and
raised excise duties on tobacco products. In addition,
strong primary care and outpatient care contribute
to minimising hospital admission rates for diabetes
and congestive heart failure, which are about half
the EU average. Bundled payments, whereby a single
payment covers all costs of services supplied by
multiple providers for a defined episode of care, also
play a role in coordinating care for diabetes, COPD
and cardiovascular disease patients.
Although above the EU average, influenza
vaccination rates were on a downward trend
before the pandemic
In 2019, the Netherlands vaccinated 61% of its
population over the age of 65 for seasonal influenza
– well above the EU average of 42%, although still
below the target of 75% recommended by the
104
104
111
113
115
118
120
129
130
132
134
138
139
146
152
156
157
159
160
175
195
222
226
239
241
253
293
306
326
326
59
63
64
65
65
65
66
68
71
71
73
75
76
77
79
83
85
90
92
92
124
133
133
133
165
176
186
188
196
210
0 50 100 150 200 250 300 350
0 50 100 150 200 250
104
104
111
113
115
118
120
129
130
132
134
138
139
146
152
156
157
159
160
175
195
222
226
239
241
253
293
306
326
326
59
63
64
65
65
65
66
68
71
71
73
75
76
77
79
83
85
90
92
92
124
133
133
133
165
176
186
188
196
210
0 50 100 150 200 250 300 350
0 50 100 150 200 250
104
104
111
113
115
118
120
129
130
132
134
138
139
146
152
156
157
159
160
175
195
222
226
239
241
253
293
306
326
326
59
63
64
65
65
65
66
68
71
71
73
75
76
77
79
83
85
90
92
92
124
133
133
133
165
176
186
188
196
210
0 50 100 150 200 250 300 350
0 50 100 150 200 250

13
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
WHO. However, influenza vaccination rates in the
Netherlands among those aged 65 and over have
decreased by nearly 20 percentage points in the last
10 years. Influenza vaccinations are free for people
over the age of 60, yet vaccination campaigns are
obstructed by uncertainty about the effectiveness and
side effects of the vaccine, as well as the perceived
low risk of contracting or dying from influenza. This
perception may have changed during the COVID-19
pandemic, however, as demand for the flu vaccine
grew. Some GP practices temporarily asked individuals
between 60 and 70 years old with no underlying
conditions to refrain from getting a flu vaccination to
prioritise doses for those over 70 years old.
Dutch cancer survival rates are high but
screening rates for breast and cervical cancer
are decreasing
The Netherlands offers population screening
programmes for cervical cancer, breast cancer and
colorectal cancer. Cervical cancer screening has a
participation rate similar to the EU average, with
56% of women aged 20-69 screened within the past
two years, although participation has declined over
recent years from 68% in 2007. Similarly, breast
cancer screening rates are higher than the EU
average (76% compared to 59%), but participation
has also decreased over the last decade (Figure 12).
The relatively new Colorectal Cancer Screening
Programme (2014) covers all individuals between
55 and 75 years of age. A programme evaluation
in 2019 found that participation rates (73%) were
above expectations, with 3.9million people sending
in self-screening tests between 2014 and 2017,
contributing to higher than anticipated detection of
new colorectal cancer cases. Based on these results, it
is predicted that by 2030 nearly one in five colorectal
cancer cases and over one in three colorectal cancer
deaths may be prevented (RIVM, 2019).
Figure 12. Breast cancer screening rates are high, but have declined over the last 10 years
Not Th EU vrg s unwghtd For most countrs, th dt r bsd on scrnng progrmms, not survs
Sourcs OECD Hlth Sttstcs 2021 nd Eurostt Dtbs
Five-year cancer survival rates have improved over the
last decade and are generally above the EU average
(Figure 13). Although the Netherlands does not have
a national cancer plan, health care professionals,
researchers, policy makers and patient organisations
have come together in the Cancer Survivorship Care
Taskforce to advocate a national action plan that
recognises the continuing needs of cancer patients
and survivors. This aligns with one of the key action
areas of the recent Europe’s Beating Cancer Plan
to improve quality of life of cancer patients and
survivors, including rehabilitation and measures to
support social integration and re-integration in the
workplace (European Commission, 2021a).
Selected country
95
83
81
80
77
76
75
74
72
72
69
66
61
61
61
60
60
59
56
54
53
53
50
49
39
39
36
31
31
9
0
10
20
30
40
50
60
70
80
90
100
-

14
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 13. Five-year survival rates across six cancers exceed the EU23 average
Not Dt rfr to popl dgnosd btwn 2010 nd 2014 Chldhood lum rfrs to cut lmphoblstc cncr
Sourc CONCORD Progrmm, London School of Hgn & Tropcl Mdcn
1. The data from the Eurofound survey are not comparable to those from the EU-SILC survey because of differences in methodologies.
Promising initiatives have arisen to improve the
quality of health care
In the Dutch health care system, competing insurers
are expected to play a key role in improving quality
through contract negotiations with health care
providers (see Section 4). In practice, insurers
emphasise volume and price more than quality
in their contracting decisions, partly due to the
fragmentation and administrative burden of
collecting quality indicators. The Dutch Health Care
Institute has been tasked with developing reliable
and meaningful quality indicators and drawing
up a multi-year care improvement agenda, in
consultation with all parties involved in health care.
These initiatives can then be used to improve care,
enhance shared decision making and ultimately guide
contracting with providers.
Furthermore, some insurers have started creating
bottom-up longer-term contracts with providers
centred on value-based care, where providers and
professionals can define key performance indicators
for quality of care and delivery innovations. Medical
professional groups and the government also
contribute to quality improvement activities, such
as a new long-term care quality framework aims to
improve the quality of care in nursing homes. An
initiative to provide “the right care at the right place”
(de juiste zorg op de juiste plek) also has gained
momentum, and has helped physicians and patients
to determine the appropriate setting for COVID-19
treatment (see Section 5.3).
52 Accessibility
Very few Dutch people reported unmet needs
for medical treatment until the COVID-19
pandemic
In the Netherlands, government regulation guarantees
universal and equal access to affordable care. As a
result, the Dutch tend to report very low levels of
unmet needs for medical care (Figure 14). However,
this changed during the COVID-19 pandemic:
according to the Eurofound (2021) survey
1
, 15% of
respondents reported that they needed a medical
examination or treatment that they had not received
during the first 12 months of the pandemic. The
average reported for the EU as a whole was 21%.
The Netherlands did not shut down providers
at a national level, yet at various points during
the pandemic some hospitals postponed
non-urgent treatments due to regional outbreaks.
The professional organisations of dentists and
paramedical care providers decided to postpone all
non-emergency treatments from mid-March until
early May 2020. Cancer screening appointments were
also postponed from the onset of the pandemic until
mid-May (colon cancer), mid-June (breast cancer) and
July 2020 (cervical cancer). To resume care, multiple
stakeholder groups worked together to create a list
of diagnoses with an urgency indication, aiming to
address the most urgent plannable care first. The
Netherlands also encouraged teleconsultations as
much as possible, with about 40% of the population
taking part in a remote consultation (Eurofound,
2021).
Prostate cancer Childhood leukaemia Breast cancer Cervical cancer Colon cancer Lung cancer
Netherlands: 89 % Netherlands: 90 % Netherlands: 87 % Netherlands: 68 % Netherlands: 63 % Netherlands: 17 %
EU23: 87 % EU23: 85 % EU23: 82 % EU23: 63 % EU23: 60 % EU23: 15 %

15
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 14. The Dutch population had among the
lowest levels of unmet needs in the EU in 2019
Not Dt rfr to unmt nds for mdcl xmnton or trtmnt
du to costs, dstnc to trvl or wtng tms Cuton s rqurd n
comprng th dt cross countrs s thr r som vrtons n th
surv nstrumnt usd
Sourc Eurostt Dtbs, bsd on EU-SILC (dt rfr to 2019, xcpt
Iclnd 2018)
The health system provides broad coverage,
with voluntary health insurance covering some
gaps
Around 99.9% of the Dutch population has health
insurance, which covers a wide range of services.
Among other things, the benefits package includes
primary care, outpatient specialist care, hospital care,
maternal services, in vitro fertilisation (maximum
of three cycles), physiotherapy for chronic illness,
mental health treatment and ambulance transport.
Public spending accounts for 91% of inpatient care,
85% of outpatient care and 67% of outpatient
pharmaceuticals – all above the EU averages
(Figure 15).
The Netherlands covered the costs of COVID-19
testing, but individuals needed a physician referral
for a test until June 2020 (see Section 5.3). In an
unprecedented yet far-sighted measure, the Dutch
Healthcare Institute, which advises the Minister
of Health on the services to include in the basic
benefits package, determined that rehabilitation
care for COVID-19 patients should be included
if recommended by a physician. Specifically,
a maximum of 50 physical therapy sessions, 8
occupational therapist treatments and 7 dietician
sessions are reimbursable for up to six months after
COVID-19 infection.
Dental care for adults and some paramedical care
are not covered by the benefits package. Many
Dutch people purchase VHI to cover these services
– particularly dental care. Despite not being covered
in the benefits package, a very low proportion of the
population (0.4%) report unmet needs for dental care,
which is substantially below the EU average of 2.8%.
Figure 15. The public share of financing is higher than the EU average across all areas of health care, with the
exception of dental care
Not Outptnt mdcl srvcs mnl rfr to srvcs provdd b gnrlsts nd spclsts n th outptnt sctor Phrmcutcls nclud prscrbd
nd ovr-th-countr mdcns s wll s mdcl non-durbls Thrputc pplncs rfr to vson products, hrng ds, whlchrs nd othr
mdcl dvcs
Sourc OECD Hlth Sttstcs 2021 (dt rfr to 2019 or nrst r)
CCoouunnttrryy LLooww iinnccoommee TToottaall ppooppuullaattiioonn HHiigghh iinnccoommee LLooww iinnccoommee TToottaall ppooppuullaattiioonn HHiigghh iinnccoommee
Selected country
0 5 10 15 20
Estonia
Greece
Romania
Finland
Latvia
Poland
Iceland
Slovenia
Slovakia
Ireland
Belgium
Denmark
Italy
Portugal
EU 27
Bulgaria
Croatia
Lithuania
Sweden
France
Cyprus
Hungary
Norway
Czechia
Austria
Germany
Luxembourg
Netherlands
Spain
Malta
Low incomeTotal populationHigh income
% reporting unmet medical needs
Hh ncome Totl populton Low ncome
Unmet needs for medical care
NNeetthheerrllaannddss
89%
91%
0% 50% 100%
EU
Netherlands
Inpatient care
75%
85%
0% 50% 100%
Outpatient medical
31%
12%
0% 50% 100%
Dental care
57%
67%
0% 50% 100%
Pharmaceuticals
37%
45%
0% 50% 100%
Therapeutic
Inpatient care
Outpatient
medical care Dental care Pharmaceuticals
Therapeutic
appliances
Publc spendn s proporton of totl helth spendn b tpe of servce

16
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Health care costs are partly paid through an
out-of-pocket mandatory deductible
OOP spending fell from a peak of 11.6% of total
health spending in 2014 to 10.6% in 2019, and stands
well below the EU average of 15.4% (Figure 16). A
large share of OOP spending in the Netherlands
comes from the mandatory deductible, which requires
patients to pay a minimum amount before the insurer
begins to cover services. The mandatory deductible
increased from EUR150 in 2008 to EUR385 in 2016.
The intention was that it should grow in line with
other items in the health budget, but in 2017 the
government coalition decided to keep the deductible
at its current level, while some opposition parties
wanted to abolish it entirely. The deductible does not
apply to GP care, maternity care, district nursing and
care for children under the age of 18, which are all
available without cost-sharing.
The main categories of OOP spending include
pharmaceuticals, inpatient and long-term care
contributions under the Long-term Care Act. Since
2019, the Netherlands has capped OOP spending on
pharmaceuticals at EUR250 per year. For residential
long-term care, the country applies income-
dependent cost-sharing, ranging from no cost-sharing
to EUR2419 per month, although not all OOP
payments are related to care delivery and may include
housing costs. Furthermore, the Social Support Act
offers the opportunity for municipalities to provide
financial compensation for health care costs incurred
by patients with chronic conditions on low incomes,
and some municipalities negotiate insurance policies
with generous benefits targeted at low-income groups.
Figure 16. Inpatient care and pharmaceuticals account for over 40% of out-of-pocket payments
Not Th EU vrg s wghtd VHI lso ncluds othr voluntr prpmnt schms
Sourc OECD Hlth Sttstcs 2021 Eurostt Dtbs (dt rfr to 2019)
The Netherlands has easily accessible health
care services
The Netherlands has a dense network of health care
providers, ensuring high geographical availability of
services. In 2020, fewer than 0.15% of the population
had to travel more than 10 minutes by car to the
nearest GP practice, and GP out-of-hours centres
cover care outside office hours. However, GP practices
struggle to replace GPs after retirement, and shortages
are becoming a concern.
Although there have been a substantial number
of mergers between hospitals over the last decade,
this has not yet affected the number of locations for
accessing health care. In the Netherlands, 99% of the
population lived within 30 minutes from a hospital by
car in 2020 (Volksgezondheidenzorg, 2021). However,
the Dutch system has been experiencing excessive
waiting times in some outpatient departments.
Mental health care for children is of particular
concern, as waiting times can exceed one year. It
remains unclear how the pandemic will affect waiting
times in the longer term.
Typically, insurance companies have the option of
reimbursing only 75% of costs of services provided
by non-contracted providers. This could result in
financial barriers to accessing some hospitals for
patients who purchase cheaper (“budget”) insurance
policies that contract a limited number of providers.
During the COVID-19 pandemic, insurers agreed
to cover care delivered by all hospitals in 2020 and
2021, even if they are outside their networks (see
Section 5.3).
Government/compulsory schemes 82.6%
VHI 6.8%
Inpatient 2.1%
Outpatient medical
care 1.7%
Pharmaceuticals 2.3%
Dental care 0.7%
Long-term care 1.8%
Others 2%
Government/compulsory schemes 79.7%
VHI 4.9%
Inpatient 1.0%
Outpatient medical
care 3.4%
Pharmaceuticals 3.7%
Dental care 1.4%
Long-term care 3.7%
Others 2.2%
Netherlands
Overall share of
health spending
Distribution of OOP
spending by function
OOP
10.6%
EU
Overall share of
health spending
Distribution of OOP
spending by function
OOP
15.4%

17
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Concerted policy efforts to reduce
pharmaceutical expenditure have paid off
The Netherlands spends less on outpatient
pharmaceuticals than most other EU countries (see
Section 4). Several factors – including a long history
of volume and price control policies, a conservative
approach by GPs to issuing prescriptions and
well-established health technology assessment (HTA)
processes – have contributed to this result. Further,
the share of generic medicines by volume in the
pharmaceuticals market is the second highest after
Germany among EU countries for which data are
available. These efforts to control prices and promote
generics contribute to more affordable medicines for
patients.
A promising development is the BeNeLuxA
initiative, which aims to improve collaboration on
pharmaceutical policy and procurement; it includes
co-operation between Belgium, the Netherlands,
Luxembourg, Austria and Ireland in the fields of
horizon scanning, information sharing and policy
exchange, HTA, and pricing and reimbursement.
The BeNeLuxA initiative’s goals are consistent
with the European Commission’s pharmaceutical
strategy for Europe, adopted in November 2020,
which aims to ensure that patients have access to
innovative and affordable medicines while supporting
the competitiveness, innovative capacity and
sustainability of the EU’s pharmaceutical industry
(European Commission, 2020).
53 Resilience
This section on resilience focuses mainly on the
impacts of and responses to the COVID-19 pandemic
2
.
As noted in Section 2, the pandemic had a major
impact on population health and mortality in the
Netherlands, with around 18000 COVID-19 deaths
recorded between January 2020 and the end of August
2021. Measures taken to contain the pandemic
also had an impact on the economy, and Dutch
GDP is estimated to have declined by 3.8% in 2020,
compared to an EU average fall of 6.2%.
The Netherlands’ response to COVID-19
included measures at both regional and
national levels
The first case of COVID-19 was identified on
27February 2020 in the province of Noord-Brabant.
By 6March, residents of the province were advised
to stay at home and limit social contacts. This was
scaled up to the entire country by 12March as the
number of cases rose; the Netherlands quickly
implemented a 1.5-metre physical distancing
2. In this context, health system resilience has been defined as the ability to prepare for, manage (absorb, adapt and transform) and learn from shocks (EU Expert
Group on Health Systems Performance Assessment, 2020).
requirement and closed schools, restaurants
and non-essential in-person work, as well as
implementing other restrictive measures in the
following days (Figure 17). The measures to prevent
transmission remained in place through April 2020,
and primary schools were the first to reopen on
11May.
Further relaxation of measures continued through
summer 2020, but high infection rates in large cities
prompted some regional measures in August. As
September and October brought progressively higher
case numbers, restrictive measures heightened,
limiting the number of people who could gather
in a group and shutting down public venues. On
15December 2020, the Netherlands imposed the
strictest national restrictions to date, followed by a
curfew lasting from 23January 2021 until 28April
2021. Again, primary schools reopened first, on
8February 2021. The Netherlands progressed through
its four phases of reopening between 28April 2021
and 26June 2021. Shortly after the final reopening
phase, the Netherlands saw an exponential rise in
cases, mostly among young adults. This dropped
sharply in late summer after a reimposition of
measures restricting nightlife and large events.
The Netherlands had pandemic preparedness
tools in place prior to COVID-19
The Netherlands has a comprehensive pandemic
response plan, which was a key plank in the country’s
preparedness toolkit. Coordinated by the RIVM, it
describes in detail the general actions to take in the
case of an infectious disease crisis, including which
measures should be taken in which phase of the
crisis, and who is responsible for determining the
crisis phase.
A fragmented laboratory landscape initially
limited the number of tests performed
Prior to June 2020, testing for COVID-19 required
individuals to obtain a physician referral. After
1June, those with symptoms could register for testing
using a dedicated phone number without a referral,
but bottlenecks in testing capacity caused some
accessibility gaps. Generally, testing is performed
at the central test locations of the public health
services, under the coordination of the RIVM. At
the end of 2020, “XL” testing facilities were opened
at the national airport and in large cities; these
operated as public–private partnerships. Self-tests
started to become available at the end of March 2021
in some pharmacies, with further expansion to all
supermarkets and pharmacies in April 2021.

18
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
In September 2020, the Netherlands Court of Audit
published an evaluation of the country’s testing policy
(Algemene Rekenkamer, 2020). The report revealed
that the government did not have a clear view of
the capacity of the Dutch testing laboratories and
the supplies necessary for testing. The Netherlands
has a fragmented landscape of labs that use a
multitude of testing systems, which have experienced
varying problems with acquiring sufficient supplies.
As a result, the number of tests performed has
lagged behind the available capacity. For example,
in September 2020 the total testing capacity was
28000 per day, but the number of tests conducted on
average every day was 10000 below this capacity. This
contributed to the Netherlands having lower weekly
testing rates for much of 2020, but by September it
had surpassed the EU average (Figure 18).
Figure 18. Testing activity in the Netherlands caught up to the EU average in September 2020
Not Th EU vrg s wghtd (th numbr of countrs ncludd n th vrg vrs dpndng on th w)
Sourc ECDC
Figure 17. The number of COVID-19 cases reported in the second wave far exceeded that in the first wave
Not Th EU vrg s unwghtd (th numbr of countrs usd for th vrg vrs dpndng on th w)
Sourcs ECDC for COVID-19 css nd uthors for contnmnt msurs
Weekly cases per 100 000 population
0
50
100
150
200
250
300
350
400
450
500
Netherlands European Union
12 Mrch 2020
Dutch ctzens dvsed to
st home nd lmt socl
contcts
October 2020
Restrctons
re-ntroduced
23 Jnur 2021
Curfew
mplemented
26 June 2021
Fourth step of the
reopenn pln ll
estblshments open
28 Aprl 2021
Frst step of the reopenn
pln curfew lfted
1 June 2020
Resturnts nd
brs reopen
TTeessttiinngg aaccttiivviittyy
Note: The EU average is weighted (the number of countries included in the average varies depending on the week).
Source: ECDC.
Data extracted from ECDC on 15/03/2021 at 12:41 hrs.
CCoouunnttrryy 1100//0022//22002200 1177//0022//22002200 2244//0022//22002200 0022//0033//22002200 0099//0033//22002200 1166//0033//22002200 2233//0033//22002200 3300//0033//22002200 0066//0044//22002200
Austria #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A 139
Belgium #N/A #N/A 1 38 86 148 236 333 464
Bulgaria #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A #N/A
Croatia 0 0 4 3 13 48 103 158 218
Cyprus #N/A #N/A #N/A 7 2 26 43 40 43
Czechia 0 0 1 7 40 116 248 399 422
Denmark 0 0 6 14 85 126 172 485 478
Estonia 0 0 4 18 91 201 557 840 726
CCoouunnttrryy
Austria
Belgium
Bulgaria
Cyprus
Czechia
Denmark
European Union
Finland
France
Greece
Hungary
Iceland
Italy
Latvia
Lithuania
Malta
Netherlands
Norway
Portugal
Romania
Slovakia
Spain
Sweden
0
500
1 000
1 500
2 000
2 500
Belgium European Union Germany Netherlands
Weekly tests per 100 000 population
WWeeeekk
30-Dec-19
6-Jan-20
13-Jan-20
20-Jan-20
27-Jan-20
3-Feb-20
10-Feb-20
17-Feb-20
24-Feb-20
2-Mar-20
9-Mar-20
30-Mar-20
6-Apr-20
13-Apr-20
20-Apr-20
27-Apr-20
4-May-20
11-May-20
18-May-20
25-May-20
1-Jun-20
8-Jun-20
29-Jun-20
6-Jul-20
13-Jul-20
20-Jul-20
27-Jul-20
3-Aug-20
10-Aug-20
17-Aug-20
24-Aug-20
31-Aug-20
7-Sep-20
28-Sep-20
5-Oct-20
12-Oct-20
19-Oct-20
26-Oct-20
2-Nov-20
9-Nov-20
16-Nov-20
23-Nov-20
30-Nov-20
7-Dec-20
28-Dec-20
4-Jan-21
11-Jan-21
18-Jan-21
25-Jan-21
1-Feb-21
8-Feb-21
15-Feb-21
22-Feb-21

19
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Some public health services had to limit contact
tracing activities due to capacity constraints
In addition to running testing locations, the 25
regional public health services oversee contact
tracing activities. The services temporarily reassigned
nearly all health care-related personnel to perform
contact tracing and staff helplines. Contact tracing
started when the Netherlands recorded its first case
in February 2020. When case numbers peaked in the
middle of September 2020, 10 of the public health
services announced that they had to limit contact
tracing: at this time, they only had the capacity to call
individuals living in the same household or those at
high risk. In addition, informed contacts were asked
to report to the public health service only if they had
symptoms.
The Dutch contact tracing app experienced
delays in launching due to regulatory hurdles
The Dutch government developed the “Coronamelder”
(Corona detector) application to support tracing of
contacts of people confirmed to have COVID-19.
Downloading and using the app is voluntary, and
infections can be reported anonymously. At first, the
Netherlands issued a tender and evaluated seven
apps, but after an initial assessment none of these
appeared to meet the necessary privacy criteria.
Therefore, the Dutch government started developing
its own open source app with a group of in-house
experts. It was piloted in a few regions in August
2020 in a testing phase, and the national launch was
originally planned for 1September. After delays in
legislative approval, the app was launched nationally
on 10October 2020, and it became inter-operable with
apps from other European countries at the end of
November 2020.
Debates on the value of wearing face masks
continued until autumn 2020
Initially, the RIVM stated that face masks have a
limited effect on preventing transmission and could
lead to a misperception of safety, compromising
physical distancing rules. The government supported
this view, but made face masks compulsory on
public transportation from 1June 2020, as physical
distancing was not feasible. The government also
granted local mayors discretion on requiring face
masks, following petitions by several mayors,
who pointed out that physical distancing was not
feasible owing to the concentration of people. As
evidence on the efficacy of face masks increased, on
14October 2020, the Netherlands made mask-wearing
compulsory for everyone aged 13 and older inside
public buildings, with some exemptions. The
conflicting guidance about whether to wear a face
mask contributed to fewer than 20% of Dutch people
wearing a mask outside the home between April and
September 2020, but mask-wearing rose sharply by
the end of 2020 (Figure 19).
Figure 19. The mask-wearing rate shot up after it
became obligatory in October 2020
Sourc YouGov dt (http//wwwcovddthubcom/)
The Netherlands rapidly scaled up its intensive
care unit bed capacity to accommodate
COVID-19 patients
Before the COVID-19 pandemic, the Netherlands had
1150 available ICU beds occupied at a 70% rate on
average. The number of ICU beds in the Netherlands,
at 6.7 beds per 100000 population, falls below many
other countries in Europe, including neighbouring
Germany (33.4) and Belgium (17.4). At the beginning
of April 2020, the number of patients with COVID-19
treated in ICUs exceeded pre-existing capacity
(Figure 20). In response, the country quickly made a
plan to increase its ICU bed capacity progressively
in March and April, surpassing 1700 beds to treat
COVID-19 patients in the second week of April. In
June 2020, the number of COVID-19 patients in
ICUs dropped below 100 and remained low over
the summer. The National Coordination Centre for
Distribution of Patients took on a steering role in
the allocation of COVID-19 patients among Dutch
hospitals.
0
20
40
60
80
100
Netherlands Sweden France Italy
% of people reporting to always wear a mask outside their home

20
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Figure 20. Intensive care unit occupancy rates exceeded pre-existing capacity only for a short period
Not Th blu ln rprsnts th dl numbr of COVID-19 ptnts n ICU unts th orng ln rprsnts th ntl bd cpct n ICU unts bfor th
pndmc th orng dshd ln rprsnts th ddtonl bd cpct moblsd durng th pndmc
Sourcs OECD/Europn Unon (2020) Llor (2020)
Patients were transferred within and outside
the Netherlands for treatment
To ensure optimal use of ICU beds, COVID-19 patients
and other patients who potentially required ICU care
were sometimes transferred to other hospitals. For
instance, at one point during the first wave, 32 of the
34 COVID-19 patients in the Groningen hospitals in
the north of the Netherlands were from the southern
provinces of Noord-Brabant and Limburg. These
transfers involved up to 100 patients per day at the
end of March 2020, but tapered off by the end of
April. The army coordinated the operation using
ambulances, mobile ICUs, a special ICU bus and
two helicopters, with assistance from police escorts
to ensure smooth transfers. The Netherlands also
transferred patients to Germany, and included the use
of ICU beds in Germany in its preparation plans for
the second wave.
General practitioners coordinated COVID-19
care while implementing measures to maintain
routine services
Outside of hospitals, GPs are the first contact point
for potential COVID-19 cases. GPs determine whether
the patient should be admitted to hospital, and
until June 2020 decided whether the patient should
receive testing. If possible beforehand, the physician
discusses the consequences of an ICU admission in
a shared decision-making process with the patient,
which is standard practice in the Netherlands. Based
on this discussion, patients are able to decide for
themselves whether to receive treatment in an ICU or
at home.
To maintain routine care, GPs were advised to
organise separate office hours for patients with
respiratory complaints, to abolish walk-in office hours
and to use video instead of face-to-face consultations
whenever possible. Despite these care adaptations,
the volume of services provided decreased
significantly, particularly in the first wave. Between
12March and 20April, GPs issued approximately
360000 fewer referrals than usual, and about 290500
previously issued referrals did not lead to a specialist
consultation.
The COVID-19 vaccination rollout encountered
some initial obstacles but accelerated quickly
The initial vaccination plan created by the Dutch
Health Council prioritised individuals over the age
of 60 and at-risk groups as the first to receive a
COVID-19 vaccination. This prioritisation largely
reflected the risk of COVID-19 mortality for these
groups, particularly those living in long-term care
facilities. However, hospital organisations emphasised
that health workers in COVID-19 wards and ICU
units should receive the first vaccinations, followed
by nursing home personnel and GPs. This conflicting
advice, combined with delays in procuring the
vaccine, led to a slower start to vaccinations than
in many other EU countries. After a slow start, the
vaccination rate increased and surpassed the EU
average in May 2021. This contributed to a reduction
in the number of deaths due to COVID-19 in the
Netherlands (Figure 21).
The RIVM oversees the vaccination campaign, and
initially planned to use channels for other vaccination
efforts, such as seasonal influenza, which function at
the local level. However, the low storage temperatures
Per 100 000 population
Feb
Mar
Apr
May
Jun
Jul
Aug
Sep
Oct
Nov
Dec
ICU COVID-19 patients
0
2
4
6
8
10
12
14
16
ICU bed capacity prior to COVID-19 ICU bed surge capacity during the first wave of COVID-19 ICU COVID-19 patients
Per 100 000 population

21
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
of some vaccines and the small scale of GP practices
made this impractical, and the strategy had to adjust
rapidly to include larger-scale vaccination centres.
The first COVID-19 vaccinations were performed for
acute care staff and elderly people over the age of
75, followed by nursing home personnel. GPs began
administering vaccines on 16February 2021 when
the first vaccine that did not require low storage
temperatures became available. By the end of August
2021, 63% of the population had received two doses
(or equivalent) of a COVID-19 vaccine – nearly 10
percentage points above the EU average.
Figure 21. COVID-19 deaths dropped during the vaccination campaign
Not Th EU vrg s unwghtd (th numbr of countrs usd for th vrg vrs dpndng on th w)
Sourcs ECDC for COVID-19 css nd Our World In Dt for vccnton rts
A highly decentralised data structure and
privacy protection groups limit sharing of
health information
The Netherlands does not have a centralised
electronic health records system, and many different
providers offer electronic health record systems
that lack interoperability. An organisation facilitates
access to patient medical records in the case of
emergency care. Normally, this requires acquiring
an explicit written consent from patients in their
place of residence. During the COVID-19 pandemic,
patients were transferred to different regions, and
asking for consent was not always possible, so
temporary guidance permitted GPs to share patient
data with other providers without prior consent.
Privacy protection organisations considered this a
controversial measure, as they are concerned that
third parties could have access to the data besides
the treating physician. This conversation is likely to
continue in the context of the European Health Data
Space, which is designed promote better exchange
and access to different types of health data to support
health care delivery and health research and policy
making (European Commission, 2021b).
COVID-19 weekly mortality and vaccination rates
Note: The EU average is unweighted (the number of countries used for the average varies depending on the week).
0
10
20
30
40
50
60
70
0
1
2
3
4
5
6
Netherlands-deaths EU-deaths Netherlands-vaccination EU-vaccination
Weekly deaths per 1 000 000 population
% of the population with two doses (or equivalent)
?

22
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
6 e fndns
• At 81.5 years in 2020, life expectancy in the
Netherlands remains higher than the EU
average by about one year. Gains have slowed
over the last decade, and life expectancy
temporarily fell by over 8 months between
2019 and 2020 during the COVID-19 pandemic.
Lung cancer, stroke and ischaemic heart
disease accounted for nearly one fifth of
deaths in 2019, but 1 in 15 deaths in 2020 were
attributed to COVID-19.
• The Netherlands has lower mortality from
preventable and treatable causes than the
EU average. Lung cancer contributes to 30%
of all preventable deaths, while colorectal
cancer and breast cancer account for 40% of
treatable deaths. Mortality rates from other
treatable causes – such as ischaemic heart
disease, stroke and pneumonia – are among
the lowest in the EU. Even though cancer
causes a large share of preventable and
treatable deaths, five-year cancer survival
rates in the Netherlands exceed the EU
average.
• The Dutch population generally reports low
unmet needs for medical treatment, and
government regulation guarantees universal
and equal access to affordable care. In 2019,
only 0.2% of the surveyed population reported
unmet medical needs, but additional survey
evidence shows that over 15% of respondents
had to forgo care in the first 12 months of
the COVID-19 pandemic. Many non-urgent
services were cancelled or postponed, which
may further increase waiting times that had
already been rising in outpatient settings.
• The Netherlands is among the highest
spenders on long-term care and prevention
in the EU, and among the lowest spenders
on outpatient pharmaceuticals and medical
devices. Several factors may have contributed
to low pharmaceutical spending, including
a long history of volume and price control
policies, a conservative approach by general
practitioners to issuing prescriptions
and well-established health technology
assessment processes. International
collaboration through the BeNeLuxA initiative
also aims to improve collaboration on
pharmaceutical policy and procurement.
Public spending covers a high percentage of
health care expenditure, with the exception
of dental care, and many people have dental
coverage through voluntary health insurance.
Out-of-pocket expenditure in the Netherlands,
at just over 10%, is considerably below the
EU average of 15%, while voluntary health
insurance spending exceeds the EU average.
• While the Netherlands had a national
pandemic response plan in place and a high
level of preparedness before the COVID-19
pandemic, the health system response
encountered obstacles. In particular, testing,
contact tracing and vaccination efforts
suffered from limited capacity, fragmentation
and lack of coordination. More positively, the
pre-existing primary care gatekeeper system
offered shared decision making between the
patient and provider to determine the desired
treatment for COVID-19 patients.
• The need for a coordinated response to the
COVID-19 pandemic – for example, in contact
tracing and testing – overruled pre-existing
structures in the Dutch health care system
that separated payers and providers and
distanced the Ministry of Health from direct
intervention in the system. Temporary
legislation updated financial relationships and
patient management to enable the necessary
national-level responses, such as transferring
patients between regions and sharing patient
data.

23
Stte of Helth n the EU The Netherlnds Countr Helth Profle 2021
Countr bbrevtons
Austr AT
Belum BE
Bulr BG
Crot HR
Cprus CY
Czech CZ
Denmr D
Eston EE
Fnlnd FI
Frnce FR
Germn DE
Greece EL
Hunr HU
Icelnd IS
Irelnd IE
Itl IT
Ltv LV
Lthun LT
Luxembour LU
Mlt MT
Netherlnds NL
Norw NO
Polnd PL
Portul PT
Romn RO
Slov S
Sloven SI
Spn ES
Sweden SE
e sources
ronemn M et l (2016), Th Nthrlnds hlth
sstm rvw Hlth Sstms n Trnston, 18(2)1-239
OECD/Europen Unon (2020), Hlth t Glnc
Europ 2020 – Stt of Hlth n th EU Ccl
Prs, OECD Publshn
References
Alemene Reenmer (2020), Tstn op Coron, https//
wwwreenmernl/publctes/rpporten/2020/09/23/
testen-op-coron
EU Expert Group on Helth Sstems Performnce
Assessment (HSPA) (2020), Assssng th rslnc of
hlth sstms n Europ n ovrvw of th thor,
currnt prctc nd strtgs for mprovmnt
Eurofound (2021), Lvng, worng nd COVID-19 surv,
thrd round (Februr-Mrch 2021)
Europen Commsson (2020), A phrmcutcl strtg
for Europ
Europen Commsson (2021), Europ’s Btng Cncr
Pln
Europen Commsson (2021b), Th Europn Hlth
Dt Spc
Llor A (2020), Numbr of ICU bds ndd wll dcrs
to norml lvls b 1 M, OMT expects,
https//
dutchrevewcom/news/number-of-cu-beds-needed-wll-
decrese-to-norml-levels-b-1-m-omt-expects
RIVM (2019), Bvolngsondrzo drmnr s
succsvol Blthoven
Volsezondhedenzor (2021), Publc hlth nd hlth
cr nformton
http//wwwvolsezondhedenzornfo
WHO Reonl Offce for Europe, Europen Commsson,
Europen Observtor on Helth Sstems nd Polces
(2021), COVID-19 Helth Sstems Response Montor –
The Netherlnds

Stte of Helth n the EU
Countr Helth Profle 2021
The Countr Helth Profles re n mportnt step n
the Europen Commsson’s onon Stt of Hlth n
th EU ccle of nowlede broern, produced wth the
fnncl ssstnce of the Europen Unon The profles
re the result of ont wor between the Ornston
for Economc Co-operton nd Development (OECD)
nd the Europen Observtor on Helth Sstems nd
Polces, n cooperton wth the Europen Commsson
The concse, polc-relevnt profles re bsed on
trnsprent, consstent methodolo, usn both
quntttve nd qulttve dt, et flexbl dpted
to the context of ech EU/EEA countr The m s
to crete mens for mutul lernn nd voluntr
exchne tht cn be used b polcmers nd polc
nfluencers le
Ech countr profle provdes short snthess of
· helth sttus n the countr
· the determnnts of helth, focussn on behvourl
rs fctors
· the ornston of the helth sstem
· the effectveness, ccessblt nd reslence of the
helth sstem
The Commsson s complementn the e fndns of
these countr profles wth Compnon Report
For more nformton see eceuropeu/helth/stte
Plese cte ths publcton s OECD/Europen Observtor on Helth Sstems nd Polces (2021),
Th Nthrlnds Countr Hlth Profl 2021, Stt of Hlth n th EU, OECD Publshn, Prs/Europen
Observtor on Helth Sstems nd Polces, Brussels
ISBN 9789264942196 (PDF)
Seres Stte of Helth n the EU
SSN 25227041 (onlne)
