
Diffusing Capacity:
2017 ATS/ERS Standards
for single-breath carbon uptake
in the lung
Susan Blonshine RRT, RPFT, FAARC, AE-C

Joint ATS/ERS Taskforce
Recent literature reviewed
Surveyed current technical capabilities of
instrumentation manufactured
Recommendations reflect consensus of task
force related to
– Evidence
– Expert opinion where peer-reviewed evidence
was not available or incomplete

Update of 2005
Update in regards to RGA systems
Provide new calculation standards
incorporating continuous gas analysis
Standard restricted to single-breath
technique
Five committee members from 2005 and
four new members

RGA versus Current Systems
Focused on Rapid-response Gas Analyzers
(RGA)
– new suggestions and requirements for labs and
manufacturers required for systems with a RGA
– gas analyzers with a 0 to 90% response time of
less than or equal to 150 ms
– Real-time, continuous gas analyzers but tend to
use discreet measurements
– Allow marked improvements using data with
continuous measurements

RGA versus Current Systems
Authors do state that the new standards do
not make older systems that use discrete
alveolar sampling and slower gas analyzers
obsolete (classical systems)

Equipment Requirements
A reminder that any error in flow and the
calculation of volume results in a
corresponding error in DLCO
Requirements are included for both RGA
systems and classical discrete sampling
systems

Equipment Requirements
Flow accuracy required to be ± 2% over a
range of ± 10 L/sec
Volume accuracy required to be ± 2.5% (±
75 ml) instead of ± 3.5% with a 3-L syringe
– Volume accuracy must be maintained across
range of gas compostions and concentrations

Equipment Requirements
RGA response time (analyzer rise time)
required to be ≤150 milliseconds (new)
– Not required for classical discrete samples
Analyzer linearity for both RGA and
discrete sample systems ± 1.0% from ±
0.5% in the 2005
Equipment Requirements
RGA systems have bot a lag time for the
sample to reach the analyzer and the
analyzer response time to consider
Gas concentration signal must be shifted
and precisely aligned with the flow signal
– 100 ms increase in 0-90% response time, error
in DLCO increases 0.7%

Graphic Display

Phase Alignment

Equipment Requirements
CO analyzer accuracy for both RGA and
discrete sample systems is ≤10 ppm
(±0.3% of 0.3% CO) (2005 was ± 0.5% of
0.3% CO)
Interference from CO2 and water vapor for
both RGA and discrete sample systems is
≤10 ppm error in CO (when CO2 and water
vapor are ≤5

Equipment Requirements
Digital sampling rate now specified as a
minimum of ≥100 hz with a resolution of 14
bits. A 1000 hz sampling rate recommended.
Analyzer drift should ≤ 10 ppm for CO and
0.5% of full scale for the tracer gas over 30
seconds.
– manufacturers should provide a test mode to test
Barometric pressure sensor accuracy is
required to be within ±2.5%.

Manufacturer Requirements for RGA
Monitor and report end-expiratory tracer
gas and CO concentrations
– alert the operator if washout from previous
testing is incomplete.
Compensation for end-expiratory gas
concentrations prior to test gas inhalation in
the calculation of VA and DLCO.
Ensure proper alignment of gas
concentration signals and the flow signal

Manufacturer Requirements for RGA
Measure anatomic dead-space using the Fowler
method.
Display a graph of exhaled gas concentration
versus volume (not time) to confirm point of
dead-space washout and to report the amount
of manual adjustment if this was done.
Measure VA using all of the tracer gas data
from the entire maneuver in the mass balance
equation.

Manufacturer Requirements for RGA
Report the DLCO adjusted for the change in
PAO2 due to barometric pressure.
– recommended (but not required)
– Ability to input simulated digital test data and
compute DLCO, VA, TLC and Vb with ± 2%
accuracy expected.
– Report the DLCO adjusted for change in PAO2 due
to PACO2 with ± 2% accuracy.
Additional requirements
Maximum inspiratory pressure for demand
valves has been reduced to <9 cmH2O
Machine deadspace for adult testing has
decreased to 200 ml from 350 ml
– machine deadspace should be smaller for
children and patients with a VC <2.0 L

Calibration and QC Requirements
Daily volume calibration must now be
performed three time with a 3-liter syringe
with using varying flow rates between 0.5
and 12.0 L/sec (injection times 0.5 – 6.0
seconds). Accuracy was not previously
specified and now must be <2.5% error.
– Disposable flow sensor from the batch used
must be tested each day
– Recheck if temperature changes 3 degrees C or
relative humidity changes by more than 15%

Calibration and QC Requirements
Calibration recheck also recommended
when differnces between VI and VC or VA
and TLC are apparent
Timer accuracy was specified in the 2005
standards. There are no timer specifications
in the 2017 standards.

Calibration and QC Requirements
Flow sensor zeroing prior to testing is now
required.
Gas analyzer linearity must now be checked
monthly. The 2005 standards specified
every three months. Manufacturers are
urged to automate this process.
A monthly calibration syringe leak test is
now required.

Analyzer Linearity Check
Serial syringe dilutions
DLCO simulation with high precision gases
In absence of above, manufacturer must
provide test option like patient, but reported
VA at ATP with 3-L syringe

Calibration and QC Requirements
Both biological and calibration syringe QC
testing are now required weekly. Previously
either biological or calibration syringe QC
were to be performed weekly.
Calibration and QC Requirements
BioQC requiring action are relaxed to a >12%
change or >3 ml/min/mmHg (whichever is larger)
from a simple >10% change ***
– 2017 standards also state that a mean of 6 prior tests
should be used
– Manufacturers urged to developed automated QC
QC and calibration records can be kept in a digital
file

Calibration and QC Requirements
Syringe QC required measured VA to be within ± 300 ml of 3-L
{STPD to BTPS conversion factor} 24% factor
– Absolute DLCO less than 0.5 ml CO/min/mmHg (.166 SI)
ERROR NOTED: Correction factor should be ATPD to BTPS
"The calculation of VA must be within 300 mL of 3 L times the
ATPD to BTPS (body temperature, ambient pressure, saturated with
water vapour conditions) correction factor, which is 310/Tamb x
PB/(PB-47), where PB is the barometric pressure in mmHg and
Tamb is the ambient temperature in degrees kelvin.“
– With 72 degrees Fahrenheit = 295.4 degrees kelvin, this would be
approximately a 12% correction factor.

Calibration and QC Schedule

Additional Maintenance
Replace permeable tubing according to
manufacturer recommendations
Chemical gas analyzers should have a
replacement schedule

Patient Condition
Subject should not breathe supplemental
oxygen for > prior to the test
Refrain from smoking on day of test
Record time of last cigarette
– Correct for COHb

Test Performance
Deep breaths during TV pre-test avoided in the
2005, not included in 2017 standards
Maximum time for exhalation to RV is 12
seconds
Inhale rapidly to TLC in less than 4 seconds
VI target based on patient’s largest VC ≥90
– VI of ≥85% of the patient’s largest VC is acceptable
if VA is within 200 ml or 5% (whichever is larger) of
the patient’s highest VA from acceptable DLCO
maneuvers.

Test Performance
With RGA exhalation following BHT continue to
RV to calculate VA using a mass-balance
equation
– Total expiratory time for discrete sample systems
(washout and sample collection time) is still ≤4
seconds but is specified as ≤12 seconds in RGA
systems
DLCO test mixture required to contain 21% O2,
.3% CO, tracer, balance N2

Test Performance
Wait between tests (4 minutes minimum, 10
minutes for patients with severe obstruction)
– tracer gas concentration at end-exhalation (prior to
the inhalation of the test gas mixture) should be ≤ 2%
of the inspired concentration
Recommend end-exhalation concentrations of
CO (prior to inhalation of the test gas mixture) be
used to adjust DLCO tests for CO back-pressure,
to calculate COHb and to compensate for the
effects of water vapor and CO2 on gas analyzers

Potential Problems in Breathing
Manuever

Washout and Sample Collection
RGA systems
– Collection prior to point of deadspace washout
understimates DLCO
– Collection beyond will overestimate DLCO
Classical systems
– Washout volume .75 to 1.0 L
– Decrease to .5 L when VC less than 2 L

Analysis Window

Breath Hold Time

Test Performance
Effect of prior testing (spirometry,
bronchodilators and N2 washouts) on DLCO
– bronchodilators are unlikely to affect DLCO and may
therefore be used prior to DLCO testing
– prior spirometry efforts may affect DLCO but this
has not been proven and therefore makes no
recommendations against performing spirometry
prior to DLCO testing
– After N2 washout, time for alveolar O2 levels to
return to normal is needed (2 times O2 wash-in time)

VA Calculation
Classical systems
– Reported at BTPS, converted to STPD to
calculate DLCO
– Need VI and change in tracer gas
– Need to know equipment and anatomical DS
RGA systems
– DS is measured by Fowler method
– Anatomic is Fowler minus equipment DS
– Higher VA and DLCO (8 to 15% in COPD and
uncontrolled asthma)
May want to report 2005 DLCO and RGA
VA

Fowler Dead-Space

Test Quality Grading

Grading System
This is considered an interim grading
system until studies can be completed to
validate it based on the 2017 standards
Further research is needed

Which DLCO to report?
Average 2 or more grade A maneuvers that
are repeatable
Average DLCOs from all grade A if not
repeatable
Only 1 grade A, report result
If no acceptable, average maneuvers with B,
C, and D scores
If only F grade, no DLCO reported

Other Recommenations
RGA systems calculate VA using mass-
balance equations
Equation for calculating anatomical deadspace
using height is different from 2005
Measurement of anatomical dead space using
the Fowler technique discussed in detail
Discuss flow and gas analyzer signal
alignment in detail.
Discuss KCO

Other Suggestions
Phase III slope for ventilation
inhomogeneity
Repeatability 2.0 ml/min/mmhg
Scoring/grading system for test quality
based on inspired volume, breath-holding
time and sample collection time
New equation to correct DLCO for end-
exhalation CO, altitude and barometric
pressure correction

Other Suggestions
Equations to estimate barometric pressure at
altitude that were not in the previous
standards.
2005 standards included equations to
correct DLCO for alveolar volume that are
not discussed and not included in the 2017
standards.
Adjustments are made in predicted value,
not measured

Available Results to Report
DLCO adjusted for barometric pressure
DLCO LLN and/or Z-score
VA LLN and/or Z-score
KCO (instead of DLCO/VA)
KCO LLN and/or Z-score
Barometric pressure
Breath-hold time
Fowler anatomical dead space (RGA systems only)
Single-breath TLC (RGA systems only)
Test quality grade for acceptable maneuvers
Reference values source
Graphs of full maneuver
Graphs of exhaled gas concentrations versus volume (RGA systems
only).
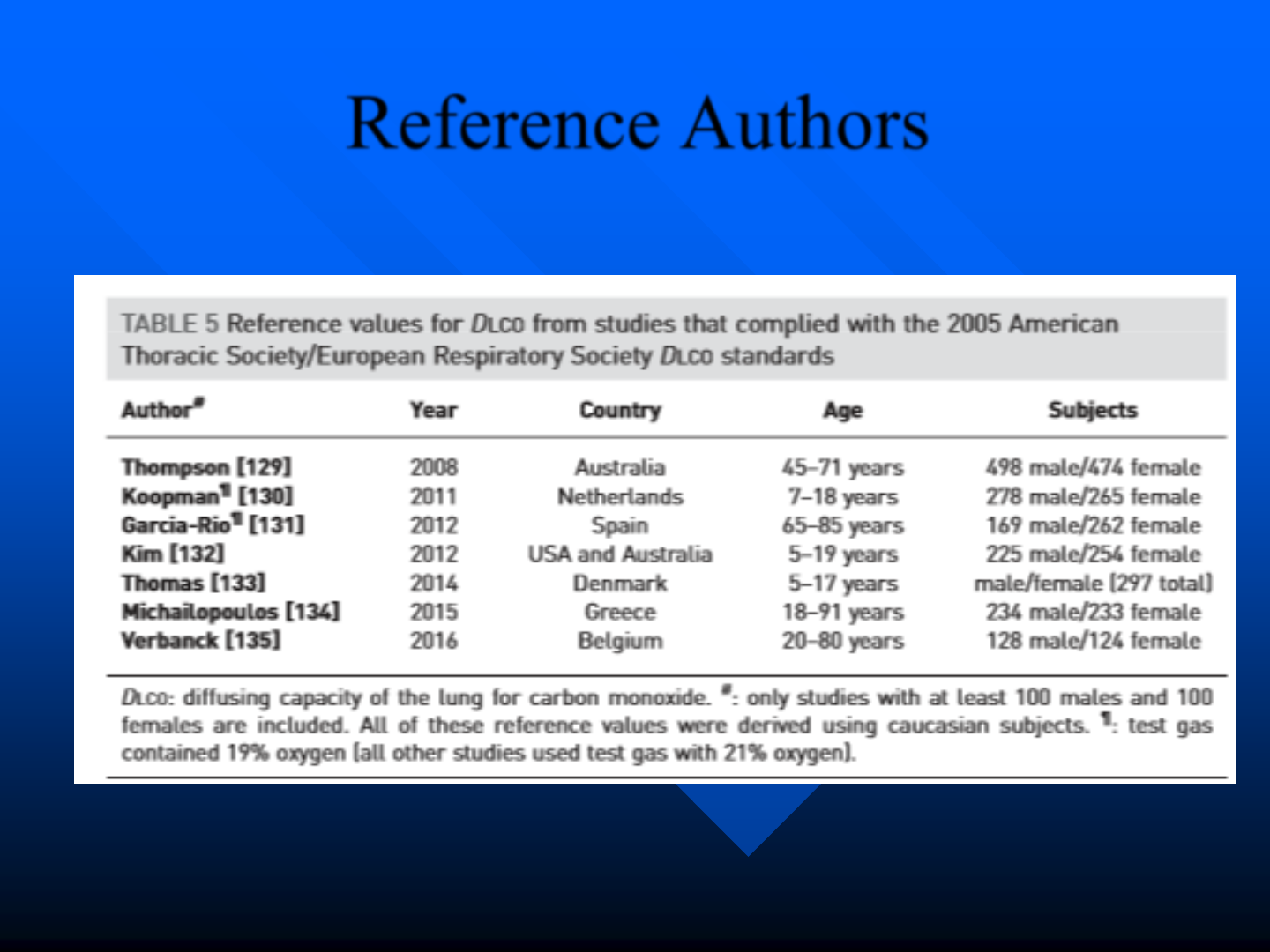
Reference Authors

Other Considerations
New equipment will meet or exceed 2017
standards
Universal format for output needed
New standards for interpretation needed
Ten area identified for further research

Any Questions?
Susan Blonshine BS, RRT, RPFT, FAARC, AE-C
TechEd Consultants, Inc.
www.techedconsultants.com
