

We value and appreciate you as a
member of our exceptional team at
SSM Health. Thank you for being a
healing presence to our patients, their
families, each other, and all those we
serve. You are SSM Health!
At SSM Health, we are committed to
offering a flexible benefits package
that you can personalize to fit your
needs and those of your family. You
may choose the benefits that are best
for you.
To understand the benefit options
completely, including benefits that may
be offered at no cost, it is important
that you read the materials outlined in
this guide.
Once again, thank you for your
commitment and dedication to our
Mission and for providing an
exceptional experience for our patients
and those we serve.
What’s New in 2024 and Benefit Reminders ............ 1
Important Benefit Contacts and Resources .............. 5
Benefit Eligibility and Enrollment .............................. 6
Medical Plans ........................................................... 8
Pharmacy Benefits .................................................. 15
Pharmacy Directory ................................................ 17
Discounted Medical Premiums ............................... 18
Dental Plans ........................................................... 21
Vision Plans ............................................................ 23
Pre-tax Savings ...................................................... 25
Retirement Savings Program ................................. 29
Paid Time Off .......................................................... 32
Life Insurance ......................................................... 36
Professional Development ...................................... 38
Additional Benefits .................................................. 40
Required Notices .................................................... 43
This informational booklet provides key features of the
personal benefits offered at SSM Health and is for reference
purposes only. When there is a discrepancy between this
information and information in the Summary Plan Description
(SPD), the SPD will prevail.
1
What’s New in 2024 & Benefits Reminders
WellFirst Health is now Medica
The WellFirst Health medical plan is now Medica. SSM Health employees will continue to use their existing network of
providers and continue to access their member account at wellfirstbenefits.com/employees. New Medica ID cards for the
2024 plan year will be distributed to all plan participants prior to January 1, 2024.
2024 Medical Plan Rate and Cost Sharing Changes
SSM Health continues its commitment to keeping the cost of medical plan premiums and care affordable for you and your
family, while balancing the pressure of higher costs for services and increased plan utilization. The monthly premium
increase for the medical plans is limited to $10 - $50. To align with the market, Plan deductibles and out-of-pocket
maximums will increase between $100-$200. You may view the new rates and cost-sharing information in the medical
plan section of this booklet.
Pharmacy Benefit Update: Cost Sharing Changes and Savings Options
Pharmacy copays will be increasing between $3 - $10 based on the prescription drug’s tier and whether you are
purchasing a 30-day or 90-day supply. You are encouraged to take advantage of the significant discounts that are
available through your local SSM Health Pharmacy. If you are not close to an SSM Health pharmacy, you can take
advantage of their mail order option. SSM Health Pharmacies will also be offering a “6 for $6” program. This program
offers you a six (6) month supply of certain prescriptions for a one-time payment of $6 dollars. More information about
this program and the eligible prescription drugs, visit ssmhealth.com/benefits or the Benefits App in Workday.
Spouse/LDA Surcharge Waiver – Active Election Reminder
If you are covering an adult on your medical plan (a spouse or legally domiciled adult) and you are eligible for the
surcharge waiver, you must submit the waiver through Workday. No supporting documentation or paper forms are
required, you but must complete the electronic certification of your surcharge status prior to the 2024 plan year. You are
encouraged to submit your 2024 waiver during Benefits Open Enrollment to ensure your waiver will be applied effective
January 1, 2024. The surcharge will automatically apply until you have submitted a waiver for the 2024 plan year
and refunds cannot be issued. Reminder, the surcharge only applies to an adult (spouse or LDA) that you are covering
on the medical plan. It does not apply to any dependent children under the age of 26 that you may be covering.

2
Out-of-Area Coverage Recertification
If you or a covered family member do not reside within the WellFirst Health/SSM Health service area, you may apply for
out-of-area coverage and access care through the nationwide FirstHealth network of providers and facilities. You must
submit an out-of-area certification form each plan year. You may check the zip code directory to confirm you are still
eligible and submit the certification form at wellfirstbenefits.com/employees. Note, complete the certification form before
January 1, 2024 as you must be approved for out of area coverage before you begin or continue using the FirstHealth
network.
Cost-Effective Care Options: Your SSM Health Care Team
If you have not yet established a relationship with an SSM Health Primary Care Provider, you are encouraged to do so.
You may find an SSM Health provider by visiting wellfirstbenefits.com/employees. You may also access same day care
through the SSM Health Express Virtual Care or Urgent Care options. Video, e-visits and in-person appointments are
available by visiting ssmhealth.com or logging into your MyChart account.
Dental and Vision Plan Updates
There will be no rate changes to the Dental Base plan. Increases to the Dental Plus plan will be limited to $4 - $9 per
month based on your coverage election. There are no rate changes to the Vision Plan premiums.
Health Savings Account Limits Increased
Effective January 1, 2024, you may contribute an additional $300 per year for employee-only coverage and an additional
$550 per year if you are covering dependents to your Health Savings Account (HSA). Employees who have elected the
WellFirst Health Savings Plan and meet eligibility requirements may participate in the HSA. The SSM Health contributions to
your HSA remain the same. Review the Health Savings Account section of this booklet for additional information.
Flexible Spending Accounts – 2024 Limits Announced; HCFSA Carry Over Provision Reminder
Employees who elect to fund a Health Care Flexible Spending Account (HCFSA) may contribute up to $3,050 pre-tax.
Employees who elect to fund a Dependent Daycare Flexible Spending Account (DCFSA) may contribute up to $5,000 pre-
tax per household. If you are a highly compensated employee (annual compensation of $150,000 or more), your DCFSA
contribution is limited to $2,500 due to non-discrimination testing required by the IRS.
If you elect a minimum of $100 in your HCFSA for plan year 2024, you may carry over up to $570 of your 2023 HCFSA
funds. Minimum balance that can be carried over is $25. Review the Flexible Spending Account section of this booklet
for additional information and to understand important program guidelines and timelines.

3
Short-Term Disability Buy-Up
Good news! There will be a reduction in the Short-term Disability Buy-Up rates for 2024. Visit the enrollment system in
Workday to view the cost of the buy-up option and the amount of benefit it would provide you.
Legacy Planning and Beneficiary Resources through Securian Financial
Employees who are eligible for and covered by the SSM Health life insurance policies may access a variety of online
resources, including basic will preparation and budget analysis, tax planning, and grief support. Employees may visit
LifeBenefits.com/Lfg (username: lfg, password: resources) or call 877-849-6034 to access the tools and resources.
Benefits Plus – Voluntary Benefits
You are encouraged to visit the Benefits Plus Portal to review comprehensive voluntary benefit information and access
valuable employee discounts. See the Voluntary Benefits section of this booklet for additional information about these
offers. Reminder, during Benefits Open Enrollment only, you may enroll in or make changes to Accident, Critical Illness,
and Hospital Indemnity Insurance as well as the Prepaid Legal Services offered through MetLife. At any time, you may
purchase Identity Theft Protection, Auto and Home Insurance, and Pet Insurance.
Benefits Plus – MetLife Prepaid Legal Services Now Offers Family First
If you elect the MetLife Legal Plus Plan, Family First has been added to provide for eldercare counseling and referral
services through a Care Team that can provide guidance and solutions. Premiums will reflect a $1 monthly increase to
allow for these added benefits. To learn more about these services, you may view an informational video.
Benefits Plus – Purchasing Power
To ease the burden that unexpected household expenses can cause, SSM Health has partnered with Purchasing
Power. While paying with cash is always the best option, when cash is not available, Purchasing Power offers an easy
way to get products you need now with the option to pay for them directly through your paycheck over time. No credit
checks are required. To be eligible, you must have annual earnings of at least $20,000 and be an active, benefit-eligible
employee who has completed at least 90 days of service. Open the Benefits App in Workday and select Purchasing
Power or visit ssmhealth.purchasingpower.com to learn more. Note, this is not a discount program, but may help you
avoid costly payday loans and/or rent-to-own options.
DailyPay
SSM Health now partners with DailyPay to provide on-demand access to your earned pay. Learn more about and/or
enroll in DailyPay at dailypay.com/employee. Note, Physicians and Executives are not eligible to participate.

4
Announcing new System-Wide Wellness Program: myhealthylife
We know that many of you are looking for easy, attainable ways to live your healthiest life. To support you in that goal, we
are excited to introduce myhealthylife, the SSM Health Employee Wellness Program. Beginning in 2024, you will have
access to the resources and tools you need to improve your well-being and will be encouraged to participate in fun,
rewarding personal challenges that promote self-care. Through the Sharecare app, you can make small steps that lead to
big changes in your everyday life. Watch for program details that will be shared later in 2023.
Long-Term Care Insurance to be offered in 2024
With the increased focus on the need for long-term care protection, SSM Health will be offering a Long-Term Care benefit
that can be purchased through payroll deduction and will offer group rates. More information about the available options
and a special enrollment period will be offered in 2024. Note, long-term care will not be included during the current
benefits open enrollment – but will have its own special enrollment period in 2024.
Expanded Professional Development Opportunities – Announcing FlexPath Funded
In addition to traditional tuition reimbursement, a new educational offering known as FlexPath Funded will provide up to
$5,250 each year in upfront tuition benefits. Eligible employees may use FlexPath funds for coursework towards a degree
from select online universities or toward online skills-based courses in a wide variety of areas and interests. Watch for
information about this exciting new program that will be shared in the coming weeks and months.
5
Important Benefits Contacts & Resources
Comprehensive Benefit Information
Access informational videos, helpful tools, and comprehensive plan documents by
visiting ssmhealth.com/benefits.
Benefits and Workday Support
Contact People Services at 844-776-6947 during business hours
Monday-Friday, 7 am – 5 pm or create an AskHR case 24/7.
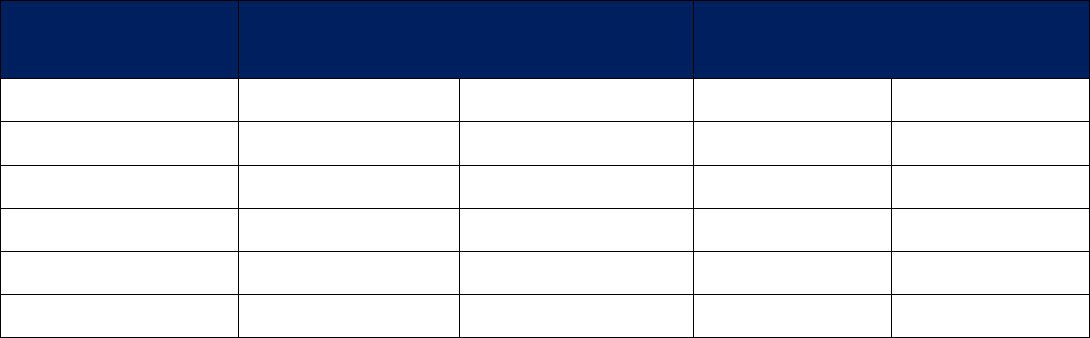
Benefit Vendors/Administrators – 2024 Plan Year
Vendor Name
Benefit Administered
Website
Phone
Medica/WellFirst Health
Medical Plan
wellfirstbenefits.com/employees
877-274-4693
Navitus
Prescription Plan
navitus.com
866-333-2757
Delta Dental of Missouri
Dental Plan
deltadentalmo.com
800-335-8266
VSP
Vision Plan
vsp.com
800-877-7195
Optum Financial
HSA and FSA Accounts
optumfinancial.com
844-881-0124
Fidelity
403(b)/401(k)/457(b) Plans
netbenefits.com
800-343-0860
Securian Financial
Life Insurance
securian.com
833-810-8262
Sedgwick
Leave of Absence & Short-Term Disability
mysedgwick.com/ssmhealth
855-253-0820
New York Life Group Benefits
Long-Term Disability
mynylgbs.com
800-362-4462
Corestream
Benefits Plus (Voluntary Benefits)
includes Purchasing Power Program
ssmhealth.corestream.com
855-925-5700
Personal Assistance Services (PAS)
Employee Assistance Program
mypaseap.com
Company code: SSM
800-356-0845
SSM Health at Work (employees of
Greater Fond Du Lac Ministries)
Employee Assistance Program
SSM Health at Work
800-458-8183
IMPORTANT NOTICE:
At SSM Health, we send benefits
reminders and notifications via
work email and Workday –
remember to check these on a
regular basis.

6
Benefit Eligibility and Enrollment
For benefit eligibility, you must be regularly scheduled to work at least half-time (40 hours) or more per pay period.
“Regularly scheduled” means that you are on file with Human Resources as having a 0.5 full-time equivalent (FTE) or
higher status. For example, a 0.4 FTE working extra hours does not qualify as “regularly scheduled.” Benefits are effective
on the first day of the month coinciding with or following hire date.
Full-time Benefits-Eligible Status
Part-time Benefits-Eligible Status
64+ hours pp (.80 – 1.0 FTE)
40 – 63 hours (.50 - .79 FTE)
If you are a benefits-eligible employee, you may also choose to cover your eligible dependents. Eligible dependents
include:
• An eligible child up to age 26 (your child(ren): biological, foster, adopted, step or a child for whom you have legal
guardianship)
• Disabled child(ren) age 26 and older may be eligible for benefits
• Your spouse
• A Legally Domiciled Adult (LDA)
Note, you may only cover an LDA on your health plans (medical, dental and vision); only ONE adult (Spouse or
LDA) may be covered on your health plan(s) at one time.
• The dependent child(ren) of an LDA
Legally Domiciled Adult
If you are not covering a spouse on your plan(s), you have an opportunity to cover another adult on your plan(s) through
the Legally Domiciled Adult (LDA) option.
An LDA could be an adult child (over the age of 26) who no longer meets the definition of eligible child, a parent, relative
or another adult. The LDA must be at least 19 years of age and reside in the same household as you. The LDA’s
dependent child(ren), even if the child(ren) reside in another household, can also be covered. If covering an LDA or a
child of an LDA, make sure you indicate their relationship to you as an LDA or LDA Child when entering their information
in Workday. There are important tax implications and supporting documentation requirements that apply to the LDA
option. If you are interested in covering an LDA and/or and LDA’s child on your benefit plan(s), review the LDA Verification
Guidelines and Imputed Income Tax Tables available at ssmhealth.com/benefits.

7
Making Changes to Your Benefits
Qualified Change in Status
If you have a qualified change in status during the plan year, you may be
allowed to change your level of coverage before December 31. IRS guidelines
limit the type of election change that can be made following each type of
change in status. Report ANY qualified changes in status through your Workday
Benefits App within 31 days of the event if you want to change your benefit
election(s) to reflect the change. Premiums will be collected from the date of
the Qualifying Event.
Eligible changes in status include, but are not limited to:
•
Family changes such as marriage, divorce, legal separation, annulment,
death of your spouse or dependent, birth, adoption, or placement for
adoption of your child, or your dependent child ceases to satisfy the
plan’s eligibility requirements.
•
Changes in employment status by you or your family member such as termination or commencement of
employment, strike or lockout, commencement of or return from an unpaid leave of absence, change in worksite, or
a switch from full-time to part-time or from salaried to hourly employment (or vice versa) that causes you or your
family member to lose or gain eligibility for coverage.
Loss of Medicaid or Children’s Health Insurance Program (CHIP) Eligibility
Benefit changes must be submitted through the Benefits Apps in Workday within 60 days of the date Medicaid or CHIP
coverage terminates.
Open Enrollment
The other opportunity to make changes to your benefits is during the benefits open enrollment period. This gives you a
chance to re-evaluate your benefit needs and make changes. You will receive open enrollment materials in
October/November for elections to be effective January 1.
IMPORTANT NOTICE: IRS guidelines
limit when certain election changes can
be made.
These include:
• Qualified Changes in Status
• Loss of Medicaid or Children’s
Health Insurance Program
(CHIP) Eligibility
• Open Enrollment

8
Medical Plans
At SSM Health, the needs of the patient come first – and that includes you and your family. That’s why all SSM Health
Plan options cover the same services. There is no need to compare your medical plan options based on services. Instead,
review the cost-sharing amounts – the premiums, deductibles, copayments, and out-of-pocket maximums – to determine
what meets your preferences or needs. If you would like help choosing the plan best for you, consider using the Benefit
Enrollment Decision Support Tool. Note – WellFirst Health is transitioning to a new name – Medica. You will begin to see
the Medica name integrated into your ID cards and medical plan materials in 2024.
All SSM Health employees will be able to choose from the same three medical
plan options:
• Medica/WellFirst Plus option ($500 individual deductible)
• Medica/WellFirst Base option ($1,100 individual deductible)
• Medica/WellFirst Health Savings option ($1,600 individual deductible;
paired with an SSM Health funded Health Savings Account)
You may select one of four coverage tiers: Employee Only, Employee +
Spouse/LDA, Employee + Child(ren), or Employee + Family
Provider Network
The Medica/WellFirst Health Network is the primary provider network for plan members. Visit
wellfirstbenefits.com/employees to view the Provider Directory.
Out-of-Area Coverage – Certification Form is Required Each Plan Year
If you or a covered family member is residing outside of the SSM Health service area, you may apply to have your
medical claims covered as out-of-area. Any eligible out-of-area member, regardless of region, has access to the
FirstHealth network. To search for a provider, visit firsthealth.com. To determine eligibility, visit
wellfirstbenefits.com/employees and review the list of SSM Health Employee Health Plan network zip codes to determine
if you or your covered dependents qualify as out of area. If your home zip code is not listed, complete the out-of-area
form. You will need to complete and submit the out-of-area form so your claims are covered. Please wait until
Medica/WellFirst Health has approved your out of area status before you or your covered dependents begin using the
FirstHealth network. You must resubmit the out-of-area form each plan year.
IMPORTANT NOTICE:
As part of the transition to Medica,
new ID cards will be sent to all plan
participants before January 1, 2024.
You may continue to access your
member portal and order additional
ID cards at:
wellfirstbenefits.com/employees.

9
Your Annual Total Cost for Health Care
Since your health care needs are personal to you and there are many factors to consider, SSM Health has an online
Benefit Enrollment Decision Support Tool to help you compare your medical plan options. The tool includes 12 months
of your medical and pharmacy claim information (if available) and allows you to enter basic information about yourself
and your anticipated health care expenses. It will provide you information about your total anticipated costs under each
of the SSM Health Medical Plan options – including the premiums you would pay out of your paycheck – and your
estimated out-of-pocket cost-sharing expenses. This tool is completely confidential and is designed to assist you with
your benefit enrollment decisions. Note, the tool does not enroll you in your benefit elections. Visit the enrollment
system in Workday, to enroll in your benefits.
Cost-sharing Amounts
Medica/WellFirst Plus
Option
Medica/WellFirst Base
Option
Medica/WellFirst Health Savings
Option
Annual Deductible
$500 per person
$1,100 per person
$1,600 employee only
$1,000 per family
$2,200 per family
$3,200 per family
Coinsurance
15%
15%
15%
Deductible/Coinsurance Limit
If you reach this limit, you will only be responsible for copays until you
reach the Out-of-Pocket Maximum.
$2,600 per person
$5,100 per person
$3,100 employee only
$5,200 per family
$10,200 per family
$6,200 per family
Annual Out-of-Pocket Maximum
Copays are applied to this limit. Once you reach the Out-of-Pocket
maximum, you will have no additional out-of-pocket expenses.
$4,100 per person
$6,600 per person
$4,600 employee only
$8,200 per family
$13,200 per family
$9,200 per family
Preventive Services
Many preventive services are covered at no cost to you.
For additional information on these services, click here.
Primary Care Visit
$20
$25
$20 copay after deductible
Specialist Office Visit
$30
$40
15% after deductible
Urgent Care
$40
$40
$40 after deductible
Emergency Services
(Note: physician services may be billed separately)
$200 copay
$200 copay
$200 copay after deductible
Prescription Drug
(SSM Health Pharmacy)
$8/$20/$40 copay
$8/$20/$40 copay
$8/$20/$40 copay after deductible
Prescription Drug
(Other In-Network Retail Pharmacy)
$16/$40/$80 copay
$16/$40/$80 copay
$16/$40/$80 copay after deductible
Medical Plan Contribution Discount
Pharmacy Benefit
Discount recipients have prescription copays
waived for covered prescriptions filled at in-
network pharmacies.
Discount recipients have
prescription copays waived once
the deductible has been met.

10
Medical Plan Secondary Networks: Mid-Missouri and Oklahoma
The Medica/WellFirst Health Network remains the primary provider network for plan members. If your employment is
based in the Mid-Missouri or Oklahoma regions where there is limited access to local SSM Health Primary Network
options for care, you may choose to use providers in a Secondary Network, where higher deductibles, coinsurance,
copays, and out-of-pocket maximums apply. The Secondary Network in Mid-Missouri is available through HealthLink. The
Secondary Network in Oklahoma is available through Health Care Highways. Reminder, you may access SSM Health
Network providers from any region and take advantage of the lower deductibles, coinsurance, copays, and out-
of-pocket maximums available through an SSM Health – Primary Network provider.
Cost-sharing Amounts –
Secondary Network
(Mid-Missouri & Oklahoma)
Medica/WellFirst Plus
Option
Medica/WellFirst Base
Option
Medica/WellFirst Health Savings
Option
Annual Deductible
$700 per person
$1,600 per person
$2,100 employee only
$1,400 per family
$3,200 per family
$4,200 per family
Coinsurance
30%
30%
30%
Deductible/Coinsurance Limit
If you reach this limit, you will only be responsible for copays
until you reach the Out-of-Pocket Maximum.
$4,600 per person
$6,600 per person
$4,600 employee only
$9,200 per family
$13,200 per family
$9,200 per family
Annual Out-of-Pocket Maximum
Copays are applied to this limit. Once you reach the Out-of-
Pocket maximum, you will have no additional out-of-pocket
expenses.
$6,100 per person
$8,100 per person
$6,100 employee only
$12,200 per family
$16,200 per family
$12,200 per family
Preventive Services
Many preventive services are covered at no cost to you. For additional information on these services, click here.
Primary Care Visit
$20
$25
$20 after deductible
Specialist Office Visit
$35
$45
30% after deductible
Urgent Care
$40
$40
$40 after deductible
Emergency Services
(Note: physician services may be billed separately)
$200 copay
$200 copay
$200 copay after deductible
Prescription Drug
(SSM Health Pharmacy)
$8/$20/$40 copay
$8/$20/$40 copay
$8/$20/$40 copay after deductible
Prescription Drug
(Other In-Network Retail Pharmacy)
$16/$40/$80 copay
$16/$40/$80 copay
$16/$40/$80 copay after deductible
Medical Plan Contribution
Discount Pharmacy Benefit
Discount recipients have prescription copays waived
for covered prescriptions filled at in-network
pharmacies.
Discount recipients have
prescription copays waived once
the deductible has been met.
11
Medica/WellFirst Health Savings Option and SSM Health-funded Health Savings Accounts
The Medica/WellFirst Health Savings Option is paired with a Health Savings Account (HSA). If you elect the
Medica/WellFirst Health Savings Option, SSM Health will provide HSA contributions to your HSA on a per pay period
basis. The annual HSA contribution is pro-rated based on the effective date of your coverage in the Medica/WellFirst
Health Savings Option. HSA funds may be used once they are available in your account.
You may contribute additional pre-tax dollars to your HSA account and may change your own HSA contributions at any
time. See page 25 to review important IRS guidelines.
Medica/Health Savings
Option Coverage Level
Annual HSA Contribution Provided by SSM Health
Annual HSA Employee Contribution Limits
Full-Time Employee
Per Pay Period
Annually
Up to Age 55
*Age 55+
Employee Only
$19.23
Up to $500
$3,650
$4,650
Employee + Dependents
$38.46
Up to $1,000
$7,300
$8,300
Part-Time Employee
Per Pay Period
Annually
Up to Age 55
*Age 55+
Employee Only
$9.62
Up to $250
$3,900
$4,900
Employee + Dependents
$19.23
Up to $500
$7,800
$8,800

12
Medical Plan Premiums
SSM Health reviews the cost of the employee health plans and options each year and is committed to ensuring
affordable health care is available. Medical premiums are outlined in the table below with both pre-tax monthly and per
pay period amounts.
IMPORTANT - you may qualify for a Medical Plan Contribution Discount which could provide up to a 25% - 100%
reduction in your medical premiums. To see if you qualify for this discount, please refer to page 18 or click here to view an
informational video.
Note, the premium is deducted each pay period, so the amount shown per pay period is taken out of your paycheck 26
times per year. The amount shown does not include the $69.23 per pay period Spouse/LDA surcharge (if applicable). The
surcharge may be waived if you qualify; review the information on the next page.
Medica/WellFirst Plus Option
Medica/WellFirst Base
Option
Medica/WellFirst Health
Savings Option
Average
Monthly
Per Pay
Period
Average
Monthly
Per Pay
Period
Average
Monthly
Per Pay
Period
Full-Time Employee Premiums (64 – 80 hours per pay period)
Employee Only
$130
$60
$95
$43.85
$95
$43.85
Employee + Child(ren)
$275
$126.92
$205
$94.62
$205
$94.62
Employee + Spouse/LDA
$335
$154.62
$240
$110.77
$240
$110.77
Family
$455
$210
$325
$150
$325
$150
Part-Time Employee Premiums (40 – 63 hours per pay period)
Employee Only
$210
$96.93
$150
$69.23
$150
$69.23
Employee + Child(ren)
$430
$198.46
$320
$147.69
$320
$147.69
Employee + Spouse/LDA
$530
$244.62
$370
$170.77
$370
$170.77
Family
$750
$346.15
$560
$258.46
$560
$258.46

13
Spouse/LDA Surcharge
A $69.23 pre-tax per pay period surcharge will be added to the medical plan for employees who are covering a spouse or
LDA on their medical plan, if that spouse/LDA is eligible for group medical coverage through his/her employer. You are
eligible to waive this surcharge if your spouse/LDA is:
• also employed by SSM Health
• self-employed or unemployed
• retired with no other group health coverage available
• eligible for Medicare/Medicaid/Tricare with no other group
health coverage available
• employed but not eligible for employer-provided medical
coverage or
• employed but medical coverage provided by employer
does not meet ACA affordability standards. Your
spouse/LDA may contact their employer’s human
resources department to verify whether the coverage
provided meets the ACA affordability standard.
Note, you will see the Surcharge Waiver card presented during your enrollment event if you are covering an adult on the
medical plan. If you are NOT electing medical coverage or are NOT covering an adult on your medical plan, you will NOT
be charged the surcharge.
SSM Health Express Virtual Care
SSM Health Express Virtual Care offers online assessment and treatment for a wide range of conditions, from minor
illnesses and injuries to urgent needs. Both Video Visits and E-Visits are available. Click here for more information and to
start a visit.
MyChart
You are encouraged to enroll in MyChart and download the mobile app. MyChart gives you 24/7 access to your health
record and enables you to schedule appointments online, review test results, communicate with your physician and more.
IMPORTANT NOTICE:
You must submit your surcharge waiver, through
Workday, each plan year. No supporting
documentation is required, but the surcharge will
be applied at the beginning of each plan year
unless and until you submit the online waiver.
Refer to the Workday Job Aid for step-by-step
instructions on how to complete and submit the
waiver.
You may submit a Spouse/LDA surcharge waiver
at any time, but the waiver will only apply going
forward and refunds cannot be issued.
Note: You will see the Surcharge Waiver card
presented during your enrollment event,
regardless of your medical plan election. If you
are NOT electing medical coverage or are NOT
covering an adult on your medical plan; you will
NOT be charged the surcharge. While you may
choose to “waive” the surcharge during the
enrollment process, so it appears as “waived” on
your benefits statement, you are not required to
do so. If you are not covering an adult on your
medical plan, you will not be charged the
surcharge, even if you do not act on that card.

14
Medica/WellFirst Health EPO/PPO PRN Plan
In compliance with the Affordable Care Act, SSM Health completes a required analysis (known as the “look back period”)
each year and offers a medical plan to employees who worked the required number of hours, even if they were not
“scheduled” hours. If you are deemed eligible to enroll in the Medica/WellFirst EPO/PPO Health PRN medical plan, you
will be contacted with enrollment instructions. Eligibility for coverage after each plan year will be determined during the
next “look back period”. If you do not work the required hours during the next look back period, you will not be eligible for
this plan for the next stability period. See the plan details and premiums provided below. View the Summary Plan
Description (SPD) at ssmhealth.com/benefits for complete plan and coverage details.
*This plan does not provide Minimum Essential Coverage (MEC), as defined
by the ACA.
Please also note the following:
• Legally Domiciled Adults (LDAs) are not eligible for this plan.
• This plan is not eligible for the Medical Contribution discount.
• The spouse/LDA surcharge does not apply to this plan.
• This offer only applies to the ACA medical plan and no other benefits
are included (e.g., dental, vision, life insurance).
Medica/WellFirst Health EPO/PPO Health PRN
Plan
Cost-Sharing Amounts
Annual Deductible
$5,000 per person/$10,000 per family
(Does not apply to preventative services)
Coinsurance
30% after deductible
Annual Out-of-Pocket Maximum
$8,000 per person/$16,000 per family
Primary Care Visit
30% after deductible
Specialist Office Visit
30% after deductible
Urgent Care
30% after deductible
Emergency Services
30% after deductible
Diagnostic Tests
30% after deductible
Hospital Services
30% after deductible
Prescription Drug
Annual Out-of-Pocket Maximum: $1,850 per person/$3,700 per family
Tier 1 & 2 = 20% of cost, Tier 3 = 40% of cost
Coverage Level
Per Pay Period
Premiums
Employee Only
$253.85
Employee + Spouse
$392.31
Employee + Child(ren)
$489.23
Employee + Family
$692.31

15
Pharmacy Benefits
Pharmacy benefits are included in your medical plan and are accessible at your local SSM Health Pharmacy and
nationwide at most retail pharmacies. See page 17 for a list of SSM Health Pharmacies and visit Navitus.com for a
complete list of other In-Network Retail Pharmacies. Note, while most pharmacies are in the Navitus Network, the
following retailers are not in-network: CVS (including any CVS-owned Target or Schnucks), Kmart, Meijer, and Dierbergs.
You are encouraged to take advantage of the significant discounts that are available through your local SSM Health
Pharmacy. If you are not close to an SSM Health pharmacy, you can use their convenient mail order option. SSM Health
Pharmacies will also be offering a six for $6 dollars program. This program offers you a six (6) month supply of certain
prescriptions for a one-time payment of $6 dollars. For more information about this program and the drugs included, visit
ssmhealth.com/benefits or the Benefits App in Workday.
*Certain specialty prescriptions are covered under the plan only when filled by an SSM Health specialty pharmacy. This program is part of your
pharmacy benefit and is mandatory. Mandatory means your specialty medication must be obtained via an SSM Health specialty pharmacy. Employees
and covered dependents who utilize specialty medications may see savings on their medications through the copay max plus program. Note: this
program does not apply to employees who are enrolled in the Medica/WellFirst Health Savings Plan.
Medica/WellFirst Plus &
Medica/WellFirst Base Option
Medica/WellFirst Health
Savings Option
SSM Health Pharmacy
In-Network Retail Pharmacy
SSM Health
Pharmacy
In-Network
Retail
Pharmacy
30-day supply
90-day supply
30-day supply
90-day supply
Tier 1
Formulary generic and
preferred drug
$8 copay
$20 copay
$16 copay
$40 copay
Copays after Deductible
Tier 2
Formulary brands and
high-cost generics
$20 copay
$50 copay
$40 copay
$100 copay
Copays after Deductible
Tier 3
Non-Formulary brands
and generics*
$40 copay
$100 copay
$80 copay
$200 copay
Copays after Deductible
Mail Order
Service
Mail order can be a convenience for members who take maintenance medications. You may receive up to a 90-day supply
and enjoy significant discounts from an SSM Health pharmacy. Contact your local SSM Health pharmacy to start the
process. COSTCO also offers a mail order service at pharmacy.costco.com. You do not need to be a member of COSTCO
to use the service.

16
Maintenance Medication
Maintenance medication must be filled as a 90-day supply. You may need to contact your provider/prescriber for a 90-day
prescription. Filling your maintenance medication as a 90-day supply helps you save money (as you will only need to pay
2.5 times a regular copay for a 90-day supply), avoid missing doses of your medication, and minimize your trips to the
pharmacy. Note, this requirement does not apply to specialty medications. If you have any questions about if your
maintenance medication is subject to this requirement, call Navitus Customer Care at 866-333-2757. Reminder: Your
local SSM Health Pharmacy provides mail order service for maintenance medications. Save time and money by
exploring this option.
Vaccination Benefit
The following vaccines (COVID-19, Influenza, Tetanus, Pneumonia, MMR, Hepatitis, Varicella, Shingles, Meningitis, and
HPV) are covered under the Pharmacy Benefit and may be obtained directly at the pharmacy for no cost. Visit
Navitus.com to view the comprehensive Pharmacy Directory. SSM Health adult pharmacies also provide the vaccination
service, and you may use the pharmacy vaccination service for your annual SSM Health-required flu shot.

17
Pharmacy Directory
St. Louis
Wisconsin
SSM Health St. Mary’s Hospital – St. Louis
1035 Bellevue Ave.
St. Louis, MO 63117
314-768-8870
SSM Health Pharmacy
1821 S. Stoughton Rd. Suite 300
Madison, WI 53716
608-260-6500
SSM Health Prescription Center
10 Tower Dr. Suite 300
Sun Prairie, WI 53590
608-825-3690
SSM Health Pharmacy Waupun
904 W. Main St.
Waupun, WI 53963
920-324-3010
SSM Health DePaul Hospital – St. Louis
12266 DePaul Dr. Suite 105
Bridgeton, MO 63044
314-344-7300
SSM Health Pharmacy
1211 Fish Hatchery Rd. Suite 300
Madison, WI 53715
608-252-8044
SSM Health Prescription Center
740 Reena Ave., Suite 300
Fort Atkinson, WI 53538
920-568-3515
SSM Health Pharmacy Plus
420 E Division St.
Fond du Lac, WI 54935
920-926-8585
SSM Health Outpatient Center
711 Veterans Memorial Parkway Suite 102
St. Charles, MO 63303
636-669-2223
SSM Health Prescription Center
3200 E. Racine St. Suite 300
Janesville, WI 53546
608-371-8100
SSM Health Pharmacy Main
145 N. Main St.
Fond du Lac, WI 54935
920-926-4660
SSM Health Prescription Center
Health Plaza 421 Camelot Dr.
Fond du Lac, WI 54935
920-926-5455
SSM Health Cardinal Glennon Pharmacy
1465 S Grand Blvd
St. Louis, MO 63104
314-577-5677
SSM Health Prescription Center
752 N. High Point Rd. Suite 300
Madison, WI 53717
608-824-4500
SSM Health Pharmacy West
912 S. Hickory Rd.
Fond du Lac, WI 54935
920-929-7480
SSM Health Pharmacy – Monroe
515 22nd Ave.
Monroe, WI 53566
608-325-3111
SSM Health Pharmacy at SLU Hospital
1225 South Grand Blvd
St. Louis, MO 63104
314-257-3450
SSM Health Prescription Center
700 S Park St., Suite 300
Madison, WI 53715
608-256-6465
SSM Health Pharmacy Markesan
730 N Margaret St.
Markesan, WI 53946
920-398-3261
SSM Health Prescription Center
753 N Main St., Suite 300
Oregon, WI 53575
608-835-7175
SSM Health Prescription Center
2825 Hunters Trail
Portage, WI 53901
608-745-3001
SSM Health Prescription Center
130 Corporate Drive, Suite 300
Beaver Dam, WI 53916
920-885-8510
Mid-Missouri
Oklahoma
Southern Illinois
SSM Health St. Mary’s Hospital – Jefferson City
2505 Mission Dr.
Jefferson City, MO 65109
573-681-3740
SSM Health St. Anthony Hospital – Oklahoma City
608 N.W. 9
th
St., Suite 3200
Oklahoma City, OK 73102
405-815-5655
SSM Health Good Samaritan Hospital – Mt. Vernon
2 Good Samaritan Way #120
Mt. Vernon, IL 62864
618-899-4999

18
Discounted Medical Premiums
At SSM Health, we believe that all people have a right to health care. To help us achieve this vision for optimum health,
we offer a medical plan contribution discount program for employees. This program is offered to improve access to
affordable health care coverage by discounting employee contribution requirements (premiums) and providing additional
pharmacy benefits. Watch this brief informational video to learn more.
How Much Is the Discount?
If you are a full-time employee, you may be eligible for the 25%, 50%, 75%, or 100% discount level. If you are a part-time
employee, you will receive the same dollar amount in discount that a full-time employee receives for the same
election/level of discount.
If you are approved to receive any level of the discount, you will also receive the benefit of no pharmacy copays for
yourself and your covered dependents. Exception: If you elect the Medica/WellFirst Health Savings Option (High
Deductible Health Plan), you will receive waived pharmacy copays once you have met your deductible. The discount
applies to all levels of medical coverage: single, employee plus child(ren), employee plus spouse/LDA or employee +
family. The table below illustrates the discount levels:
How Do You Know if You are Eligible?
Refer to the table on the next page to determine the level of discount for which you may qualify. The discount level is
based on your total income (line 9 of Form 1040) and number (#) of tax exemptions as reported on your 2022
Federal Income Tax Return(s) and as determined by the current Federal Income Guidelines. The current federal income
guidelines may be accessed here and are also shown below. Note, even if your family size or income has since changed,
the 2022 Federal Income Tax Return is the consistent standard used to determine eligibility.
Discount Levels
(A) Household Income less than 100% of the Federal Income Guidelines
100% discount
(B) Household Income > or = 100% but < 200% of the Federal Income Guidelines
75% discount
(C) Household Income > or = 200% but < 300% of the Federal Income Guidelines
50% discount
(D) Household Income > or = 300% but < 400% of the Federal Income Guidelines
25% discount
Note, part-time employees receive the actual dollar amount in discount that a full-time employee receives for that same medical
plan election and level of discount.

19
Household Income and Family Size – 2024 Eligibility Guidelines
When and How Can You Apply for the Discount?
The Medical Plan Contribution Discount must be renewed each year during the annual open enrollment period. Outside of
Open Enrollment, applications may be submitted, through the Workday Request App, within 31 days of becoming eligible
for and enrolling in SSM Health medical coverage – either as a new hire or as the result of a status change or other
qualifying event. For more information about how to apply for this discount, view the program overview and application
guide available at ssmhealth.com/benefits.
How Will You Know if You are Approved for the Discount?
You will receive a Workday notification indicating your application was approved or denied. Check both your work email
and Workday inbox regularly. Note, if you are not approved for the discount or are not approved for the level of discount
you expected, you may use the date of that notification as a “qualifying event” to choose a less expensive medical plan
election.
How Will the Discount be Applied?
Your paycheck will reflect the full medical premium deduction. Beginning with the January 5, 2024, pay date, you will see
a credit in the amount of the discount in the earnings section of your pay slip. The discount is only applied for pay periods
in which you also have a medical contribution (premium) deducted from your pay. To see how the Medical Plan
Contribution Discount may apply to you, please review the example, and use the worksheet provided on the next page.
# in Household
(# of tax exemptions)
(A)
100% of the Federal
Income Guidelines
(B)
200% of the Federal
Income Guidelines
(C)
300% of the Federal
Income Guidelines
(D)
400% of the Federal
Income Guidelines
1
$14,580.00
$29,160.00
$43,740.00
$58,320.00
2
$19,720.00
$39,440.00
$59,160.00
$78,880.00
3
$24,860.00
$49,720.00
$74,580.00
$99,440.00
4
$30,000.00
$60,000.00
$90,000.00
$120,000.00
5
$35,140.00
$70,280.00
$105,420.00
$140,560.00
6
$40,280.00
$80,560.00
$120,840.00
$161,120.00
7
$45,420.00
$90,840.00
$136,260.00
$181,680.00
8
$50,560.00
$101,120.00
$151,680.00
$202,240.00

20
Discounted Medical Premiums – Example & Worksheet
Note, if Eddie were a part-time employee, his per pay period discount would be $157.50, the same dollar amount he
would receive as a full-time employee with the same plan election. The $157.50 would be subtracted from the part-time
premium cost of $346.00 for an actual per pay period premium cost of $188.50.
Medical Plan Contribution Discount Worksheet
Eddie Example
Full-Time Employee
Your Information Here
2022 Family Size
(# of exemptions claimed on your 2022 Federal Tax
Return)
4
2022 Household Income
(Total Income as reported on line 9 of Form 1040)
$40,000
Discount Level
(See charts on page 18 and 19)
Household Income > or =
100% but < 200% of the
Federal Income Guidelines
Medical Plan Election
Family coverage –
Medica/WellFirst Plus Option
Medical Premium Deduction
(Per pay period)
$210.00
% Discount
.75
Discount amount credited on paycheck
(Multiply the medical premium per pay period cost by
the discount %)
$157.50
Actual per pay period premium cost
(Subtract the discount amount from the medical
premium per pay period)
$52.50

21
Dental Plans
SSM Health, in partnership with Delta Dental, provides two dental
plans from which to choose: Dental Plus or Dental Base. You may
use any dentist you choose; however, using an in-network provider
offers additional discounts and enhances the total services you may
receive under the annual maximum benefit. Visit deltadentalmo.com
for information on the provider network. Click here for more
information on how to make the most of your Dental Plan and visit
ssmhealth.com/benefits to access comprehensive dental plan
documents.
Dental Plus
Dental Base
Annual Deductible – you will pay
$50 per person/$150 family
$100 per person/$300 family
Annual Maximum – plan will pay
$2,000 per person
$1,000 per person
Preventive Services –
Deductible does not apply
Routine exam, cleaning, x-rays
100%
100%
Basic Services
80%
50%
Major Services
50%
50%
Orthodontic Services (includes adults)
Note, orthodontic benefits are not available for
services related to “do it yourself” orthodontic kits.
50%
N/A
Lifetime Ortho Maximum - plan will pay
$2,000
N/A
IMPORTANT NOTICE:
If you are not making a change to your level of
coverage for 2024, you may continue to use your
current dental card. If you change your level of
coverage, you will receive a new dental card.
You may always access your card by visiting
deltadentalmo.com.

22
Dental Plan Premiums
Premiums are taken out of your paycheck 26 times per year.
Dental Plus
Dental Base
Average Monthly
Per Pay Period
Average Monthly
Per Pay Period
Full-Time Employee Premiums (64 – 80 hours per pay period)
Employee Only
$15.00
$ 6.92
$7.00
$3.23
Employee + Child(ren)
$40.00
$18.46
$15.75
$7.27
Employee + Spouse/LDA
$35.00
$16.15
$17.50
$8.08
Family
$50.00
$23.08
$26.25
$12.12
Part-Time Employee Premiums (40 – 63 hours per pay period)
Employee Only
$25.00
$11.54
$12.00
$5.54
Employee + Child(ren)
$65.00
$30.00
$24.00
$11.08
Employee + Spouse/LDA
$55.00
$25.38
$30.00
$13.85
Family
$75.00
$34.62
$42.00
$19.38

23
Vision Plans
The Vision Plan can assist with the cost of eye exams, lenses, frames, and contact lenses. The plan is administered by
VSP, a national leading vision plan provider. The plan design includes copays for in-network coverage and
reimbursements (up to plan limits) for out-of-network coverage. Visit vsp.com to access plan details and valuable discount
offers.
Exam and Materials Plan
Exam Only Plan
Note: If you are electing the Medica/WellFirst Plus or Medica/WellFirst Base Medical
Plan, these plans cover an annual eye exam. However, the copay is higher, and the
network of providers is limited. If you elect one of these medical plan options and do
not need lenses or frames, you may want to opt out of the VSP vision plan.
VSP Provider
Out-of-Network Provider
How often each covered
member can use services
Comprehensive Vision Exam
$10 copay
$40 allowance
Once every plan year
Lenses – Glass or Plastic
$25 copay
$40 - $125 allowance
Once every plan year
(if not using the contact lens benefit)
OR
Contact Lenses
$150 allowance + evaluation
and fitting covered + additional
discounts
$105 allowance
($210 allowance if medical
necessity)
Once every plan year
(if not using the glasses lens benefit)
Standard Frames
$190 allowance; $25 copay if
lenses not purchased
$45 allowance
Once every two plan years
VSP Provider
Out-of-Network Provider
How often each covered
member can use services
Comprehensive Vision Exam
$10 copay
$40 allowance
Once every plan year
IMPORTANT NOTICE:
You may print an ID card by
visiting vsp.com. VSP does
not mail ID cards.

24
Vision Plan Premiums
Premiums are taken out of your paycheck 26 times per year.
Exam and Materials
Exam Only
Average Monthly
Per Pay Period
Average Monthly
Per Pay Period
Full and Part-Time Employee Premiums (40 – 80 hours per pay period)
Employee Only
$7.15
$3.30
$3.50
$1.62
Employee + Child(ren)
$13.76
$6.35
$7.75
$3.58
Employee + Spouse/LDA
$12.93
$5.97
$7.25
$3.35
Family
$22.01
$10.16
$12.50
$5.77

25
Pre-Tax Savings
Health Savings Account
A Health Savings Account (HSA) allows you to set aside pre-tax dollars today to
pay for out-of-pocket medical expenses for yourself and your eligible tax
dependents, now and in the future, even if those tax dependents are not covered
on your WellFirst Health Savings medical plan.
IRS guidelines outline eligibility for participating in an HSA. To participate in the
Health Savings Account (HSA), you must meet all the requirements listed below:
• You must be enrolled in the Medica/WellFirst Health Savings Plan (High
Deductible Health Plan)
• You cannot be claimed as a dependent on someone else’s tax return
• You cannot have any other health coverage, including enrollment in another health plan, Medicare, or
military/veteran health benefits.
• You cannot be a recipient of Department of Veteran Affairs (VA) benefits within the past three months, except for
preventive care. If you are a veteran with a disability rating from the VA, this exclusion does not apply.
• You cannot have a foreign address (outside the U.S.)
• If you cover your spouse under the Medica/WellFirst Health Savings Plan, your spouse cannot have a standard
healthcare FSA; he or she may have a limited Healthcare FSA, if available. Note, SSM Health does not offer a
limited purpose FSA.
If you enroll in Medicare or another health plan, make sure to contact People Services and ask to speak to a Benefits
Analyst and/or consult your tax professional. Learn more about HSA eligibility by visiting the Optum Financial website.
Please note that dependents are different for HSAs than they are for medical plans. HSAs define dependents based on
tax status, while the Affordable Care Act (ACA) requires medical plans to cover dependents up to age 26.
Important - there may be tax penalties if you receive HSA contributions when you are not eligible or if you use HSA funds
to pay for an ineligible dependent (even if they are covered on your Medica/WellFirst Health Savings medical plan).
IMPORTANT NOTICE:
If you already have a debit card
from Optum Financial you will
continue to use that card until it
expires. You may request a new
card or additional cards at any
time directly from Optum
Financial.

26
The IRS breaks dependent status for HSA and FSA plans into two categories: qualifying child and qualifying relative.
Note, the definitions below only apply to HSA and FSA plans and may differ from who is eligible to be covered as a
dependent on your health plans. See the plan eligibility guidelines on page 6 for information on covering dependents.
A qualifying child: must bear a certain relationship to the claimant (such as through blood, foster care, adoption, or legal
guardianship), can't turn 19 during the calendar year (or 24 if enrolled in college), must share a primary residence with the
claimant for at least half of the calendar year, and must not provide more than half of their own financial support.
A qualifying relative: must bear a certain relationship to the claimant, must not be a qualifying child of any other person,
must earn less income than the exemption amount ($4,700 for 2023), must receive more than half of their financial
support from the claimant, and must reside with the claimant for the entire year.
Review this brief video for more information and to see if a Health Savings Account is right for you. It is your responsibility
to ensure you are following the IRS guidelines. If you have questions or concerns about these guidelines, please speak
with your financial advisor or contact Optum Financial.
If you elect the WellFirst Health Savings Option, SSM Health will provide per pay period contributions to your HSA. You
may contribute additional pre-tax funds up to the annual IRS limit.
Note, if you do not wish to make your own contributions, set your contribution to $0. If you waive the enrollment, you will
not receive the per pay period contributions from SSM Health.
Important - If you cover your spouse under the Medica/WellFirst Health Savings Plan, your spouse cannot have a
standard Healthcare FSA; he or she may have a limited Healthcare FSA, if available. SSM Health does not offer a limited
purpose FSA.
Medica/WellFirst Health
Savings Option
Coverage Level
Annual HSA Contribution Provided by SSM Health
Annual HSA Employee Contribution Limits
Full-Time Employee
Per Pay Period
Annually
Up to Age 55
*Age 55+
Employee Only
$19.23
Up to $500
$3,650
$4,650
Employee + Dependents
$38.46
Up to $1,000
$7,750
$8,750
Part-Time Employee
Per Pay Period
Annually
Up to Age 55
*Age 55+
Employee Only
$9.62
Up to $250
$3,900
$4,900
Employee + Dependents
$19.23
Up to $500
$7,800
$8,800

27
Flexible Spending Account – Health Care FSA
The Health Care FSA allows you to set aside pre-tax income (minimum of $100; up to $3,050 maximum annual
contribution) to pay for eligible health care expenses that are incurred by you or your dependents and have not been
covered by other plans. Review this brief video for more information and to see if a Health Care FSA is right for you.
You do not have to be enrolled in the Medica/WellFirst Health medical plans to participate in the Health Care FSA;
however, you cannot be enrolled in the Medica/WellFirst Health Savings Option (High Deductible Health Plan). Per IRS
Regulations, the Health Care FSA benefit is not available to participants in the Medica/WellFirst Health Savings Option
who have an HSA.
Important timelines apply to HCFSA funds and are subject to IRS “use it or
lose it” guidelines. Generally, any Health Care FSA funds you contribute in
2024 must be used by December 31, 2024, unless the carry-over provision
applies. Claims that are eligible for reimbursement for the 2024 plan year must
be submitted to Optum by March 31, 2025.
Carry Over - If you enroll in the HCFSA for plan year 2024, you may carry
over up to $570 of your 2023 HCFSA funds. The minimum balance that can
be carried over is $25. Carry over funds from the 2023 plan year will be added
to your 2024 HCFSA approximately 7-10 days after the 2023 plan year has
finalized on March 31, 2024. The maximum carryover amount from 2024 to
2025 will be $610.
If you need help spending your Health Care FSA funds, visit the FSA store available at store.optum.com.
Note, if you have a mid-year change and are no longer actively participating in the HCFSA, your debit card will be
deactivated, and you will have up to 90 days following the date you end your participation in the HCFSA to submit claims
to Optum for eligible expenses that were incurred while your account was active.
Important Notice - per IRS Regulations, the Health Care FSA benefit is not available to participants in the
Medica/WellFirst Health Savings Option who have an HSA.
IMPORTANT NOTICE:
If you already have a debit card from
Optum Financial you will continue to
use that card until it expires. Your
2024 annual contribution will be re-
loaded on your card. You may
request a new card or additional cards
at any time directly from Optum
Financial. If this is your first year in
the Health Care FSA you will receive
a new debit card, pre-loaded with your
annual contribution.

28
Flexible Spending Account – Dependent Daycare FSA
The Dependent Daycare FSA allows you to set aside pre-tax income (minimum of $100; up to $5,000 maximum annual
contribution per household; $2,100 maximum annual contribution for highly compensated individuals) to pay for eligible
child or other dependent daycare expenses. Your children must be under the age of 13 to be considered eligible. Refunds
cannot be issued if you enroll in error. Review this brief video for more information and to see if a Dependent Daycare
FSA is right for you.
Plan elections are reviewed and audited each year to ensure the plan meets the
IRS Nondiscrimination Testing requirements. Because of this, highly
compensated employees may only set aside $2,500 in dependent daycare funds
for plan year 2024. You are a highly compensated employee if your SSM Health
compensation is $150,000 or more.
Participating in the HSA does not impact your ability to participate in the
Dependent Daycare FSA. You may participate in a Dependent Daycare FSA and
the HSA.
Important Notice: FSA funds are subject to IRS guidelines and are “use it or lose
it”. Any Dependent Daycare FSA funds you contribute in 2024 must be used by
December 31, 2024. Claims that are eligible for reimbursement for the 2024
plan year must be submitted by March 31, 2025.
IMPORTANT NOTICE:
You do not receive a debit card for
your Dependent Daycare FSA.
Funds are available in your DCFSA
account on a per pay period basis
and are not pre-loaded like the
HCFSA.
You may submit for reimbursement
as funds are available in your
account by submitting your receipts
to Optum Financial.

29
Retirement Savings Program
Achieve Financial Security for Retirement
SSM Health provides a market-competitive retirement program that is consistent with our Mission, Vision and Values and
is designed to assist you in achieving financial security for your retirement. To learn more about the retirement savings
program, access the Retirement Savings information available at ssmhealth.com/benefits. Manage your account via the
Fidelity Retirement website at netbenefits.com or via the NetBenefits mobile app. You may schedule a one-on-one
appointment with a Fidelity Workplace Financial Consultant at Fidelity.com/schedule.
Basic-Fixed Contribution
SSM Health provides an annual basic/fixed contribution to all employees who qualify. To qualify, you must work a
minimum of 1,000 hours in the payroll year and be actively employed on the last day of the payroll year. You are not
required to make employee contributions to receive the basic/fixed contribution. The employer basic/fixed contribution is
3% of your eligible compensation (up to the annual IRS limit) or a minimum of $1,400, whichever is greater. The $1,400
minimum contribution is pro-rated based on hours worked in the plan year. The annual IRS limit for eligible retirement
compensation was capped at $330,000 for 2023. Limits for 2024 will be published once announced by the IRS.
Match Contribution
Employees who work a minimum of 1,000 hours per payroll year may be eligible for the Employer Match. SSM Health
matches $0.50 on the dollar for the first 6% of employee contributions on a per pay period basis (up to IRS annual limits).
The match is provided on a per pay period basis. You are immediately eligible to receive Employer Matching
Contributions upon your SSM Health employment if the following requirements are met:
• You are a benefit-eligible employee scheduled to work a minimum of 1,000 Hours in the payroll year (40 hours
per pay period) and
• You are contributing to the 403(b) or 401(k) Plan.
If your scheduled hours are under 1,000 Hours in a payroll year, but you complete 1,000 Hours during the payroll year
and are actively employed on the last day of the payroll year, you will receive the Employer Matching Contribution in the
first quarter of the following year after your hours worked have been determined.

30
Match True-Up
If you make uneven contributions to the plan during the payroll year and/or max out your contributions early in the payroll
year, the match true-up enables you to still maximize the match. If you are eligible and are employed on the last day of the
payroll year, the match true-up will be calculated to account for and provide any missing match contributions in the first
quarter of the following year. You might also be eligible for a match true-up if you are on track to complete 1,000 hours,
but your employment ends prior to the end of the payroll year due to death, disability, or severance on or after reaching
age 65.
Important note: the matching funds from SSM Health are provided on a per pay period basis. The maximum amount in matching funds
that may be awarded in 2024 will be subject to IRS limits. To maximize the match, contribute at least 6% of your eligible compensation
to your employee contribution account.
Annual Compensation Limit
Retirement plan compensation limits are defined by the IRS each year. For plan year 2023, the annual IRS limit for
eligible retirement compensation is capped at $330,000. Limits for 2024 will be published once announced by the IRS.
Vesting
Employees are vested in both the basic/fixed and match contributions after three years of eligible service in which the
employee completes 1,000 hours.
Retirement Savings Plans: 403(b) and 401(k)
All employees are eligible to participate. The voluntary 403(b) or 401(k) plans allow you to contribute pre-tax or post-tax
(Roth) dollars to an investment plan administered by Fidelity. There are many investment options from which to choose. If
you are employed by a for-profit SSM Health ministry, you may participate in the 401(k). For plan year 2023, you may
contribute up to $22,500. If you are going to be age 50 or older in the plan year, you may also contribute up to an
additional $7,500 (for a total of $30,000) under the catch-up provision. You may make changes to your 403(b) or 401(k)
account at any time through Fidelity’s netbenefits.com website. Contribution limits for 2024 will be published once
announced by the IRS.
Auto Enrollment and Auto Escalation
To make saving for retirement even easier, newly hired employees are automatically enrolled with a 3% pre-tax
contribution after 30 days of employment with SSM Health. Contributions will be increased by 1% each plan year until the
6% contribution level is reached. You may opt out of auto enrollment/escalation or change your employee contributions at
any time through the Fidelity site at netbenefits.com.

31
Deferred Compensation: 457(b)
Eligible employees (physicians, managers and above) may also contribute to the 457(b) up to the annual IRS limit. For
plan year 2023, up to $22,500 may be contributed. Contribution limits for 2024 will be published once announced by the
IRS. Due to IRS regulations, this plan may only be offered to employees of non-profit ministries. You may enroll in the
457(b) via the Fidelity Retirement website at netbenefits.com.
Defined Benefit (DB) Pension Plan
Effective January 1, 2021, all employees who were Grandparented into the Defined Benefit (DB) Pension Plan moved to
the higher match and basic contribution plan available through the Defined Contribution (DC) Plan. The Defined Benefit
plan was frozen on December 31, 2020. All accrued, vested benefits remain available to employees and may be
accessed based on plan provisions. Pension statements that reflect the estimated final value of the pension benefit were
mailed in early 2021 and are available upon request.
Financial Wellness Resources
Financial wellness is an important step in preparing for your financial future. As an SSM Health employee, you have
access to confidential tools and resources to help you address current financial concerns and improve your financial
wellness. Connect with financial planning resources available through both Fidelity and your Employee Assistance
Program.
Fidelity
Retirement and Financial
Planning Resources
netbenefits.com
800-343-0860
Personal Assistance Services (PAS)
Employee Assistance Program
mypaseap.com
Company code: SSM
800-356-0845
SSM Health at Work
(Employees of Greater Fond Du Lac Ministries)
Employee Assistance Program
SSM Health at Work
800-458-8183
we want to link somewhere else?

32
Paid Time Off (PTO)
Paid Time Off (PTO) includes vacation time, holidays, sick days, personal time, and the elimination period for short-term
disability benefits. PTO is accrued each pay period based on the actual number of hours that you are paid and on eligible
low census hours (up to a maximum of 80 hours per pay period). Note, hours paid by Short-Term Disability are not
eligible for PTO accrual. To be eligible to accrue PTO, you must be regularly scheduled to work at least half-time (40
hours) or more per pay period. “Regularly scheduled” means that you are on file with Human Resources as having a 0.5
full-time equivalent (FTE) or higher status.
Unused PTO carries over from year to year but the maximum amount of PTO that you have in your accrual bank is 1.5
times your annual accrual amount. If you reach your maximum PTO hours, at any point during the year, you will need to
utilize, sell, or donate PTO to accrue additional hours. View the PTO guidelines at ssmhealth.com/benefits.
Note, market-specific PTO programs apply to employees working a 7-on/7-off schedule. The schedules shown below do
not apply to director-level people leaders, executives, and physicians. Executives and physicians should refer to the
applicable Benefits Booklet for information about Paid Time Off. Directors should refer to the next page.
Accrual
Rate
(per hour paid)
Annual
Max
(hours)
Annual Max
(days)
*based on 8-hour days
Overall
Max
(hours)
Overall Max
(days)
*based on 8-hour days
Staff PTO Schedule
Less than 1 year of service – 8 hours loaded on date of hire
.0885
192
24
288
36
More than 1 but fewer than 5 years of service
.0923
192
24
288
36
5 or more but fewer than 10 years of service
.1077
224
28
336
42
10 or more but fewer than 15 years of service
.1192
248
31
372
46.5
15 or more but fewer than 20 years of service
.1269
264
33
396
49.5
20 or more years of service
.1385
288
36
432
54
Management/Advanced Practitioner PTO Schedule
Less than 1 year of service – 8 hours loaded on date of hire
.1153
248
31
372
46.5
More than 1 but fewer than 5 years of service
.1192
248
31
372
46.5
5 or more but fewer than 10 years of service
.1269
264
33
396
49.5
10 or more years of service
.1385
288
36
432
54

33
Director Level PTO
SSM Health utilizes an informal time off model for *director-level, people leaders. Under this approach, time off is taken as
needed. There is no need to record the time away within the timekeeping system or monitor a PTO bank. It is expected
that directors will be prudent under this approach, focusing appropriate attention to their role and leadership
responsibilities. As a general guideline, it is expected that total time taken will not exceed six weeks per year, including
holidays. Director-level PTO does not have cash value, is not eligible for the PTO Sell or PTO Donation programs and
does not pay out upon separation of employment. *If you are in a director-level position that accrues PTO at the
management level, please refer to the schedule on page 32. If you have questions about what PTO program applies to
you, please speak with your leader or open an AskHR case.
PTO Sell
If you are in a position that accrues PTO, you have the option to sell (cash out) a portion of your PTO at any time
throughout the year. The following guidelines apply:
• PTO Sell requests may be submitted up to two times each calendar year from Jan. 1 – Dec. 31
• You may sell up to a maximum of 80 hours each calendar year
• You must maintain a minimum PTO balance of 40 hours after each PTO Sell
• Per the IRS guidelines, PTO Sell hours are paid at 85% of the full value and are taxed at the supplemental rate
• PTO hours are paid at the base rate of pay for the primary job you hold
PTO Sell requests are submitted through the Absence App in Workday. Both the browser/desktop version and the mobile
app may be used to submit your request. The timing of the request will impact when the hours will be paid out. Note:
Directors, Executives and Physicians are not eligible for PTO Sell.
PTO Donation/PTO Emergency
If you are in a position that accrues PTO, you may donate up to 80 hours of PTO to a medical emergency leave bank on
an annual basis. You may “recommend” the recipient but may not make the donation contingent on the time going to the
desired recipient. PTO hours may be donated through the Request App in Workday.
If you are in a position that accrues PTO and you experience an emergency that meets the IRS-defined requirements, you
may request hours from the medical emergency leave bank by submitting an application through the Request App in
Workday. Up to 160 hours may be awarded annually. View the PTO guidelines at ssmhealth.com/benefits for additional
information. Note: Directors, Executives and Physicians are not eligible for the PTO Donation/PTO Emergency program.
PTO Hardship
If you are in a position that accrues PTO, you may request a payout from your PTO bank if you experience a serious
financial hardship. The payout is limited to the amount of the hardship or half your PTO balance at the time of the request
(whichever is lower) up to a maximum of 80 hours per calendar year. PTO hours are paid at the base rate for your primary

34
job held and are paid at 85% of full value. The hardship must meet the IRS eligibility requirements. You may request PTO
Hardship through the Request App in Workday. View the PTO guidelines at ssmhealth.com/benefits for additional
information. Note: Directors, Executives and Physicians are not eligible for the PTO Donation/PTO Emergency program.
Bereavement Leave
You may take up to three scheduled shifts with pay in the event of the death of a family member; up to five scheduled
shifts with pay are provided if the loss is a spouse or child/stepchild. View the bereavement leave guidelines at
ssmhealth.com/benefits.
Paid Parental Leave
One week paid parental leave is available to you if you are in a benefit eligible position and have completed at least 90
days of employment with SSM Health. The leave, which is intended to cover bonding time, provides 40 hours of paid
leave (pro-rated based on FTE), includes adoptions, and compliments maternity leave for the birth parent. View the PTO
Guidelines at ssmhealth.com/benefits for additional information.
Short-Term Disability
As a benefit eligible employee, you are covered by a Short-Term Disability (STD) plan that replaces 60% of your income
when you are medically unable to work due to a serious health condition. The first week (seven calendar days) of
disability is an elimination period during which disability benefits are not paid. You will use PTO to satisfy the elimination
period while you are medically unable to work before STD benefits begin (unless taking unpaid WI FMLA).
Following the elimination period, you may be eligible to receive a benefit. The 60% Short-Term Disability coverage is
provided by SSM Health at no premium cost to you (with minimum weekly benefits). You have the option to “buy up” to a
75% STD plan. You will see the cost of the buy-up option when you go through the enrollment process. You may enroll in
the buy-up option during the annual open enrollment period or within 31 days of becoming benefit eligible either as a new
hire or through a qualifying work/life event.
Note, once short-term disability payments begin, you may not use PTO. Once short-term disability payments end, you
may begin using your PTO if you need additional time away from work.
Employees who transitioned into the STD benefit from former illness banks or salary continuation receive an automatic
buy-up to 75%. The 75% Short-Term Disability coverage is provided by SSM Health at no cost, based on their former
illness bank balance at 2019 year-end.

35
If you were part of an acquisition that occurred after January 1, 2020, your automatic “buy up” date may differ than what is
shown above but is still based on a 3, 5, or 7-year benefit schedule. If you are not sure if you are covered by the
automatic “buy up”, create an AskHR case and a Benefits Analyst will assist you.
Maternity Benefits
If you are accessing Short-Term Disability due to maternity leave, 100% of your income will be replaced for up to six
weeks for a routine delivery or up to eight weeks for a c-section. The first week (seven calendar days) elimination period
still applies. The 100% maternity leave coverage is provided by SSM Health with no premium cost to you.
Living Donor Benefits
If you are accessing Short-Term Disability to serve as a living donor, 100% of your income will be replaced for up to six
weeks with no benefit maximum. The first week (seven calendar days) elimination period is waived. The 100% living
donor benefit is provided by SSM Health with no premium cost to you. The living organ donations that qualify for this
benefit include kidney, liver, and bone marrow.
Long-Term Disability
After 90 days of being medically unable to work, you are eligible to apply to receive a Long-Term Disability benefit of 60%
of your salary up to a maximum of $10,000 per month. The 60% Long-Term Disability coverage is provided by SSM
Health with no premium cost to you. Executives and physicians should refer to the applicable benefit booklet for LTD
information. Note: You must exhaust all PTO before LTD payments begin.
For more information about the Short and Long-Term Disability plans, including Maternity Benefits and Paid Parental
Leave, review the Leave of Absence Resource Guide available in the Benefits App in Workday.
Important note for Directors with the Flexible Time Off Model.
Directors with the Flexible Time Off Model will be provided up to six (6) weeks of paid time off in a rolling calendar year.
The six weeks will be applicable to the seven-calendar day elimination period associated with a Short-Term Disability
claim and leaves with no associated benefit pay. Leave time in excess of the allowed six weeks will be unpaid.
Balance as of December 2019
Automatic “buy up” provided through the last
payroll occurring in
25-49% of maximum
December 2022 (3 years)
50-74% of maximum
December 2024 (5 years)
75%+ of maximum
December 2026 (7 years)

36
Life Insurance
SSM Health offers both employer-paid and voluntary life insurance to provide financial security should the unexpected
occur. For more information about life insurance, visit ssmhealth.com/benefits. The life insurance benefits outlined below
apply to both full and part-time benefit employees. Note, per industry standards, employee and spouse life insurance and AD&D
are subject to benefit reduction based on age. The benefit reduces to 65% at age 65 and to 50% at age 70.
Employer-Paid Life Insurance Coverage
General Guidelines
Staff
1X pay up to $500,000
While SSM Health pays for the cost of this basic life policy, per federal regulations,
employees must pay tax on the imputed income for the “value” of any employer-
provided life insurance that exceeds $50,000. Click here to view the IRS guidelines. If
you do not want to pay tax on this imputed income, you may waive the basic life
insurance during enrollment. If you waive your Basic Life and then later choose to enroll
in Basic Life, you will be subject to Evidence of Insurability. Please note: If you choose
to opt out of Basic Life and you do not purchase Voluntary Employee Life, you cannot
elect Dependent or Spouse Life.
Manager and above,
including Advanced
Practitioners
2X pay up to $1M
Employer-Paid Accidental Death &
Dismemberment Insurance (AD&D)
General Guidelines
Staff
1X pay up to $500,000
Accidental Death and Dismemberment (AD&D) Insurance is not subject to imputed
income tax and therefore, may not be waived.
Manager and above,
including Advanced
Practitioners
2X pay up to $1M
Employee-Paid Optional Insurance (Life and
AD&D)
Guaranteed Issue and Evidence of Insurability (EOI)
Note: EOI only applies to Life Insurance; AD&D is guaranteed issue.
Staff
Multiples of pay up to
8X, capped at $2M for
life insurance; Multiples
of pay up to 8X, capped
at $1M for AD&D.
Newly eligible: May elect up to the lesser of 3x annual salary or $1M without Evidence
of Insurability (EOI). During Open Enrollment: If currently enrolled, may increase
coverage 1x up to the lesser of 3x annual salary or $1M; If not currently enrolled, any
election requires Evidence of Insurability (EOI). Securian will contact you, via email, to
complete the Evidence of Insurability (EOI) process. If you do not complete the process
your request to purchase life insurance above the guaranteed issue amount will be
cancelled and/or denied. You will not be charged for any additional life insurance
premiums, above the guaranteed issue amount, until your Evidence of Insurability is
confirmed by Securian.
Manager and above,
including Advanced
Practitioners

37
Dependent Life Insurance
Guaranteed Issue and Evidence of Insurability (EOI)
Spouse
*LDA’s are not eligible
to be covered on
dependent life.
Increments of $25,000
up to $250,000
Newly eligible: May elect up to $50,000 without Evidence of Insurability (EOI).
During Open Enrollment: Any increase in coverage requires Evidence of Insurability
(EOI). Securian will mail your spouse an Evidence of Insurability (EOI) packet.
If you do not complete the process, your request to purchase life insurance above the
guaranteed issue amount will be cancelled and/or denied. You will not be charged for
any additional life insurance premiums, above the guaranteed issue amount, until your
Evidence of Insurability is confirmed by Securian.
Eligible Child
Increments of $5,000 up
to $25,000
All coverage is guaranteed issue – no EOI required.
Dependent AD&D
Guaranteed Issue and Evidence of Insurability (EOI)
Spouse
*LDA’s are not eligible
to be covered on
dependent life.
Increments of $25,000
up to $100,000
All coverage is guaranteed issue – no EOI required.
Eligible Child
$10,000 or $25,000
Benefit Scout
Access Benefit Scout at lifebenefits.com/ssm2 to access a one-stop shop for life insurance benefits information and
coverage guidance tools.
Additional Lifestyle Benefits
Additional services are automatically offered to those enrolled in Life Insurance; there is no additional cost for these
benefits.
Travel Assistance
If you are planning to travel 100 miles or more from home, access pre-trip planning and emergency services through
RedpointWTP. Learn more at: LifeBenefits.com/travel
Life Insurance-related Financial and Grief Resources
For confidential advice and support, including free will preparation services, contact Securian’s LifeWorks at (877) 849-
6034. Learn more at lifebenefits.com/lfg, username: lfg and password: resources.

38
Professional Development
At SSM Health, we invest in your personal and professional growth and development. Review the programs below to find
educational options that best align with your goals and interests. Comprehensive program information and policies are
available at ssmhealth.com/benefits.
Tuition Benefits
Tuition Reimbursement Program
Tuition Reimbursement helps cover the cost of tuition for both job-related degree programs, cohort programs and certain
specialty certification programs. Full-time employees are eligible for up to $4,200 annually and part-time employees are
eligible for up to $2,100 annually. You are eligible for tuition benefits after 90 days of employment. Learn more about
Tuition Reimbursement through the Benefits App in Workday or at ssmhealth.com/benefits.
Tuition Discounts and Cohort Programs
SSM Health has also established tuition discounts and cohort programs with a variety of universities. These programs
offer a reduced tuition rate with the goal of providing affordable continuing and higher education for our workforce. To
learn more about the specific tuition discount agreements or cohort programs offered to SSM Health employees visit SSM
Health Tuition Discount Program.
Announcing FlexPath Funded
In addition to traditional tuition reimbursement, a new educational offering known as FlexPath Funded will provide up to
$5,250 each year in upfront tuition benefits. Eligible employees may use FlexPath funds for coursework towards a degree
from select online universities or toward online skills-based courses in a wide variety of areas and interests. Eligibility
guidelines apply. Watch for information about this exciting new program that will be shared in the coming weeks and
months.
Note, the traditional tuition reimbursement and FlexPath Funded programs cannot be used in the same calendar year.
MyLearning: Continuing Education
On-demand, self-guided virtual offerings that provide continuing education credit. A variety of clinically focused topics,
along with leadership and professional development options for non-clinicians are offered. Open the MyLearning App in
Workday to access the courses.

39
Manager’s Toolkit
Tools and resources for leaders are available through the Leaders Tool App in Workday. On demand, self-guided virtual
offerings available on a wide variety of management topics.
SLUCare Faculty Tuition Remission
Employees of SLUCare Physician Group who hold SLU Faculty positions are also eligible for SLU’s tuition remission
benefits. SLU tuition remission plan guidelines apply and there may be tax implications. Visit the SLU Tuition Benefits
site for more information or contact benefits@slu.edu if you have questions. Note: while you have access to both SSM
Health and SLU tuition benefits, any SLU Tuition remission benefits used in a calendar year will also apply to the
maximum Tuition Reimbursement or FlexPath Funded benefits you would be eligible to receive from SSM Health in that
same calendar year.

40
Additional Benefits
Adoption Assistance
The Adoption Assistance program can reimburse you for normal agency fees and legal fees incurred for the adoption of a
minor child, up to the maximum amount allowed per adoption. To be eligible, you must have completed at least six (6)
months of employment and apply for reimbursement within 60 days of the finalization date. For more information, view
the Adoption Assistance program guidelines available at ssmhealth.com/benefits.
DailyPay
SSM Health now partners with DailyPay to provide on-demand access to your earned pay. Learn more about and/or
enroll in DailyPay at dailypay.com/employee. Note, Physicians and Executives are not eligible to participate.
Purchasing Power
To ease the burden that unexpected household expenses can cause, SSM Health has partnered with Purchasing
Power. While paying with cash is always the best option, when cash is not available, Purchasing Power offers an easy
way to get products you need now with the option to pay for them directly through your paycheck over time. No credit
checks are required. To be eligible, you must have annual earnings of at least $20,000 and be an active, benefit-eligible
employee who has completed at least 90 days of service. Open the Benefits App in Workday and select Purchasing
Power or visit ssmhealth.purchasingpower.com to learn more. Note, this is not a discount program, but may help you
avoid costly payday loans and/or rent-to-own options. Note, payroll deductions for Purchasing Power payments will be
listed as BenefitsPlus Voluntary on your payslip.
Employee Assistance Program
A free, confidential counseling and referral service designed to assist both you and your immediate family. The Employee
Assistance Program (EAP) can provide resources on health, finances, retirement planning, childcare planning, family
issues and much more. EAP services are provided by Personal Assistance Services (PAS). You may reach them at:
mypaseap.com (company code: SSM) or 800-356-0845. Note, if you are employed by a Greater Fond du Lac ministry,
you will use the SSM Health at Work EAP. You may reach them at 800-458-8183.

41
Benefits Plus
Benefits Plus provides exclusive employee rates on a variety of programs. Premiums for these specially negotiated plans
are paid through payroll deduction, making it safe, easy, and convenient for your budget.
Benefit
Description
How to Enroll
Accident Insurance
Accident insurance helps you pay for the medical and out-of- pocket
costs that you may incur after an accidental injury.
View coverage options and
enroll in Workday during
Open Enrollment or within
31 days of a qualifying
work/life event.
Critical Illness
Critical illness insurance provides additional coverage for medical
emergencies like heart attack, stroke, or cancer.
Hospitalization
Hospital indemnity insurance helps offset hospitalization expenses that
may not be covered under your medical plan.
Legal Services
MetLife Legal Plans provides access to attorneys for many common legal
issues. The Family Care
Identity Theft Protection
LifeLock provides an all-in-one membership for your Cyber Safety.
Enroll at any time through
the Benefits Plus portal.
Auto and Home
Insurance
Streamline shopping for auto and home insurance; get real-time, side by
side rate quotes so you can find the policy that works best for your needs
and budget.
Pet Insurance
There are two plans from which to choose. A traditional insurance plan
offered through Nationwide and a discount program offered through Pet
Benefit Solutions.
Purchasing Power
A purchasing program that enables eligible employees to purchase goods
through the convenience of payroll deduction. Payments will be listed as
Benefits Plus Voluntary on your pay slip.
Visit Purchasing Power for
more information.
Discount Shopping
(FREE)
Find great deals on electronics, travel, entertainment, clothes, gifts and
more in one convenient location.
Access at any time
through the Benefits Plus
portal.

42
Wellness Resources
We know that many of you are looking for easy, attainable ways to live your healthiest life. To support you in that goal, we
are excited to introduce myhealthylife, the SSM Health Employee Wellness Program. Beginning in 2024, you will have
access to the resources and tools you need to improve your well-being and will be encouraged to participate in fun,
rewarding personal challenges that promote self-care. Through the Sharecare app, you can make small steps that lead to
big changes in your everyday life. Watch for program details that will be shared later in 2023. You may also access
current well-being resources through the Well-Being App in Workday.
Via Benefits
Via Benefits provides no-cost professional assistance in finding health insurance coverage. Comparison tools make it
simple to evaluate plans, and licensed benefit advisors are available to help explore coverage options. Via Benefits is not
an insurance carrier but is a service offering guidance and access to a wide selection of Medicare and Individual and
Family Plans. Because of the partnership with SSM Health, complimentary services are provided free of charge to SSM
Health employees. Via Benefits offers the following services that may be accessed year-round:
• Personalized assistance with professional benefit advisors
• Support for an annual health care coverage checkup
• Decision support tools and information available online 24/7 including
Are you retiring and have questions about Medicare?
Visit https://my.viabenefits.com/SSMHealth, or contact customer support at (833) 414-1435.
Are you going to be COBRA-eligible (i.e. moving to a non-benefit eligible status or separating employment)?
Visit https://marketplace.viabenefits.com/SSMHealth or contact customer support at (833) 414-1436.

43
Required Notices
Uniform Glossary
The Summary of Benefits and Coverage (SBC) final regulations require group health plans and health insurance issuers
to provide the Uniform Glossary in a common format and use terminology that is understandable by the average plan
enrollee or individual covered under an individual policy.
How to Access the Uniform Glossary
The Uniform Glossary may be reviewed and obtained at the following websites:
• The Center for Consumer Information & Insurance Oversight (CCIIO) at cciio.cms.gov
• U.S. Department of Labor at dol.gov/ebsa/healthreform and healthcare.gov
• Paper copies of the Uniform Glossary are also available upon request.
Written Translation of the Uniform Glossary
Plans and issuers are also required to provide notices in a culturally and linguistically appropriate manner. This includes
providing access to written translation of the Uniform Glossary in Spanish, Tagalog, Chinese and Navajo for certain
geographic areas.
HHS will provide written translation of the Uniform Glossary in the above listed languages at the following websites:
cciio.cms.gov and dol.gov/ebsa/healthreform
Health Insurance Marketplace Coverage Options
To assist you as you evaluate options for you and your family, this notice provides some basic information about the
Marketplace available at healthcare.gov and employment based health coverage offered by your employer.
Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP)
If you or your children are eligible for Medicaid or CHIP and you are eligible for health coverage from your employer, your
state may have a premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP
programs. If you or your children aren’t eligible for Medicaid or CHIP, you won’t be eligible for these premium assistance
programs, but you may be able to buy individual insurance coverage through the Health Insurance Marketplace. For more
information, visit healthcare.gov. View information about the Children’s Health Insurance Program (CHIP) here.
