
Environmental Infection Prevention:
Guidance for Continuously Maintaining a
Safe Patient Care and Survey-Ready Environment
A Guide by Joint Commission Resources
Sponsored by

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
DISCLAIMER
is guide was supported in part by funding from NexClean. All content in this guide was created and
controlled only by Joint Commission Resources (JCR). You are solely responsible for any decision to use
the guide for assisting your health care organization. It is only a guide, and you have to decide whether
it needs to be tailored to t the practices and settings at your organization. JCR’s provision of this guide,
as funded by NexClean, is on a non-exclusive basis, and is not an endorsement of that company or its
products or services; it is also not a statement that NexClean’s expertise or products or services are superior
to those of other comparable companies. JCR, as a matter of policy, does not endorse products or services.
JCR may make available all the subject matter in this guide to any other party interested in furthering
JCR’s eorts to improve quality and safety.
JOINT COMMISSION RESOURCES MISSION
e mission of Joint Commission Resources (JCR) is to continuously improve the safety and quality of
health care in the United States and in the international community through the provision of education,
publications, consultation, and evaluation services.
© 2018 Joint Commission Resources. All rights reserved. is guide may not be reproduced in any form or
by any means without written permission from JCR. Send requests to make copies of any part of this work
Joint Commission Resources, Inc. (JCR), a not-for-prot aliate of e Joint Commission, has been
designated by e Joint Commission to publish publications and multimedia products. JCR reproduces
and distributes these materials under license from e Joint Commission.
Printed in the USA 5 4 3 2 1
For more information about JCR, please visit http://www.jcrinc.com.

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com3
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
H
ealth care-associated infections (HAIs) remain a
major cause of patient morbidity and mortality in the
United States, with approximately one out of every 20
hospitalized patients developing an HAI. Although con-
tamination of the patient care environment by microor-
ganisms has long been recognized as a potential con-
tributor to infection transmission, only in recent years has
the significance of environmental contamination been
fully realized. Environmental surfaces such as counter-
tops, sinks, curtains, bedrails, bedside tables, and nurse
call controls can serve as reservoirs for microorganisms
that then may be transmitted to patients or health care
workers when environmental cleaning and disinfection
are inadequate. According to the Centers for Disease
Control and Prevention (CDC), eective and consistent
cleaning and disinfection of the environment in health
care facilities are essential in reducing the incidence of
HAIs.
E.H. Spaulding developed a classification scheme in 1968
to classify items to be disinfected or sterilized based on their
degrees of risk of infection to patients. Hospitals still use
this scheme to guide disinfection and sterilization activ-
ities. The Spaulding system categories are as follows:
1. Critical. Critical items are objects that enter or come
into contact with sterile tissues or the vascular sys-
tem and that have a high risk of transmitting infection.
These include such items as surgical instruments,
cardiac and vascular catheters implants, and objects
placed into the vascular system, such as needles.
Critical patient care items are reprocessed to make
them sterile; that is, all microorganisms, including bac-
terial spores, are killed.
2. Semi-critical. Semi-critical items include those that
come into contact with nonintact skin or mucous mem-
branes, such as respiratory therapy equipment, anes-
thesia equipment, and flexible endoscopes. These
items are processed with high-level disinfection to
eliminate all microorganisms—except for high num-
bers of bacterial spores.
3. Noncritical. Noncritical patient items touch intact skin
only. Because the skin acts as an eective barrier to
most microorganisms, these items pose a low risk
of transmitting infections. Noncritical items include
crutches, blood pressure cus, stethoscopes, and a
variety of other medical accessories as well as non-
medical accessories, such as recreational equipment.
Noncritical items are processed with low- or interme-
diate-level disinfection processes.
See Tool 1 on page 7 for a sample schedule for cleaning
and disinfecting various equipment based on Spaulding
system categories.
This document provides 1) essential elements for eective
environmental infection prevention, and 2) tools for ongo-
ing assessment of environmental infection prevention
practices in health care facilities for noncritical items and
those surfaces that undergo low-level disinfection by unit/
department sta or environmental services sta. Guidance
for high-level disinfection and sterilization can be found in
the High-Level Disinfection and Sterilization Boosterpak
from The Joint Commission, available at https://www.joint-
commission.org/assets/1/6/TJC_HLD_BoosterPak.pdf.
Essential Elements for Environmental
Infection Prevention
While there are various ways to validate the eective-
ness of environmental cleaning and disinfection, all have
demonstrated significant deficiencies in routine cleaning
and disinfection of patient rooms and medical equipment,
with as many as 50% of surfaces still with pathogens pres-
ent after terminal cleaning.
Environmental contamination prevention strategies pri-
marily fall into four categories:
1. Equipment and disinfectant selection
Environmental Infection Prevention:
Guidance for Continuously Maintaining a
Safe Patient Care and Survey-Ready Environment

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com4
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
2. Preventive maintenance and deep cleaning
3. Adherence to proven methods of cleaning and
disinfection
4. Automated disinfection technologies
Equipment and Disinfectant Selection
Equipment and disinfectant selection is key to eec-
tively preventing infections in the environment. A multi-
disciplinary team rather than individual units or depart-
ments should do equipment and disinfectant selection.
Team members should include infection preventionists,
hospital leaders, housekeeping sta, clinical sta, and
other environment of care professionals. Review man-
ufacturers’ instructions and relevant national guidelines
before purchasing equipment so that you are confident
that the equipment can be properly disinfected and will
not pose a patient or health care worker safety risk. Here
are some considerations when purchasing equipment
and disinfectants:
• Can the equipment be cleaned and disinfected
with a chemical already approved for use in
your organization? Or does the equipment require
introduction of and education on a new chemical?
• Are all surfaces of the equipment able to be
disinfected? For example, are there minimal crevices?
And what about upholstery or wood, which are harder
to disinfect eectively?
• Does the equipment have components that may rust
or deteriorate with repeated cleaning and disinfection?
• For upholstery, can the fabric be disinfected? Maybe
consider vinyl instead of cloth. Does furniture have
open arms to minimize crevices for bed bugs?
• Can flooring surfaces be routinely and easily cleaned
and disinfected? For example, consider a hard
surface instead of carpet.
• When selecting disinfectants, consider the following:
– Equipment compatibility. Try to minimize
the number of disinfectants that are needed.
Preparing a grid listing all equipment and their
disinfectant compatibilities may be helpful in
choosing disinfectants to purchase. Ideally, limit
number of disinfectants stocked to two or three.
(See Tool 2 on page 8 for a sample equipment and
disinfectant compatibility grid.)
– Wet contact time. Try to choose disinfectants
with the shortest wet contact time to aid in sta
compliance.
– Antimicrobial activity. Evaluate what
organisms against which the disinfectant is
eective.
– Choose disinfectants with the lowest possible
risk to sta while still considering the other criteria
listed above.
Preventive Maintenance and Deep
Cleaning
Once equipment has been selected, it must be main-
tained 1) to prevent or reduce the burden of environ-
mental contamination that occurs during use, and 2) to
ensure that the surfaces can be properly cleaned and
disinfected. Routinely assessing surfaces for the follow-
ing can help reduce the burden of contamination:
• Remove tape or other adhesive residue.
• Address surface rust.
• Ensure that Velcro®, if present, is in good condition.
(Minimize Velcro® whenever possible.)
• Ensure that there are no cracks or chips in laminate on
furniture, countertops, and cabinetry.
• Avoid tears or holes in upholstery or mattresses. Patch
any holes or tears with an approved product that can
be cleaned and disinfected (that is, no tape).
• Maintain casters, wheels, tracks, and so forth on
equipment so they function properly and do not build
up debris, dust, or other matter.
• Unclog drains, and routinely remove hard water and
mineral deposits from ice machines, water dispensers,
and any other equipment with water present.
• Ensure that decorative water features, if present, have
correct chemical levels to prevent bacterial growth.
• Properly store equipment and supplies in clean
locations (for example, cabinets, covered linens,
storage rooms, and plastic covers if required by the
organizational policy).
• Routinely clean air vents and change filters per
manufacturers’ instructions.
Cleaning is the removal of foreign material (for exam-
ple, soil, organic material) from objects and is normally
accomplished using water with detergents or enzymatic
products. Thorough cleaning is required before high-
level disinfection and sterilization because inorganic
and organic materials that remain on surfaces interfere

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com5
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
with the eectiveness of disinfection. While most orga-
nizations have some sort of routine cleaning schedule
for equipment and surfaces, deep cleaning is often not
performed due to operational issues, for example, rooms
being occupied, lack of back-up equipment, or stang.
Developing and maintaining a deep cleaning process
may contribute to more ecient routine cleaning and
will result in more eective disinfection processes. Items
that may be considered for a deep cleaning schedule
include the following:
• Air ducts and grills
• Ice dispensers and storage chests
• Carpeting
• Window blinds and shades
• Privacy curtains
• Clothing washers and dryers
• Mattress and pillow covers
• Beds and bed frames
• Other room furniture and furnishings
Adherence to Proven Methods of Cleaning
and Disinfection
Environmental cleaning interventions can improve the
thoroughness of cleaning and reduce contamination on
surfaces. Interventions have ranged from substituting
one disinfectant for another, such as using hypochlo-
rite for disinfecting rooms of patients with Clostridium
dicile infection, to environmental education programs
with feedback and monitoring. While many studies
have shown a decrease in environmental contamina-
tion, a decrease in HAI rates, and in some cases, an
elimination of an outbreak, it is still unclear which inter-
ventions were most eective because there are very
few well-controlled studies. The organization must
maintain a thorough knowledge of and adherence to
the manufacturers’ instructions for cleaning and disin-
fecting all equipment. Additional studies are needed to
determine optimal frequency of disinfection (terminal,
daily, or more frequent), prioritization of special disin-
fection procedures (high risk units or entire facility), and
the role or added benefit for automated devices such
as ultraviolet light, particularly when standard clean-
ing and disinfection methods have been optimized and
validated.
Strategies to assist with adherence to proven cleaning
and disinfection methods include the following:
• Ensure that sta are educated to their role in
cleaning and disinfection, including
– What cleaner/disinfectant to use on what
equipment
– How to properly apply or use the cleaners/
disinfectants provided by the organization (that is,
wet contact times)
– Who is responsible for disinfecting various
equipment (for example, environmental services,
department/unit sta)
– Frequency in which to disinfect various types
of equipment and surfaces
• Ensure that departments can order only approved
cleaners/disinfectants
Automated Disinfection Technologies
Recent technologies for reducing the burden of patho-
gens on surfaces include antimicrobial surfaces, ultra-
violet light disinfection, deep cleaning/disinfection with
steam or vaporized hydrogen peroxide, and other tech-
nologies. While current studies show reduction in surface
contamination, studies demonstrating corresponding
reduction in HAIs are limited. Organizations may want to
evaluate these technologies for use in addition to exist-
ing proven environmental infection prevention strate-
gies. If using these technologies, organizations should
do the following:
• Ensure that manual cleaning and disinfection are done
prior to use.
• Develop priorities for the use of these technologies
(for example, critical care units, operating rooms,
oncology wards.
• Determine frequency of use of these technologies that
is operationally feasible (for example, at discharge,
end of each day in operating rooms, weekly, monthly.
See Tool 3 on page 9 for an Environmental Infection
Prevention Assessment that you can use to assess your
organization’s practices against Joint Commission stan-
dards for infection prevention and control as they relate
to the environment of care.

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com6
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
REFERENCES
1. Weber, D, Anderson, D, Rutala, W. “The role of the surface
environment in healthcare-associated infections.” August 2013.
www.co-infectiousdiseases.com Accessed January 2018.
2. Rutala W.A., Weber D.J., and the Healthcare Infection Control
Practices Advisory Committee: Guideline for Disinfection and Ster-
ilization in Healthcare Facilities, 2008. www.cdc.gov/hicpac/pdf/
guidelines/Disinfection_Nov_20 08.pdf. Accessed January 2018.
3. Spaulding E.H.: Chemical disinfection of medical and surgical ma-
terials. In Lawrence C.A., Block S.S. (eds.): Disinfection, Sterilization
and Preservation. Philadelphia: Lea & Febiger, 1968, pp. 517–531.
4. Donskey, C. (2013). Does improving surface cleaning and disin-
fection reduce health care-associated infections? American Jour-
nal of Infection Control 41, S12-S19.
5. Centers for Disease Control and Prevention. Guideline for En-
vironmental Infection Control in Health Care Facilities, 2003.
https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmen-
tal-guidelines.pdf. Accessed March 2018.

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com7
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
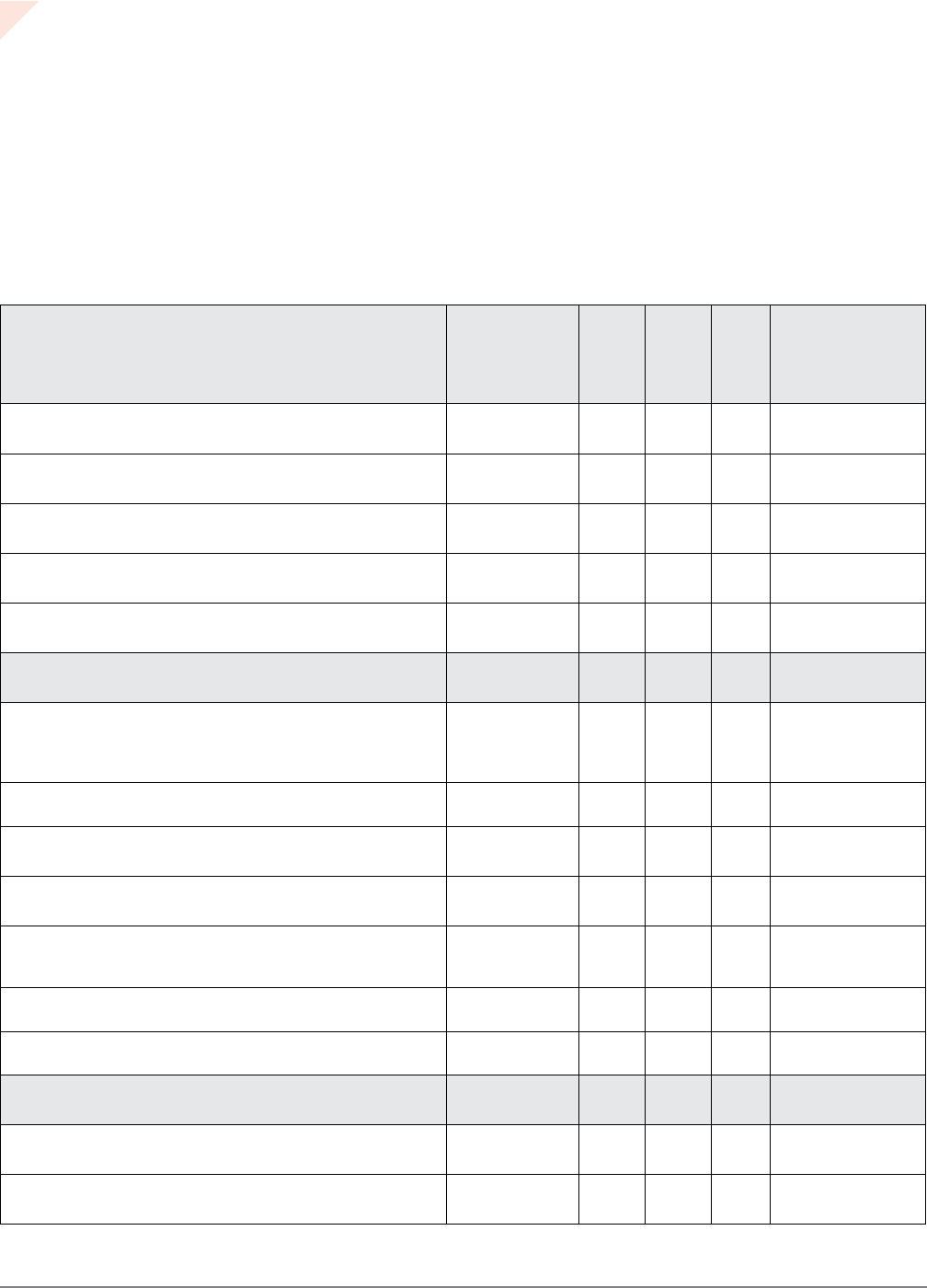
Equipment Spaulding
Classification
Clearning/
Disinfection
Frequency
Person/
Department
responsible
Approved
Disinfectant/
Cleaner
Example: Intravenous pump Non-critical
Daily, when visibly soiled and
between patients
Environmental Services Facility-approved
disinfectant (list
brand name of
disinfectant)
Example: Microwave oven Non-critical
Daily
Food and Nutrition
Services
Facility-approved
bleach disinfectant
Example: Wheelchair Non-critical
Daily and when visibly soiled
Unit sta Facility-approved
disinfectant
Example: Ice and water
dispenser
Non-critical
Daily and when visibly soiled
Food and Nutrition
Services
Facility-approved
bleach disinfectant
Example: Thermometer Non-critical
Between each patient use
Unit sta Facility-approved
disinfectant
Example: Glucometer Non-critical
Between each patient use
Unit sta Facility-approved
disinfectant
Example: Bronchoscope Semi-critical
Between each patient use
Pre-clean at point of use
by unit sta, high-level
disinfection by facility-
determined department
(for example, Sterile
Processing)
Facility- and
manufacturer-
approved high-level
disinfectant or
sterilant
Example: Mattress Non-critical
Between each patient, when
visibly soiled
Environmental Services,
unit sta
Facility-approved
disinfectant
Tool 1. Equipment Cleaning and
Disinfection Schedule
• All equipment and furniture should be routinely evaluated for intact surfaces that can be appropriately disinfected.
• Any damaged surfaces should either be repaired or replaced (for example, patch mattresses; repair chipped laminate; replace equipment
with cracked plastic; remove rust).
• Equipment should be kept in good working order, with preventive maintenance performed on a routine basis and per manufacturers’
instructions.
Department: __________________________________________________________________________________
Date last reviewed/updated: _______________________________________________________________________

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com8
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
Tool 2. Equipment-Disinfectant
Compatibility Assessment Tool
• Identify the equipment located in your unit/department that you are responsible for disinfecting.
• Determine the disinfectants approved for use in the instructions for use (IFUs) that your organization has approved/provides, and list them
across the top of this tool with the contact time.
• Identify the equipment manufacturer and obtain the manufacturer’s IFUs.
• Place a check mark in the corresponding box under each approved disinfectant for each piece of equipment.
• Once completed, determine the disinfectant that is compatible with the majority of your equipment, with the goal of stocking and using as
few dierent disinfectants as possible (ideally, bleach plus one additional disinfectant) and with the shortest contact time.
Assessment Date: _______________________________________________________________________________
Participants: ___________________________________________________________________________________
Equipment/Surface Manufacturer
Disinfectant #1
(e.g. quaternary
ammonia)
Disinfectant #2
(e.g. quaternary
ammonia)
Disinfectant #3
(e.g. alcohol-free quat)
Bleach
Hydrogen peroxide
Comments
Contact Time (minutes)
3 2 10 1 1
Example: Vitals machine
✔ ✔ ✔
Example: Blood pressure cu
✔ ✔ ✔ ✔ ✔
Example: Intravenous (IV)
pump
✔ ✔ ✔ ✔
Example: Cardiac monitor
✔ ✔
© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com9
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
Tool 3. Environmental Infection Prevention
Assessment Tool
Department: ___________________________________________________________________________________
Assessment Date: _______________________________________________________________________________
Reviewer: _____________________________________________________________________________________
General Environment Joint
Commission
Standard(s)
Yes No N/A Comments/
Actions
Floors and walls are clean and free of spills, dust, stains, tape,
and adhesive residue.
IC.02.02.01
Furnishings (for example, mattresses, chairs, beds, tables) are
free of holes, tears, tape, adhesive residue, stains, and rust.
IC.02.02.01
Curtains, window blinds, vents, sinks and all horizontal surfaces
are clean and dust free.
IC.02.02.01
Ceiling tiles are free of stains, leaks, and holes. IC.02.02.01
All drinks are covered in patient care areas. No food is in patient
care areas.
IC.02.02.01
Supply and Medication Storage Areas
Clean supplies and equipment are clean and free of spills, dust,
stains, tape, and adhesive residue and are kept separate from
dirty supplies and equipment. If required by facility policy, clean
equipment is labeled or bagged as clean.
IC.01.04.01
No patient care supplies are stored underneath sinks or draining
pipes.
IC.02.02.01
Items used to prepare medications are clean. If single patient use,
these are labeled (for example, pill cutters and crushers).
IC.02.02.01
Sterile supplies are stored in a clean, dry enclosed area. IC.02.02.01
Supplies are stored 8 to 10 inches above the oor. All bottom wire
racks in clean supply rooms have a plastic cover or solid bottom
shelf.
IC.02.02.01
No expired supplies (for example, hand sanitizer, soap,
disinfectant wipes, disinfectant solutions)
IC.02.02.01
Corrugated shipping boxes are not stored in clean and sterile
storage locations in clinical areas.
IC.02.02.01
Nourishment Areas
Refrigerators are clean, and freezers are defrosted. IC.02.01.01
Only patient food is stored in refrigerators and freezers found in
patient rooms.
IC.02.01.01

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com10
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
Nourishment Areas Joint
Commission
Standard(s)
Yes No N/A Comments
Refrigerated patient food brought from home is labeled with the
patient’s name and date made or obtained. No food items greater
than 3 days from the date made or obtained are found.
IC.02.01.01
Refrigerator logs are complete and accurate. IC.02.01.01
Refrigerator temperatures are appropriate. Corrective actions are
documented for temperatures falling out of range.
IC.02.01.01
Microwaves, ice machines and other appliances are clean. IC.02.02.01
Linen and Waste
Clean linen is stored on clean, covered shelves or in enclosed
cabinets separate from dirty linen.
IC.02.02.01
Soiled linen is stored in appropriate plastic bags, in a covered
hamper, or in the soiled utility room.
IC.02.02.01
Sharps containers are not overlled (that is, less than 3/4 full). IC.02.01.01
Trash is disposed of appropriately. Trash in soiled utility rooms is
contained, not overowing or lying on the oor.
IC.02.01.01
Soiled utility room has at least one red receptacle for potentially
infectious medical waste labeled with BIOHAZARD signage.
IC.02.01.01
Soiled reusable instruments that require high-level disinfection
or sterilization are pre-cleaned and stored and transported in a
covered biohazard marked container (for example, endoscopes,
surgical instruments). Soiled instruments are not on countertops
or lying in sinks.
IC.02.02.01
Environmental Services, Hand Hygiene, and Supplies
There is an adequate supply of liquid soap, alcohol-based hand
sanitizer, and paper towels. No expired soap or gel is found.
IC.01.04.01
Dispensers are functional. IC.01.04.01
Sta with direct patient contact do not have articial or long
natural nails.
IC.01.04.01
Sta can verbalize how they know what equipment is clean or
dirty and who is responsible for cleaning and disinfecting it.
IC.02.02.01
Sta can verbalize correct wet contact times for facility-approved
disinfectants and when to use each disinfectant (for example,
bleach versus quaternary ammonia).
IC.02.02.01
Sta can verbalize frequency of cleaning and disinfection of
various pieces of equipment.
IC.02.02.01
Environmental services sta can verbalize correct order if
cleaning and disinfecting a patient room.
IC.02.02.01
Sta use personal protective equipment correctly for cleaning and
disinfection (for example, gloves are not worn in hallways or room
to room).
EC.02.02.01
IC.02.01.01

© 2018 JOINT COMMISSION RESOURCES www.jcrinc.com11
Environmental Infection Prevention: Guidance for Continuously Maintaining a Safe Patient Care and Survey-Ready Environment
Environmental Services, Hand Hygiene, and Supplies Joint
Commission
Standard(s)
Yes No N/A Comments
Environmental services sta can verbalize correct use of cleaning
and disinfection solutions (for example, no double-dipping rags,
frequency of mop head changes).
IC.02.02.01
Environmental services carts are secured. EC.02.02.01
Environmental services closets do not contain patient care
supplies or supplies that may be compromised by moisture
(for example, toilet paper). These items should be stored in a
dedicated clean storage room or cabinet.
IC.02.02.01
If cleaning and disinfection solutions are not ready to use, sta
can verbalize correct dilution per manufacturer’s instructions.
Measuring containers and required personal protective equipment
are available and used.
EC.02.02.01
IC.02.02.01
Secondary containers for cleaners and disinfectants are labeled
per facility policy and in compliance with OSHA requirements. Per
OSHA 29 CFR 1910.1200(f), the employer shall ensure that each
container of hazardous chemicals in the workplace is labeled,
tagged, or marked with the following information:
Identity of the hazardous chemical(s) contained therein; and
Appropriate hazard warnings, or alternatively, words, pictures,
symbols, or combination thereof, which provide at least general
information regarding the hazards of the chemicals, and which,
in conjunction with the other information immediately available to
employees under the hazard communication program, will provide
employees with the specic information regarding the physical
and health hazards of the hazardous chemical.
EC.02.02.01
IC.02.01.01
Deep Cleaning and Preventive Maintenance Joint
Commission
Standard(s)
Yes No N/A Comments
Mattresses, pillows, and covers are in good repair, without holes,
tears, or staining.
Bed frames are clean and in good repair (including side rails,
hinges, casters or wheels, and bases).
Carpet, if present, is clean, without stains, and on a routine
extraction schedule.
Ice machines and storage bins are clean and maintained.
Privacy curtains are visibly clean and on a routine cleaning/
laundering schedule.

