
2
Welcome to Research Day!
On behalf of the Office of Research, we welcome you to Research Day 2019. This annual event brings
together MCW scientists, clinicians, staff and students for a day of networking and discovery. This year’s
event focuses on the theme of Team Science. As we anticipate new programs and activities stemming
from the Research Strategic Plan, we celebrate the dynamic research and collaborative culture that leads
to high quality, innovative science.
We hope you can join our first ever Team Science Sessions, in which the Cardiovascular Center,
Neuroscience Research Center, and Cancer Center are each presenting on a collective team project
brought to fruition in the environment of a center. The goal of these Sessions is to provide insight to the
elements that make team science work.
We are once again hosting a lunch hour Keynote Talk and are thrilled to welcome renowned population
science expert and member of the National Academy of Medicine, Kirsten Bibbins-Domingo, MD, PhD,
MAS. Dr. Bibbins-Domingo is the Lee Goldman, MD Endowed Chair in Medicine, Professor and Chair of
the Department of Epidemiology and Biostatistics, and Professor of Medicine. She is the inaugural Vice
Dean for Population Health and Health Equity in the UCSF School of Medicine. She will be presenting
“Cardiovascular Disease and Precision Prevention” in the Alumni Center at noon.
Following the Keynote, this year’s Poster Session will stretch from the MCW Cafeteria Lobby through to
the Hub Gallery. We invite anyone and everyone to connect and conversate with 120+ researchers
representing 24 different departments, institutes, and centers. We hope that this bridging of our set-up
inspires the same bridging that leads to exciting new research projects.
This catalog not only contains the research showcased on Research Day, it also includes an institutional
overview across our many departments and centers. You can also meet a diverse cross-section of MCW
investigators in the monthly Research Publication Series.
Thank you for joining us as we celebrate all things research!
Ann B. Nattinger, MD, MPH, MACP Cecilia Hillard, PhD
Associate Provost for Research Associate Dean for Research

3
Table of Contents
Research Day
Schedule ........................................................................................................................................................................ 5
Acknowledgements ....................................................................................................................................................... 6
About Keynote Speaker Dr. Kirsten Bibbins-Domingo ................................................................................................... 7
Poster Session Map ........................................................................................................................................................ 8
Abstract Index ................................................................................................................................................................ 9
Abstract Text ................................................................................................................................................................ 18
MCW Research Overview
Funding ..................................................................................................................................................................... 147
Publications................................................................................................................................................................ 154
Society for Research Excellence ................................................................................................................................. 159
About the Office of Research ..................................................................................................................................... 160
Resources, Centers & Institutes
All of Us Research Program .................................................................................................................................... 165
Cancer Center ......................................................................................................................................................... 166
Cancer Center Redox & Bioenergetics Shared Resource ....................................................................................... 167
Cardiovascular Center ............................................................................................................................................ 169
Center for Advancing Population Science .............................................................................................................. 170
Center for AIDS Intervention Research ......................................................... (see Psychiatry & Behavioral Medicine)
Center for Biomedical Mass Spectrometry Research ............................................................................................. 171
Center for Healthy Communities and Research ..................................................................................................... 172
Center for Imaging Research .................................................................................................................................. 173
Center for Immunology .......................................................................................................................................... 174
Center for Infectious Disease Research ................................................................................................................. 175
Center for International Blood & Marrow Transplant Research ............................................................................ 176
Center for Microbiome Research ........................................................................................................................... 177
Center for Neurotrauma Research ......................................................................................................................... 178
Center of Systems Molecular Medicine ................................................................................................................. 180
Children’s Research Institute ................................................................................................................................. 181
Clinical & Translational Sciences Institute .............................................................................................................. 182
Comprehensive Injury Center ................................................................................................................................ 184
Drug Discovery Center ........................................................................................................................................... 185

4
Genomic Sciences & Precision Medicine Center .................................................................................................... 186
Institute for Health & Equity .................................................................................................................................. 188
National Biomedical EPR Center ............................................................................................................................ 192
Neuroscience Research Center .............................................................................................................................. 193
Research Computing Center .................................................................................................................................. 194
Wisconsin CIREN (Crash Injury Research and Engineering Network) .................................................................... 195
Versiti Blood Research Institute ............................................................................................................................. 196
Basic Science Departments
Biochemistry .......................................................................................................................................................... 197
Biomedical Engineering .......................................................................................................................................... 201
Biophysics ............................................................................................................................................................... 203
Cell Biology, Neurobiology & Anatomy .................................................................................................................. 205
Microbiology & Immunology.................................................................................................................................. 206
Pharmacology & Toxicology ................................................................................................................................... 210
Physiology .............................................................................................................................................................. 212
Clinical Departments
Anesthesiology ....................................................................................................................................................... 216
Dermatology ........................................................................................................................................................... 217
Emergency Medicine .............................................................................................................................................. 218
Family & Community Medicine ....................................................(see Center for Healthy Communities & Research)
Medicine................................................................................................................................................................. 219
Neurology ............................................................................................................................................................... 235
Neurosurgery ............................................................................................... (see Center for Neurotrauma Research)
Obstetrics & Gynecology ........................................................................................................................................ 236
Ophthalmology & Visual Sciences .......................................................................................................................... 238
Orthopaedic Surgery .............................................................................................................................................. 240
Otolaryngology & Communication Sciences .......................................................................................................... 243
Pathology ............................................................................................................................................................... 244
Pediatrics ................................................................................................................................................................ 246
Physical Medicine & Rehabilitation ........................................................................................................................ 247
Plastic Surgery ........................................................................................................................................................ 248
Psychiatry & Behavioral Medicine.......................................................................................................................... 249
Radiation Oncology ................................................................................................................................................ 253
Radiology ................................................................................................................................................................ 254
Surgery ................................................................................................................................................................... 257
Urology ................................................................................................................................................................... 268

Jump to Table of Contents 5
Research Day Schedule
Thursday, September 19, 2019
11:00 a.m. – noon
Discovery Classroom
Lunch will be
provided, RSVPs
requested.
Team Science Sessions
These brief talks highlight a collaborative, interdisciplinary team brought together in the
environment of an MCW center. Hosted by Susan Cohen, MD.
Cardiovascular Center presents:
"AHA Strategically Focused Hypertension Research Center"
Mingyu Liang, MB, PhD
Neuroscience Research Center presents:
"Multidisciplinary Study of Traumatic Brain Injury"
Chris Olsen, PhD
Cancer Center presents:
"Pancreatic Cancer Working Group"
Mike Dwinell, PhD & Susan Tsai, MD
Noon – 1:00 p.m.
Alumni Center
Doors Open &
Lunch Available
at 11:45 a.m.
Keynote Talk
“Cardiovascular Disease and Precision Prevention”
Kirsten Bibbins-Domingo, PhD, MD, MAS
Lee Goldman, MD Endowed Chair in Medicine
Professor and Chair, Dept of Epidemiology & Biostatistics
Professor of Medicine
Vice Dean for Population Health and Health Equity
University of California, San Francisco
Member, National Academy of Medicine
Read Dr. Bibbins-Domingo’s Biography
1:00 – 3:00 p.m.
MCW Cafeteria Lobby
to Hub Gallery
Poster Session
Posters will be judged for monetary awards in 5 categories.
View Poster Session Map

Jump to Table of Contents 6
Research Day Acknowledgements
Research Day is sponsored by the Office of Research. Thank you to Cecilia Hillard, PhD, for leading the planning team, and
Susan Cohen, MD, for hosting the Team Science Sessions. Thanks to the following individuals for reviewing and judging our
Poster Session presenters:
• Akiko Mammoto, MD, PhD, Assistant Professor, Neonatology, Pediatrics
• Alison Kriegel, PhD, Associate Professor, Physiology
• Allan Cowley, Jr, PhD, Professor, Physiology
• Andreas Beyer, PhD, Associate Professor, Medicine, Cardiology
• Antje Kroner-Milsch,MD, PhD, Assistant Professor, Neurosurgery
• Aron Geurts, PhD, Associate Professor, Physiology
• Banani Banerjee, PhD, Associate Professor, Medicine, Gastroenterology
• Benjamin Gantner, PhD, Assistant Professor, Medicine, Endocrinology
• Caitlin O'Meara, PhD, Assistant Professor, Physiology
• David Clark, PhD, Director, Research Office, Human Research Protection Program
• David Gutterman, MD, Sr. Associate Director, Professor, Medicine, Cardiology
• Debebe Gebremedhin, PhD, Associate Professor, Physiology
• Debra Scott, PhD, Manager, Office of Research, Research Systems
• Elizabeth Jacobs, MD, Associate Dean, Professor, Medicine, Pulmonary
• Heather Toth, MD, Professor, General Internal Medicine
• Jacquelyn Kulinski, MD, Assistant Professor, Medicine, Cardiology
• Jenifer Coburn, PhD, Professor, Medicine, Infectious Disease
• Jim Antczak, PhD, Assistant Director, Research Office, Office of Technology Development
• John Imig, PhD, Professor, Pharmacology & Toxicology
• John Meurer, MD, MBA, Institute Director, Institute for Health and Equity
• Joseph Barbieri, PhD, Professor, Microbiology and Immunology
• Julie Panepinto, MD, MSPH, Professor, Pediatrics, Hematology and Oncology
• Justin Grobe, PhD, Associate Professor, Physiology
• Kalpa Vithalani, PhD, Assistant Director, Research Office, Office of Technology Development
• Kelsey Porada, Clinical Research Coordinator, Pediatric Hospital Medicine
• Kevin Boggs, PhD, Director, Research Office, Office of Technology Development
• Li-Shu Wang, PhD, Associate Professor, Medicine, Hematology and Oncology
• Matthew Durand, PhD, Assistant Professor, Physical Medicine & Rehab-Cardiovascular
• Monty McKillop, PhD, Manager, GMPVecotr Production Facility, Pediatrics
• Nancy Dahms, PhD, Professor, Biochemistry
• Oleg Palygin, PhD, Assistant Professor, Physiology
• Purushottam Laud, PhD, Professor, Biostatistics, Institute for Health and Equity
• Robert Lochhead, PhD, Assistant Professor, Microbiology and Immunology
• Sadie Larsen, PhD, Associate Professor, Psychiatry
• Susan Cohen, MD, Associate Professor, Pediatrics
• Susan Taylor, MD, MPH, Associate Professor, Pediatrics, Anesthesiology
• Suresh Kumar, PhD, Assistant Professor, Pathology
• Tadanori Mammoto, MD, PhD, Assistant Professor, Neonatology, Pediatrics
• Tami Maier, PhD, RBP, Assistant Biological Safety Officer, Department Environmental Health and Safety
• Tom Aufderheide, MD, Professor, Emergency Medicine
• Xiao Chen, MD, PhD, Associate Professor, Medicine, Hematology and Oncology
• Xiaowen Bai, PhD, Associate Professor, Cell Biology, Neurobiology and Anatomy
• Zeljko Bosnjak, PhD, Professor, Medicine, Endocrinology
Jump to Table of Contents 7
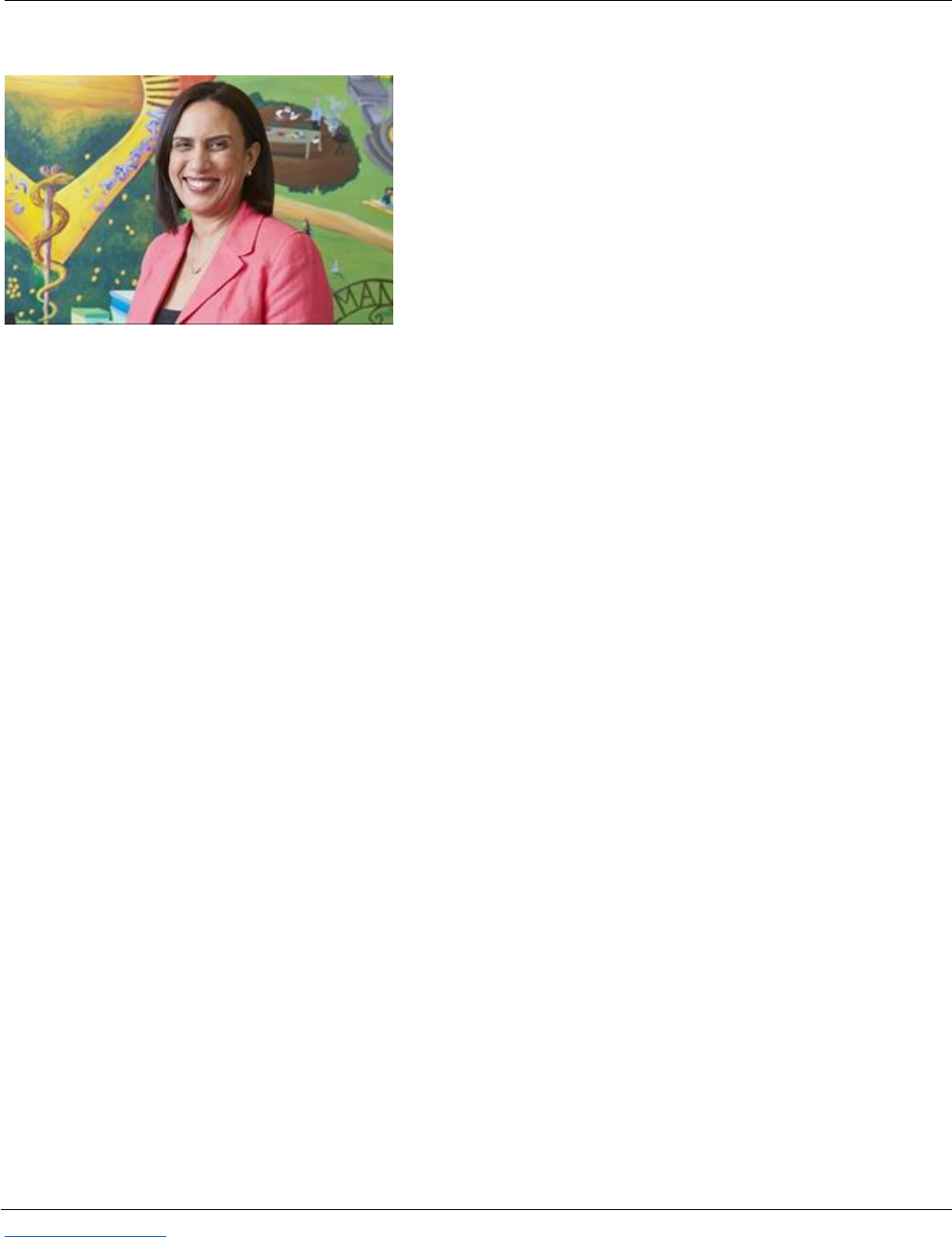
About Keynote Speaker Dr. Kirsten Bibbins-Domingo
Kirsten Bibbins-Domingo, PhD, MD, MAS is the Lee Goldman,
MD Endowed Chair in Medicine, Professor and Chair of the
Department of Epidemiology and Biostatistics, and Professor
of Medicine. She is the inaugural Vice Dean for Population
Health and Health Equity in the UCSF School of Medicine. Dr.
Bibbins-Domingo co-founded the UCSF Center for Vulnerable
Populations at Zuckerberg San Francisco General Hospital, a
research center focused on discovery, implementation, policy,
advocacy, and community engagement for communities at
risk for poor health and inadequate healthcare. She is one of
the PIs of the UCSF Clinical and Translational Science Institute.
A general internist at Zuckerberg San Francisco General Hospital, Dr. Bibbins-Domingo has expertise in
cardiovascular disease, hypertension, diabetes, and chronic kidney disease with a particular interest in the
development of these conditions in young adults. She is an NIH-funded researcher who uses observational
studies, pragmatic trials, and simulation modeling to examine effective clinical, public health, and policy
interventions aimed at prevention. She leads the UCSF Cardiovascular Disease Policy Model group that conducts
simulation modeling, disease projections, and cost-effectiveness analyses related to cardiovascular disease in
the US and in other national contexts.
Dr. Bibbins-Domingo was a member of the US Preventive Services Task Force from 2010-2017 and led the Task
Force as the vice-chair and chair from 2014-2017. She is an inducted member of the American Society for Clinical
Investigation, the Association of American Physicians, and the National Academy of Medicine.
Dr. Bibbins-Domingo is a trustee of Princeton University and a director on the board of the San Francisco
General Hospital Foundation.

Jump to Table of Contents 9
Abstract Index
Metabolism, Endocrine & Digestive
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
1
Brian Hoffmann, PhD
Biomedical
Engineering
Metabolic Effects Associated with Chronic Artificial
Sweetener Consumption
Junior Faculty
2
Katherine M Allen
Maternal Fetal
Medicine
Elevated Levels of FGF21 In the Placenta of
Macrosomic Infants
Student
3
NOT PRESENTING:
Arjun Mainali
Neurology
Serum Aminotransferases Level in Patients with
Type 2 Diabetes Mellitus attending a Tertiary Care
Center, Kathmandu
Student
4
Rachel Harrison, MD
Obstetrics and
Gynecology:
Maternal-Fetal
Medicine
The association between provider type and the
choice of pharmacologic agent for treatment of
gestational diabetes
Clinical Fellows
& Residents
5
Simone Scalia
Pediatrics
Immunogenic Epitope Profiling in Fabry Disease
Patients Undergoing Enzyme Replacement Therapy
Postdoctoral
Fellow
6
Rybova J
Pediatrics:
Hematology/Oncology
Acid Ceramidase Deficiency Leads to Skin
Inflammation and Impaired Adipogenesis in a
Mouse Model of Farber Disease
Postdoctoral
Fellow
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
7
Gunnar Whealy, BS
Department of
Orthopaedic Surgery
Shoulder ROM in Youth Baseball Pitchers: Pain vs.
No Pain
Student
8
Madeline Perlewitz
Orthopaedic Surgery
Knee Arthrofibrosis Following Tibial Plateau
Fracture Treated with Arthroscopic Lysis of
Adhesions with Manipulation
Student
9
Michael Ziegele
Orthopaedic Surgery
Arthroscopic Lysis of Adhesions with Manipulation
for Management of Resistant or Late Presenting
Arthrofibrosis Following Total Knee Arthroplasty
Clinical Fellows
& Residents
10
Gwendolyn Hoben
Plastic Surgery
Targeted Muscle Reinnervation in Rat Spared Nerve
Injury Models Neuropathic Amputation-Related
Pain Relief
Junior Faculty
11
Timothy Ridolfi, MD
Surgery: Colorectal
Surgery
Changes in the Enteric Serotonin Signaling System
Following Low Anterior Resection
Senior Faculty
12
Katherine Hu, MD
Surgery: Colorectal
Surgery
Alvimopan use in the setting of Abdominoperineal
Resection: a retrospective cohort study
Clinical Fellows
& Residents
13
Richard W. Walsh
Surgery: Division of
Cardiothoracic
Surgery
A Bridge to the Fridge? Changes in BMI Post Left
Ventricular Assist Device Implant
Student
14
Bryce Toburen
Urology
Are Patients with Gender Dysphoria Counseled on
Fertility Preservation Prior to Hormonal Therapy
Initiation?
Student
15
Kaylee Luck
Urology
IMPACT OF BILATERAL ORCHIECTOMY IN
REDUCTION OF HORMONE MEDICATION REGIMEN
IN GENDER DYSPHORIA
Student

Jump to Table of Contents 10
Population, Community Health & Outcomes
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
16
Olaitan Akinboboye
CAPS
1 / 1 The Relationship between C-Reactive Protein
and Mortality in Adults with Diabetes: Influences of
Demographic Characteristics, Lifestyle Behaviors,
and Medications
Student
17
Joanna Obaoye
CAPS
Assessing the Relationship between Lifetime, Daily,
and Chronic Job Discrimination and Mortality in a
Nationally Representative Sample of Adults
Student
18
Oluwatoyin Olukotun,
PhD, RN
CAPS
Chronic Disease Risk and Onset in Adults with a
History of Incarceration
Postdoctoral
Fellow
19
Sean O'Toole
CAPS
Investigating Racial/Ethnic Disparities in Cognitive
Decline for Older Adults with Diabetes
Student
20
Timothy Corwin
CAPS
Independent relationship between financial
hardship and time to diabetic kidney disease
Student
21
Jordan A. Gliedt
CAPS and
Neurosurgery
The relationship between patient satisfaction and
health care expenditures in adults with spine
related disorders: an analysis of the 2008-2015
Medical Expenditures Panel Survey (MEPS).
Junior Faculty
22
Danielle Olsen
Family and
Community Medicine
Utilizing Arts Based Data Generation Techniques to
Develop Socio-technical Anger Interventions in the
Veteran Population
Student
23
Lillian Zheng
Medicine: Geriatrics,
VA Hospital
Multimorbidity and Functional Status among
Geriatric Veterans
Student
24
Steven A. John
Psychiatry and
Behavioral Medicine:
Center for AIDS
Intervention Research
Post-exposure prophylaxis (PEP) awareness and
prescribing practices among US primary care
providers and HIV specialists
Junior Faculty
Education
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
25
Adhitya Ramamurthi,
Devashish Joshi,
Michelle Botts
Surgery: Division of
Cardiothoracic
Surgery
Implementing Virtual Reality in Medical Education
and Training
Student
Kidney
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
26
Jessica Hayes
Pediatric Hospital
Medicine
Timing of renal ultrasound for first febrile UTI in
young children: Sooner or later?
Student

Jump to Table of Contents 11
Cancer
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
27
Gayatri Sharma
Biomedical
Engineering
Photo triggered liposomes for delivery of
immunostimulatory cytokines to solid tumors
Postdoctoral
Fellow
28
Sean D. McGarry
Biophysics
Magnetic resonance imaging based radio-pathomic
maps of epithelium and lumen density localize high
grade prostate cancer independent of variability in
pathological annotation
Student
29
Shannon L. Walker,
MEd
CAPSs and Institute
for Health and Equity
Trends in Healthcare Expenditures among Adult
Cancer Survivors in the United States, 2008-2016
Student
30
Brad Taylor
CTSI and GSPMC
Advancing the Science of Translation Through the
Establishment of the CTSI Translational Informatic
and Bioinformatic Research Unit
Junior Faculty
31
NOT PRESENTING
Eric Fair
Nuclear Medicine
Retrospective Quantitative Analysis Comparing
Respiratory Gated to Non-respiratory Gated 18F-
FDG PET/CT Imaging in Patients Undergoing
Evaluation for Primary Lung Cancer
Clinical Fellows
& Residents
32
Robyn Oldham
Pediatrics
CAR-modified Th1/Tc1-Polarized T-Rapa Cells
Dissociate Inflammatory Cytokine Secretion from
Anti-Tumor Cytotoxicity
Research
Support Staff
33
Anahi Cruz
Pediatrics
Murine models to study NK immunotherapy against
sarcoma
Student
34
Kayvon Kiani
Radiology : Abdominal
Imaging
Accuracy of MRI-TRUS Fusion Targeted Prostate
Biopsy and Quality Review
Student
35
Matthew Scheidt, MD
Radiology: VIR
Outcomes following endovascular interventions for
bleeding events in head and neck cancer patients
Junior Faculty
36
Guillermo A. Urrutia
Surgery
Cell Cycle Dependent Inhibition of G9a Induces Cell
Death via Replication Catastrophe in Pancreatic
Cancer
Postdoctoral
Fellow
Blood, Immunity & Infection
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
37
Ankan Gupta
Pediatrics
Rescuing Exhausted CD8 T cells: Targeting
Phosphatase a Novel Strategy?
Postdoctoral
Fellow
Pulmonary
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
38
NOT PRESENTING
Gary C Mouradian
Physiology
Acute and chronic changes in the control of
breathing in a rat model of bronchopulmonary
dysplasia
Junior Faculty
39
Victor Magana, El-
Sayed H. Ibrahim
Radiology
Assessment of Regional Heart Function in
Pulmonary Hypertension Using MRI
Student

Jump to Table of Contents 12
Technology, Methods & Resources
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
40
Chris Hansen
Biomedical Engineering
High Resolution Lymphatic Imaging with a Dual
NIR-SWIR Multispectral Imaging System
Student
41
Jennifer R Smith
Biomedical Engineering
RGD: data and tools for precision models of
human disease
Research
Support Staff
42
Mir Hadi Razeghi
Biomedical Engineering
Computational study of Microwave ablation versus
Plasmonic Nanoparticle Mediated Photothermal
Therapy for Liver Tumors
Student
43
Cagatay Dursun
Biomedical Engineering:
Computational Biology
and Bioinformatics
PhenoGeneRanker: A Tool for Gene Prioritization
Using Complete Multiplex Heterogeneous
Networks
Student
44
Abdul K. Parchur
Biomedical Engineering
NIR-II Emitting Quantum Dots for in vivo Preclinical
Imaging Applications
Research
Support Staff
45
Wendy M. Demos
GSPMC: Bioinformatics
Research and
Development Laboratory
Applications and Methods to Give Meaning to
Exome and Genome Based Data in Research
Research
Support Staff
46
Michael T.
Zimmermann
GSPMC: Bioinformatics
Research and
Development Laboratory
Bioinformatic and Data Analytic services offered by
the GSPMC (GSPMC)
Junior Faculty
47
Mike Tschannen
GSPMC
Innovation to Practice - Basic and Translational
Research Tools, Services, and Assays in GSPMC
Research
Support Staff
48
Young-In Chi
GSPMC: Bioinformatics
Research and
Development Laboratory
Advancing Cancer Precision Medicine through
Innovative Methods for the Interpretation of
Genomic and Epigenomic Data Generated by Next
Generation Sequencing
Junior Faculty
49
Atefeh (Lida)
Zeighami
GSPMC: Bioinformatics
Research and
Development Laboratory
Developing and Implementing a Robust and
Thorough RNA-Seq Data Analysis and Deliverable
Report
Research
Support Staff
50
Stefano Rosati
GSPMC: Bioinformatics
Research and
Development Laboratory
Quality & Precision in the Next Generation Era: An
analysis of Illumina Chemistry & Quality score
changes
Research
Support Staff
51
Swarnendu Tripathi
GSPMC: Bioinformatics
Research and
Development Laboratory
Protein Scores for the Advancement of Precision
Medicine and Genomics Data Interpretation:
Application to RAS Proto-Oncogenes
Research
Support Staff
52
Jenica Abrudan
GSPMC: Bioinformatics
Research and
Development Laboratory
A comprehensive, interactive, and visual RRBS
analysis pipeline
Research
Support Staff
53
Venkata Krishna
Puppala
Medicine:
Cardiovascular Medicine
Permanent Pacemaker (PPM) Detected Activity
Time is More Sensitive to Changes in Activity
Levels than Pedometers in Sedentary Older
Patients
Junior Faculty

Jump to Table of Contents 13
Technology, Methods & Resources
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
54
Caroline Davitt
Obstetrics &
Gynecology:
Maternal-Fetal
Medicine
Clinical Survey Research: Design, Validation &
Dissemination
Student
55
Schneider, Ellen Anje
Pathology
Effect of -80°C Storage on RNA from Snap Frozen
Placental Tissue
Research
Support Staff
56
Kemi Adeyanju
Pediatrics
Regulatory T Cell Differentiation via Engagement of
the PD1/ PDL1 Co-Inhibitory Pathway.
Postdoctoral
Fellow
57
Angela Lemke
Physiology
Somatic Cell Genome Editing Program: Dissemination
and Coordinating Center
Research
Support Staff
58
Michael N Grzybowski
Physiology
Gene Editing Rat Resource Center (GERRC): Rat
models for heart, lung and blood studies
Research
Support Staff
59
Rebecca Schilling
Physiology
Hybrid Rat Diversity Program (HRDP): A rat resource
for systems genetics
Research
Support Staff
60
Alexandra Fairchild
Radiology: VIR
Evaluation of procedural time and radiation exposure
in celiac plexus block using iGuide fluoroscopic
navigation versus CT guidance
Junior Faculty
61
Eric Hohenwalter, MD
Radiology: VIR
A prospective study evaluating a novel class of
software for Quantifying successful tissue perfusion
during lower extremity endovascular stent placement
Senior Faculty
62
Sarah White, MD
Radiology: VIR
Does implementation of an effective midline catheter
program for vascular access in a large academic
hospital decrease rates of bloodstream infections?
Senior Faculty
63
Sean Tutton, MD
Radiology: VIR
Advanced Guidance and Access Techniques for
Challenging Osteoid Osteoma Ablations
Senior Faculty
Neuroscience
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
64
Bin Pan
Anesthesiology:
Research
Ectopic activity from injured dorsal root ganglion
neurons triggers hyperalgesia and allodynia in rats
with spinal nerve ligation
Junior Faculty
65
Elizabeth Roth
Anesthesiology:
Research
Repetitive Mild Traumatic Brain Injury Induces Long-
Term Cognitive Impairment in Rats
Research
Support Staff
66
Briana Meyer
Biophysics
Feasibility and Optimization of Perfusion MRI in the
Rat Cervical Spinal Cord
Student
67
Seung-Yi Lee
Biophysics
MRI predictors of neurological function in a rat model
of cervical spinal cord contusion injury
Student
68
Morgan E. Nitta
Neurosurgery
Acute effects of sport-related concussion on
neuroactive kynurenine pathway metabolites and
their association with post-concussion mood
symptoms
Student
69
Luisa Bohorquez-
Montoya1
Neurosurgery,
Biomedical
Engineering and
Radiology
Diffusion tensor imaging and quantitative
susceptibility mapping in concussed adolescents with
and without persistent symptoms
Postdoctoral
Fellow

Jump to Table of Contents 14
Neuroscience
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
70
Jose Rosas
Neurosurgery,
Microbiology and
Immunology
Loss of IL-12p40 mediates a beneficial effect on
recovery after spinal cord injury.
Student
71
Christina Behlke
Pharmacology &
Toxicology
Role of Microglial CB2 Receptors in the
Hyperlocomotor Effects of Cocaine
Student
72
Alex Barrington
Radiology
Prediction of Cellularity in Glioblastoma using MRI
Radiomic Features
Student
73
Allison Lowman
Radiology
A precise comparison of heterogeneous
pathological features of glioblastoma at autopsy to
T1 subtraction maps
Research
Support Staff
74
Samuel Bobholz
Radiology
Comparison of MRI Radiomics and Histomic
Features in Glioblastoma
Student
75
Alexander Cohen
Radiology: Imaging
Research Center
Longitudinal Reproducibility of MR Perfusion Using
the 3D pCASL with Multiple Postlabeling Delay
Research
Support Staff
Cardiovascular & Stroke
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
76
Boran Katunaric
Anesthesiology:
Cardiovascular Center
SPHINGOSINE-1-PHOSPHATE INDUCED
VASODILATION OF HUMAN ARTERIOLES: ROLE OF
S1P RECEPTOR 1
Postdoctoral
Fellow
77
Harsimran S. Kalsi
Biomedical
Engineering
Endothelialization of a Novel Flow Diverter Using
Magnetic Capture
Student
78
Jaidip Jagtap
Biomedical
Engineering
Dynamic contrast-enhanced near-infrared
fluorescence imaging to probe altered vascular
changes in rat models
Research
Support Staff
79
Emily Nordquist
Herma Heart Institute
A Model to Study the Aortic Valve Response to
Endothelial Injury
Student
80
Mamatha Kakarla
Medicine:
Cardiovascular
Downregulation of Fis1 in Endothelial Cells Does
Not Impact Normal Endothelial Cell Mitochondrial
Bioenergetics, Metabolism, or Mitochondrial
Protein Content
Research
Support Staff
81
Benjamin C. Hofeld
Medicine:
Cardiovascular
Disease
Lactobacillus plantarum 299v Supplementation
Results in Anti-Inflammatory Changes in
Mononuclear Cell Gene Expression in Men with
Stable Coronary Artery Disease Who Do Not Drink
Alcohol Daily
Clinical Fellows
& Residents
82
Megan Reinhard
Obstetrics: MFM
Survey of antepartum women to assess barriers to
sequential compression device compliance
Student
83
Kaitlyn Thatcher
Pediatrics
Structure-Function-Molecular Relationships of the
Extracellular Matrix of Aortic Valves in Mouse
Models of Human Disease
Research
Support Staff
84
Punashi Dutta
Pediatrics
The pharmacological XPO1 antagonist KPT-330
prevents aortic valve calcification via a novel C/EBP
□ signaling pathway
Postdoctoral
Fellow
85
Vinal Menon
Pediatrics
Hyperphosphatemia-induced aortic valve
calcification in the setting of chronic kidney disease
Postdoctoral
Fellow

Jump to Table of Contents 15
Cardiovascular & Stroke
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
86
Bailey Dye
Pediatrics
The Role of α-Smooth Muscle Actin in Mitral Valve
Prolapse
Student
87
Pablo Nakagawa
Physiology
Susceptibility of Mice Lacking Renin-b to Chronic
Angiotensin II Infusion
Postdoctoral
Fellow
88
Micaela Young, El-
Sayed H. Ibrahim
Radiology
Magnetic Resonance Imaging for Non-Invasive
Assessment of Cardiac Function in Small Animals
Student
89
Parag Patel, MD
Radiology: VIR
TransCarotid Artery Revascularization (TCAR): A
Single-Center One Year Experience
Senior Faculty
90
Johnny Shepherd
Surgery: Cardiothoracic
Hospital Length of Stay Predicts Mortality and
Readmission Rates in Advanced Heart Failure
Student
91
Mohammed
Kamalia
Surgery: Cardiothoracic
Surgery
Detection of Seasonal Trends in National Donor Heart
Availability Using the UNOS Dataset
Student
Clinical
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
92
Susan Taylor
Anesthesiology: Pediatric
Anesthesiology
Perioperative Ketorolac Administration Increases
Post-tonsillectomy Bleeding In A Tertiary Pediatric
Hospital; A Quality Review Of 8582 Operations
Senior Faculty
93
Mike Andresen
GSPMC: Bioinformatics
Research and
Development Laboratory
Agilent V4 and V7 exome capture kits: A systematic
comparison of kit performance and implications of
clinical use for CNV
Research
Support Staff
94
Zachary Colvin
Obstetrics & Gynecology:
Maternal Fetal Medicine,
Pediatrics
Duration of labor induction in nulliparous women
with preeclampsia and maternal and neonatal
outcomes
Clinical Fellows
& Residents
95
Talia Coney
Obstetrics and
Gynecology
Maternal Outcomes of Pregnancies Complicated by
Fetal Life Limiting or Lethal Conditions
Clinical Fellows
& Residents
96
Esha Afreen
Obstetrics and
Gynecology: Maternal
Fetal Medicine
State Law Designed to Decrease Post-operative
Opioid Prescriptions: Is it Best for the Patient?
Student
97
Elizabeth Suelzer,
MLIS, AHIP
Office of Research: MCW
Libraries
Still feeling the effects: a citation analysis of the
highly cited, retracted article on MMR vaccines and
autism
Research
Support Staff
98
Satvir Kalsi
Pain Medicine and
Rehabilitation
Chronic Pelvic Pain After Sling Surgery - A case series
Student
99
Andrea Cyr, D.O.
Physical Medicine and
Rehabilitation
Ultrasonographic Comparison of the Lateral
Epicodyle in Manual Wheelchair-Users
Clinical Fellows
& Residents
100
Jennifer Yacub
Martin
Physical Medicine and
Rehabilitation
Reducing readmissinos by standardizing discharge
summary documentation
Junior Faculty
101
Jacob Pfeiffer
Physical Medicine and
Rehabilitation
Conservative Pain Management of Pre-Sacral
Schwanomma: A Case Report
Clinical Fellows
& Residents
102
Meagan Jozwiak
Physical Medicine and
Rehabilitation
Complex Regional Pain Syndrome Management: An
Evaluation of the Risks and Benefits of Spinal Cord
Stimulator Use in Pregnancy
Clinical Fellows
& Residents

Jump to Table of Contents 16
Clinical
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
103
Benedikt Pleuhs
Psychiatry
Provider level barriers to PrEP implementation in the
United States: a systematic review
Student
104
Peter DeVries MD
Psychiatry and
Behavioral Medicine
Lithium Monitoring and Outcomes in the Perioperative
Period: A Quality Improvement Project
Clinical Fellows &
Residents
105
Robert Hieb, MD
Radiology: VIR
TransCarotid Artery Revascularization (TCAR): High-Risk
Anatomical Lesions and Other Advantages Over Trans-
Femoral Approach
Senior Faculty
106
Kaila Redifer
Tremblay, MD
Radiology: VIR
Percutaneous Cryoablation for the Treatment of Extra-
Abdominal Desmoid Tumors
Clinical Fellows &
Residents
107
William Rilling, MD
Radiology: VIR
Correlation between right artial pressures as measured
by echocardiography (ECHO) versus direct right heart
pressure measurements in patients undergoing
transjugular intrahepatic portosystemic shunt(TIPS)
placement
Senior Faculty
N/A
NOT PRESENTING:
Zeeshan Qazi
Radiology
Expectations of Critical Radiology Result
Communication
Student
Basic Science
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
108
Shima Sadri
Biomedical
Engineering
Modeling the Kinetics and Regulation of NADPH
Oxidase 2 Assembly and Activation Facilitating Electron
Flow and Superoxide Generation
Student
109
Jamie Wendt-
Andre
GSPMC
Genomic profiling for Personalized Medicine -
technologies and services offered by the GSPMC
Research
Support Staff
110
Angela Mathison
GSPMC, Surgery
Aurora Kinase B-phosphorylated HP1a Functions in
Chromosomal Instability
Junior Faculty
111
Raul Urrutia
GSPMC, Surgery
Precision Medicine Approaches in Pancreatic Cancer
Revealed New Therapeutic Targets Derived from
Tumor-Stroma Cross-Talk
Senior Faculty
112
Thiago Milech De
Assuncao
GSPMC, Surgery
Work at the Precision Medicine Simulation Unit
Identifies a Novel, Alternative Spliced Isoform of the
Cancer-Associated Epigenomic Regulator, HP1y
Research
Support Staff
113
Tim Stodola
GSPMC, Surgery
The Histone 9 Methyl Transferase, G9a, is a Direct
regulator of the cell cycle regulator, Cdkn1A (p21)
During KRAS-Mediated PDAC Initiation
Postdoctoral
Fellow
114
Jennifer Geurts
GSPMC
Genomic variation in PDAC-predisposing genes
identified using the MCW germline exome panel
Junior Faculty
115
Romica Kerketta
GSPMC
Proteomics, RNA-Seq, ATAC-Seq, RRBS, and Multi-
parametric ChIP-Seq Intergration Reveal the Early
Epigenomic Landscape of Oncogenic Kras Signaling
Research
Support Staff
116
Nikita R. Dsouza
GSPMC
Developing surface-based scores for interpreting
genomic variants
Research
Support Staff

Jump to Table of Contents 17
Basic Science
Poster #
Presenter(s):
Dept/Division:
Abstract Title:
Category:
117
Diego Rodrigues
Coelho
Medicine: Endocrinology
NOS1-derived nitric oxide regulates NFκB activation
and macrophage polarization
Postdoctoral
Fellow
118
Flavio Romero
Palma
Medicine: Endocrinology
Use of chemogenetic systems and biosensors to
generate and sense H2O2 within organelles in live
cells: implications for epigenetics and cell biology
Postdoctoral
Fellow
119
Veronica Paviani
Medicine: Endocrinology
Effect of ROS in the mitochondrial metabolic changes
that promote macrophage polarization
Postdoctoral
Fellow
120
Kathryn Hendee
Pediatrics
Role of endothelial YAP1/TAZ signaling in lung
regeneration
Postdoctoral
Fellow
121
Megan Muyleart
Pediatrics
Effects of age-dependent changes in cell size on
endothelial cell growth through YAP1
Research
Support Staff
122
Kevin Jennings
Pediatrics, Microbiology
& Immunology
Growth Phase and Osmotic Stress Drive Subcellular
Localization of Enterococcus faecalis OGIRF_11271, a
Conserved Protein Involved in Cell Envelope Integrity
Student
123
Jesus J Ferre-
Fernandez
Pediatrics:
Developmental Biology
Insights of the role of FOXC1 gene in ocular
development using a double foxc1a/foxc1b knockout
zebrafish line
Postdoctoral
Fellow
124
Lisa Fraser
Pediatrics:
Gastroenterology
Succinate acts through tuft cells to stimulate Paneth
cell secretion
Postdoctoral
Fellow
125
Murtaza S Nagree
Pediatrics: Hem/Onc
SMA-Like Phenotype in a Mouse Model of Acid
Ceramidase Deficiency
Student
126
Tessa Miller
Radiation Oncology
Administration of pegylated-human growth factors
(PEG-HGF) and lisinopril for mitigation of acute
radiation syndrome
Research
Support Staff
127
Tracy Gasperetti
Radiation Oncology
Advancing a rat model of leg-out partial-body
irradiation for testing mitigators of ARS and DEARE
under the FDA Animal Rule
Research
Support Staff
128
Ying Zhang
Radiation Oncology
A Framework of Automatic Contour Quality
Validation for MRI-Guided Online Adaptive Radiation
Therapy
Clinical Fellows
& Residents

Research Day 2019
Jump to Table of Contents 18
Metabolism, Endocrine & Digestive
Poster #
1
Abstract Title:
Metabolic Effects Associated with Chronic Artificial Sweetener Consumption
Presenter(s):
Brian Hoffmann, PhD
Authors:
Dhanush Haspula, Mark Roethle, Martin Hessner, and Brian Hoffmann
Dept/Division:
Biomedical Engineering
Category:
Junior Faculty
Introductions:
As the diabetes epidemic grows worldwide, there is a heightened awareness of how modern day
diets may contribute to the increased incidence of disease. To combat the dietary intake of sugar,
there has been a drastic increase in the consumption of non-caloric artificial sweeteners (NCAS) in
everyday diets. However, a number of studies suggest that NCAS cause counterintuitive metabolic
derangements that may contribute to negative health outcomes. Conversely, there are limited
duration studies focused on weight management suggesting the opposite, thus creating
controversy. One confounding factor of studies in the field is that the NCAS are very biochemically
different, yet studies often generalize the compounds.
Methods:
Our study aimed to test the hypothesis that the chronic consumption of NCAS subtypes that are
absorbed intact will lead to distinct metabolic derangements that compound diabetes risk factors.
To test this hypothesis, we supplemented the diet of BioBreeding diabetes resistant (DR+/+) rats
with aspartame (metabolized) and acesulfame potassium (Ace-K+, not metabolized) for three
weeks in their drinking water. Weight, food intake, water intake, and blood glucose levels were
monitored throughout the study. At the end of the dietary supplementation untargeted and
targeted mass spectrometry-based metabolomics analysis were performed on plasma samples.
Further follow-up was performed in vivo using BioBreeding type 1 diabetes prone (DRlyp/lyp) rats
to measure the rate to onset and in vitro using at cardiac microvascular endothelial cells
(RCMVECs) to measure cardiometabolic effects.
Results:
BB-DR rats consuming the NCAS in the drinking water had a significant increase in blood glucose
versus the control group receiving normal water. Plasma metabolomics analysis revealed there
were distinct alterations in lipid and energy metabolism in the rats, with a greater effect resulting
from Ace-K+ consumption. It was also observed that Ace-K+ accumulated in the plasma of DR+/+
rats (21+10 µM; N=6). RCMVECs derived from Sprague-Dawley rats were treated with a dose-
response of Ace-K+ for up to three weeks and they exhibited impairment in the in vitro tube
formation, cell viability, and ROS (p<0.05; N=3). Through qPCR analysis, these same RCMVECs
displayed significant differences in insulin signaling, glucose metabolism, and inflammatory
regulatory genes (p<0.05; N=4). In further tests, we also observed that a chronic Ace-K+ diet
accelerated the rate of type 1 diabetes onset in the DRlyp/lyp rat model.
Conclusions:
Overall, results of this study suggests that the accumulation of absorbed NCAS have the potential
to lead to metabolic flux that may be important during the development of diabetes, especially in
genetically susceptible individuals.
Acknowledgements:
Support for this project was provided by NIH/NIDDK (DK105043 to BRH), the Mayo Clinic MRC
(pilot award provided by the U24DK100469 grant to BRH), and the Children’s Research Institute
(CRI19301, to MH).

Research Day 2019
Jump to Table of Contents 19
Metabolism, Endocrine & Digestive
Poster #
2
Abstract Title:
Elevated Levels of FGF21 In The Placenta of Macrosomic Infants
Presenter(s):
Katherine M Allen
Authors:
Katherine M Allen, Rachel K Harrison, MD; Aaron Naatz; Jennifer McIntosh, DO; John Corbett PhD;
Meredith Cruz, MD
Dept/Division:
Maternal Fetal Medicine
Category:
Student
Introductions:
Fibroblast growth factor 21 (FGF21) is a multifunctional protein implicated in disorders of
metabolic dysregulation and linked to childhood obesity. Previous studies demonstrated increased
FGF21 expression in the placenta women with gestational diabetes mellitus (GDM); however, it
has not been studied in relation to fetal weight at birth. Our aim was to investigate protein and
RNA expression of FGF21, FGF receptor 1 (FGFR1), and a transcription factor, peroxisome
proliferator-activated receptor alpha (PPARa), comparing macrosomic infants to those with
appropriate weight for gestational age at birth.
Methods:
Placental samples were obtained from the maternal surface of six term pregnancies complicated
by macrosomia and ten term uncomplicated appropriate for gestational age pregnancies. Women
were excluded if they delivered prematurely or had a diagnosis of preeclampsia. The subjects were
matched to controls based on mode of delivery and early pregnancy body mass index (BMI). Levels
of FGF21 and PPARa protein expression and FGF21 and FGF receptor mRNA expression were
measured via western blot analysis and RNA RT-PCR. Protein expression were normalized to
GAPDH levels from the same samples.
Results:
The baseline characteristics including maternal age, pre-pregnancy BMI, time from delivery to
procurement, and gestational age at delivery were statistically similar between groups. Fetal
weight was statistically different between the two groups (p=0.00026). There was no statistically
significant increase in levels of FGF21 mRNA or protein in the placentas of the macrosomic infants;
however, there is a trend toward higher levels (OR=2.14, p=0.6811
; OR=2.4, p=0.3001, respectively). In addition, we did not identify a statistically significant increase
in FGF receptor mRNA (OR=2.09, p=0.6768) and or PPARa, however, the trend is toward increased
levels of these in the placentas of macrosomic infants.
Conclusions:
Our data show no significant difference but a positive trend of increasing FGF21, FGFR1, and
PPARa protein expression in the placenta of macrosomic infants. There was also a positive trend of
higher FGFR1 mRNA expression.

Research Day 2019
Jump to Table of Contents 20
Metabolism, Endocrine & Digestive
Poster #
3 (NOT PRESENTING)
Abstract Title:
Serum Aminotransferases Level in Patients with Type 2 Diabetes Mellitus attending a Tertiary Care
Center, Kathmandu
Presenter(s):
Arjun Mainali
Authors:
Mainali A, Uprety N, Adhikari P, Pathak UN
Dept/Division:
Observer in Medical college of Wisconsin in the Department of Neurology ( Current)
Category:
Student
Introductions:
Nonalcoholic fatty liver disease is increasing with the rise in obesity and metabolic risk factors like
diabetes mellitus. Type 2 diabetics are highly prone to deranged liver function test. Increase in
serum aminotransferases level is an indicator of hepatocellular injury. The aim of this study is to
correlate serum aminotransferases level with anthropometric measurements, diabetic retinopathy
and types of treatment received in diabetics
Methods:
A total of 236 patients (142 females) of age more than 40 years with type 2 diabetes attending
Nepal Medical College and Teaching Hospital between February 2016 and January 2017 were
included in this cross-sectional observational study. Blood samples were sent for fasting blood
sugar, HbA1c, and serum aminotransferases tests. Body mass index and waist-hip ratio were
measured as per standard protocol. Fundoscopy was done in all patients. Pearson and
independent t-test were applied to see the correlation between the variables
Results:
The mean HbA1c was 8.01± 2.08. In the subgroup analysis, serum aminotransferases level was
significantly high in patients with poor glycemic control, higher body mass index and waist-hip
ratio (p-value < 0.001). Patients with diabetic retinopathy also had higher serum
aminotransferases level (p-value < 0.001). Pearson correlation between HbA1c with serum alanine
aminotransferases level was significant (r=0.76, n=5, p-value < 0.001).
Conclusions:
Serum aminotransferases level is high amongst diabetic patients with poor glycemic control and
with higher body mass index and waist-hip ratio and with the presence of diabetic retinopathy.

Research Day 2019
Jump to Table of Contents 21
Metabolism, Endocrine & Digestive
Poster #
4
Abstract Title:
The association between provider type and the choice of pharmacologic agent for treatment of
gestational diabetes
Presenter(s):
Rachel Harrison, MD
Authors:
Rachel Harrison, MD; Caroline Davitt; Ashley Wong; Meredith Cruz, MD; Anna Palatnik, MD
Dept/Division:
Obstetrics and Gynecology: Maternal-Fetal Medicine
Category:
Clinical Fellows & Residents
Introductions:
After failure of an initial trial of diet and exercise for gestational diabetes mellitus (GDM), insulin is
considered the preferred treatment as it does not cross the placenta and achieves strict metabolic
control. However, in many clinical situations oral hypoglycemic agents are prescribed as the first-
line pharmacotherapy. The objective of this study was to examine the association between the
type of provider and the choice of initial pharmacologic agent for women with GDM.
Methods:
This was a retrospective cohort study of women with a singleton pregnancy and diagnosis of
GDMA2 delivering in a single tertiary care center between May 2011 and April 2019. GDM was
diagnosed using Carpenter-Coustan two-step approach. Variables including maternal
demographics, GDM characteristics, and provider type (general OBGYN, Maternal-Fetal Medicine
(MFM) or endocrinology) were compared between women receiving insulin versus oral
hypoglycemic agent (metformin or glyburide) as the first-line pharmacologic agent using bivariable
and multivariable analyses.
Results:
Out of 422 women included in the analysis, 18% were managed by MFM, 54% by general OBGYN,
and 28% by endocrinology. 47.6% received insulin as a first line pharmacologic agent. Women
started on insulin were more likely to be older (32.6 vs 31.1 years, p=0.002), non-Hispanic white
race (68.6% vs 51.1%, p=0.003), privately insured (66.2% vs 50.0%, p<0.001), to have chronic
hypertension (8.3 vs 1.8%, p=0.002), and were more likely to be diagnosed at an earlier gestational
age (24.8 vs 26.3 weeks, p=0.012). Women who were started on insulin were also more likely to be
managed by an endocrinologist compared to MFM or general OBGYN (52.7% vs 16.4% vs 30.9%,
p<0.001). After adjusting for potential confounding variables, women with GDMA2 managed by
endocrinology were more likely to receive insulin for GDM (aOR 9.13, 95% CI 4.27-20.39).
Additionally, women without insurance were less likely to receive insulin than those with private
insurance (aOR 0.26, 95% CI 0.11-0.63).
Conclusions:
In this analysis women with GDMA2 who were managed by endocrinology were more likely to be
prescribed insulin as a first-line pharmacologic agent. Women without insurance were less likely to
receive insulin.
Reference 1:
American College of Obstetricians and Gynecologists. "Gestational diabetes mellitus. ACOG
practice bulletin no. 180." Obstetrics and Gynecology (July 2017)
Reference 2:
Langer, Oded, et al. "Gestational diabetes: the consequences of not treating." American journal of
obstetrics and gynecology 192.4 (2005): 989-997.
Reference 3:
Crowther, Caroline A., et al. "Effect of treatment of gestational diabetes mellitus on pregnancy
outcomes." New England Journal of Medicine 352.24 (2005): 2477-2486.

Research Day 2019
Jump to Table of Contents 22
Metabolism, Endocrine & Digestive
Poster #
5
Abstract Title:
Immunogenic Epitope Profiling in Fabry Disease Patients Undergoing Enzyme Replacement
Therapy
Presenter(s):
Simone Scalia
Authors:
Simone Scalia, Ju Huang, Lucía López-Vásquez, Murtaza S. Nagree, Gabrielle Geddes, Chien-Wei
Lin, Jeffrey A. Medin
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
Fabry disease (FD) is a rare genetic lysosomal storage disorder caused by deficiency of α-
galactosidase A (α-Gal A), an enzyme responsible for catabolism of globotriaosylceramide (GB-3).
Defects in α-galactosidase A result in GB-3 accumulation in cells throughout the body and multi-
system symptomatology. The standard-of-care for FD is enzyme replacement therapy (ERT). Two
ERTs are currently available for the treatment of FD, agalsidase α (aga α) and agalsidase Β (aga Β).
However, immune responses against these ERTs have been observed, and correlate with reduced
treatment efficacy. Herein we identify the immunoreactive epitopes associated with these
therapies. We hope to use these data to develop and evaluate novel, less immunoreactive, α-
galactosidase A proteins for ERT that could lead to improved therapy for FD.
Methods:
Anti-α-Gal A IgG titers were determined via ELISA in 23 aga α-treated FD patients, 21 aga Β-
treated FD subjects, and 6 non-treated (naÏve) FD individuals. Plasma from a healthy donor was
used to generate a standard curve and antibody levels were calculated as the fold-change in
absorbance in comparison to the healthy donor. Immunogenic epitopes were identified by
analyzing data collected by PEPperMAP technology. To test if mice have an analogous α-Gal A
immune-reaction, 2 Fabry mice were immunized with purified human α-galactosidase A in
complete Freund’s adjuvant. Plasma samples were analyzed via ELISA and PEPperMAP.
Results:
Anti-α-Gal A IgG titers were determined via ELISA in 23 aga α-treated FD patients, 21 aga Β-
treated FD subjects, and 6 non-treated (naÏve) FD individuals. Plasma from a healthy donor was
used to generate a standard curve and antibody levels were calculated as the fold-change in
absorbance in comparison to the healthy donor. Immunogenic epitopes were identified by
analyzing data collected by PEPperMAP technology. To test if mice have an analogous α-Gal A
immune-reaction, 2 Fabry mice were immunized with purified human α-galactosidase A in
complete Freund’s adjuvant. Plasma samples were analyzed via ELISA and PEPperMAP.
Conclusions:
We have profiled anti-α-Gal A immunoreactive epitopes generated by standard-of-care ERT
treatments for FD. High-titer patients share 5 strongly reactive epitopes, most of which were seen
in both aga α- and aga Β-treated patients. Low-titer patients displayed a more diverse set of
reactive epitopes. We also report that 3 of these 5 strongly reactive epitopes are seen in Fabry
mice immunized with human α-Gal A. Thus, we will use these mice for developing and evaluating
the immunoreactivity of novel variant α-Gal A modified to reduce immunogenicity, and thereby
improve outcome from ERT or future gene therapy based treatments for FD.
Reference 1:
Colomba P, Scalia S, Cammarata G, Zizzo C, Francofonte D, Savica V, Alessandro R, Iemolo F, Duro
G. Fabry disease, a complex pathology not easy to diagnose. Cardiogenetics, 2015 Vol.5 No.1, doi:
10.4081/cardiogenetics. 2015.5612.
Reference 2:
Deegan PB. Fabry disease, enzyme replacement therapy and the significance of antibody
responses. J Inherit Metab Dis. 2012 Mar;35(2):227-43.
Acknowledgements:
The authors would like to thank the patients, their families, and their physicians for participating
in this study. The authors also would like to thank past and present members of the Medin lab for
technical support and advice.

Research Day 2019
Jump to Table of Contents 23
Metabolism, Endocrine & Digestive
Poster #
6
Abstract Title:
Acid Ceramidase Deficiency Leads to Skin Inflammation and Impaired Adipogenesis in a Mouse
Model of Farber Disease
Presenter(s):
Rybova J
Authors:
Rybova J, Kuchar L, Oliveri R, Sikora J, Medin JRybova J
Dept/Division:
Pediatrics: Hematology/Oncology
Category:
Postdoctoral Fellow
Introductions:
Farber disease (FD) is a rare lysosomal storage disorder caused by mutations in the ASAH1 gene
that encodes acid ceramidase. Acid ceramidase is a lysosomal hydrolase that catalyzes the
degradation of ceramide into sphingosine and free fatty acid. Acid ceramidase deficiency leads to
lipid accumulation in many tissues, and resultant FD. Typical manifestations of classical FD include
formation of subcutaneous nodules, accumulation of joint contractures and development of a
hoarse voice [1]. Abnormal skin development has also been reported in FD patients but a detailed
study has not been performed. Here we conduct a pathophysiological study of the skin in a mouse
model of FD. We demonstrate altered lipid composition, storage of non-degraded lipid substrates
affecting mainly the dermis, and significant inflammation and impaired adipogenesis in the skin of
FD mice.
Methods:
The skin of 5- and 9-week-old FD and wild type mice were fixed in 4% PFA for histology and
ultrastructural analysis. Frozen skin was used for flow injection analysis combined with
electrospray ionization mass spectrometry of lipid species. Dermal fibroblasts and the stromal
vascular fraction of adipose tissue (SVF) were isolated from 5-week-old mice. Both types of cells
were used for differentiation into adipocytes and characterized by immunofluorescence and
OilRedO stain. Lysosomal and inflammatory proteins were evaluated by western blot analysis.
Results:
Increased accumulation of infiltrated macrophages and lysosomal protein Cathepsin D was
observed in FD dermis. Storage bodies in Schwann cells and peripheral cells of sebaceous glands
and outer root shafts of hair were also noticed. The observed pathology was more pronounced in
older FD mice. FD mice also displayed a reduction in adipocyte tissue in their hypodermis layer.
We also identified a wide spectrum of accumulated ceramide species (mainly with C16:0 and
C24:1 fatty acid) as well as sphingomyelin and ceramide monohexoside in the skin of FD mice.
Following several cell passages, fibroblasts isolated from FD mice showed reduced proliferative
capacity and strong vacuolization leading to cell death. Reduced proliferation was also observed
in mutant SVF. Compared to WT and fibroblast-derived adipocytes, only SVF-derived adipocytes
from FD mice showed reduced positivity for adipocyte marker Adiponectin, and reduced OilRedO
fat staining. Fibroblast- and SVF-derived adipocytes from FD mice showed increased accumulation
of inflammatory (Stat3, NF-kB) and lysosomal (LAMP1, Cathepsin D) proteins.
Conclusions:
Using our FD mouse model, we demonstrate profound biochemical and structural pathology in
skin cells of acid ceramidase deficient mice. Interestingly, only SVF showed impaired adipocyte
differentiation in FD mice suggesting the possible involvement of acid ceramidase in adipocyte
tissue development. We will next study the transcriptional regulation of adipogenesis in these
mice.
Reference 1:
Yu F: Orphanet Journal of Rare Diseases, 2018

Research Day 2019
Jump to Table of Contents 24
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
7
Abstract Title:
Shoulder ROM in Youth Baseball Pitchers: Pain vs. No Pain
Presenter(s):
Gunnar Whealy, BS
Authors:
Gunnar Whealy, BS; Justin Ling-LeBlanc, BS; Ghulam Mujtaba, BS; Xue-Cheng Liu, MD, PhD;
Shayne Fehr, MD
Dept/Division:
Orthopaedic Surgery
Category:
Student
Introductions:
Baseball participation in America is at an all time high with 6.7 million children aged 6-17 year old
playing annually, making it the most popular youth sport. Pitching injuries, however, are also
increasing. Previous studies have identified multiple causes for these injuries including improper
mechanics, culture of “playing through pain”, and number of pitches thrown. Research is lacking
regarding ways to identify players at risk. Thus, our study aims to determine (1) average internal and
external rotation range of motion (ROM) in a pediatric pitching population, (2) if history of throwing
injuries (non-surgical) or pain is related to increased and easily identifiable differences in joint ROM.
Methods:
IRB approval was granted prior to the study. Informed consent and assent were obtained for each
subject. 52 male pitchers between the ages of 9 and 14 years old were recruited from Milwaukee
metro-area baseball clubs. Participants completed a questionnaire indicating current elbow or shoulder
pain or if they have had an arm injury or pain that has kept them out of at least one practice or game in
the past year. An exam was then conducted to obtain anthropometric data for each subject which
includes height, weight, BMI. A licensed physical therapist (blinded to pain category) measured
maximum passive internal and external rotation angles of the shoulder with the shoulder at 90-90
abduction/flexion. Joint mobility was assessed using the Beighton hypermobility scale. Subjects were
stratified into two groups, those that had experienced pain, and those that did not, and were
compared via unpaired two-tailed heteroscedastic t-test. BMI-for-age percentile was calculated using
the CDC growth chart calculator. Exclusion Criteria: Children who have fractured a bone in their
throwing arms that required surgery, sustained ligament tears or other injuries in their throwing arms
that required surgery, have current arm pain were excluded from the study.
Results:
External rotation was greater in the dominant arm compared with the non-dominant arm (p<0.01).
Internal rotation was reduced in the dominant arm when compared with the non-dominant arm
(p<0.01). There was no significant difference between pain and no-pain groups when evaluating
maximal passive range of motion in either arm. Beighton hypermobility score between pain and no
pain groups was not significant (p=0.25). BMI-for age percentile between pain and no pain groups was
not significant (p=0.14). Total range of motion between pain and no pain groups was not significant
(p=0.05).
Conclusions:
Contrary to our initial hypothesis, this study suggests that there is not a strong association between
upper extremity passive range of motion, and history of debilitating injury or pain in the past year.
Interestingly, we found that players could achieve greater external rotation in their dominant arms, but
less internal rotation compared to their non-dominant arms regardless of history of pain. Further
studies should investigate if this could be due to musculoskeletal remodeling secondary to the
repeated pitching motion. Limitations of this study include limited sample size, age range, and
exclusively male gender participants. Further studies should compare pitchers to a non-pitcher
population to further develop generalizability to broader populations. Variation exists in passive range
of motion between dominant and non-dominant arms in male youth baseball pitchers. Measuring
external and internal rotation has poor utility for identifying history of arm pain in male youth baseball
pitchers.
Acknowledgements:
Glenn, Kedric, MD; Damrow, Derek S, MD; Hadro, Adam E, MD; Apolinario, Michael A, MD; Newlin,
Susan; Brian Butler; Dept of Orthopaedic Surgery

Research Day 2019
Jump to Table of Contents 25
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
8
Abstract Title:
Knee Arthrofibrosis Following Tibial Plateau Fracture Treated with Arthroscopic Lysis of Adhesions
with Manipulation
Presenter(s):
Madeline Perlewitz
Authors:
Austin Middleton, Madeline Perlewitz, Adam Edelstein, Carole Vetter
Dept/Division:
Orthopaedic Surgery
Category:
Student
Introductions:
Post-traumatic arthrofibrosis of the knee is a common problem after operative management of tibial
plateau fractures, with a reported incidence as high as 12% (1). The optimal treatment strategy has
not been defined. The purpose of this study is to quantify the efficacy of arthroscopic lysis of
adhesions with manipulation for the treatment of arthrofibrosis of the knee in patients that have
undergone operative repair of a tibial plateau fracture.
Methods:
The records of all patients that underwent arthroscopic lysis of adhesions with manipulation of the
knee by a single surgeon since 2001 were retrospectively reviewed. Patients were included if they
had developed arthrofibrosis secondary to open reduction internal fixation (ORIF) of a tibial plateau
fracture and failed conservative management. Charts were reviewed for demographic information
and historical information including date of injury, prior interventions, and diagnosis at the time of
lysis. Knee extension, flexion and total range of motion (ROM) were recorded preoperatively,
intraoperatively, and postoperatively at intervals of 1 week, 4 weeks, 8 weeks, 12 weeks, and any
additional follow-ups. Total ROM was compared at the different time intervals using paired-sample
t-tests. A general linear regression model was used for multivariate analysis to determine predictors
of changes in flexion and extension. All results are considered significant at the 0.05 level.
Results:
A total of 28 patients (15 male, 13 female) with an average age of 44.0 years and BMI of 26.2 kg/m2
were included in the analysis. Mean time since index open reduction internal fixation (ORIF) was 5.8
months. 19 patients underwent external fixation prior to ORIF, with an average duration of 17 days
(min 5, max 34). The average preoperative range of motion was 57.7 degrees. There were significant
improvements in ROM following intervention at all time points compared to preoperative values
(p<0.00001), with mean improvements of 59.4  13.7 degrees intraoperatively, 34.1  23.4
degrees at 1 week, 39.4  19.5 degrees at 4 weeks, 37.9  31.9 degrees at 8 weeks, and 43.2 
33.5 degrees at 12 weeks. At 4 and 12 weeks postoperatively, increased external fixation duration
was associated with greater increases in ROM (p=0.017, p=0.048). Further, at 1 and 4 weeks
postoperatively, increased time since index ORIF was associated with smaller increases in ROM
(p=0.005, p=0.003). 4 patients required revision lysis of adhesions for failure to achieve adequate
range of motion. At final followup of revision lysis of adhesions, motion increased by a mean of 25.3
degrees, though this was not significant (p=0.23).
Conclusions:
Arthroscopic lysis of adhesions with manipulation for knee arthrofibrosis following operative
management of tibial plateau fractures provides a sustained and significant improvement in knee
range of motion.
Reference 1:
Reahl GB, Marinos D, O’Hara NN, et al. Risk Factors for Knee Stiffness Surgery After Tibial Plateau
Fracture Fixation: J. Orthop. Trauma. 2018 Sep;32(9):e339-e343.

Research Day 2019
Jump to Table of Contents 26
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
9
Abstract Title:
Arthroscopic Lysis of Adhesions with Manipulation for Management of Resistant or Late Presenting
Arthrofibrosis Following Total Knee Arthroplasty
Presenter(s):
Michael Ziegele
Authors:
Austin Middleton , Michael Ziegele, Adam Edelstein, Carole Vetter
Dept/Division:
Orthopaedic Surgery
Category:
Clinical Fellows & Residents
Introductions:
Arthrofibrosis is a known complication of total knee arthroplasty (TKA) with significant implications
on post-operative function. Closed manipulation is the treatment of choice for arthrofibrosis
identified within 90 days of TKA. Treatment for arthrofibrosis that has failed prior interventions or
that presents beyond 90 days remains controversial.
Methods:
A retrospective analysis was performed of patients that underwent arthroscopic lysis of adhesions
(LOA) with manipulation for post-TKA arthrofibrosis. Patients were excluded if they underwent
arthroscopic LOA for an indication other than stiffness or decreased range of motion following TKA.
Charts were reviewed for patient characteristics, time from TKA, prior interventions, and range of
motion data. Extension, flexion, and total range of motion were recorded preoperatively,
intraoperatively, and throughout followup at specified intervals. Extension and flexion were
compared at the different time intervals using Wilcoxon signed-rank tests.
Results:
A total of 13 patients (6 male /7 female) with mean age of 66.3 years were included. Average time
since index TKA was 35.6 months (3.7 - 209.5). 10 of 13 patients had undergone prior interventions
for arthrofibrosis, which included prior closed MUA, open LOA, and revision arthroplasty. Mean
preoperative knee flexion and extension values for the cohort were 76.5  17.4 and -4.6  6.1
degrees respectively. Post-operative improvements in knee flexion were significant at all time
points compared to preoperative values, with mean improvements of 14.7  15.5 degrees at 1
week (p=0.011), 14.4  14.3 degrees at 4 weeks (p=0.007), 17.0  14.9 degrees at 8 weeks
(P=0.012), and 24.2  13.2 degrees at 12 weeks (p=0.031). There were no complications.
Conclusions:
Arthroscopic lysis of adhesions with manipulation achieves significant improvements in knee ROM
for treatment-refractory or late-presenting arthrofibrosis after TKA.

Research Day 2019
Jump to Table of Contents 27
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
10
Abstract Title:
Targeted Muscle Reinnervation in Rat Spared Nerve Injury Models Neuropathic Amputation-
Related Pain Relief
Presenter(s):
Gwendolyn Hoben
Authors:
Elizabeth Roth BS, Cheryl Stucky PhD, Quinn Hogan MD, Gwendolyn Hoben MD PhD
Dept/Division:
Plastic Surgery
Category:
Junior Faculty
Introductions:
The success of targeted muscle reinnervation (TMR) in preventing or relieving amputation-related
neuropathic pain has been well shown in clinical studies. However, many questions remain about
the changes in pain pathways and neuronal regeneration induced by TMR. These questions are
most readily answered in an animal model. Pre-clinical animal studies using amputation are
problematic as limb sensation and stimulation-related pain behaviors cannot be tested,
precluding assessment of pain. We hypothesize TMR can be used to treat neuropathic pain that
follows peripheral nerve transection in the spared nerve injury model, a robust, well-validated
model of neuropathic pain. This model retains the limb, which allows for standard rodent pain
behavior testing.
Methods:
Spared nerve injury was performed in male rats by unilaterally ligating the common peroneal and
tibial nerves. After 3 weeks, the rats developed a robust and consistent neuropathic pain
phenotype and two interventions were studied: 1. TMR: the neuromas were excised and the
animals underwent coaptation of the common peroneal and tibial nerves to nerve branches to
the biceps femoris; and 2. Neuroma Excision (NE): the neuromas were excised and the muscle
branches divided but no coaptations were performed. The plantar skin in the sural distribution
was tested with von Frey threshold, pin touch hyperalgesia, and hypersensitivity to dynamic
mechanical stimulation (brush), acetone (cold), and heat (Hargreaves) to characterize pain
behavior prior to intervention and at 1 and 3 weeks following intervention. The healthy
contralateral limb was tested as an internal control.
Results:
The spared nerve injury caused a robust pain phenotype with increased hyperalgesic responses,
reduced Von Frey thresholds, and increased cold sensitivity. One week after TMR, pain behaviors
were significantly changed compared to pre-intervention pain measures, while pain measures did
not change in the NE group. In the TMR group, hyperalgesia responses to pin were reduced 80%
within 1 week following TMR but did not change significantly following NE. Von Frey thresholds
returned to the baseline following TMR but remained significantly elevated in the NE group. There
was also a trend to reduced cold hypersensitivity in the TMR group.
Conclusions:
This rodent model mirrors the clinical results found in TMR and allows for measurement of
allodynia, hyperalgesia, and sympathetic-related pain behavior changes. This model will allow for
determining the underlying mechanisms at the dorsal root ganglion and axonal levels responsible
for the clinical outcomes of TMR surgery.
Acknowledgements:
Many thanks to the Neuroscience Research Center, the Department of Anesthesiology, the Stucky
lab group, Nicole Newkirk, and Ashley Schamerhorn.

Research Day 2019
Jump to Table of Contents 28
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
11
Abstract Title:
Changes in the Enteric Serotonin Signaling System Following Low Anterior Resection
Presenter(s):
Timothy Ridolfi, MD
Authors:
Katherine Hu, MD; Jacqueline Blank, MD; Alex Dombeck. BS; Carrie Peterson MD, MS; Kirk Ludwig,
MD; Timothy Ridolfi, MD
Dept/Division:
Surgery: Colorectal Surgery
Category:
Senior Faculty
Introductions:
Low anterior resection syndrome (LARS) is common following rectal resection and linked to post-
operative quality of life. Animal models have demonstrated changes in serotonin signaling that
have been postulated to cause LARS, but this has not been evaluated in humans. The objective of
this study was to identify alterations in the serotonin signaling pathway of the enteric nervous
system after low anterior resection (LAR), and to correlate these changes with post-operative
bowel function.
Methods:
This was a prospective cohort study conducted between October 2015 and September 2017.
Adult patients with rectal cancer who underwent LAR with stapled anastomosis were included.
Colonic biopsy samples were taken at time of initial surgery, loop ileostomy reversal, and one-
year surveillance colonoscopy. Expression of serotonin transporter (SERT), 5-HT3, and 5HT-4
receptors were measured and correlated to bowel function. Bowel function was assessed using
the Memorial Sloan Kettering Bowel Function Index preoperatively and at each subsequent clinic
visit.
Results:
There was a pattern of initial decrease, followed by partial recovery, seen in all patients for 5-
HT3a, 5-HT4, and SERT expression. Bowel function was inversely correlated with recovery of SERT
expression (Spearman rho -0.89, p=0.02). There was no significant correlation between 5-HT3a
and 5-HT4 expression and bowel function.
Conclusions:
Following LAR, there was change in serotonin receptor expression, with a pattern of initial
decrease followed by partial recovery of serotonin receptors. Those with largest recovery of the
SERT protein demonstrated the worst post-operative bowel function.

Research Day 2019
Jump to Table of Contents 29
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
12
Abstract Title:
Alvimopan use in the setting of Abdominoperineal Resection: a retrospective cohort study
Presenter(s):
Katherine Hu, MD
Authors:
Katherine Hu, MD; Rachel Henning, BA; Lisa Rein, MS; Aniko Szabo, PhD; Carrie Peterson, MD; Kirk
Ludwig, MD; Timothy Ridolfi, MD
Dept/Division:
Surgery: Colorectal Surgery
Category:
Clinical Fellows & Residents
Introductions:
Alvimopan is a peripherally acting u-opioid antagonist designed to reverse opioid-induced side
effects on gastrointestinal function without compromise of pain relief. It is indicated for patients
undergoing bowel resection with primary anastomosis and has been demonstrated to reduce
length of stay and cost after colon resection surgeries. Alvimopan is commonly included in
institutional enhanced recovery protocols, thus some patients receive the drug after
abdominoperineal resection (APR) despite a lack of bowel anastomosis. Our study aims to
evaluate the clinical impact of alvimopan in patients undergoing APR in a national cohort.
Methods:
This was a retrospective cohort study of data from a national administrative database. Using ICD-9
codes, we queried the Vizient Clinical Database for all patients undergoing laparoscopic and open
APR between 1/1/2015 and 06/30/2017. Patients were stratified into laparoscopic and open
procedures for descriptive statistics. The association between alvimopan use and other variables
was assessed with Chi-square and Kruskal-Wallis tests. Multivariate linear regression was
performed with length of stay (LOS) as primary outcome of interest.
Results:
Of the 759 patients who met inclusion criteria, 426 (56.1%) underwent open and 333 (43.9%)
underwent laparoscopic APR. Alvimopan was given to 165 (21.7%) total patients and overall was
associated with decreased mean LOS (6.9 vs 8.6 days, p<0.01). In patients undergoing
laparoscopic APR, 70 (21.0%) received alvimopan, with an associated decrease in mean LOS from
5.5 to 7.1 days, p<0.01). After adjusting for comorbidities using Elixhauser comorbidity index,
multivariate linear regression demonstrated alvimopan was associated with a 15% decrease in
LOS (effect ratio 0.85, p=0.04). In the open APR group, 95 (22.3%) received alvimopan, which was
associated with decreased mean LOS (7.8 vs 9.8 days, p<0.01). After adjusting for comorbidities,
alvimopan was associated with a 7% decrease in LOS (effect ratio 0.93, p=0.33), though this did
not meet statistical significance.
Conclusions:
The use of alvimopan is associated with reduction in LOS for patients undergoing laparoscopic
APR. In open APR patients, alvimopan was also associated with decreased LOS, but did not meet
statistical significance after adjusted multivariate analysis. It is possible that the findings in the
open APR group were confounded by diversity of the patient population, as these patients are
more likely to undergo complex procedures, such as flap reconstruction or pelvic exenteration,
that may contribute to increased length of stay. A randomized controlled trial may be warranted
to evaluate if alvimopan provides benefit to patients undergoing APR.
Research Day 2019
Jump to Table of Contents 30
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
13
Abstract Title:
A Bridge to the Fridge? Changes in BMI Post Left Ventricular Assist Device Implant
Presenter(s):
Richard W. Walsh
Authors:
Richard W. Walsh, Sakthi K. Sundararajan, MD, David L. Joyce, MD & Asim Mohammed, MD
Dept/Division:
Surgery: Division of Cardiothoracic Surgery
Category:
Student
Introductions:
Weight gain after left ventricular assist device (LVAD) implant may result in transplant listing loss in
obese patients. We studied weight changes post LVAD amid BMI categories based on the hypothesis-
changes in BMI impact transplant candidacy.
Methods:
We received IRB approval and subsequently performed retrospective review on patients of LVAD
implant at an academic medical center between 1/1/2012 and 12/31/2018. We collected demographic
and clinical data, then stratified them into 4 groups based on BMI at implantation: < 30, 30-35, 35-40,
and > 40. BMI data was collected at 12 and 6 months prior to implant, time of implant, and post
implant at 3 and 6 months. A BMI cutoff >35 provided contraindication for transplant listing candidacy.
Descriptive summary of variables was given with median and range or group frequency and
percentages or mean and standard deviation. Scatter plot visualized correlation between weight
difference changes over time. Additional lines overlaid on the plots indicate correlation trend. Mixed
effects model was performed to estimating associations between weight difference and variables
(time, BMI Implant). Bar plots were performed displaying move from <35 BMI at time of implant to
>35 BMI after 6 months post LVAD and the move from >35 BMI at the time of implant to <35 BMI after
6 months post LVAD.
Results:
A total of 108 patients underwent LVAD implant at our center with complete data available for 59
patients. Baseline characteristics include mean age: 56.0 +/- 11.9, 69.4% male, mean implant BMI:
30.1 +/- 6.9, Number of patients in each implant BMI group (<30, 30-35, 35-40, and >40) is 30, 16, 9,
and 4 respectively. There was no consistent pattern with weight change across differing implant BMIs.
Among patients with implant BMI’s of <30, 30-35, 35-40, and >40, the percentage that lost transplant
candidacy due to high BMI were 0, 31, 55, and 100 percent respectively.
Conclusions:
Patients with a BMI within 5 points of the typical threshold of 35 for transplant candidacy demonstrate
significant variability in response to LVAD therapy. However, all patients with implant BMIs >40 failed
to regain transplant candidacy due to high BMI. These data support the concept of implementing
aggressive weight loss protocols as a standard of post LVAD treatment in obese patients.
Reference 1:
Inotrope Dependent End Stage Heart Failure: Testing the Obesity Paradox Bahrami, Mubashir H. et
al. Journal of Cardiac Failure, Volume 23, Issue 8, S106 - S107
Reference 2:
Bariatric Surgery as a bridge to Cardiac transplantation in patients with LVAD Pullatt, Rana et al.
Surgery for Obesity and Related Diseases, Volume 14, Issue 11, S121 - S122
Reference 3:
Amanda R. Vest, Angelo DeNofrio, Alexandra Coston, Sakthi K. Sundararajan, Matthew Lawrence,
Nathan G. Yuen, Lauren Parsly, Michael S. Kiernan, David DeNofrio, Gregory Couper, Edward Saltzman,
Impact of Early Weight Changes after Left Ventricular Assist Device Implantation on Subsequent
Survival, Journal of Cardiac Failure, Volume 24, Issue 8, Supplement, 2018, Page S18, ISSN 1071-9164
Acknowledgements:
A big thank you and appreciation to all those that help with the cardiac surgery research group that
Dr. David Joyce leads, especially the other physicians that offer suggestions and knowledge in the
group. Thank you also to Dr. Paul Linsky, my pathway advisor for his input on my career and for
introdcing me to the research groupThank you to my loving family for their support in my medical
career

Research Day 2019
Jump to Table of Contents 31
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
14
Abstract Title:
Are Patients with Gender Dysphoria Counseled on Fertility Preservation Prior to Hormonal
Therapy Initiation?
Presenter(s):
Bryce Toburen
Authors:
Ross G Everett, MD MPH, Bryce A Toburen, BA, Kaylee M Luck, BS, Johnathan Doolittle, MD and
Jay I Sandlow, MD
Dept/Division:
Urology
Category:
Student
Introductions:
Introduction: National guidelines recommend counseling patients with gender dysphoria on the
impacts of hormone or surgical therapy on their fertility prior to beginning either intervention. In
this study, we aim to identify the compliance to these guidelines at our institution.
Methods:
Methods: Utilizing ICD codes, we identified patients with a diagnosis of gender dysphoria [GD]
treated at our institution between 2008-2018. Various parameters regarding medication
regimen, surgical intervention, fertility counseling, and fertility preservation were obtained
through retrospective review. Patient demographics and interventions were compared. All data
was analyzed in a standard statistical fashion utilizing Stata software.
Results:
Results: Upon review, 269 patients met inclusion criteria. Of these, 114 (42.4%) had a
chromosomal sex of female and 155 (57.6%) were chromosomal males. Race was divided as
75.5% White, 16.7% Black and 7.8% Other. The average age was 30.9 (S.D.±13.7). Regarding
management of GD, 171 (63.6%) had been managed by Endocrinology, 118 (43.9%) by
Gynecology, and 25 (9.3%) had seen Urology. 74 patients (27.5%) ultimately pursued some
surgical intervention. 97 patients (36.1%) were on hormonal therapy for GD prior to evaluation at
our institution and were excluded from subsequent analysis. Another 26 patients did not have
record of pursuing hormonal therapy to date. Of the remaining 146 patients, 96 (65.8%) had
documented counseling regarding fertility. On chi-square tests, age was the only demographic
found to be significantly different between those counseled on fertility and those not.
Additionally, on multinomial logistic regression, individuals ‰¤30 years were significantly more
likely to be counseled regarding fertility than those 31-50 years (RR 2.45, p=0.049) and those 51+
years (RR 5.47, p=0.013). Factors such as race, chromosomal sex, and managing specialty were
not found to be predictive. Among those patients ‰¤30 years of age, 71 of 98 (72.5%) were
counseled regarding fertility preservation.
Conclusions:
Conclusion: Compliance with national guidelines to counsel GD patients on fertility preservation
is best among younger patients, most notably those less than or equal to 30 years of age. This
appears consistent among patients of both chromosomal sexes and across different managing
specialties. Further research is needed regarding other risk factors for poor counseling as well as
to predict those patients who will be interesting in fertility preservation.

Research Day 2019
Jump to Table of Contents 32
Surgery, Ophthalmology, Otolaryngology & Orthopaedics
Poster #
15
Abstract Title:
IMPACT OF BILATERAL ORCHIECTOMY IN REDUCTION OF HORMONE MEDICATION REGIMEN IN
GENDER DYSPHORIA
Presenter(s):
Kaylee Luck
Authors:
Ross Everett, Kaylee Luck, Jay Sandlow
Dept/Division:
Urology
Category:
Student
Introductions:
The regimens of hormonal therapy for transgender females are more complex than those used
in transgender males.1 Androgens are insufficiently suppressed merely by the supplementation
of estrogen.1 Consequently, androgen reducing medications are often given to suppress
testosterone levels and reduce the dosage of exogenous estrogens required as part of
therapy.2,3 Bilateral orchiectomy [BO] is utilized as an alternative means of castration to reduce
the magnitude of hormone medication in transwomen with gender dysphoria [GD].4 However,
few reports exist which report the actual changes in hormonal medication regimen that
accompany BO. The objective of this study was to assess the impact of BO on the hormone
regimen of patients with GD.
Methods:
Individuals who underwent BO as part of their GD treatment were included in our study. Various
parameters including medication regimen and hormone levels were obtained through
retrospective review. Patient demographics and interventions were compared. All data was
analyzed in a standard statistical fashion.
Results:
Fourteen patients underwent BO as part of their treatment for GD. These patients met criteria
for BO as established by The World Professional Association for Transgender Health [WPATH]
guidelines. Median age at time of surgery was 44 years (IQR 36.5-53.3). Pre-operative and post-
operative medication regimens were available for eight patients. Of these, seven (88%) were
treated pre-operatively with spironolactone and two (25%) with finasteride. Post-operatively, six
patients (86%) were noted to have cessation of spironolactone and one patient (50%) for
finasteride. Three (38%) had reduced their exogenous estrogen supplementation. Median time
of follow-up available after surgery was 16.5 (IQR 9.8-27.8) months.
Conclusions:
BO is an effective means of negating the need for ongoing androgen reducing medication for the
majority of transgender female patients with 86% of patients stopping spironolactone post-
operatively. Additionally, 38% reduced the amount of exogenous estrogen they used. Further
research is needed to delineate improved treatment protocols for these patients after surgery.

Research Day 2019
Jump to Table of Contents 33
Population, Community Health & Outcomes
Poster #
16
Abstract Title:
1 / 1 The Relationship between C-Reactive Protein and Mortality in Adults with Diabetes:
Influences of Demographic Characteristics, Lifestyle Behaviors, and Medications
Presenter(s):
Olaitan Akinboboye
Authors:
Olaitan Akinboboye, Joni S. Williams, MD, MPH, Emma Garacci, MS, Leonard E. Egede, MD, MS
Dept/Division:
CAPS
Category:
Student
Introductions:
Evidence suggests a relationship exists between C-reactive protein (CRP) and mortality in
individuals with diabetes. However, the influence of factors such as demographics and lifestyle
and medications on this relationship remain unclear. Therefore, this study will analyze the
association between CRP and mortality in a national sample of adults with diabetes.
Methods:
This is a cross-sectional study of data from 1999-2010 National Health and Nutrition Examination
Survey (unweighted n= 3,952; Weighted n= 19,064,710). Individuals were categorized as having
diabetes if told by a doctor or other health professional they had diabetes, were taking insulin or
any other diabetes medications, or had a glycosylated hemoglobin A1c (HbA1c) ‰¥ 6.5%. Serum
CRP samples were analyzed by latex-enhanced nephelometry, and CRP concentrations were
calculated by using a calibration curve. Covariates included age, gender, race/ethnicity, education,
marital status, ratio of family income to poverty, physical activity, smoking, alcohol intake, and
diabetes medications (insulin and metformin). A multivariate logistic regression was used to
assess the influence of demographics, lifestyle behaviors, and diabetes medications on the
association between CRP and mortality.
Results:
Approximately 49% of the sample of adults with diabetes were females, with an average age of
50-69 years. After adjusting for covariates, adults with a very high-risk level of CRP (>1.0 mg/dL)
had a higher risk of mortality (HR=1.84 (95% CI: 1.25 - 2.71) compared to individuals with normal
CRP risk level (<=0.1 mg/dL). Non-Hispanic Blacks and Others had a lower risk of mortality
((HR=0.83 (95% CI: 0.67-1.04) and HR=0.68 (95% CI: 0.52-0.90), respectively) compared to non-
Hispanic Whites. Adults 70 years of age and older had a higher risk of mortality (HR=7.57 (95% CI:
4.47-12.82)) compared to those age 20-49 years. Adults on insulin had a higher risk of mortality
(HR=1.66 (95% CI: 1.29-2.13) compared to those not using insulin.
Conclusions:
In this sample of adults with diabetes, demographic and lifestyle factors and medications had an
influence on the association between CRP and mortality. Targeted interventions should focus on
these factors to reduce mortality in adults with diabetes.

Research Day 2019
Jump to Table of Contents 34
Population, Community Health & Outcomes
Poster #
17
Abstract Title:
Assessing the Relationship between Lifetime, Daily, and Chronic Job Discrimination and Mortality
in a Nationally Representative Sample of Adults
Presenter(s):
Joanna Obaoye
Authors:
Joanna Obaoye, BS; Joni S. Williams, MD, MPH; Aprill Z. Dawson, PhD, MPH; Madhuli Thakkar,
MPH; Leonard E. Egede, MD, MS
Dept/Division:
CAPS
Category:
Student
Introductions:
Discrimination is the unfair or differential treatment of individuals or communities, which is based
on prejudice against a defining characteristic of that group. The literature shows a link between
discrimination and mortality, in that higher levels of perceived discrimination is associated with
increased risk of mortality. However, most of these studies focused on daily or lifetime
experiences of racial discrimination and did not assess the influence of lesser studied forms of
discrimination such as chronic job discrimination. The aim of our study was to assess the
relationship between mortality and perceived discrimination in a nationally representative sample
of adults.
Methods:
We conducted a survival analysis of 5,555 adults using Wave 2 of the Midlife in the U.S. (MIDUS)
dataset. The outcome variable was mortality, and the predictor was perceived discrimination
(lifetime, daily, chronic job). Covariates included predisposing (age, sex, race/ethnicity, education,
marital status), enabling (income, employment status, insurance), and need factors (Body Mass
Index, high blood pressure, diabetes, stroke, cancer). Cox regression models were used to assess
the relationship between mortality and lifetime, daily, and chronic job discrimination, adjusting
for predisposing, enabling, and need factors.
Results:
In this sample, 81%, 82%, and 53% of adults reported perceived lifetime, daily, and chronic job
discrimination, respectively. The mean age of the sample was 55 years, and 46% were men.
Nearly 80% of the sample was Non-Hispanic White, 15% was Non-Hispanic Black, and 3% was
Hispanic. Approximately 37% made less than $25,000 annually. In unadjusted analyses, lifetime
perceived discrimination was statistically associated with mortality (Hazard Ratio (HR): 0.94;
p=0.032). After fully adjusting for predisposing, enabling, and need factors, there was a 9%
increased risk of mortality with perceived lifetime discrimination (HR: 1.09, p=0.034) and a 3%
increased risk of mortality with perceived daily discrimination (HR: 1.03, p=0.030). There were no
significant associations between chronic job discrimination and mortality.
Conclusions:
In this sample of adults, lifetime and daily discrimination significantly increased the risk for
mortality, after adjusting for predisposing, enabling, and need factors. Our findings support the
existing literature regarding discrimination and mortality. Future research should aim to explore
which aspects of lifetime and daily discrimination most explain the relationship with mortality, in
addition to establishing the mechanism by which discrimination increases risk of mortality.
Acknowledgements:
Support received by grants UL1TR001436 from the Clinical and Translational Award (CTSA)
program of the National Center for Research Resources and the National Center for Advancing
Translational Sciences and the National Institute of Diabetes and Digestive Kidney Diseases- NIH-
NIDDK 1R25 DK098104-05 grant

Research Day 2019
Jump to Table of Contents 35
Population, Community Health & Outcomes
Poster #
18
Abstract Title:
Chronic Disease Risk and Onset in Adults with a History of Incarceration
Presenter(s):
Oluwatoyin Olukotun, PhD, RN
Authors:
Oluwatoyin Olukotun, PhD, RN; Joni S. Williams, MD, MPH; Zhipeng Zhou, MS; Leonard E. Egede,
MD, MPH
Dept/Division:
CAPS
Category:
Postdoctoral Fellow
Introductions:
There is growing interest in the impact of incarceration on health. However, little is known about
how incarceration impacts chronic disease risk and chronic disease onset. Therefore, the aim of
this study was to assess the relationship between history of incarceration and chronic disease risk
and history of incarceration and onset of chronic disease.
Methods:
This was a longitudinal study of 12,686 adults from the National Longitudinal Survey of Youth
(NLSY) 1979 dataset. History of incarceration was the predictor and defined as any episode of
incarceration in a correctional institution. Generalized Estimating Equation (GEE) model was used
to assess the relationship between incarceration and risk of developing congestive hypertension,
diabetes, stroke and heart disease. Cox Proportional Hazard model was used to examine the
relationship between incarceration and onset of congestive heart failure, hypertension, or
diabetes. Hierarchical models were run in blocks, first for demographic variables (age, race,
gender, geographic region, marital status), second for lifestyle and clinical variables (drug use,
binge drinking, Body Mass Index, early life health limitation) and lastly, for socioeconomic
variables (poverty status, employment status and educational attainment).
Results:
In unadjusted analyses, a history of incarceration was significantly associated with an increased
odds of heart disease (OR 4.13; CI 2.19, 7.28; p<0.001). This relationship persisted after adjusting
for demographic (OR 3.44; CI 1.78, 6.65; p<0.001) and lifestyle and clinical factors (OR 3.21; CI
1.64, 6.32; p=0.001). However, after adjusting for socioeconomic factors, the relationship
between incarceration and heart disease was no longer significant (OR 1.97; CI 0.99, 3.92;
p=0.055). There were no significant relationships between history of incarceration and risk for
diabetes (OR -0.70; p=0.103), hypertension (OR 0.47; p=0.116), or stroke (OR 0.61; p=0.351) and
onset of congestive heart failure (HR 2.16; p=0.980), hypertension (HR 1.09; p=0.326), or diabetes
(HR 0.75; p=0.097).
Conclusions:
In this sample of adults, a history of incarceration was significantly associated with an increased
risk for heart disease, after adjusting for demographic, lifestyle and clinical factors, but not after
adjusting for socioeconomic factors. These findings suggest socioeconomic factors such as
educational attainment and employment status may explain the relationship between
incarceration and heart disease. Therefore, interventions to decrease heart disease risk in adults
with a history of incarceration should target employment and educational opportunities.
Additionally, more research is needed to elucidate the mechanisms through which incarceration
impacts cardiovascular health.

Research Day 2019
Jump to Table of Contents 36
Population, Community Health & Outcomes
Poster #
19
Abstract Title:
Investigating Racial/Ethnic Disparities in Cognitive Decline for Older Adults with Diabetes
Presenter(s):
Sean O'Toole
Authors:
Sean M. O'Toole, BS; Rebekah J. Walker, PhD; Emma Garacci, MS; Aprill Z. Dawson, PhD, MPH;
Jennifer A. Campbell, MPH; Leonard E. Egede, MD, MS
Dept/Division:
CAPS
Category:
Student
Introductions:
Diabetes affects 9.4% of the U.S. population, and has been independently linked to declines in
cognitive functioning and efficiency. Cognitive function exists on a spectrum from normal, to mild
cognitive impairment, and finally dementia. There are known racial/ethnic disparities in diabetes
and cognitive dysfunction. Social participation and networking has been shown to be associated
with mitigative effects on cognitive decline, irrespective of race/ethnicity. While previous
research has begun to address how race/ethnicity factors into the relationship between diabetes
and dementia, few studies have included mild cognitive impairment, nor have they assessed
whether social participation measures may help explain racial/ethnic disparities. This study fills
the gap in knowledge by including mild cognitive impairment and social participation measures
into a model designed to explain these differences.
Methods:
Data was analyzed from the Health and Retirement Study (HRS), a nationally representative,
longitudinal survey (1992 - 2016) of U.S. adults over age 50 and their spouses who were surveyed
every two years. The sample included 5,571 participants from 2008 - 2014 that had available
cognitive function measures, were age 50 years and older during their first cognitive assessment,
and had self-reported diabetes. The outcome for this study was cognitive function, characterized
as “normal”, “mild”, and “dementia”. Our predictor was race/ethnicity, characterized as “non-
Hispanic White (NHW)”, “non-Hispanic Black (NHB)”, “Hispanic”, and “other”. Covariates included
demographic (gender, age, education, household income/assets), clinical/behavioral
(comorbidities, BMI, smoking status), and social measures (perceived support, loneliness,
perceived constraints and mastery on personal control). A series of generalized estimating
equation (GEE) logistic regression models were used for the analysis. Unadjusted models were
analyzed, followed by adjusted models that were built by adding each covariate separately.
Results:
In the comparison of Dementia vs. Normal (ref) cognition: compared to NHWs, NHBs were 3.75
times more likely (OR=3.75, 95%CI 2.52 - 5.56), Hispanics 3.05 times more likely (OR=3.05, 95%CI
1.97 - 4.72), and “Others” were 3.82 times more likely (OR=3.82, 95%CI 1.47 - 9.95) than NHWs to
reach dementia. Mild Cognitive Decline vs. Normal (ref): NHB vs. NHW (ref): 2.87 (OR=2.87, 95%CI
2.37 - 3.48), Hispanic vs. NHW (ref): 1.88 (OR=1.88, 95%CI 1.49 - 2.37), and Other vs. NHW (ref):
2.20 (OR=2.20, 95%CI 1.42 - 3.39). Dementia vs. Mild Cognitive Decline (ref): NHB vs. NHW (ref):
1.44 (OR=1.44, 95%CI 1.00 - 2.06), Hispanic vs. NHW (ref): 1.72 (OR=1.72, 95%CI 1.17 - 2.52), and
Other vs. NHW (ref): 1.72 (OR=1.72, 95%CI 0.68 - 4.31).
Conclusions:
After adjusting for demographics, clinical/behavioral, and social factors, results showed that
racial/ethnic disparities persist. These findings suggest that further research is needed to address
these disparities. Some studies have suggested that cognitive assessments become routine in
diabetes follow-up visits, which could be a feasible and effective way to recognize and mitigate
cognitive impairments in individuals with diabetes, across race/ethnicity.
Acknowledgements:
Support was provided by the NIA T35 Training Grant (T35AG029793-13), Dr. Linda Meurer, MD

Research Day 2019
Jump to Table of Contents 37
Population, Community Health & Outcomes
Poster #
20
Abstract Title:
Independent relationship between financial hardship and time to diabetic kidney disease
Presenter(s):
Timothy Corwin
Authors:
Timothy Corwin; Mukoso N. Ozieh, MD, MSCR; Emma Garacci, MS; Anna Palatnik, MD; Leonard E.
Egede, MD, MS
Dept/Division:
CAPS
Category:
Student
Introductions:
An estimated 30.3 million people in the United States and over 400 million worldwide have
diabetes. One third of all individuals with diabetes develop kidney damage that causes diabetic
kidney disease (DKD). Diabetes is the leading cause of kidney disease in the United States.
Patients with diabetes experiencing financial hardship are predisposed to have a more difficult
time managing their diabetes. This study examines the relationship between financial hardship
and the development of DKD among adults with diabetes.
Methods:
Eight years of data (2006-2012) for 2,735 adults with diabetes age 50 and above from the Human
Retirement Study (HRS), a national longitudinal cohort study, was analyzed. The primary outcome
was time to DKD. DKD was based on self-report, “has your diabetes caused you to have trouble
with your kidneys or protein in your urine?”. Financial hardship measures included difficulty
paying bills, food insecurity and medication cost non-adherence. A cumulative financial hardship
score ranging from 0 to 3 was constructed based on all three measures. Cox regression models
were used to estimate the association between financial hardship, change in financial hardship
and time to DKD adjusting for demographics, socioeconomic status, and comorbidities. Statistical
analysis was performed with SAS version 9.4 (SAS Institute).
Results:
Compared to individuals with no financial hardship, individuals with financial hardship (HR=1.54,
95% CI 1.25-1.91) had a significantly higher likelihood of developing DKD over the 8-year period in
the unadjusted model (p<0.01). After adjustments, individuals with financial hardship (HR=1.30,
95% CI 1.03-1.65) maintained a significant increased likelihood of developing DKD compared to
individuals without financial hardship (p=0.02). Compared to individuals who were without
financial hardship across all surveys, those with financial hardship across all surveys (HR=1.70,
95% CI 1.15-2.54) and those who began without financial hardship and did have it in later surveys
(HR=2.10, 95% CI 1.32-3.33) had significantly higher likelihood of developing DKD (p<0.01) in the
unadjusted model. After adjustments, those who began without financial hardship and had it in
later surveys (HR=1.90, 95% CI 1.18-3.06) maintained a significantly higher likelihood of
developing DKD (p=0.02).
Conclusions:
The findings from this study show that having financial hardship significantly increases the
likelihood of time to DKD in adults with diabetes and that the transition from being without
financial hardship into financial hardship may exacerbate this relationship. Future intervention
studies focused on adults with diabetes at-risk of transitioning into financial hardship are needed.
Acknowledgements:
Support received by grants UL1TR001436 from the Clinical and Translational Award (CTSA)
program of the National Center for Research Resources and the National Center for Advancing
Translational Sciences and the National Institute of Diabetes and Digestive Kidney Diseases- NIH-
NIDDK 1R25 DK098104-05 grant

Research Day 2019
Jump to Table of Contents 38
Population, Community Health & Outcomes
Poster #
21
Abstract Title:
The relationship between patient satisfaction and health care expenditures in adults with spine
related disorders: an analysis of the 2008-2015 Medical Expenditures Panel Survey (MEPS).
Presenter(s):
Jordan A. Gliedt
Authors:
Jordan A. Gliedt, Rebekah J Walker, Aprill Z Dawson, Leonard E. Egede
Dept/Division:
CAPS and Neurosurgery
Category:
Junior Faculty
Introductions:
There is increasing emphasis in health care to improve outcomes while also achieving high patient
satisfaction with low costs. The ability to achieve this is not fully known. The relationship between
each of these aspects has not been fully explored. Specifically, the association between patient
satisfaction and health care expenditures is generally unclear and unknown in adults with spine
related disorders (SRDs). This study aimed to investigate the relationship between patient
satisfaction and total health care expenditures in adults with SRDs using 2008-2015 data from the
United States Medical Expenditures Panel Survey (MEPS).
Methods:
Responses from 15,850 adults were analysed. The MEPS Medical Conditions files was used to
identify individuals with SRDs. Frequencies and percentages were calculated for the independent
variable (composite patient satisfaction scores) and all covariates. A two-part model was
completed to estimate total health care expenditures. We adjusted for covariates added in blocks
according to the Andersen model of health care predisposing, enabling, and need categories.1
Lastly, a margins command was performed to calculate incremental costs associated with each
adjusted model.
Results:
After adjusting for predisposing factors there was a statistically significant association between
individuals with greater patient satisfaction and decreased health care expenditures such that the
most satisfied group spent $1,779 less than the least satisfied (95% CI, -2,640, -917). After
adjusting for enabling factors there was a statistically significant relationship between the highest
level of patient satisfaction and decreased health care expenditures such that the most satisfied
group spent $1,324 less than the least satisfied (95% CI, -2,192, -456). After adjusting for need
factors, there was no longer a statistically significant association between individuals with greater
patient satisfaction and decreased health care expenditures.
Conclusions:
This study found a statistically significant relationship between higher patient satisfaction scores
and decreased health care expenditures in individuals with SRDs. However, this relationship was
explained by need factors, such as various comorbidities and health status. This suggests the need
for research to understand why the relationship between patient satisfaction and health care
expenditures seen in patients with SRDs differs from those with higher physical health status,
good mental health status, chronic bronchitis, cancer, heart disease, diabetes, hypertension,
depression, and stroke.
Reference 1:
Andersen RM. Revisiting the behavioural model and access to medical care: does it matter? J
Health Soc Behav 1995; 36(1):1-10.

Research Day 2019
Jump to Table of Contents 39
Population, Community Health & Outcomes
Poster #
22
Abstract Title:
Utilizing Arts Based Data Generation Techniques to Develop Socio-technical Anger Interventions
in the Veteran Population
Presenter(s):
Danielle Olsen
Authors:
Danielle Olsen, Katinka Hooyer, PhD, Zeno Franco, PhD, Praveen Madiraju, PhD, Sheikh Iqbal
Ahamed, PhD, Tanvier Roushan, MS, Nadiyah Johnson, Kowser Patwary, MS, Bill Watson, MFA,
Nancy Smith-Watson, Jim Tasse
Dept/Division:
Family and Community Medicine
Category:
Student
Introductions:
Veterans with PTSD are at an increased risk for high-risk behaviors including aggression. Utilizing
sensors to identify early warning signs for anger may provide a strategy for just-in-time
interventions. This research involved: 1) ethnographically informed data collection of veteran
experiences of anger; 2) data generation of angry gestures with professional actors and sensors.
Methods:
10 weekly, semi-structured focus groups were conducted with three veterans. Field-notes from
the interviews were analyzed through grounded theory to develop a taxonomy of anger
expressions. These categories were used to create a deductive coding scheme to fulfill the
immediate needs of our technical design team. Through this process 12 gestures associated with
anger outbursts were identified. Method actors then performed these identified gestures while
instrumented with E4 Empatica wristbands. Data from the sensors were analyzed using K Nearest
Neighbor (KNN) and other machine learning approaches.
Results:
Methodological synthesis of computational and social science operate as a bridge to deeper
understanding of complex emotional experiences. Preliminary analysis suggests that while
expressions of anger are individualistic, there exist common emotional, physical and social
experiences that inform anger. The 12 gestures identified through the deductive coding process
were correctly classified using KNN with 67% accuracy.
Conclusions:
Initial coding shows multiple examples of anger expression within the veteran population.
Determining common anger precursors and recognizing the need for self-awareness of personal
triggers will influence the development of personalized interventions to prevent angry outbursts.
Gesture sensor results were promising, and the technical team was able
to successfully synchronize sensor accelerometer data to real-time anger expression performed
by method actors. Yet, through the use of arts-based and ethnographically informed methods
were able to reveal data not captured using IoT (internet of things) approaches such as: early
warning signs of anger involving physical stillness and staring, veteran’s ethical concerns regarding
data capture, and the physical limits of the Empatica Sensors.
Acknowledgements:
The project described was supported by the National Center for Advancing Translational
Sciences, National Institutes of Health, Award Number UL1TR001436. The content is solely the
responsibility of the author(s) and does not necessarily represent the official views of the NIH.
This project is funded by the Research and Education Program Fund, a component of the
Advancing a Healthier Wisconsin Endowment at the Medical College of Wisconsin. This project
was completed through partnership with community organizations: Dryhootch and Feast of
Crispian: Shakespeare with Veterans

Research Day 2019
Jump to Table of Contents 40
Population, Community Health & Outcomes
Poster #
23
Abstract Title:
Multimorbidity and Functional Status among Geriatric Veterans
Presenter(s):
Lillian Zheng
Authors:
Lillian Zheng, BS, Katherine Sherman, MS, Edith Burns, MD
Dept/Division:
Medicine: Geriatrics, VA Hospital
Category:
Student
Introductions:
Older adults with multiple chronic conditions (MCC) have worse function, greater health care
utilization, and earlier mortality. Patterns of multiple chronic co-morbid conditions and related
functional status have not been well-described.
Methods:
Mixed methods, cross-sectional survey of convenience sample of patients > 65 years attending
appointments at a VA primary care clinic. Measures included Activities of Daily Living (ADL),
Instrumental ADL (IADL), Short Physical Performance Battery (SPPB), MiniCog screen and a semi-
structured interview concerning patient illness perceptions. Manual chart reviews abstracted
medical history.
Results:
127 participants, mean age 76+8 years were consented and enrolled. Average number of
conditions was 11.6+4.7. The 5 most prevalent were hypertension (85%), hyperlipidemia (70%),
diabetes (46.4%), coronary artery disease (39.4%), and obesity (35.4%). Market Basket (MB)
analysis assessing patterns of MCC by “system” showed endocrine and cardiovascular (CV)
conditions co-existing with a neurological condition (65.6% of patients), musculoskeletal condition
(61.7%), genitourinary condition (53.9%), and GI condition (50.8%). For individual diseases,
hyperlipidemia and hypertension co-occurred with visual impairment (28.1% of patients),
coronary artery disease (27.3%), diabetes (27.3%), arthritis (23.4%), obesity (21.9%). Functional
status by ADL was 5.7 + 0.6 (range 0-6) and IADL was 6.5 + 1.6 (range 0-8). Short Physical
Performance Battery (SPPB), 7.9+3.3, was similar across the five MB rules for organ systems and
inversely associated with age (R2=0.25, p<.001). Individuals with positive MiniCog (16%) were
older (83.2+/-8.0 vs. 75.2+/-7.9, p<.001) and had worse SPPB scores, 5.05+3.4 vs 8.5+3.0, p<.001.
Of 48 participants queried about illness perceptions, 78.7% felt younger than actual age, but
physically hindered by MCC. 58.3% thought of comorbidities independently rather than
interrelated.
Conclusions:
The most common patterns of MCC were coexistence of hypertension, hyperlipidemia, and 1
other disease. Functional status by self-reported ADL and IADL was high, while objective
performance was in the range associated with future loss of mobility (SPPB<9) and did not differ
by pattern of MCC. Age was inversely associated with functional status (SPPB) and those with
impaired MiniCog were older and had worse SPPB. Greater appreciation of interrelationships
among conditions may be important for reducing treatment burden and improving self-
management.
Research Day 2019
Jump to Table of Contents 41
Population, Community Health & Outcomes
Poster #
24
Abstract Title:
Post-exposure prophylaxis (PEP) awareness and prescribing practices among US primary care
providers and HIV specialists
Presenter(s):
Steven A. John
Authors:
Steven A. John & Andrew E. Petroll
Dept/Division:
Psychiatry and Behavioral Medicine: Center for AIDS Intervention Research
Category:
Junior Faculty
Introductions:
Pre-exposure prophylaxis (PrEP) is currently prioritized in HIV prevention research, but post-
exposure prophylaxis (PEP) has been clinically recommended since 2005. We sought to determine
PEP awareness and prescribing practices among US primary care providers (PCPs) and HIV
specialists.
Methods:
PCPs and HIV specialists (n=480) located in 10 US cities with greatest HIV prevalence were
recruited via professional organizations between July 2014 and May 2015 to participate in an
online survey. Providers were asked about their PEP awareness and prescribing experience for
patients with potential sex-related HIV exposures, which we coded into a PEP prescribing
experience cascade with three categories: 1) PEP unaware, 2) PEP aware, no prescribing
experience, and 3) PEP prescribing experience. We examined associations of providers’
demographics (age, gender, and race/ethnicity), practice city, specialty (PCP or HIV specialist),
profession (physician, nurse practitioner, or physician assistant), clinic/hospital type (private or
public/other), and PrEP prescribing experience with their location on the PEP prescribing cascade
using fully-adjusted multinomial logistic regression.
Results:
Overall, 12.5% were unaware of PEP, 43.5% were aware of PEP but hadn’t prescribed it, and
44.0% had prescribed PEP. Providers in private clinic settings, compared to public/other settings,
were more likely to be classified in the PEP unaware group compared to PEP aware without
prescription group (RRR=3.15, p<0.01). HIV specialists, compared to PCPs, were more likely to be
classified in the PEP prescription group compared to the PEP aware without prescription group
(RRR=3.11, p<0.001). PrEP prescribers (versus PrEP non-prescribers) were more likely to be
classified in the PEP prescription group compared to PEP aware without prescription group
(RRR=7.61, p<0.001).
Conclusions:
PEP awareness was high, but a drop-off was evident between PEP awareness and prescription.
PEP prescribing variability indicates the need for more universal training nationwide, especially
among PCPs who may be more accessible to patients immediately following potential HIV
exposure.
Acknowledgements:
The authors acknowledge the contributions of other members of the study team, especially Drs.
Jennifer Walsh, Jill Owczarzak, Timothy McAuliffe, Laura Bogart, and Jeffrey Kelly. We also thank
CAIR staff and our participants.

Research Day 2019
Jump to Table of Contents 42
Educational
Poster #
25
Abstract Title:
Implementing Virtual Reality in Medical Education and Training
Presenter(s):
Adhitya Ramamurthi , Devashish Joshi, Michelle Botts
Authors:
Adhitya Ramamurthi BS, Devashish Joshi BS, Michelle Botts BS, David Joyce MD, Barb Alivo RN,
Emily Neumann RN
Dept/Division:
Surgery: Division of Cardiothoracic Surgery
Category:
Student
Introductions:
Medical education has not experienced a game-changing paradigm shift since 1910 when the
Flexner Report laid the foundation for the basic science and clinical curriculum we use today.
Virtual Reality (VR) is an emerging technology that has the potential to solve many of the
difficulties that arise from trying to gain adequate exposure to the complex decision making
challenges that face the contemporary physician. Use of VR simulators has improved acquisition
and development of surgical skills across surgical specialties. However, for VR to be successful it
must be embraced by the students themselves. This study aims to assess the interest level of
medical students towards the application of VR in medical education.
Methods:
All medical students enrolled at the Medical College of Wisconsin were given an anonymous
survey of 8 questions to gauge their knowledge and attitude towards VR. Free text space was
included for students to elaborate on their responses.
Results:
Out of a sample of 960 students, 115 completed the questionnaire (response rate ~12%). A
statistically significant relationship was found between students who believe VR will augment
their education (79.65%) and those who have used or have heard of VR (p=0.05). It was found
that students were most interested in surgical procedures and interactive physiology modules,
with no bias between gender, age, or academic year. However, with 38% of students interested in
surgery, 47% interested in a non-surgical specialty, and 15% unsure, a statistically significant
pattern was observed between desired VR modules and future specialty (p=0.001).
Conclusions:
Although opinions of what VR content would be useful differed between students, a majority
would welcome VR into their medical school curriculum. Future investigations will need to
establish a proof of concept for this technology to demonstrate improvement in performance
when VR is used to augment medical education.

Research Day 2019
Jump to Table of Contents 43
Kidney
Poster #
26
Abstract Title:
Timing of renal ultrasound for first febrile UTI in young children: Sooner or later?
Presenter(s):
Jessica Hayes
Authors:
Jessica Hayes, BS, Kelsey Porada, MA, Fatima Anibaba, MS, Caitlin Kaeppler, MD, Sarah Bauer,
MD, Anika Nelson, MD
Dept/Division:
Pediatric Hospital Medicine
Category:
Student
Introductions:
Urinary tract infections (UTI) are common in young children and are one of the most common
pediatric admission diagnoses. The American Academy of Pediatrics has a well-established clinical
practice guideline (CPG) for the diagnosis and management of the initial febrile UTI in children 2-
24 months, and many institutions have adopted their own CPGs. Our institutional inpatient CPG
recommends a renal and bladder ultrasound (RBUS); however, the timing of ultrasound in relation
to initiation of antibiotics varies among our providers. The purpose of this study is to describe
trends in our practice as well as to identify a difference in the rate of abnormal renal ultrasounds
when performed within 24 hours of initiation of antibiotics versus later in the treatment course.
Our hypothesis is that RBUS obtained less than 24 hours after initiation of antibiotics is associated
with abnormal findings, prompting additional testing.
Methods:
A retrospective chart review was performed, including all infants aged 2 to 36 months admitted to
the hospitalist service at Children’s Hospital of Wisconsin with their first febrile UTI from 2016 to
2018. Exclusion criteria included previously identified genitourinary abnormality, history of
recurrent UTIs, positive blood culture, immunodeficiency, sepsis, shock, meningitis, or another
serious comorbid condition. An abnormal ultrasound was defined as pyelonephritis, pelviectasis,
hydronephrosis or any other finding that resulted in additional testing, either a repeat RBUS or
voiding cystourethrogram.
Results:
We reviewed 87 charts; 23 patients were excluded. Of the remaining 64 patients, 65.6% (n=42)
had a RBUS within 24 hours of their first dose of antibiotics, while 34.3% (n=22) had a RBUS
performed after 24 hours. There was no statistically significant difference in the rate of abnormal
findings between patients who had a RBUS performed in <24 hours versus >24 hours (50% vs
41%; p=0.6683). There was also no significant difference in the rates of repeat imaging between
the two groups (43% vs 32%; p=0.0348).
Conclusions:
We did not find a significant difference in the rates of abnormal RBUS performed within 24 hours
of starting antibiotics versus those performed greater than 24 hours after starting antibiotics for
treatment of a febrile UTI in young children. These findings suggest there is no need to delay
RBUS for these patients. However, our study was limited by small sample size and, if repeated
with a larger group, a difference may become apparent.
Reference 1:
Spencer JD, Schwaderer A, McHugh K, Hains DS. Pediatric urinary tract infections: an analysis of
hospitalizations, charges and costs in the USA. Pediatric Nephrology, 2010. 25(12): 2469-75.
Reference 2:
AAP Subcommittee on Urinary Tract Infection. Reaffirmation of AAP clinical practice guideline: the
diagnosis and management of the initial urinary tract infection in febrile infants and young
children 2-24 months of age. Pediatrics. 2016;138(6):e20163026.

Research Day 2019
Jump to Table of Contents 44
Cancer
Poster #
27
Abstract Title:
Photo triggered liposomes for delivery of immunostimulatory cytokines to solid tumors
Presenter(s):
Gayatri Sharma
Authors:
Gayatri Sharma, Gang Xin, Jaidip Jagtap,Jonathan Ebben, Amit Joshi
Dept/Division:
Biomedical Engineering
Category:
Postdoctoral Fellow
Introductions:
The success of antibodies against PD-1/PD-L1 and CTLA-4 pathways and immune adoptive T cell
therapy checkpoints has revolutionized cancer therapy. Cytokines like IL-12 have also been
extensively evaluated for its potential to enhance antitumor immune response. Interleukin-12
antitumor activities are mediated by the activation of T and NK lymphocytes to produce IFNy.
However, the systemic bolus injections of IL-12 causes serious toxicities. A number of different
approaches are under development to deliver maximum dose of IL-12 specifically to the tumors.
In this study, the red light activable anticancer photodynamic therapy drug 2-(1-Hexyloxyethyl)-2-
devinyl pyropheophorbide-a (HPPH) was loaded in liposomes together with the immuno-
stimulating cytokine interleukin 12 (IL-12) for photo-immunotherapy of cancer. We hypothesized
that encapsulating a combination of IL-12 and HPPH in liposomes with laser-triggered release will
result in tumor specific delivery of IL-12 while minimizing systemic effects.
Methods:
The liposomes were prepared by thin-film hydration method. The comparative release of IL-12
was tested on the following formulations of liposomes: co-loaded with HPPH (400µg) and IL-12
(0.5mg), HPPH only liposomes prepared without IL-12 entrapment, IL-12 only liposomes. The
liposome size and zeta potential were determined by dynamic light scattering. All the samples of
liposomes were treated for 2 minutes with a 660 nm diode laser at room temperature using the
power output at 52 mW . The amount of IL-12 released from the liposomes was measured by
ELISA. The cytotoxic effect of laser-triggered release of IL-12 was determined on human breast
cancer cell line. The immunostimulatory effect of IL-12 was assessed on C57BL/6 implanted with
mammary tumors
Results:
The laser triggered release of IL-12 (440 ng/mL) is comparatively more as compared to normal
leakage (240 ng/mL). The in vitro co-culture model with human breast cancer cell line and CD-8 T
cells on treatment with liposomes demonstrated more apoptosis in culture treated with laser
triggered liposomes as compared to only IL-12 treated liposomes. To assess the
immunostimulatory effect of IL-12 on tumor microenvironment, C57BL/6 mice implanted with
mammary tumors were treated with systemic injection of liposomes followed by laser treatment.
The number of activated CD8+ T cells were significantly more in laser-triggered release IL-12 as
compared to only IL-12 treated liposomes.
Conclusions:
Photo triggered release of immunostimulatory cytokines by liposomes can be effective for
treatment of solid tumors.

Research Day 2019
Jump to Table of Contents 45
Cancer
Poster #
28
Abstract Title:
Magnetic resonance imaging based radio-pathomic maps of epithelium and lumen density localize
high grade prostate cancer independent of variability in pathological annotation
Presenter(s):
Sean D. McGarry
Authors:
Sean D. McGarry, John D. Bukowy, Kenneth A. Iczkowski, Allison K. Lowman, Michael Brehler,
Samuel Bobholz, Alex Barrington, Kenneth Jacobsohn, Jackson Unteriner, Petar Duvnjak, Michael
Griffin, Mark Hohenwalter, Anjishnu Banerjee, Tucker Keuter, Wei Huang, Tatjana Antic, Gladell
Paneer, Watchareepohn Palangmonthip, Peter S. LaViolette
Dept/Division:
Biophysics
Category:
Student
Introductions:
Machine learning techniques have become more prevalent in medicine over the last decade;
however, adoption in the clinic has been slow due to concerns regarding generalizability. There
are known sources of variance associated with the screening and diagnosis of prostate cancer that
could potentially impact the performance of a machine learning algorithm applied beyond its
original training set. While there is known inter-user variability in the annotation of prostate
cancer histology, the downstream effects have not been previously studied. This study addresses
the effects of varying training set labels on a previously published rad-path machine learning
technique, radio-pathomic mapping in prostate cancer.
Methods:
Clinical imaging and post-surgical tissue from 48 prospectively recruited patients was used in this
study. Tissue was sliced to match the axial T2 and whole mount slides were hematoxylin and eosin
stained. Data from 28 patients (n=33 slides) were sent to 5 pathologists to be annotated. Inter-
pathologist variability was assessed using the kappa statistic. Slides from the remaining 20
patients (n=123) were annotated by a single pathologist. Magnetic resonance images were
aligned to the T2 and the qualitative imaging was normalized. Radio-pathomic mapping (RPM)
models were trained using a partial least squares regression using clinical imaging values to
predict lumen and epithelium density. Models performance was evaluated using a receiver
operator characteristic calculated on small set of naïve data annotated by 5 pathologists and a
larger set of 123 slides annotated by a single pathologist.
Results:
Inter-pathologist variability measured using a kappa statistic ranged from 0.18-0.75 (mean =
0.62±0.25). Lumen density out performed epithelium density on the small dataset. On the larger
test set epithelium models out performed ADC (AUC = 0.85), the consensus model (AUC = 0.92)
matched the top pathologist and produced the clearest images.
Conclusions:
We demonstrate inter-pathologist independence of the radio-pathomic mapping algorithm. We
report similar inter-user variability scores to other previous papers and our small test set results
demonstrate the importance of a consistent annotation style in rad-path studies.

Research Day 2019
Jump to Table of Contents 46
Cancer
Poster #
29
Abstract Title:
Trends in Healthcare Expenditures among Adult Cancer Survivors in the United States, 2008-2016
Presenter(s):
Shannon L. Walker, Med
Authors:
Shannon L. Walker, MEd; Joni S. Williams, MD, MPH; Kaiwei Lu, MS; Aprill Z. Dawson, PhD;
Leonard E. Egede, MD, MS
Dept/Division:
CAPSs and Institute for Health and Equity
Category:
Student
Introductions:
In the United States, the increase in cancer survivorship prevalence has been attributed to longer
lifespans, an aging population, and medical advances in screening, treatment, and early disease
detection. Previous research has shown an association between cancer survivorship and
increased expenditures. However, no study has assessed trends of economic burden for cancer
survivors. This study aims to assess trends in medical expenditures between 2008 and 2016 for
cancer survivors compared to those with no history of malignancies.
Methods:
This is an analysis of 9 years of data (2008-2016) from the Medical Expenditure Panel Survey
(MEPS) (unweighted n=227,110; weighted n=236,811,875). Individuals were categorized as being
cancer survivors if they self-reported a previous diagnosis of cancer. The outcome was medical
expenditure (categorized as total expenditure, inpatient, office-based, medications, outpatient,
dental, emergency room, home health, and other); the predictor was cancer diagnosis. Covariates
included sex, age, race/ethnicity, marital status, education level, income as a ratio of the poverty
line, census region, insurance type, and comorbid conditions. Two-part statistical modeling with a
combination of binomial and positive distributions was used to evaluate differences in the
categories of medical expenditures among cancer survivors. Data was clustered into 5 time
points: 2008-2009 vs. 2010-2011 vs. 2012-2013 vs. 2014-2015 vs. 2016. Analyses were weighted
for the U.S. population. Stata v13 was used for the analyses.
Results:
In this sample of adults,11% (n=25,005,230) had a prior cancer diagnosis. Compared to
expenditures for adults with no prior cancer diagnosis ($4,720 [95% CI $4,499, $4,941]), cancer
survivors had more than twice the unadjusted mean total expenditure ($13,829 [95% CI $12,234,
$15,424]) between 2008 and 2016. After adjusting for demographic characteristics, comorbid
conditions, and time, cancer survivors had significantly higher incremental total expenditures at
$3,522 (95% CI $3,072, $3,972) compared to adults without cancer. Cancer survivors had
significantly higher incremental expenditures for office-based visits ($1,085 [95% CI $990, $1180]),
inpatient hospitalizations ($810 [95% CI $627, $992])), outpatient appointments ($517 [95% CI
$434, $600]), and medications ($409 [95% CI $295, $523) compared to adults without cancer.
Conclusions:
In this nationally representative sample of adult cancer survivors, there were statistically
significant differences in healthcare expenditures for those with a history of cancer compared to
those without, after adjusting for relevant covariates. These findings suggest cancer survivors
have higher incremental expenditures compared to adults without cancer, with significant burden
resulting from office-based, inpatient, and outpatient visits and medications.

Research Day 2019
Jump to Table of Contents 47
Cancer
Poster #
30
Abstract Title:
Advancing the Science of Translation Through the Establishment of the CTSI Translational
Informatic and Bioinformatic Research Unit
Presenter(s):
Brad Taylor
Authors:
Zimmermann, Taylor, DeVoe, J Geurts, B George, Shaker, Urrutia
Dept/Division:
CTSI and GSPMC
Category:
Junior Faculty
Introductions:
Genomics and Precision Medicine are advances in the resolution with which researcher and
clinicians can address patient needs. Appropriate infrastructure is required to enable this type of
work. Translation, or the process of bringing research knowledge into the clinic to improve the
practice, is core to the missions of MCW, CTSI, and the GSPMC. The Science of Translation is the
study of the processes of translational research.
Methods:
To empower the Science of Translation and generate tools that facilitate it, the CTSI and GSPMC
have formed the Translational Informatic and Bioinformatic Research Unit (TIBU). Now equipped
with staff cross-trained in Biomedical Informatics and Bioinformatics, the TIBU is positioned at a
critical translational nexus. We have initiated and are facilitating a series of pilot projects spanning
oncology and genomics data interpretation.
Results:
In oncology, the best care increasingly requires knowledge of each patients’ tumor genomics
profile as well as how their germline genome may influence the tumor. While not all patients will
necessarily benefit directly from genomics testing, it is not clear in advance if a patient has an
actionable genomic profile, which necessitates that patients be tested, if there is a potential
opportunity for clinical intervention. In a pilot project of the TIBU, we have collaborated with
clinical colleagues to re-analyze a set of 1,146 oncology patient clinical test results. Using our
unique point of view and bioinformatic approaches, we have highlighted the impact of the
differences and identified a significant subset of the cohort that may benefit clinically from the
data being reanalyzed in a new way. This provides for additional opportunities to answer different
clinical questions than the original test was performed to answer. We explore the practical
reasons for discrepancies in clinical oncology reporting practices and how they may have
substantive impacts on our patient population.
Conclusions:
We believe that the Science of Translation can be facilitated by establishing multi-disciplinary
teams focused on critical challenges in medicine, building the right tools to support the team, and
applying them within the right environment. Access to the right data is critical for success,
necessitating multi-institutional partnerships. The TIBU is ideally positioned to facilitate
translational research that leverages the collective strengths of multiple MCW Institutes, Centers,
and medical programs.

Research Day 2019
Jump to Table of Contents 48
Cancer
Poster #
31 (NOT PRESENTING)
Abstract Title:
Retrospective Quantitative Analysis Comparing Respiratory Gated to Non-respiratory Gated 18F-
FDG PET/CT Imaging in Patients Undergoing Evaluation for Primary Lung Cancer
Presenter(s):
Eric Fair
Authors:
E. Fair, R. Helllman, D. Bucklan
Dept/Division:
Nuclear Medicine
Category:
Clinical Fellows & Residents
Introductions:
In patients undergoing evaluation for primary lung cancer, 2-deoxy-2-(18F) fluoro-D-glucose (18F-
FDG) positron emission tomography (PET)/computed tomography (CT) is a commonly used
imaging examination for staging and treatment evaluation. Maximum and mean standardized
uptake values (SUV) are commonly reported for these patients in practice, and metabolic tumor
volume (MTV) and total lesion glycolysis (TLG) may have prognostic and treatment-related
implications. Respiratory motion can result in displacement of lesions and degrade images of the
lower chest in these patients, potentially reducing sensitivity of lesion detection and affecting the
quantitative values that may have an effect on disease staging and treatment. We aim to assess
the differences in quantitative values on non-respiratory gated versus respiratory gated FDG
PET/CT imaging for discrete pulmonary lesions in patients undergoing evaluation for primary lung
cancer
Methods:
This study retrospectively reviewed 35 patients (13 males, 22 females, median age 69) evaluated
for primary lung cancer with both non-respiratory gated and respiratory gated FDG PET/CT
imaging obtained, including 36 separate FDG PET/CT exams and 49 discrete pulmonary lesions.
Standard non-respiratory gated whole body FDG PET/CT was obtained at multiple bed positions (2
min each) except for sequentially obtained respiratory gated PET imaging at two bed positions (4
min each), encompassing the lower lung fields. An abdominal pressure sensor was used for
respiratory cycle gating from peak inspiration to peak inspiration with data gathered from mid-
expiration to mid-inspiration. The mean SUV (SUVmean) metabolic tumor volume (MTV41%), and
total lesion glycolysis (TLG41%) were segmented using the software default adaptive threshold of
41% from the maximum in the volume of interest. SUVmax, SUVmean, MTV41%, and TLG41%
were measured for each discrete pulmonary lesion on both non-respiratory gated and respiratory
gated imaging utilizing automated software to calculate values within the volume of interest.
Results:
Data analysis demonstrates an increase in SUVmax in 81.6% of lesions, an increase in SUVmean in
87.7% of lesions, a decrease in MTV41% in 87.7% of lesions, and a decrease in TLG41% in 83.7% of
lesions on respiratory gated FDG PET/CT imaging when compared to non-respiratory gated
imaging. Utilizing a paired samples T-test, there was a significant difference between non-
respiratory gated and respiratory gated imaging, respectively, for SUVmax (mean=8.5, SD=6.7 and
mean=9.2, SD=6.8, p=<.001), SUVmean (mean=5.0, SD=4.1 and mean=5.4, SD=4.1, p=<.001),
MTV41% (mean=7.5, SD=8.6 and mean=6.5, SD=8.0, p=<.001), and TLG41% (mean=57.6, SD=99.7
and mean=54.3, SD=93.8, p=0.0017). Overall, respiratory gated imaging demonstrates a 12.7%
increase in SUVmax, a 7.6% increase in SUVmean, a 38.6% decrease in MTV41%, and a 16.9%
decrease in TLG41% when compared to non-respiratory gated FDG PET/CT imaging
Conclusions:
Overall, respiratory gated FDG PET/CT imaging demonstrates a significant increase in SUVmax and
SUVmean and a significant decrease in MTV and TLG when compared to non-respiratory gated
PET/CT imaging in patients undergoing evaluation for primary lung cancer. The decrease in TLG
with respiratory gated PET/CT imaging was an unexpected consequence. Further data analysis can
evaluate the effect of lesion size, lesion location, and patient weight on these values

Research Day 2019
Jump to Table of Contents 49
Cancer
Poster #
32
Abstract Title:
CAR-modified Th1/Tc1-Polarized T-Rapa Cells Dissociate Inflammatory Cytokine Secretion from
Anti-Tumor Cytotoxicity
Presenter(s):
Robyn Oldham
Authors:
Oldham, Robyn A.A.; Felizardo, Tania; Zhu, Nathaniel; Fowler, Daniel H; Medin, Jeffrey A
Dept/Division:
Pediatrics
Category:
Research Support Staff
Introductions:
Despite noteworthy clinical successes thus far, chimeric antigen receptor (CAR)-engineered cells
have the potential to cause severe side effects. Neurotoxicity and cytokine release syndrome
(CRS), the latter characterized by increased levels of cytokines such as IL-6, IFN-y, and MCP- 1, are
common and life-threatening adverse events associated with CAR therapy. Lymphodepleting
preconditioning regimens are associated with improved clinical responses to CAR therapy, yet
lymphodepletion has also been identified as a risk factor for CRS. The ability to limit or prevent
initiation of CRS would greatly improve the safety of CAR therapy.
Previous clinical trials have shown that T-Rapa cells (patient T-cells grown ex vivo in rapamycin)
can be successfully infused back into autologous recipients after a low-dose conditioning regimen.
Post-infusion, T-Rapa cells have potent anti-cancer effector functions and demonstrate long-term
persistence.
The aim of this study is to assess T-Rapa cells as a next-generation CAR effector cell type.
Methods:
Human Th1/Tc1 T-Rapa cells were transduced by lentivirus harboring an anti-CD19-41BB-CD3ζ
CAR construct. CAR-T-Rapa cells were expanded using CD3/CD28 beads and assessed in
comparison with non-rapamycin-treated CAR-T cells, and non-transduced T cell controls.
Results:
CAR-T and CAR-T-Rapa cells were transduced at similar efficiencies and displayed similar
phenotypes at days 5 and 14 post-thaw. Both CAR-T and CAR-T-Rapa cells exhibited comparable
levels of cytotoxicity against CD19+ cancer cell lines. Further, both T and T-Rapa CAR cells
produced similar amounts of IL-2 following co-culture with CD19+ cancer cell lines. Interestingly,
CAR-T-Rapa cells produced significantly less IFN- y than CAR-T cells after co-culture with CD19+
tumor cells. This observation was consistent for CAR-T and CAR-T-Rapa cells assessed at both day
5 and day 14 post-thaw.
Conclusions:
T-Rapa cells engineered to express an anti-CD19 CAR are similar in phenotype, and are just as
effective at killing tumor cells as similarly-engineered pan T cells, but CAR-T-Rapa cells produce
dramatically less pro-inflammatory cytokines such as IFN-y. Decreased production of pro-
inflammatory cytokines may reduce the risk and severity of CRS, improving the safety of CAR
therapy. As a result, T-Rapa cells may be valuable as a next-generation CAR-T effector cell type.

Research Day 2019
Jump to Table of Contents 50
Cancer
Poster #
33
Abstract Title:
Murine models to study NK immunotherapy against sarcoma
Presenter(s):
Anahi Cruz
Authors:
Anahi Cruz, MaryJo Rademacher, BS, Jeffrey Medin, PhD, Nathan Schloemer, MD
Dept/Division:
Pediatrics
Category:
Student
Introductions:
Immunotherapy harnesses the bodies’ immune system and is an emerging treatment to fight
cancer. Murine xenograft models (human tumors grown in immunodeficient mice) have been
used to study cancer treatments for sarcoma but require a human immune system to develop
novel immunotherapies. Natural killer (NK) cells, an innate immune system cell, are known to
attack tumor cells but have been inadequately studied as immunotherapy. Transplanting human
immune cells (humanizing) can be performed in immunodeficient mice. NOD.Cg-Prkdcscid
IL2Rgammanull (NSG) mice are profoundly immunodeficient and allow engraftment of human
cells but there is poor maturation of NK cells. By using transgenic knock-in mice that are mutated
to produce human cytokines, this may allow for better maturation of NK cells and better
understanding of immunotherapy effects. We proposed utilizing three different murine models to
study human NK cell engraftment for cancer immunotherapy development: NSG, NSG-SGM3
(producing human stem cell factor, GM-CSF, and IL-3), and NSG-IL-15 (producing human IL-15).
We hypothesized that the NSG-IL15 mice will be superior in developing mature NK cells due to the
role of IL-15 in promoting NK cell development.
Methods:
Human hematopoietic stem (CD34+) cells were injected intravenously into sub-lethally irradiated
mice of NSG (n=4), NSG-SGM3 (n=4), and NSG-IL-15 (n=4) backgrounds and we monitored the
reconstitution via flow cytometry analysis of peripheral blood. NSG without human CD34+
administration and human peripheral blood were utilized as controls.
Results:
At 6 weeks, 100% of all mice strains acquired a ratio of human CD45+/ mouse CD45+ of 25% or
greater, meeting the definition of humanized. B (CD19+), T (CD3+NKp46-), NK (CD3-NKp46+), and
myeloid (CD33+) cells were present in all backgrounds. The NK cell population comprises a higher
frequency of human lymphocytes for NSG-IL15 (22.2%) when compared to NSG (6.7%; p=0.12)
and NSG-SGM3(8.3%; p=0.11). Further, the mature NK cell population (CD56dim/CD16+) was
more prevalent in the NSG-IL15 mice (84.1%) compared to NSG (31.6%; p=0.06) and NSG-SGM3
(34.4%; p=0.02). In summary, our results demonstrate a successful humanization in NSG, NSG-
IL15, and NSG-SMG3 murine models.
Conclusions:
Further, we identify the NSG-IL-15 transgenic mouse as an ideal candidate to further classify the
effector functions of mature NK cells to study NK cell mediated immunotherapy in vivo. Our
humanized murine models underwent tumor implantations and await assessment of the
differential maturation effects on human sarcoma tumor clearance.

Research Day 2019
Jump to Table of Contents 51
Cancer
Poster #
34
Abstract Title:
Accuracy of MRI-TRUS Fusion Targeted Prostate Biopsy and Quality Review
Presenter(s):
Kayvon Kiani
Authors:
Kayvon Kiani, Sarah M. Brink, Eric Fair, Kenneth Jacobsohn, Peter LaViolette & Petar Duvnjak
Dept/Division:
Radiology : Abdominal Imaging
Category:
Student
Introductions:
The current diagnosis, staging and clinical management paradigms for prostate cancer are rapidly
evolving with increased incorporation of multiparametric prostate MRI (MP-MRI). Traditionally, men
with clinically suspected prostate cancer have undergone systematic 12-core transrectal ultrasound-
guided (TRUS) biopsy for initial diagnosis and staging; however, there is a large body of growing
evidence in support of pursuing MRI as an initial step, with targeted biopsy performed in only those
men with an index lesion identified on MRI (“MRI-directed pathway”) [1]. Essential to this is a high-
quality prostate MP-MRI practice and close collaboration between radiologists interpreting the
examinations and urologists who typically perform the targeted biopsies. In this study, we evaluated
the accuracy of targeted MRI-TRUS fusion biopsies performed at our institution and performed a
detailed quality image review analysis for discordant biopsy results.
Methods:
We retrospectively evaluated 116 targeted fusion prostate biopsies in patients with known or
suspected prostate cancer, who had index lesions identified on MP-MRI (PI-RADS 3, 4 and 5).
Detection rates for prostate cancer (any grade) and clinical significant prostate cancer (Group Grade II
or higher) were assessed. A subset analysis was then performed for all discordant PI-RADS 5 lesions
(defined as negative for clinically significant cancer or negative for cancer overall), which was
performed by a board-certified radiologist with fellowship training in abdominopelvic imaging and a
current abdominopelvic imaging fellow.
Results:
A total of 116 targeted biopsies with index lesions identified on MP-MRI (39 PI-RADS 5 lesions, 60 PI-
RADS 4 lesions and 17 PI-RADS 3 lesions) were evaluated. Overall detection rates for prostate cancer
(any grade) and clinically significant disease (GG2 or higher) increased with higher PI-RADS score: 75%
(64%), 63% (28%) and 35% (12%) for PI-RADS 5, 4 and 3 categories, respectively. Our subset analysis of
discordant PI-RADS 5 lesions (14 cases) showed that the majority of discordant cases (10/14) were due
to initial misinterpretation of the MRI exam by the radiologist, typically due to preventable imaging
pitfalls (i.e. misidentification of stromal BPH nodules or post-biopsy hemorrhage) or misclassification of
PI-RADS scoring for index lesions.
Conclusions:
Our results demonstrate that cancer detection rates for prostate cancer (any grade) and clinically
significant prostate cancer (GG2 or higher) on targeted biopsy increase with PI-RADS score, in
accordance with previously published data [2]. On subset analysis of discrepant PI-RADS 5 targets, we
demonstrated that the majority of discordant lesions were due to misinterpretation of the MRI by the
radiologist, either due to misidentification of common MRI pitfalls or misapplication of PI-RADS scoring,
emphasizing the importance of standardizing MP-MRI reporting and education within our institution
[3]. Current multi-institutional studies are currently underway to generalize our conclusions and
further investigate potential shortcomings of the evolving MRI-directed pathway in prostate cancer
diagnosis and staging.
Reference 1:
1. Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-Targeted or Standard Biopsy for Prostate-
Cancer Diagnosis. NEJM 2018; 378:1767-1777.
Reference 2:
2. Venderink W, Luijtelaar AV, Bomers JG, et al. Results of Targeted Biopsy in Men with Magnetic
Resonance Imaging Lesions Classified Equivocal, Likely or Highly Likely to Be Clinically Significant
Prostate Cancer. Eur Urol 2018; 73:353-360.
Reference 3:
3. Rosenkrantz AB & Taneja SS. Radiologist, Be Aware: Ten Pitfalls That Confound the Interpretation of
Multiparametric Prostate MRI. AJR 2014; 202:109-120.

Research Day 2019
Jump to Table of Contents 52
Cancer
Poster #
35
Abstract Title:
Outcomes following endovascular interventions for bleeding events in head and neck cancer
patients
Presenter(s):
Matthew Scheidt, MD
Authors:
A. Khetarpal, S. White, R. Hieb, E. Hohenwalter, W. Lea, W. Rilling, M. Scheidt, S. Tutton, P. Patel,
A. Khetarpal
Dept/Division:
Radiology: VIR
Category:
Junior Faculty
Introductions:
Patients with head and neck cancer (HNC) who present with bleeding events have a high rate of
morbidity and mortality. Current data shows mixed outcomes after endovascular interventions.
The purpose of this study is to evaluate endovascular interventions for bleeding events in HNC.
Methods:
This is a single-center, IRB-approved, retrospective study. Patients with HNC who underwent
endovascular interventions after bleeding events including CAS and/or embolization
of external carotid or subclavian artery branch vessels from 1/1/2013 to 9/4/2018 were
evaluated. Demographic data was collected, as well as bleeding events after initial intervention,
need for re-intervention, procedure related complications, time to and cause of death.
Results:
33 patients had interventions; however, 6 were excluded due to loss of follow up or having no
intervention performed. 26/27 (96%) of patients received cancer related treatment, with 25/27
(93%) having prior radiation therapy. Sites of disease included: 9 oropharynx, 7 tongue, 6 larynx, 4
thyroid, 1 nasopharynx. 19/27 (70%) had pre-procedure imaging, of which 9/19 (47%) with active
bleeding or pseudoaneurysm. 2/27 (7%) patients underwent CAS only, 4/27 (15%) underwent CAS
and external carotid branch embolization, and 21/27 (78%) underwent external carotid or
subclavian artery branch embolization. 9/27 (33%) had a re-bleeding event, 4/9 (44%) within 30d
with a mean time to re-bleed of 72 d after initial intervention. 6/27 (22%) required repeat
intervention. There were 4/27 (15%) complications including 2 strokes, 1 endoleak, and 1 access
site pseudoaneurysm. Dates of death were documented in 19/27 (70%) patients with a mean time
to death of 76 d after initial intervention. 5/27 (26%) of these patients had a bleeding event
precipitating their death.
Conclusions:
Endovascular interventions for bleeding events in HNC resulted in a low rate of re-bleeding at 30
days; however, the mortality after 30 days was high. These findings highlight the importance of
being actively involved in goals of care discussions with patients and their families when
discussing the role of endovascular intervention for bleeding events in this patient population.

Research Day 2019
Jump to Table of Contents 53
Cancer
Poster #
36
Abstract Title:
Cell Cycle Dependent Inhibition of G9a Induces Cell Death via Replication Catastrophe in
Pancreatic Cancer
Presenter(s):
Guillermo A. Urrutia
Authors:
Guillermo A. Urrutia, Ann Salmonson, Jorge Toro-Zapata, Nelson Dusetti, Juan Iovanna, Raul
Urrutia, Gwen Lomberk
Dept/Division:
Surgery
Category:
Postdoctoral Fellow
Introductions:
Pancreatic ductal adenocarcinoma (PDAC) presents a significant health burden and is the third
leading cause of cancer-related deaths in the United States. Despite significant efforts to develop
better therapeutics to treat PDAC, the 5-year survival rate for patients has improved only
marginally. Thus, there remains an urgent need to further understand the molecular mechanisms
underlying PDAC development to identify innovative therapeutic targets. Our laboratory is
focused on utilizing epigenetic inhibitors for this purpose.
The current study focuses on an innovative therapeutic approach for the treatment of PDAC
based on leveraging the arrest of malignant cells at a time that shows increased sensitivity for the
use of certain epigenomic inhibitors. Specifically, we sought to combine inhibition of Checkpoint
kinase 1 (Chk1) and the G9a histone methyltransferase by using the small molecule inhibitors
Prexasertib and BRD4770, respectively. Therefore, we targeted simultaneously two pathways that
are necessary for the stability of replication forks.
Methods:
The antitumor effects and molecular mechanisms of the combination were assessed on well-
established L3.6 and patient derived PDAC cell lines by multiple in vitro and in vivo models and
assays, including cellular and clonogenic growth, FACS cell cycle analysis, BrdU incorporation
strategies, comet assay, western blot, immunofluorescence, as well as xenografts and
immunohistochemistry.
Results:
Using live cell imaging, we found that the growth of PDAC cells, both L3.6 and primary cell lines
from PDAC patients, is reduced by the combined inhibition of Chk1 (Prexasertib) and G9a
(BRD4770), achieving a synergistic effect. This result was recapitulated by clonogenic assays.
Combination treatment led to a highly efficient induction of cell death that could not be reversed
through addition of the pan-caspase inhibitor Z-VAD-FMK, indicating that the main mechanism
involved in this process is not caspase-dependent. To determine the underlying cellular
mechanism, we performed FACS analysis which demonstrated a significant increase of cells in S-
phase, as well as a substantial sub-G1 fraction, confirming cell death during this cell cycle stage.
Reduced BrdU incorporation of treated cells further supported these observations. To understand
the molecular mechanism, we evaluated the extent of DNA damage as measured by alkaline
comet assay, confirming generation of ssDNA breaks. We found that in response to combined
inhibition of Chk1 and G9a, PDAC cells activate the ATR-Chk1 axis, but fail at the Chk1 checkpoint
leading to replication stress, as confirmed by ssDNA generation and phosphorylation of ATR,
RPA32, CHK1 and H2A.X proteins. In vivo treatment of subcutaneous pancreatic cancer xenografts
demonstrated that combined targeting of these pathways reduces tumor growth, increasing the
replication stress response and overall DNA damage.
Conclusions:
Our results demonstrate that targeting the epigenetic regulator G9a in combination with
inhibition of the DNA damage response checkpoint offers a novel therapeutic approach for
pancreatic cancer through triggering DNA replication catastrophe.
Acknowledgements:
NIH R01CA178627 and Advancing a Healthier Wisconsin Endowment (AHW)

Research Day 2019
Jump to Table of Contents 54
Blood, Immunity & Infection
Poster #
37
Abstract Title:
Rescuing Exhausted CD8 T cells: Targeting Phosphatase a Novel Strategy?
Presenter(s):
Ankan Gupta
Authors:
Gupta A, Xin G, Bongard R, Thirugnanam K, Pokkuluri PR, Sem DS, Talipov MR, , Cui W,
Ramchandran R
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
Dual specificity protein phosphatase 5 (DUSP5) is a critical regulator of cellular inflammation and
homeostasis. Upon activation, DUSP5 dephosphorylates its only substrate phospho- extra-cellular
signal-related kinase (pERK), to regulate various cellular processes such as proliferation, growth,
survival etc. DUSP5 has been reported to be an important mediator of immune function and is
expressed in T cells. Recently we deciphered the unique mechanism by which DUSP5
dephosphorylates pERK (pTpY). Under acute viral infection condition, we reported that Dusp5
knock-out (KO) mice show T-cell survival defects. In this work, we have now extended our studies
to investigate if DUSP5 regulates the function of CD8 T cells during chronic viral infection.
Methods:
We generated bone marrow chimeric mice to investigate the impact of DUSP5 deletion, on CD8 T
cell function during chronic viral infection. LCMV clone 13 virus was used as a chronic viral
infection model. GP33 tetramer was used to identify viral antigen specific CD8 T cells. Phenotype
of CD8 T cells and different pERKs (pTpY, pT, pY) were monitored by flow cytometry. Specific
permeabilization protocols were adopted to discriminate the pERK signals from nucleus versus
cytoplasm.
Results:
During chronic viral infection, antigen-specific CD8 T cells displayed more “˜exhausted’ phenotype
in DUSP5-/- mice, compared to wild type (WT) mice. Sub-cellular localization and expression levels
of different pERKs were altered in CD8T cells from LCMV-infected Dusp5 KO mice, compared to
WT ones. These suggest that in response to inflammatory immune environment following viral
infection, cellular “˜anti-stress’ machinery was altered in Dusp5 KO CD8T cells.
Conclusions:
DUSP5 is critical in intrinsically regulating the function of CD8T cells during chronic viral infection.
Our preliminary data suggests that DUSP5 acts as “˜rheostat’ in fine-tuning the cellular
distribution of pERKs to regulate anti-viral CD8 T cell response.

Research Day 2019
Jump to Table of Contents 55
Pulmonary
Poster #
38 (NOT PRESENTING)
Abstract Title:
Acute and chronic changes in the control of breathing in a rat model of bronchopulmonary
dysplasia
Presenter(s):
Gary C Mouradian
Authors:
Gary C Mouradian, Santiago Alvarez-Argote, Ryan Gorzek, Gabriel Thuku, Teresa Michkalkiewicz,
Margaret T.T. Wong-Riley, Ganesh Konduri, Matthew Hodges
Dept/Division:
Physiology
Category:
Junior Faculty
Introductions:
Infants born very prematurely (<28 wk gestation) have immature lungs and often require
supplemental oxygen (hyperoxia). However, prolonged hyperoxia exposure can exacerbate
alveolar and pulmonary capillary development and lead to bronchopulmonary dysplasia (BPD).
BPD is associated with increased morbidity and mortality, including increased risk for sudden
infant death syndrome (SIDS). The neural mechanisms controlling breathing are highly plastic
during fetal and neonatal development. With time, infants with BPD breathe independently.
Herein we tested the hypothesis that neonatal hyperoxia exposure acutely and chronically alters
the control of breathing.
Methods:
Time-pregnant Sprague Dawley rats were housed in the BRC and at birth, when the lungs are at
the equivalent developmental period as the very preterm infant, the dam and pups were moved
into a chamber for 10 days of hyperoxia (FIO2 >90%) or normoxia (room air) exposure. At
postnatal day (P)10 all rats were under normoxic conditions. Eupneic and hypoxic ventilation was
measured at P10, 12, 14, 17, 21, 43, and 60 by whole-body plethysmography. SpO2
measurements were obtained with a mouseOx during ventilatory measurements. Airway
resistance was assessed at P10-11, 20-21, and 60. Poincare analyses were used to assess control
of breathing variability for tidal volume and breathing frequency. Lung and brain tissue were
collected from subgroups of rats on P10, 21, and 60 for quantification of lung injury and
assessment of neural architectural changes within key respiratory nuclei.
Results:
Hyperoxia exposure caused a BPD phenotype measured at P10, 21, and 60 indicated by reduced
alveolar surface area, alveolar counts, and modest increases in airway resistance. Hyperoxia-
exposed rats had chronically elevated eupneic and hypoxic ventilation and large fluctuations in
breathing variability from P10 through P60 unlike normoxic rats. Under room air conditions
hyperoxic rats at all ages maintained SpO2 values equivalent to normoxic rats driven by a
significant hyperventilation. However, hyperoxic rats were unable to sustain SpO2 value
equivalent to normoxic rats during acute hypoxia, due in part to lung injury and acutely reduced
(P12 and 14) hypoxia sensitivity. Changes in ventilation and variability at P60 were associated with
increased expansion of astrocytes within 6 of 8 and increased number of neurons in 1 of 8 key
respiratory control nuclei.
Conclusions:
The results validate the hypothesis that prolonged neonatal hyperoxia causes developmental and
sustained changes to the control of breathing, which may be centrally mediated. These studies
indicate hyperoxia associated with BPD may lead to increased respiratory rigidity and reduced
hypoxic ventilatory sensitivity during a critical developmental window, which may increase the
risk of SIDS. Together, these results suggest BPD infants have fundamentally different neural
control of breathing mechanisms.

Research Day 2019
Jump to Table of Contents 56
Pulmonary
Poster #
39
Abstract Title:
Assessment of Regional Heart Function in Pulmonary Hypertension Using MRI
Presenter(s):
Victor Magana, El-Sayed H. Ibrahim
Authors:
Victor Magana, Micaela Young, El-Sayed H. Ibrahim
Dept/Division:
Radiology
Category:
Student
Introductions:
Cardiovascular magnetic resonance imaging (CMR) is the gold standard for evaluating heart
structure and function. It is a non-invasive, safe imaging modality with high resolution and tissue
contrast while avoiding ionizing radiation. Various MRI techniques are available for evaluating
cardiac function. Specifically, MRI tagging shows value in detecting regional cardiac abnormalities,
which typically precede global dysfunction. Pulmonary hypertension (PH) is a disorder
characterized by increased blood pressure in the pulmonary circulation and the right side of the
heart. Right ventricular (RV) function is assessed for PH evaluation. This is typically done using
right heart catheterization (RHC), an invasive procedure. However, due to interventricular
coupling, left ventricular (LV) function is also affected in PH, especially in severe cases, although
little is known about LV function in PH. In this study we used MRI tagging to study LV contractility
patterns in PH patients.
Methods:
MRI tagged images were acquired in 84 PH patients confirmed by RHC. The tagged images were
analyzed using InTag software package to generate different myocardial strain components-
circumferential (Ecc), radial (Err), and longitudinal (Ell) from four-chambered and mid-ventricular
short axis tagged images. Image analysis was done by two observers and inter-observer
comparison was done using Bland-Altman analysis. Correlation analysis was conducted to study
association between MRI strain parameters, and statistical t-test was performed to study
significant measurement differences on a regional basis and between severe (N=21) and mild
(N=63) PH patients. PH was considered severe when RV pressure exceeded the LV’s resulting in
leftward septal wall bowing during systole.
Results:
Bland-Altman analysis proved good inter-observer agreement where almost all measurement
differenced lied within 2 standard deviations (SD) limit. Ecc, Err, and Ell for all patients were -
13.7±3.8%, 15.7±5.6%, and -12.6±3.0%, respectively. This shows reduced myocardial contractility
compared to normal ranges (>17%) from the literature. Regionally, septal Err (14.3±4.9%) was
significantly reduced compared to lateral values (17.8±8.4%). Further, septal Ell at the basal level
was significantly reduced compared to lateral values (-8.94±5.6% vs. -12.1±7.1%; p=.0013). Finally,
both Ecc (-12.3±3.8% vs. -14.2±3.7%; p=.04) and Err (15.1±3.9% vs. 15.9±6.0%; p=.0001) showed
significant differences between severe and mild PH cases.
Conclusions:
MRI is a valuable tool in evaluating heart function in PH patients. MRI tagging showed reduced LV
myocardial contractility, especially in severe cases where Err and Ecc were significantly reduced
compared to mild cases. Regionally, septal myocardial strain (especially Err) was significantly
reduced compared to lateral measurements. As a result of interventricular coupling, LV function is
affected in PH patients, especially in severe cases where the RV pressure exceeds the LV and
causes septal bowing. In conclusion, myocardial strain analysis using MRI tagged images provides
sensitive regional function parameters that allow for characterization of ventricular contractility
pattern in PH.
Reference 1:
Benza et al. J Am Coll Cardiol;52:1683-92
Reference 2:
Marrone et al. Int J Cardiovasc Imaging;26:665-81
Reference 3:
Ibrahim, Heart Mechanics MRI. CRC Press, 2017

Research Day 2019
Jump to Table of Contents 57
Technology, Methods & Resources
Poster #
40
Abstract Title:
High Resolution Lymphatic Imaging with a Dual NIR-SWIR Multispectral Imaging System
Presenter(s):
Chris Hansen
Authors:
Chris Hansen, Jaidip M. Jagtap PhD, Gayatri Sharma PhD, Abdul Parchur PhD, Amit Joshi PhD
Dept/Division:
Biomedical Engineering
Category:
Student
Introductions:
Near infrared (NIR) optical fluorescence has been used extensively for functional and molecular
imaging of small animals in vivo. These modalities are inexpensive, non-ionizing, require low
concentrations of contrast agents, and provide high temporal resolution. NIR-I light (700-900 nm),
and Shortwave IR (SWIR, 1100-1500nm) can travel multiple centimeters through tissue because of
low absorption, and autofluorescence. The SWIR window has lower scattering, which increases
spatial resolution compared to NIR-I, but is relatively uncommon because of the few SWIR probes
and imaging sensors. There are no FDA approved SWIR probes. Most SWIR probes are low
bandgap semiconductors, however, indocyanine green has shown SWIR emission. Simultaneous
administration of different NIR and SWIR fluorescent probes allows for the investigation of
pharmacokinetics and biodistribution as well as systemic function, pathology, and vascular
phenotypes without cross-talk. We report a combined NIR-SWIR camera system for simultaneous
video-rate imaging in the NIR and SWIR spectra in rodents allowing for co-examination of
different fluorescent probes in the same anatomic structures.
Methods:
ICG (ex/em 785/810 nm) was used as an NIR-I and SWIR probe, while ~8nm silver sulfide (Ag2S)
quantum dots were engineered to emit in SWIR (ex/em 808nm/1200nm). A combination of
785nm and 808nm laser light excited the ICG and QDs, respectively. The camera system used a
16-bit deep cooled intensifier electron multiplying charge-coupled device (emICCD) camera (PI-
MAX4, 400-900nm sensitivity) and a 16-bit deep cooled InGaAs sensor focal plane array camera
(NIRvana 640ST, 900-1700nm sensitivity) in combination with a broadband beam splitter. Image
streams were acquired using LightField software (Princeton Instruments). Image processing and
data analysis were performed using MATLAB (Mathworks, 2018b) software. ICG and QD solutions
were administered by footpad injections in immunocompromised rats.
Results:
ICG emits in both the NIR-I and SWIR and provides a relative comparison between the two in
terms of resolution and intensity. ICG is thought to bind to albumin and other proteins, while the
polyethylene glycol coated QDs are almost neutrally charged. QDs are cleared more rapidly than
ICG during lymphatic imaging, thus making QDs an attractive probe for assessing lymphatic
clearance. However, long-term effects and potential toxicity of QDs have not been examined in
humans, meaning that any translation to the clinic is in the relatively distant future.
Conclusions:
We have demonstrated the use of a dual NIR-SWIR fluorescence imaging system in rats. The
combination of increased sensitivity and resolution can pick up deeper and smaller subsurface
lymphatics which can be missed by conventional NIR fluorescence imaging, as well as
demonstrating different pharmacokinetics of the probes.

Research Day 2019
Jump to Table of Contents 58
Technology, Methods & Resources
Poster #
41
Abstract Title:
RGD: data and tools for precision models of human disease
Presenter(s):
Jennifer R Smith
Authors:
Jennifer R Smith, Stanley J Laulederkind, G Thomas Hayman, Shur-Jen Wang, Matthew J Hoffman,
Mary L. Kaldunski, Harika S Nalabolu, Santoshi LR Ellanki, Jyothi Thota, Monika Tutaj, Marek A
Tutaj, Jeffrey L De Pons, Melinda R Dwinell, Mary E Shimoyama
Dept/Division:
Biomedical Engineering
Category:
Research Support Staff
Introductions:
A major challenge for preclinical research is finding, or establishing, a good model for the human
disease of interest—one that, more or less, faithfully recapitulates the phenotypic and genetic
profile of that disease in the human system. In many cases, canonical model organisms such as
rat or mouse are acceptable models, but this is not always the case. As such, the Rat Genome
Database (RGD, http://rgd.mcw.edu) has undertaken to incorporate additional mammalian
species to allow researchers to leverage a rich dataset across multiple species to find the best
model for their needs.
Methods:
In addition to rat, RGD has always offered data for human and mouse for the purpose of cross-
species comparisons. Now these have been enhanced with data for long-tailed chinchilla
(Chinchilla lanigera), 13-lined ground squirrel (Ictidomys tridecemlineatus), bonobo (Pan paniscus,
also known as pygmy chimpanzee), dog (Canis lupus familiaris), and pig (Sus scrofa). In each case,
these species are used as models for human disease, including diseases of the inner and middle
ear, retinal diseases, cancer, heart disease, arthritis, autoimmune dysfunction and hypoxia-
reperfusion injury.
Results:
Utilizing the existing robust and adaptable infrastructure, RGD has imported gene records,
genomic data and ortholog assignments for these species from NCBI, as well as protein
information and Gene Ontology (GO) annotations where available from UniProtKB. Further
functional information has been added to these records via the assignment of GO, disease and
pathway annotations based on sequence similarity to human, rat and mouse genes. In addition to
incorporating this data into the database, work is well underway to expand RGD's suite of analysis
tools to include genes from all of these species wherever possible. Chinchilla, dog, bonobo,
squirrel and pig JBrowse genome browsers have already been made available at RGD. All of these
species have also been incorporated into the OLGA advanced search and Gene Annotator tools, as
well as the new Gene and Ortholog Location Finder (GOLF) tool and the Multi Ontology
Enrichment Tool (MOET). Also, although the available data is limited, work is underway to add
these species to the InterViewer protein-protein interaction visualizer.
Conclusions:
This expanded offering of data for multiple species and the analysis tools to easily and efficiently
leverage this data gives researchers an excellent resource for discovering precision models for
their diseases of interest.
Acknowledgements:
RGD is funded by grant HL64541 from the National Heart, Lung, and Blood Institute

Research Day 2019
Jump to Table of Contents 59
Technology, Methods & Resources
Poster #
42
Abstract Title:
Computational study of Microwave ablation versus Plasmonic Nanoparticle Mediated
Photothermal Therapy for Liver Tumors
Presenter(s):
Mir Hadi Razeghi
Authors:
Mir Hadi Razeghi, Amit Joshi
Dept/Division:
Biomedical Engineering
Category:
Student
Introductions:
Microwave Ablation is an established clinical modality for ablation of liver tumors.
Electromagnetic waves are delivered via a percutaneously placed antenna in the tumor.
Commercial microwave probes can heat up the tissue to far more than hyperthermia region,
however the thermal contours are not controllable and thus therapy outcome depends critically
on the skill of radiologist placing the probe. Microwave ablation can cause irreversible damage to
healthy surrounding tissue. Here, we contrast and computationally compare microwave ablation
with low power near-infrared (NIR) laser ablation mediated with NIR resonant and tumor trapping
gold nanoparticles and demonstrate that laser-nanoparticle ablation can maintain enough
temperature for ablation, while restricting the ablation envelope to tumors and spare normal
tissue.
Methods:
COMSOL multiphysics 5.4a was used for finite element simulations of temperature pattern for
both microwave and photothermal ablation, by assuming a porous model for describing heat-
transfer in liver. For microwave ablation an Emprint microwave system with thermosphere
technology, with 25-cm probe ,and 2- 3 cm antenna size was simulated to deliver 20 - 100 W to a
human liver tumor for ~5 minutes. Photothermal ablation was simulated with a cylindrical laser
probe (808nm) and power delivered to the tumor was 4-8 W/cm2. The geometry of human liver
derived from an anonymized MRI scan was used for simulations, and tumors were modeled to
have an uptake of ~10 picomoles of 808nm resonant gold nanorod based nanoparticles recently
developed by us. (Parchur et. al. ACS Nano, 2018)
Results:
Our results indicate that both microwave and photothermal heating can achieve ablative
temperatures in tumor. However, the electromaghnetic waves expanding throughout the liver
and adjacent tissues cause irreversible damage due to very high temperature induction. Our
calculations demonstrate that for microwave ablation, the temperature and off-target thermal
damage is not controllable by varying power level if tumors are in challenging anatomical
locations.
Conclusions:
Photothermal ablation with plasmonic nanoparticles is an efficient method for treatment of liver
tumor. The ability of restricting the nanoparticle distribution in tumors can localize the therapy
envelop to tumors and protect normal tissue. However, the symmetrical nature of microwave
ablation limits the ability of controlling the temperature pattern without significant damage to
healthy tissues.

Research Day 2019
Jump to Table of Contents 60
Technology, Methods & Resources
Poster #
43
Abstract Title:
PhenoGeneRanker: A Tool for Gene Prioritization Using Complete Multiplex Heterogeneous
Networks
Presenter(s):
Cagatay Dursun
Authors:
Cagatay Dursun; Naoki Shimoyama; Mary Shimoyama; Michael Schlappi; Serdar Bozdag
Dept/Division:
Biomedical Engineering: Computational Biology and Bioinformatics
Category:
Student
Introductions:
Uncovering genotype-phenotype relationships is a fundamental challenge in genomics. Gene
prioritization is an important step for this endeavor to make a short manageable list from a list of
thousands of genes coming from high-throughput studies. Network propagation methods are
promising and state of the art methods for gene prioritization based on the premise that
functionally-related genes tend to be close to each other in the biological networks. Recently, a
new network propagation method called Random Walk with Restart on Multiplex Heterogeneous
Networks (RWR-MH) has been developed. RWR-MH performs random walk with restart on multi-
layered gene networks that are connected to a single-layer disease similarity network and ranks
disease-associated genes based on a set of known disease genes. Although, these methods are
very effective in gene prioritization, they are known to be biased toward high degree genes in the
network.
Methods:
In this study, we present an improved version of RWR-MH and its application on multi-omics
datasets of rice to effectively prioritize the cold tolerance related genes. Our method allows multi-
layer gene and disease networks. It also calculates empirical p-values of gene ranking using
random stratified sampling of genes based on their connectivity degree in the network.
Results:
Cold stress is a major factor in limiting the tropical plant of rice (Oryza sativa) crop yield in
northern hemisphere of the world. However, the genes that are related to cold tolerance in Oryza
sativa cultivars remain elusive. In order to prioritize cold tolerance related genes in rice, we
applied the improved RWR-MH on a multiplex heterogenous rice network. We created three-layer
cultivar similarity network namely, EL similarity, LTSS similarity, and genotype similarity network.
We also created three-layer gene interaction network, namely co-expression, protein-protein
interaction and pathway interaction network. We connected cultivar similarity network to the
gene network based on the GWAS results. We run the algorithm on this multiplex heterogenous
network using two known cold tolerance related genes as seeds and ranked all the genes.
Conclusions:
To evaluate our results, we performed GO enrichment of top 200 ranked genes. Our results
showed that the top 200 genes were enriched in GO terms such as “cell-wall” and “fatty-acid”
production, which are known to be related in cold tolerance in rice. As a negative control, we also
performed GO enrichment of the bottom 200 ranked genes and observed no GO enrichment as
expected. We also observed that candidate genes from GWAS results were ranked lower in
overall when the known cold-tolerant genes are used as seeds compared to using random seed
genes. Top-ranked genes also exhibited significant p-values suggesting that their rankings were
independent of their degree in the network. In conclusion, our results reported several novel
cold-tolerant genes that can be used for further experimental validation.
Acknowledgements:
This study was funded in part by grant HL64541 from the National Heart, Lung, and Blood
Institute on behalf of the NIH (to M. Shimoyama) and USDA AFRI NIFA grant @2016 6701302487
and #2018 67014027470 (to M. Schlappi).

Research Day 2019
Jump to Table of Contents 61
Technology, Methods & Resources
Poster #
44
Abstract Title:
NIR-II Emitting Quantum Dots for in vivo Preclinical Imaging Applications
Presenter(s):
Abdul K. Parchur
Authors:
Abdul K. Parchur, Jaidip M. Jagtap, Gayatri Sharma, Sandra Holzhauer, Weiqing Jing, Bryon D.
Johnson; Matthew Riese, Hu Wenquan, Fang Zhi, Qing Miao and Amit Joshi
Dept/Division:
Biomedical Engineering
Category:
Research Support Staff
Introductions:
Near-infrared (NIR) region with low tissue absorption enables background and auto-fluorescence
free visualization of targeted disease processes. We illustrate NIR emitting Ag2S QDs variants (<8-
nm) for deep-tissue imaging in the 2nd NIR window for (i) T-cell tracking in vivo and (ii) early
detection of intracranial haemorrhage (ICH) in mouse models imaged with a home-built NIR
imaging system
Methods:
Ag2S QDs were engineered with positive (-NH2), negative (-COOH), and neutral (mPEG) surface
charge and strongly luminesce at 1200-nm. For cell-tracking both positive and negative surface
charge of Ag2S QDs was incubated with different concentration of Ag (0-100 μg/mL) for rapid
uptake in isolated mouse T-cells (C57BL/6J, 50, 000 cells/well) and optimal incubation time and
concentration was determined and tested for cytotoxicity. The ability of labeled T-cells
to retain biological activity was tested in a RAG-/- mouse (no native T-cells) infected with Listeria
strain Lm-OVA. For direct in vivo imaging of vascular deficits induced by hyperglycemia induced
ICH in cerebral cavernous malformation (CCM) mouse models, PEGylated QDs with -6.7mV
surface charge were tail vein injected (200 μL of 30μg/mL Ag) in age matched CCM1
heterozygous mice (n=6) and controls (C57BL, n=6). Both groups were treated with STZ, and
monitored until the blood glucose rise to 300-500 mg/dL. Brain ROI-time series was compared
between CCM1 heterozygous and control mice. For verification of ICH, excised mice brains post
NIR imaging were imaged with micro-CT images. H&E stain was used for microscopic examination
of CCM1 tissues and verify ICH in locations identified by micro-CT.
Results:
30-60 min incubation was sufficient to label T-cells with negatively charged (-20mV) QDs with
concentration equivalent to 50-75 μg/mL of Ag with minimal cytotoxicity whereas positively
charged QDs (+18 mV) exhibited dose-dependent cytotoxicity. The bio-distribution of labelled T-
cells significantly altered in mice with Listeria infection compared to control mice, with T-cell
localization observed in liver and gut. After termination of imaging, mice were sacrificed, and liver
and spleen of mice were homogenized to extract T-cells for testing activation. The ex vivo flow
cytometric analysis confirmed the expression of the cell surface marker CD69 on CD8+ T cells,
confirming activation only in Listeria infected mice. For imaging ICH in mice, NIR-II fluorescence
image from control and CCM1 mice at 10s post injection of QDs demonstrated increased wash-in
in CCM1 mice treated with STZ. Mean NIR-II intensity from both control and CCM1 group is
statistically significant differences in contrast kinetics was observed (p<0.05). micro-CT and H&E
analysis verified the presence of ICH.
Conclusions:
This study validates that deep penetrating SWIR QDs labeled T cells can be used for whole-body T-
cell tracking as well as for monitoring the development of vascular pathologies such as in
hyperglycemia induced ICH in mouse models of CCM.
Research Day 2019
Jump to Table of Contents 62
Technology, Methods & Resources
Poster #
45
Abstract Title:
Applications and Methods to Give Meaning to Exome and Genome Based Data in Research
Presenter(s):
Wendy M. Demos
Authors:
Wendy M Demos M.S. 1, Jenica Abrudan1Ph.D. 1, Lida Zeighami M.S. 1, Stefano Rosati B.S. 1,
Michael Zimmermann Ph.D. 1,2,3
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
The widespread use of Whole Genome Sequencing (WGS) and Whole Exome Sequencing (WES) for
research discovery creates demand for efficient and effective workflows to support a diversity of
applications including understanding mechanisms of human disease and genetic predisposition. The
basic output of a standard WGS/WES analysis is a variant call file (VCF). The VCF serves as a listing of
coordinates where samples differ from a defined reference genome. All variants have standard
information such as location, quality metrics, and coverage counts, but additional data in the VCF usually
relates to meaning of the variant and how it is distributed across a sample or cohort. Due to the size of
WGS/WES, thousands to millions of variants can be called, necessitating scalable approaches. We have
developed a workflow and reporting infrastructure to efficiently bring together raw data processing and
annotation to give meaning to variants found in WGS and WES based research initiatives.
Methods:
We have developed research specific WES and WGS workflows to compliment the long-standing clinical
genomics services of the GSPMC. The underlying framework for the data processing utilizes the broadly
used Genome Analysis Tool Kit (GATK) (1) and implementation based on the Broad Institute best
practices. We have also deployed a technical filtering method which filters out low quality data and is
customizable for single sample or cohort approaches. In order to support the flexibility in annotation
resources required to drive research, we have integrated BioR(2) and SnpEff into our workflow to
annotate genomic data with clinically relevant and domain-specific information, to enhance the scope of
research and support discovery.
Results:
We developed a standardized analysis workflow that processes raw sequence files and provides quality
metrics, data visualizations, and knowledge-based annotations to facilitate the interpretation of
experimental results. The workflow generates an interactive web-based report which provides at-a-
glance insights to the quality of NGS sequencing, impactful data summaries including the variant
landscape, prioritization and classification of genetic variation, and variant distribution to facilitate
further interpretation of the annotated data. We demonstrate the application of our workflow on a
cohort of Qatari subjects with and without type 2 diabetes(3).
Conclusions:
We believe the systematic and comprehensive annotation of genomic data is required for extracting the
most meaning out of each study. Therefore, we have built a robust end-to-end workflow that can be
applied to a broad spectrum of research applications, increasing efficiency, standardization, and data
interpretability. This process enables researchers to efficiently identify the most promising candidates in
their study, develop hypotheses, and effectively reach to the next stage of their research endeavors.
Reference 1:
Van der Auwera GA, Carneiro M, Hartl C, Poplin R, del Angel G, Levy-Moonshine A, Jordan T, Shakir K,
Roazen D, Thibault J, Banks E, Garimella K, Altshuler D, Gabriel S, DePristo M, From FastQ Data to High-
Confidence Variant Calls: The Genome Analysis Toolkit Best Practices Pipeline 2013 Current Protocols in
Bioinformatics 43:11.10.1-11.10.33
Reference 2:
Kocher JP, Quest DJ, Duffy P, et al. The Biological Reference Repository (BioR): a rapid and flexible
system for genomics annotation. Bioinformatics. 2014;30(13):1920-1922.
Reference 3:
O’Beirne SL, Salit J, Rodriguez-Flores JL, Staudt MR, Abi Khalil C, Fakhro KA, et al. (2018) Exome
sequencing-based identification of novel type 2 diabetes risk allele loci in the Qatari population. PLoS
ONE 13(9): e0199837. https://doi.org/10.1371/journal.pone.0199837 (SRA accession #SRP061463,
BioProject 288292).

Research Day 2019
Jump to Table of Contents 63
Technology, Methods & Resources
Poster #
46
Abstract Title:
Bioinformatic and Data Analytic services offered by the GSPMC
Presenter(s):
Michael T. Zimmermann
Authors:
Michael Zimmermann, Stephano Rosati, Atefeh (Lida) Zeighami, Jenica Abrudan, Raul Urrutia
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Junior Faculty
Introductions:
Precision Medicine encompasses a wide array of new technologies that enable researchers and
clinicians to address new questions - to increase the specificity of care that drives improvements
for patients’ diagnosis or treatment. Precision Medicine often begins with genomic profiling. The
human genome is a big place and different tests are warranted depending on how comprehensive
a view is needed. That is, GSPMC supports a range or DNA-based testing from whole-genome,
through exome, to custom panel testing. DNA-based testing allows clinicians and researchers to
diagnose genetic diseases, explore genotype-phenotype associations, and to determine
unrecognized genomic contributors to established conditions. Beyond DNA testing, transcriptomic
and epigenomic sequencing enable researchers to understand regulatory changes that may
change the presentation of, or supersede, information in the DNA.
Methods:
Bioinformatics is the discipline of processing the large amount of data from these assays and
generating information that is human interpretable. Data analytics is a broad area including the
management of data itself and the computation needed to support bioinformatics. Data
visualization, statistical assessment, and effective communication are required for successful
analytic and bioinformatic outcomes. Further, analyses must help to directly address the critical
questions that clinicians and researchers aim to answer. Therefore, we have assessed a wide
range of technologies.
Results:
Our bioinformatics team has assembled and continues to improve upon a suite of standardized
and comprehensive analysis reports that span the technologies supported by GSPMC. Specific
assays have translated into clinical tests, while a broader portfolio is offered to support research.
For DNA-based assays, we comprehensively identify alterations (SNV, INDEL, Copy Number, etc.)
to annotate and investigate how they change genes, cis- and trans-regulatory regions, pathways,
and cellular processes. We emphasize variant annotation and interpretation. Within
transcriptomic analyses, we identify differential expression of gene transcripts and gene sequence
changes. We emphasize RNA quality control, differentially expressed genes or transcripts, and
which high-level patterns in the dataset most strongly differentiate among conditions. For
epigenetic sequencing, we map the methylation landscape of the genome, present robust
summaries, identify differentially methylated regions, and annotate likely downstream effects.
Across all analyses, we aim to support data interpretation. All services are also available to
researchers as well, for projects, grants, clinical trials, and collaborative needs.
Conclusions:
GSPMC is focused on the vision of new knowledge changing the practice of medicine and
increasing the resolution and quality of research services. We want every individual to benefits
from a lifetime of tailored care through Precision Medicine, enabled by robust bioinformatics
support.

Research Day 2019
Jump to Table of Contents 64
Technology, Methods & Resources
Poster #
47
Abstract Title:
Innovation to Practice - Basic and Translational Research Tools, Services, and Assays in GSPMC
Presenter(s):
Mike Tschannen
Authors:
Angela Mathison, Michael Tschannen, Veronica Ramos, Chuck Salmonson, Raul Urrutia
Dept/Division:
GSPMC
Category:
Research Support Staff
Introductions:
Genomics is being used to understand, prevent, detect, and treat diseases with precision, and
GSPMC is at the forefront of these innovative discoveries. Pairing cell and molecular biology
techniques with NexGen sequencing allows for mechanistic dissection of the initiation,
establishment, and progression of diseases. Our goal is to advance research and innovative
clinical diagnostics at MCW that allows the efficient translation of new technologies and
applications to basic, translational, and clinical research,1 so as to address the unmet needs of
patients and the community. Here, we provide examples that highlight these activities
Methods:
To facilitate the translation of innovation to practice, GSPMC has established consultations for
researchers with a service product that has the potential to be used in patient care as well as
initiating the experimental plan, designing state-of-the-art library preparation and sequencing
technologies, and bioinformatic support for translating data to knowledge. Working in close
collaboration with the molecular diagnostic laboratory, we are also able to finetune innovations
enabling translation to the clinic. All of these services are available to basic and translational
researchers to ensure that Precision Medicine becomes a reality for all patients.
Results:
The GSPMC has established a full spectrum work flow that include consultation and facilitation
customizable per need from extraction-to-analysis sequencing services with troubleshooting and
data bioinformatics support. GSPMC now extracts DNA and RNA from blood, formalin-fixed
paraffin-embedded (FFPE), and fresh frozen cells or tissues. By understanding the input source
material, the R&D team adjusts protocols to produce the most accurate and relevant data. Once
extracted, GSPMC applies optimized methods to interrogate intact or degraded DNA through
genome and exome sequencing. Beyond the relatively stable genetic information, GSPMC also
provides dynamic snapshots of cellular activity at the molecular level through transcriptomic
sequencing (RNAseq). The R&D team’s refined methods can even unlock expression data through
low-input and single cell technologies. Finally, with the explosion of epigenomics and an
understanding that there are multiple layers of expression control beyond the genomic sequence,
GSPMC offers reduced representation bisulfite (RRBS) and chromatin immunoprecipitation (ChIP)
sequencing. With all GSPMC services, bioinformatic support is available to collaborate, analyze,
interpret, and integrate these diverse data sources.
Conclusions:
GSPMC’s vision is to innovate and drive cutting-edge technologies that will advance basic
mechanistic understanding of disease etiology, pathophysiology, and potential therapeutics with
the goal of increasing the knowledge base in translational, personalized medicine research. Using
experience from a variety of projects, GSPMC will tailor assays, provide services and collaborate
to address the current and future needs of researchers throughout MCW.
Reference 1:
1. Goldblatt, EM and Lee, W-H. From bench to bedside: the growing use of translational research
in cancer medicine. Am J Transl Res 2010;2(1):1-18

Research Day 2019
Jump to Table of Contents 65
Technology, Methods & Resources
Poster #
48
Abstract Title:
Advancing Cancer Precision Medicine through Innovative Methods for the Interpretation of
Genomic and Epigenomic Data Generated by Next Generation Sequencing
Presenter(s):
Young-In Chi
Authors:
Michael Zimmermann, Angela Mathison, Young-In Chi, Gwen Lomberk, Brian Volkman, and Raul
Urrutia
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Junior Faculty
Introductions:
Clinical application of DNA-based testing using high-throughput technologies has led to the
identification of many novel variants, many of which lack prior clinical evidence, making their
implications for the patient uncertain. For this reason, they are categorized as Variants of
Uncertain Significance (VUS).1 We must move “beyond the base pairs” in order to gather and
interpret genomics data, establish molecular mechanisms, and translate tumor genomics data
into actionable knowledge. We have established the Precision Medicine Simulation Unit (PMSU)
by joining a multidisciplinary team to apply experimental and computational simulations for how
genetic variation alters the function of epigenetic regulators. We are starting with a set of
regulators that, when altered, are known to cause congenital diseases or drive cancer.
Methods:
Computational tools for simulating the atomic-level effects of variants on protein structure and
dynamics are well established, but have not achieved systematic use in clinical settings. We are
applying molecular modeling and simulation to generate specific hypotheses for the molecular
effects of VUSs identified during the course of clinical genomics sequencing. Detailed
computational analyses represent an additional level of information for the interpretation of VUSs
- information that is overlooked by current clinical guidelines. Because the dynamics of each
protein differ from one another, we generate protein-specific metrics for quantifying how variants
affect the protein. Additionally, our process leverages multiple established disease variants as well
as polymorphisms as comparators for determining the significance and consistency of VUS-
associated effects.
Following computational simulations, we are applying in vivo cell-based assays to investigate how
the molecular effects alter structure and function of the proteins and downstream properties of
cellular regulatory networks. Specifically, nuclear magnetic resonance (NMR) spectroscopy will
allow for in vitro discovery of the gene’s biophysical structure and predict functional alterations.
Functional assays are next used as an in vivo interpretive assay to determine the type of alteration
(enhanced, reduced). Finally, as variants will be focused toward epigenetic regulators, RNA-seq
and ChIP-seq are used to understand the global regulation and biological pathways that are key
drivers in disease and cancer.
Results:
Here we present our process for molecular modeling, biophysical structure analysis, and
epigenetic sequencing data for specific examples of VUS identified through next-generation
sequencing of clinical cases presenting with undiagnosed diseases or in cancer. Functional
validation using experimental protein-based and cell-based assays confirmed the effects
predicted by modeling.
Conclusions:
We believe molecular modeling and functional genomics will become an increasingly important
component in the process of interpreting the effects of human genetic variation. Therefore, we
are optimistic that this study will yield novel information with a rapid translational potential for
treating human disease.

Research Day 2019
Jump to Table of Contents 66
Technology, Methods & Resources
Poster #
49
Abstract Title:
Developing and Implementing a Robust and Thorough RNA-Seq Data Analysis and Deliverable
Report
Presenter(s):
Atefeh (Lida) Zeighami
Authors:
Atefeh (Lida) Zeighami, Jenica Abrudan, Stefano Rosati, Romica Kerketta, Wendy Demos, Raul
Urrutia, Michael T. Zimmermann
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
RNA-Seq is a technique to quantify gene expression and thereby study transcriptomic differences
between biologic conditions.
We broadly divide RNA-Seq analysis in two parts: Experimental and Computational. Experimental
methods and their quality control (QC) are critical foundational steps. Thus, we have developed a
robust system for monitoring sample and experimental quality throughout our process. The
experimental output of RNA-Seq is raw nucleotide sequences. Computational analyses begin from
these data. There are different software and pipelines available to analyze raw data and generate
feature (gene/exon/transcript) quantification, identify deferentially expressed genes, discover
novel transcripts, annotate functions affected, call expressed variants, and detect gene fusions .
As scientific inquiry is constantly evolving, robust yet flexible bioinformatics approaches are
required to facilitate research.
Methods:
To process RNA-Seq data, we have built two workflows based, one on “pseudo alignment”
(Kallisto) and one on “standard alignment” (MapRseq) methods. These custom RNA-Seq pipelines
intake raw reads and output a comprehensive and interactive web-based report. We have
significantly decreased our processing time through automation, included additional quality
controls, quality assurance, robustness checks, and built in statistical analysis to create a
comprehensive report. We are integrating batch correction techniques such as Conditional
Quantile Normalization and Empirical Bayesian methods to facilitate normalization, data
integration, and to avoid spurious associations, resulting in a more robust differential expression
analysis.
Results:
We have expanded our workflow a tool to generate an interactive and comprehensive web-based
report to deliver the results of RNASeq and Differentially Expressed Analyses, along with QC
metrics, and presented in accessible ways. This report includes summary of experiments/samples,
sequencing metrics, pre-alignment/alignment quality assessment, Gene/Exon counts (raw and
normalized value), batch effect removal results, Differential expression analysis (using two
different approaches, Pairwise and GLM) and visualization such as PCA plot, Scree plot, Sample
clustering dendrogram, PCA loading, Venn diagram, Volcano plot, HeatMap and DE-PCA plot. The
workflows have also been improved to support analysis multiple organisms including human, rat,
mouse, and pig.
Conclusions:
We have Developed and Implemented a Robust and Thorough RNA-Seq Data Analysis and
Deliverable Report tool, under continual analytic improvement, to facilitate research analyses.
Reference 1:
Bray, N.L., et al., Near-optimal probabilistic RNA-seq quantification. Nat Biotechnol, 2016. 34(5):
p. 525-7.
Reference 2:
Kalari, K.R., et al., MAP-RSeq: Mayo Analysis Pipeline for RNA sequencing. BMC Bioinformatics,
2014. 15(1): p. 224.

Research Day 2019
Jump to Table of Contents 67
Technology, Methods & Resources
Poster #
50
Abstract Title:
Quality & Precision in the Next Generation Era: An analysis of Illumina Chemistry & Quality score
changes
Presenter(s):
Stefano Rosati
Authors:
Stefano Rosati B.S., Mike Andresen B.S., Wendy M Demos M.S., Jenica Abrudan Ph.D., Lida Zeighami
M.S., Michael Zimmermann Ph.D.
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
The NovoSeq 6000, Illumina’s flagship genetic sequencer represents the latest breakthrough of high throughput
sequencing technology. The NovoSeq’s largest flowcell the S4 can reliably generate 16-20 billion paired end reads
in 44 hours. The NovoSeq can run two flow cells concurrently, and has multiple smaller flowcells available to it,
lending itself to both flexibility and immense throughput. While the NovoSeq represents a much-needed
throughput gain needed to drive the precision medicine era, subtle changes were quietly made to the NovoSeq’s
sequencing chemistry and to its fastq quality estimate algorithm
1,2
. NovoSeq chemistry uses two channel SBS
sequencing, to allow for faster data generation. Red fluorescence represents C bases, green represents T,
red+green represents A, and no fluorescence represents G
1
. This chemistry may lead to inaccurate quality of “G”
bases, as well as difficulty discerning heterozygous C/T sites from A sites. Simultaneously, NovoSeq’s phred
quality score is revamped from previous technologies. Previous generations of sequencers assessed quality from
a scale of Q10 through Q40 to 4 possible quality scores
2
: Q2, Q12, Q23 and Q37. Illumina documentation states
the base quality assessment is “highly accurate”, but little literature has compared the sequencing output quality.
In this study, we assess the effect of these changes on per base quality assessment.
Methods:
23 whole exome sequencing samples (WES), 11 whole genome (WGS) libraries and 1 Mitochondrial control were
library prepped individually. All 35 libraries were run on an Illumina MiSeq 50 base pair kit, and subsequently run
on the NovaSeq (S1, S2, or SP) 2 x 150 base pair kits. The first 50 bases of 10,000 randomly selected reads were
converted to probability scores. Quality scores were averaged by base and were compared between the MiSeq
and the NovaSeq sequencing output.
Results:
A comparison of the mean phred scores of the first 50 bases of sequencing showed the per-base MiSeq phred
score Q37.543 or probability of accuracy was 99.981%. The NovoSeq phred score was Q36.086, meaning
probability each base call being accurately was 99.975%. A comparison of the average basecall for all bases shows
NovoSeq data has a large cluster around phred score of 36, with a tail reaching down towards a basecall
probability of .9992. The MiSeq basecall probabilities have higher basecall probability, with a shorter tail. Plotting
the average quality per base for both instruments shows that the MiSeq quality has lower quality to start reads.
The read quality then reaches maximum basecall probability around base 21. NovoSeq quality scoring has a much
more consistent base quality for reads. A higher standard deviation can be seen for NovoSeq basecall qualities.
Conclusions:
NovoSeq basecall quality scores are show more variability in their quality calls, as the probability assigned to one
of four quality scores, whereas the MiSeq has many intermediate qualities that can be assigned. Phred scores of
Q2, Q12, Q23 and Q37 equate to a basecall probability of 36.90%, 93.69%, 99.49% and 99.98% respectively. The
logarithmic nature of phred scores is misleading as there is only .49% difference between Q23 and Q37 base
qualities. MiSeq sequencing quality scores compared to the new NovoSeq quality scores do not seem to drastically
affect raw quality assessment of sequenced reads. However, it cannot be ignored that some pipelines may be
more susceptible to the effect of NovoSeq chemistry and quality scores than others. All bioinformatic pipelines
should be adequately tested using NovoSeq data before use. The trenching of NovoSeq quality scoring has one
very positive impact on sequencing data: as NovoSeq fastq data has many less possible characters, files are much
more compressible. This is a very welcome to a field that has seen a massive explosion of data3. Increased
compressibility lowers the unseen cost storing clinical and research genomic data- making the technology more
accessable for everyday use.
Reference 1:
Illumina (2017). NovaSeq„¢ 6000 System Quality Scores and RTA3 Software. https://www.illumina.com/content/dam/illumina-
marketing/documents/products/appnotes/novaseq-hiseq-q30-app-note-770-2017-010.pdf
Reference 2:
Illumina (2018). Illumina CMOS Chip and One-Channel SBS Chemistry. https://www.illumina.com/science/technology/next-
generation-sequencing/sequencing-technology/2-channel-sbs.html
Reference 3:
Stephens, Zachary D., Skylar Y. Lee, Faraz Faghri, Roy H. Campbell, Chengxiang Zhai, Miles J. Efron, Ravishankar Iyer, Michael C.
Schatz, Saurabh Sinha, and Gene E. Robinson. "Big data: astronomical or genomical?." PLoS biology 13, no. 7 (2015): e1002195.

Research Day 2019
Jump to Table of Contents 68
Technology, Methods & Resources
Poster #
51
Abstract Title:
Protein Scores for the Advancement of Precision Medicine and Genomics Data Interpretation:
Application to RAS Proto-Oncogenes
Presenter(s):
Swarnendu Tripathi
Authors:
Swarnendu Tripathi, Nikita R. Dsouza, Raul A. Urrutia, Michael T. Zimmermann
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
Genetic variants activating Rat sarcoma (RAS) genes are among the most recurrent somatic
alterations in human cancers. Interestingly, germline genetic variants in RAS are also responsible
for rare congenital diseases (e.g., Noonan and Constello Syndromes). There are two highly
recurrent RAS activating variant sites in cancer (hotspots), but many genetic alterations are
observed outside of the hotspot sites - somatically in cancer, in rare diseases, and in the currently
healthy adult population. This genetic spectrum differs for each member of the RAS family.
Experimental data indicate that each type of alteration at the hotspots can lead to different
downstream effects and that non-hotspot variants may not alter the protein in the same way as
hotspot mutations; non-hotspot variants may not have the same implications for clinical
management. Thus, better methods to evaluate how genetic variation outside of the hotspots
affects RAS function is needed in order to interpret their effects.
Methods:
We propose a computational framework to better interpret the broad genetic variation RAS
proteins and what it may mean for RAS function. We developed a system for the application of
many individual scores that account for data at the DNA sequence, protein sequence, and 3D
protein structural levels. Choosing many scores that assay a broad range of protein properties will
help to identify the specific molecular effects of each genomic variant. At each level, we chose a
subset of scores that each provide information about a different type of property based on our
knowledge of proteins as well as the correlation structure between the scores when individually
applied to a dataset of genomic variants.
Results:
We applied our scoring system to the GTPase domain of seven RAS family proteins. We used
multiple sources spanning cancer, germline disease, and the healthy population to provide a more
comprehensive view of RAS variation. Our bioinformatic filtering criteria identified 935 unique
protein variants across seven RAS genes. We used the many individual scores to assess the
differences among RAS variants and identified groups of variants that affect the protein in similar
ways. We believe each of these groups will represent a different mechanism of dysfunction. Using
the same data, we trained a machine learning classifier to distinguish from among germline
pathogenic, somatic, and non-disease genetic variants, to learn which patterns of altered features
best associated with pathogenicity.
Conclusions:
We demonstrated that information relevant to interpreting genomic variants that are not
currently predictable or available from the DNA sequence can be derived from a computational
study of the protein 3D structure. We believe that our approach is applicable to a broad range of
the human proteome and will become an important criterion in future versions of guidelines for
the interpretation of genomic variants.

Research Day 2019
Jump to Table of Contents 69
Technology, Methods & Resources
Poster #
52
Abstract Title:
A comprehensive, interactive, and visual RRBS analysis pipeline
Presenter(s):
Jenica Abrudan
Authors:
Jenica Abrudan, Lida Zeighami, Romica Kerketa, Wendy Demos, Raul Urrutia, Michael
Zimmermann
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
Gene expression is not only regulated by genetic changes, but by epigenetic changes such as DNA
methylation. One technique for studying genome-wide DNA methylation levels is Reduced
Representation Bisulfite Sequencing (RRBS).
Methods:
We used Bismark[1] to align sequencing reads to the reference genome because it is an RRBS-
specialized aligner with high community support. The methylated CpG sites and the DMRs were
identified using DMRfinder[2]. The coverage, methylation rate and end-user report are generated
using custom analysis in the R(3.5.1) programming language.
Results:
We developed an analysis pipeline to assess changes in DNA methylation and how they associate
with treatment groups or characteristics of the study cohort. Our process identifies differentially
methylated CpGs (DMCs) and regions (DMRs) and provides a set of data visualizations, statistical
comparisons, and knowledge-based annotations to facilitate their interpretation. First, we outline
the scope and goal of each project. Second, details regarding the setup and experimental
conditions are presented to facilitate review of quality control metrics. Third, multiple quality
control results from the perspective of the raw sequencing data, the aligned data and the raw
CpG data allowing the end-user to quickly assess the quality and reliability of the results. Next,
we statistically assess DMCs and show patterns across the study cohort that most strongly
associate with differences among samples using Principal Component Analysis (PCA). DMCs are
used as input to calculate the DMRs. We annotate DMRs for their likely cis-acting affect by
identifying nearby genes. We distinguish the likely biologic effect on genes by the location of the
DMR - if it is within the promoter, first exon, gene body, etc. Finally, we use the genes associated
with DMRs in pathway analysis. We visually represent the pathways genes are involved in and if
applicable allow for a visual comparison of the overlap of the genes across different experimental
conditions.
Conclusions:
The DNA methylation pipeline of the GSPMC Service Line has delivered to researchers a
standardized, efficient, and reproducible process and delivers a set of data quality assessment,
QC, and data visualization summaries. We have developed and will continue to improve this
workflow to provide an efficient, robust, and thorough analysis service.
Reference 1:
Krueger, F. and S.R. Andrews, Bismark: a flexible aligner and methylation caller for Bisulfite-Seq
applications. Bioinformatics, 2011. 27(11): p. 1571-2.
Reference 2:
Gaspar, J.M. and R.P. Hart, DMRfinder: efficiently identifying differentially methylated regions
from MethylC-seq data. BMC Bioinformatics, 2017. 18(1): p. 528.

Research Day 2019
Jump to Table of Contents 70
Technology, Methods & Resources
Poster #
53
Abstract Title:
Permanent Pacemaker (PPM) Detected Activity Time is More Sensitive to Changes in Activity
Levels than Pedometers in Sedentary Older Patients
Presenter(s):
Venkata Krishna Puppala
Authors:
Venkata Krishna Puppala, Benjamin C Hofeld, Sudhi Tyagi, Amberly Anger, Scott J Strath, Judith
Fox, Marcie G Berger, Michael E Widlansky
Dept/Division:
Medicine: Cardiovascular Medicine
Category:
Junior Faculty
Introductions:
Sedentary behavior increases the risk cardiovascular disease. In patients with permanent
pacemakers (PPM), physical activity (PA) can be monitored using PPM-embedded accelerometers
to measure pacemaker detected active hours (PDAH). We recently showed that low PDAH (‰¤2
hours/day) is a strong predictor of mortality. Our hypothesis is that a Physical Activity Counseling
Intervention (PACI) administered to at risk, sedentary individuals will increase PDAH and
pedometer-based average daily step counts.
Methods:
A total of 13 ambulatory patients aged >55 years (age 80±6 years, 84.6% female) with implanted
PPMs averaging ‰¤ 2 hours of PDAH daily average were included in this study. Patients were
randomized to Usual Care (UC) or our PACI group (n=6, 7 respectively). Step counts measured by
pedometer (Omron HJ-112) and PDAH data were obtained at baseline and following 12 and 24
weeks of intervention. Data analysis was performed using unpaired t-tests, Pearson’s chi-square,
and general linear models for repeated measures as appropriate.
Results:
PDAH increased in all subjects over the intervention period by an average of 33% (P=0.01). This
increase did not differ by study group. PDAH significantly increased between weeks 1 and 12
(1.60±0.33 to 2.08±0.57 hours) with a trend toward a decrease between 12 and 24 weeks
(1.88±0.43 hours, P=0.052). Pedometer-based step counts did not differ over time in all subjects
(P=0.08) or by study group (P=0.12). Step counts and PDAH significantly correlated at baseline
(r=0.60, P=0.03). This correlation disappeared by week 12 (r=0.17, P=0.96) and the measurements
remained uncorrelated at week 24 (r=-0.04, P=0.90). The step counts at each time point remained
highly correlated with each other (Pearson’s r ranging from 0.75-0.90).
Conclusions:
Monitoring the impact of PA improving interventions can be performed using PDAH. In this
previously sedentary cohort, the increase in PDAH, without step count change and with poor
correlation with PDAH at weeks 12 and 24, suggests that active time was augmented by non-
ambulatory means or otherwise was not detectable by pedometer in this patient population. the
increase in PA suggests that patient awareness of the ability to monitor PA through a PPM can
increase PA in these patients.
Acknowledgements:
This grant was funded by an investigator-sponsored research grant to from Medtronic, Inc (CR-
3476). Dr. Widlansky is additionally supported by HL125409, HL128240, HL144098, and
R38HL143561, and AHA Strategically Focused Research Network grant (Hypertension Network).
Drs. Tyagi and Puppala were supported by T32GM089586. Dr. Hofeld is supported by
R38HL143561. Dr. Strath is supported by CA215318 and R21HD094565. The content is solely the
responsibility of the authors and does not necessarily represent the official views of the National
Institutes of Health

Research Day 2019
Jump to Table of Contents 71
Technology, Methods & Resources
Poster #
54
Abstract Title:
Clinical Survey Research: Design, Validation & Dissemination
Presenter(s):
Caroline Davitt
Authors:
Caroline Davitt, Kathryn Flynn, PhD, Anna Palatnik, MD
Dept/Division:
Obstetrics & Gynecology: Maternal-Fetal Medicine
Category:
Student
Introductions:
Survey research is a powerful tool to assess current practices in clinical medicine. Grounded in
psychological theory, the cognitive interview evolved as a qualitative method of providing face
validity to survey methodology. Rather than examining if the survey worked with a pilot, cognitive
interviewing attempts to understand how the survey is working. This allows researchers to
identify discrepancies in comprehension among respondents and gaps in information sought from
inquiry. Upon revision and final validation, a survey can then be administered, most frequently
electronically, to a representative population. The objective of this study was to design and
validate a provider survey focused on management of gestational diabetes.
Methods:
Extensive literature review was conducted of national and international surveys on the subject:
pharmacotherapy in gestational diabetes mellitus. Questions were generated based on previous
surveys and current literature guiding physician practice. The cognitive interview was designed to
evaluate at least three processes in Tourangeau’s original cognitive model of survey response for
each question; comprehension, retrieval from memory of relevant information, decision
processes, and/or response processes. Motivation and degree of satisficing were also examined
where appropriate. Cognitive interviewing was conducted concurrently, as opposed to
retrospectively, with both “think aloud” methodology and verbal probing. The survey was revised
and field experts consulted on question structure. Approval for dissemination through
professional society was sought (Pregnancy-Related Collaborative Research Network (PRCRN),
American College of Obstetrics & Gynecology (ACOG), Society for Maternal-Fetal Medicine
(SMFM)) and survey was transferred into a Qualtrics online platform (Qualtrics International Inc.,
2002, Seattle, WA).
Results:
Twenty survey questions were generated with input from a maternal-fetal medicine specialist and
a population scientist with experience in survey research. Seven providers from three different
subspecialties (Maternal-Fetal Medicine (2), General Obstetrics & Gynecology (3), Endocrinology
(2)) and various years in practice completed cognitive interviews. Interviews were conducted in-
person, one-on-one for an average time of 40 minutes per interview. Three questions were
completely reformatted after the interview to facilitate comprehension. The answer choices for
seven questions were altered to reflect accurate physician clinical practice. Finally, skip logic was
introduced to alleviate question burden for occupied providers. Electronic dissemination
substantiated via official societal posting, newsletter and email will occur in the Fall of 2019.
Conclusions:
Properly orchestrated clinical research survey design is both time and labor-intensive. The
product is a tool to accurately assess medical practice, in this case, among providers.
Multidisciplinary planning including psychology, sociology and clinical medicine are essential to
successful survey generation. Here, we describe the cognitive interview as a validation method as
well as the optimization of response rates among busy medical providers.
Reference 1:
Tourangeau, R. (1984). Cognitive sciences and survey methods. Cognitive aspects of survey
methodology: Building a bridge between disciplines, 15, 73-100.
Acknowledgements:
Rachel Harrison, MD; Rachel Cusatis, PhD; Kevin Regner, MD

Research Day 2019
Jump to Table of Contents 72
Technology, Methods & Resources
Poster #
55
Abstract Title:
Effect of -80°C Storage on RNA from Snap Frozen Placental Tissue
Presenter(s):
Schneider, Ellen Anje
Authors:
Schneider, Ellen Anje; Patton, Mollie; McIntosh, Jennifer; Pan, Amy
Dept/Division:
Pathology
Category:
Research Support Staff
Introductions:
Cryopreservation is integral to biorepository operations but inherently stressful to tissue.
Ribonucleic Acid (RNA) is a vital part of biomedical research but because of the ubiquity of
environmental RNAase and the fragility of RNA, researchers prefer to use fresh tissue for
requests. However, fresh tissue can be difficult to offer given the limitations of tissue transport,
study inclusion criteria, and biorepository staffing. Being able to offer researchers frozen tissue
with an estimated RNA quality would expand opportunities in maternal research.
Methods:
The Medical College of Wisconsin (MCW) Tissue Bank undertook a quality control (QC) study to
assess the RNA quality of cryopreserved placenta samples stored for differing amounts of time in -
80°C. Samples were collected as 75-100-micron sections using a Leica Cryostat from OCT
embedded snap frozen placenta tissue and isolated using a QuickGene 810 and Kurabo RNA from
Tissue Kit. Quality and quantity of RNA was assessed using a NanoDrop 2000 spectrophotometer.
Analysis of Variance (ANOVA) was performed to compare the ratios among the three groups and
a t test was used for comparison between two groups. A P<0.05 was considered significant. The
three cohorts of six samples each were stored for >18 months, 13-18 months, and <12 months for
a total N of 18.
Results:
There was no statistically significant difference among the three cohorts in A260/A280 ratio
(P=0.066) or in A260/A230 ratio (P=0.21). Comparing the > 18-month cohort to the combination
of the other two cohorts <18-months old showed that the older cohort had a significantly lower
A260/A280 ratio (1.91±0.07 vs 1.78±0.13, P=0.018) but there was no significant difference looking
at the A260/A230 ratio (P=0.13). The range of A260/A280 ratios across all 18 samples was 1.58 to
2.01; ratios close to 2.0 are considered pure. The A260/A230 ratios ranged from 0.18 to 1.26
across all 18 samples; high A260/A230 ratios relative to the A260/A280 ratio or ratios higher than
2.0 are considered pure.
Conclusions:
These results suggest that RNA quality is resilient in -80°C up to 18 months and that banked
normal placenta specimens can be used for RNA acquisition. Further testing is necessary to
determine full research applications of RNA from frozen tissue and factors contributing to sample
quality.

Research Day 2019
Jump to Table of Contents 73
Technology, Methods & Resources
Poster #
56
Abstract Title:
Regulatory T Cell Differentiation via Engagement of the PD1/ PDL1 Co-Inhibitory Pathway.
Presenter(s):
Kemi Adeyanju
Authors:
Kemi Adeyanju, Blake Hill and Jeffrey Medin
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
An area of immunotherapy under development is the use of adoptive cell transfer of Foxp3+
regulatory T cells (Tregs) to treat autoimmune diseases such as Type 1 Diabetes, inflammatory
bowel disease and graft-versus-host-disease (GVHD). Preclinical studies in murine models have
shown that adoptive cell transfer of ex vivo generated Tregs can ameliorate autoimmune diseases
and prevent transplant rejection. Currently at least fifty clinical trials have either been completed
or are ongoing to test the efficacy of Tregs. Previously, we showed that conventional T cells
overexpressing programmed death ligand 1 (PDL1) via a lentiviral vector were able to convert T
helper type 1 (Th1) cells into Tregs through binding of PDL1 to its receptor programmed cell death
1 (PD1). Here, we evaluated if a novel scalable manufacturing strategy involving truncated PDL1
protein affixed to beads could induce Treg differentiation.
Methods:
We designed an expression vector comprising the truncated extracellular domain of PDL1 as well
as polyhistidine and biotin tags. In addition to wild-type (WT) PDL1, we used computer modeling
of the crystal structure of PDL1 binding to PD1 to design and produce PDL1 variants that
theoretically have increased binding affinity to PD1. The recombinant WT and variant proteins
(PDL1A, PDL1C and PDL1D) were produced in a mammalian expression system, purified via nickel
affinity chromatography, and biotinylated in an enzymatic reaction. The biotinylated PDL1
proteins were then immobilized onto streptavidin-coated Dynabeads and incubated with primary
human Th1 cells. Two days later the cells were phenotyped by flow cytometry for expression of
the Treg- and Th1-specific transcription factors, Foxp3 and Tbet, respectively. The cells were also
analyzed by Western blot to determine if the PD1/PDL1 pathway was activated.
Results:
Foxp3 expression was induced in the Th1 cells by WT as well as the variant beads. A higher
percentage of Tregs were obtained following incubations with our PDL1 WT and variants beads
than incubation with TGFbeta. Furthermore, incubation with PDL1A, PDL1C, and PDL1D beads led
to more Foxp3+Tbet+ double-positive cells than incubation with the WT beads. Western blot data
showed increased phospho-PTEN (pPTEN) and a concominant decreased expression of phospho-
AKT (pAKT) after incubation of Th1 cells with PDL1 beads compared to Th1 cells cultured alone.
Conclusions:
This data suggests that the truncated PDL1 construct is able to induce Th1 cell differentiation to
Tregs. Increased pPTEN and decreased pAKT expression indicates that the differentiation to Tregs
was prompted by engagement of the PD1/PDL1 signalling pathway. Functionality of the cells
generated using the PDL1-coated beads will subsequently be evaluated in vitro via suppression
assays and in vivo utilizing a mouse model of GVHD to determine the ability of the Tregs
manufactured using our novel protocol to ameliorate pathogenesis of the disease.

Research Day 2019
Jump to Table of Contents 74
Technology, Methods & Resources
Poster #
57
Abstract Title:
Somatic Cell Genome Editing Program: Dissemination and Coordinating Center
Presenter(s):
Angela Lemke
Authors:
Angela Lemke, Aimee Steffenhagen, Jeff De Pons, Anne Temple, Rebecca R. Schilling, Jennifer R.
Smith, Monika Tutaj, Michael N. Grzybowski, Marek Tutaj, Jyothi Thota, Kristin Nord, Matthew J.
Hoffman, Stacy Zacher, Kent Brodie, Ryan Spellecy, Arthur R. Derse, Aron M. Geurts, Mary
Shimoyama, Melinda R. Dwinell
Dept/Division:
Physiology
Category:
Research Support Staff
Introductions:
The NIH Common Fund’s Somatic Cell Genome Editing (SCGE) program goal is to lower the
barriers for new genome editing therapies and to accelerate development of safe and more
effective methods to edit the genomes of disease-relevant somatic cells and tissues in patients.
The SCGE program objectives include testing genome editing reagents and delivery systems in
better animal models, assessing unintended biological effects, improving in vivo delivery of
genome editing machinery, expanding the human genome engineering toolkit, and coordinating
partnerships and disseminating information.
Methods:
The SCGE Consortium initiatives each have distinct goals. The Medical College of Wisconsin was
awarded the Dissemination and Coordinating Center (DCC) in early 2019. The primary goals of the
DCC are to facilitate interactions and communication between consortium initiatives, develop and
disseminate the SCGE Toolkit, and establish a Collaboration Opportunity Fund to accelerate
collaborative and innovative research among members of the SCGE Consortium.
Results:
In the first six months of the award, the DCC has established a communication platform to allow
for individual and group communication, established two subcommittees and three working
groups, launched the new SCGE MCW DCC website (https://scge.mcw.edu/), hosted an in-person
meeting in Washington DC among the SCGE Consortium members and NIH staff, crafted the
Collaboration Opportunity Fund award announcement, is developing the key data elements for
data submission for each initiative, and has outlined the structure of the SCGE Toolkit.
Conclusions:
Through the SCGE DCC at MCW, the research community will be able to explore the discoveries
from the various initiatives, learn about somatic cell genome editing, and access data as the
results are published. The research tools developed will be made available to the research
community to accelerate new therapeutic approaches for both rare and common diseases.
Acknowledgements:
Research reported in this poster was supported by the NIH Common Fund, through the Office of
Strategic Coordination/Office of the NIH Director under Award Number 1U24HG010423-01.

Research Day 2019
Jump to Table of Contents 75
Technology, Methods & Resources
Poster #
58
Abstract Title:
Gene Editing Rat Resource Center (GERRC): Rat models for heart, lung and blood studies
Presenter(s):
Michael N Grzybowski
Authors:
Michael N Grzybowski, Jason Klotz, Rebecca Schilling, Anne Temple, Allison Zappa, Lynn Lazcares,
Jessica Niebuhr, Shawn Kalloway, Jamie Foeckler, Akiko Takizawa, Aron M Geurts, Melinda R
Dwinell
Dept/Division:
Physiology
Category:
Research Support Staff
Introductions:
Transgenesis and gene editing in the rat has produced gene-modified strains which can be used to
validate a gene underlying a quantitative trait locus or human association, or to design follow up
studies to define function and physiological roles of genes or sequence variants. We are currently
in the fifth year of developing rat models for investigators to validate human variation and study
function and mechanism for genes implicated in heart, lung and blood disorders. The Gene Editing
Rat Resource Center (GERRC, http://rgd.mcw.edu/wg/custom_rats/gerrc) is an NHLBI-funded R24
resource program to generate, distribute, and cryopreserve novel rat models to the research
community.
Methods:
Investigator-initiated applications to produce novel genetically modified rat strains were received
from laboratories across the world and reviewed by an external advisory board for scientific merit
and potential broad interest to the heart, lung, blood, and sleep disorder research community.
Custom knockout, knockin, and transgenic rat models continue to be developed.
Results:
To date, we have transferred over 21,000 microinjected embryos, resulting in 4700+ live-born
pups of which 3600+ have been screened for transgenesis or mutagenesis of the target gene. Of
these, we have successfully generated ~630 pups containing transgenes or targeted mutations in
95 genes, distributed among 16 inbred, outbred, consomic and congenic rat strains frequently
used in cardiovascular research. After confirming germline transmission, heterozygous breeders
are distributed to the requesting investigator and then each model is made available to the rat
research community. Sperm is cryopreserved to maintain a permanent source of these models.
Conclusions:
Collectively, the GERRC resource represents the largest collection of genetically modified rat
models which are distributable to any investigator through a standard materials transfer
agreement at the cost of rearing and shipping. We will discuss the general progress of genetic
engineering in rats, current challenges for the field, and opportunities for future developments.
Acknowledgements:
Research reported in this poster was supported by National Heart, Lung, and Blood Institute of
the National Institutes of Health, R24HL114474.

Research Day 2019
Jump to Table of Contents 76
Technology, Methods & Resources
Poster #
59
Abstract Title:
Hybrid Rat Diversity Program (HRDP): A rat resource for systems genetics
Presenter(s):
Rebecca Schilling
Authors:
R. Schilling, A. Takizawa, L. Lazcares, A. Temple, M. Hoffman, S. Tsaih, M. Tutaj, M. Shimoyama, A.
Geurts, M. Dwinell
Dept/Division:
Physiology
Category:
Research Support Staff
Introductions:
Genetic susceptibility to disease, sensitivity to environmental elements, and pharmacogenomics
are critical components of the concepts of precision medicine. Rats are a major model for
studying complex disease mechanisms, behavioral phenotypes, environmental factors, and for
drug development and discovery. Inbred rat strains control for genetic background and allow for
repeated, reproducible molecular, cellular, and whole animal phenotyping. Through the
development of the Hybrid Rat Diversity Program, a powerful panel of inbred rats with genomic,
physiologic, and behavioral phenotype data will serve as a catalyst for research in many fields.
Methods:
The Hybrid Rat Diversity Panel (HRDP) will consist of 96 inbred rat strains to maximize power to
detect specific genetic loci associated with complex traits while maximizing the genetic diversity
among strains. The 96 strain panel consists of 33 genetically diverse inbred strains and two panels
of recombinant inbred panels: FEXL/LEXF (33 strains, Japan) and HXB/BXH (30 strains, Czech
Republic). Embryo resuscitation and breeding are underway at the Medical College of Wisconsin
(MCW). Whole genome sequencing for all 96 strains will be performed by the GSPMC (MCW)
sequencing core to achieve 30X coverage (Illumina NovaSeq S4). Liver and brain transcriptome
analysis will be done for the entire HRDP panel through PhenoGen
(http://phenogen.ucdenver.edu) at the University of Colorado (Tabakoff and Saba). Genomic,
phenotype, and strain information will be made available through the Hybrid Rat Diversity Panel
portal at the Rat Genome Database (http://rgd.mcw.edu). MCW will partner with the Rat
Resource & Research Center (RRRC, http://www.rrrc.us) at the University of Missouri for strain
distribution.
Results:
To date, ten strains have been rederived from cryopreserved embyros and colonies are being
established for phenotyping, tissue biobanking, and whole genome sequencing. With these newly
established strains, we currently have more than 25 strains available of the 96 HRDP strains.
Whole genome sequence has been generated for 32 strains and analysis is underway. Male and
female brain and liver samples have been collected for RNAseq. Tissue biobanking and general
phenotyping is complete for the first 10 strains of the HRDP panel.
Conclusions:
The HRDP will provide a genetically stable population of rat strains with fully sequenced genomes,
transcriptomes for brain and liver, and general phenotypic characterization to be used for systems
genetic studies and fine mapping of complex traits.
Acknowledgements:
Funding: National Institutes of Health, Office of the Director, R24OD024617

Research Day 2019
Jump to Table of Contents 77
Technology, Methods & Resources
Poster #
60
Abstract Title:
Evaluation of procedural time and radiation exposure in celiac plexus block using iGuide
fluoroscopic navigation versus CT guidance
Presenter(s):
Alexandra Fairchild
Authors:
M. Koets, A. Fairchild, R. Heib, E. Hohenwalter, W. Lea, S. Tutton, S. White
Dept/Division:
Radiology: VIR
Category:
Junior Faculty
Introductions:
The development of fluoroscopic navigational software has allowed for increased percutaneous
procedural efficiency compared to traditional CT guided procedures. In this study, we evaluate
radiation exposure, procedure time, and procedural efficiacy in patients who underwent a celiac
plexus block performed with iGuide assistance or CT guidance.
Methods:
Patients who underwent a celiac plexus block either with iGuide assistance or CT guidance from
2012 -2018 were included in this retrospective IRB approved study. Radiation exposure in mGy
and procedure time in minutes were both compared between iGuide and CT guided procedures
using a two-sample t-test. Procedural efficacy was also compared.
Results:
86 patients (46M/40F; mean age 57 years) who underwent an image guided celiac plexus block
were initially evaluated. 11 patients were excluded due to utilization of ultrasound needle
guidance during the procedure. 44 patients (15M/29F; mean age 59 years) underwent iGuide
assisted celiac plexus blocks and 31 patients (16M/15F; mean age 55 years) underwent CT guided
celiac plexus blocks. Radiation exposure in iGuide-assisted celiac plexus blocks was significantly
lower compared to CT guided celiac plexus blocks (702±284 vs. 1100±906 mGy, p=0.01).
Procedural time for iGuide-assisted celiac plexus blocks was lower when compared to CT guided
celiac plexus blocks; however, not statistically significant (66±19 vs. 76±30 minutes, p=0.09). No
difference in procedural efficacy was noted.
Conclusions:
iGuide navigation provides an improvement over conventional CT guidance as demonstrated by a
significant decrease in radiation exposure and overall decrease in procedural time.

Research Day 2019
Jump to Table of Contents 78
Technology, Methods & Resources
Poster #
61
Abstract Title:
A prospective study evaluating a novel class of software for Quantifying successful tissue
perfusion during lower extremity endovascular stent placement
Presenter(s):
Eric Hohenwalter, MD
Authors:
B Bodell, S Schafer, M Back, E Hohenwalter, P Patel, S White, P Rossi, R Hieb
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
2D DSA during LE endovascular revascularization provides immediate, but subjective information
on the success of treatment. However, no quantifiable data to predict treatment outcomes is
obtained. The purpose of this study is to evaluate a prototype post-processing method for pre-
and post-treatment parenchymal tissue enhancement characteristics on 2D DSA by suppressing
vasculature and evaluating the underlying contrast time curve information.
Methods:
This IRB approved study evaluated 18 patients undergoing LE revascularization. The software
algorithm used a band pass filter to suppress vascular structures and a gain multiplier to enhance
the underlying end-tissue enhancement in each image. The contrast time curves for each pixel in
a 2D DSA series were evaluated for: Time to peak (TTP), time to half peak (THP), time of arrival
(TOA), and area under the curve (AUC). Resulting parametric images displayed the values in a
color wash, compressing the underlying functional information of the complete 2D DSA run into a
single color image. The parametric images were evaluated by a group of board certified IRs.
Patients were followed up at 30, 90, and 180-day intervals to assess clinical outcomes.
Results:
Of the 18 enrolled patients, 5 were excluded due to failed revascularization. Therefore, 13 patient
images were included. THP demonstrated usefulness as a measure for the contrast flow
differential between different angiosomes, with larger differences indicating the degree of
sluggish flow in the affected angiosome compared to neighboring unaffected angiosomes. TOA
was useful for assessing areas of occlusion or stenosis proximally. AUC proved useful as a measure
of total contrast passing through the ROI. AUC differentials in neighboring angiosomes were a
predictor for pre-treatment disease severity while changes between pre and post intervention in
the same angiosome characterized improvement.
Conclusions:
2D DSA images have an underlying wealth of information derivable from the contrast-time density
curves. While difficult to gleam from visual review alone, parametric color coding of underlying
functions may be helpful to better understand treatment efficacy.

Research Day 2019
Jump to Table of Contents 79
Technology, Methods & Resources
Poster #
62
Abstract Title:
Does implementation of an effective midline catheter program for vascular access in a large
academic hospital decrease rates of bloodstream infections?
Presenter(s):
Sarah White, MD
Authors:
T. Park, J. Eklund, J. Riesenberg, S. White
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
Recently, the use of peripherally inserted central catheters (PICCs) has increased dramatically and
has been shown to contribute significantly to major complications such as central line associated
blood stream infections (CLABSIs). Increasing midline use can reduce the rate of CLABSIs;
however, this could potentially increase minor complications such as leaking and dislodgement.
Therefore, this study aims to evaluate the ease of use and safety of midline catheters by surveying
end users of vascular access devices (VAD) and comparing the rates of complications between
PICCs and midlines.
Methods:
Thiswas an IRB-approved study. Participants froma pool of nurse representatives from each unit
throughout the hospital (n¼24) ere asked to identify complication trends and maintenance issues
associated with VAD use. In addition, a single-center retrospective chart review was performed
using a REDCap QA/AI database of all patients with midlines (n¼510) and PICCs (n¼510) inserted
from March 2017-July 2018. The EMR was reviewed for the following complications: catheter-
related bloodstream infection (CR-BSI) or CLABSI, phlebitis, infiltration, leaking, dislodgement, and
thrombosis
Results:
Nurses reported that the most commonly seen complication was dislodgement, while thrombosis
was seen the least. In addition, blood draw, labeling, and flushing were the most frequent issues
with midline use. In the retrospective study, CLABSI/CR-BSI rate was significantly higher in PICCs
than in midlines (c2¼9.43, p¼0.002). Furthermore, there was no significant difference in the
incidence of thrombosis and the minor complications of phlebitis, infiltration, and dislodgement;
however, midlines were found to have a significantly higher rate of leaking (c2¼8.12, p¼0.004).
Conclusions:
PICCs were found to have a significantly higher rate of major complications versus midlines, which
were associated with a higher incidence of minor complications. The hospital wide VAD policy
change to reduce PICC usage and increase midlines was warranted to reduce CLABSIs.

Research Day 2019
Jump to Table of Contents 80
Technology, Methods & Resources
Poster #
63
Abstract Title:
Advanced Guidance and Access Techniques for Challenging Osteoid Osteoma Ablations
Presenter(s):
Sean Tutton, MD
Authors:
D Shnayderman, A Tadros, S White, E Weil, S Dybul, S Tutton
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
To review advanced image guidance and techniques for the safe and effective
ablation of osteoid osteomas (OO) in atypical locations.
Methods:
OO are benign, invariably painful, osteoblastic tumors. They are most frequently seen in the
femur and tibia, which account for 50-60% of lesions. Radiofrequency ablation (RFA) is a well-
established minimally-invasive treatment for these lesions. OO adjacent to joints and in small
bones present unique technical challenges, including fractures, chondromalacia, tendon
disruption, neurovascular injury, and skin burns. Advanced imaging guidance and access
techniques have allowed treatment of OO in challenging locations affording greater accuracy and
mitigating potential complications.
Results:
The use of advanced guidance and access techniques, including real-time multiplanar reformats,
navigation software, and orthopedic access tools were reviewed in small bone and juxta-articular
OO in those undergoing RFA at our institution. Data presented will include lesion size, post
procedure pain relief and complications. Atypical lesions were found in 8 patients (4 male); mean
age, 24 years, (range 13- 42). Lesion locations included lunate, medial humeral epicondyle, 3rd
proximal phalanx of the foot, 1st metatarsal, 3rd metatarsal, proximal fibula with close proximity
to deep fibular nerve, iliac bone with extension into the SI joint, and T12 pedicle with extension
into the costovertebral junction. Mean lesion size was 8.9 mm (range 5-13). CT guidance with
multi-planar reformatting, orthopedic power drill, and, in several cases, needle guidance
software were used. Adjunctive techniques included neurologic monitoring with EMG and
Somatosensory Evoked Potentials and ankle nerve block. The minimum clinical follow-up was 5
days (mean, 19 weeks; range, 1- 52). All patients reported resolution of pre-procedure pain.
During follow-up, none of the patients had any major complication.
Conclusions:
The use of real-time multi-planar CT guidance, navigation software and orthopedic tools allowed
for safe ablation of OO in challenging locations with resolution of pain related disability at short
follow-up.

Research Day 2019
Jump to Table of Contents 81
Neuroscience
Poster #
64
Abstract Title:
Ectopic activity from injured dorsal root ganglion neurons triggers hyperalgesia and allodynia in
rats with spinal nerve ligation
Presenter(s):
Bin Pan
Authors:
Bin Pan, Dongman Chao, Guoliang Yu, Quinn Hogan
Dept/Division:
Anesthesiology: Research
Category:
Junior Faculty
Introductions:
Peripheral nerve injury may cause hyperalgesia, allodynia and ongoing pain by increasing the
ectopic activity of primary afferent neurons. The question on whether injured afferents or their
uninjured neighbors is the main source that contributes to pain behavior after nerve injury is still
debatable. With the help of our newly developed dorsal root ganglion (DRG) field stimulation
(GFS) technique, which can be used to precisely block ectopic activity of DRG neurons while have
no effects on surrounding neural tissues, we tested which afferent (injured or uninjured) that
contributes to the pain after spinal nerve ligation (SNL), which provides distinct injured afferent
(lumbar 5th spinal nerve, L5) and uninjured neighbors (lumbar 4th spinal nerve, L4).
Methods:
In vivo single unit recording from fibers teased from the 4th and 5th lumbar dorsal root is
employed 2 weeks after SNL, in which L5 spinal nerve is ligated.
Results:
First, dorsal root fibers from L5 showed higher spontaneous activity (60% of fibers) than L4 (20%)
after SNL. GFS can block those spontaneous activity. Second, L5-, not L4-, GFS blocked
hyperalgesia and allodynia, and ongoing pain (with conditioned-place preference). Third, we
employed in vivo single unit dorsal horn (DH) recording to record activity of wide dynamic range
(WDR) neurons. After SNL, L5-, not L4-, GFS inhibited spontaneous activities of WDR neurons,
elevated threshold to induce action potential firing of DH neurons during punctate mechanical
stimulus (1.1mm tip, 26g) and noxious punctate mechanical stimulus threshold mechanical
stimulation (100µm tip, 16g).
Conclusions:
These results suggest that injured nerve, not uninjured neighbors, triggers hyperalgesia, allodynia
and ongoing pain by increasing spontaneous firing of DRG neurons, which facilitate firing of dorsal
horn projection neurons.
Acknowledgements:
NIH Grant R01NS103812

Research Day 2019
Jump to Table of Contents 82
Neuroscience
Poster #
65
Abstract Title:
Repetitive Mild Traumatic Brain Injury Induces Long-Term Cognitive Impairment in Rats
Presenter(s):
Elizabeth Roth
Authors:
Elizabeth Roth, Keguo Li, Quinn Hogan, Wai-Meng Kwok, Amadou Camara, Bin Pan
Dept/Division:
Anesthesiology: Research
Category:
Research Support Staff
Introductions:
Traumatic brain injury (TBI) affects at least 10 million people worldwide and 3 million people in
North America. Mild TBI (mTBI), including concussions, accounts for 70-90% of all TBI cases. A
significant number of mTBI patients experience enduring symptoms, including headaches, mild
cognitive dysfunction, emotional lability, psychiatric symptoms, and an increased risk of
neurodegenerative disease. Repetitive closed head impact model of engineered rotational
acceleration (rCHIMERA) is a recently developed nonsurgical animal model of TBI that primarily
produces diffuse axonal injury characterized by white matter inflammation and axonal damage,
which mimic the mTBI in in human beings and make rCHIMERA an ideal model of mTBI. However,
the majority of works on rCHIMERA are in mice, which are not suitable for modeling the complex
behavioral effects in human subjects. This study was designed to validate the rCHIMERA-induced
rat mTBI model using advanced behavioral tests.
Methods:
Animals (n=55) received 6 closed-head impacts over 2 days (3 impacts on each day, with 30-
seconds between impacts), all at either 2 or 3 Joules (J) of energy during dexmedetomidine (IV,
0.2mg/kg/hr). Control animals has anesthesia only. To identify behaviors changed by mTBI, testing
included behavioral spectrometry, which captures detailed representations of spontaneous
behaviors in an open field, automated home-cage behavior analysis, rotarod test, and fear
conditioning.
Results:
In 10 rats with 3J impact, 2 animals died of intracranial hemorrhage and 1 rat died as a result of
nasal hemorrhage, which indicates severe TBI. In 45 rats with 2J impact, no rats died from the
injury. Behavioral spectrometry did not identify any changes in open field behavior. However,
home-cage monitoring showed injured rats had reduced sleeping, eating, drinking, stretching,
grooming, and walking distance at 1 week and 1 month after mTBI compared to baseline (n=5).
These measures were not different from shams at 3 months after mTBI (n=7 shams and 7 mTBI).
Injury did not affect motor activity and motor learning with rotarod test, but did impair
associative fear learning and memory in fear conditioning tests 4 weeks and 3 months after mTBI
(n=9 shams and 9 mTBI).
Conclusions:
These results suggest that mTBI in rats with 2J of energy induces short-term changes in affect and
activity, and long-term cognitive impairments, validating this as a model that replicates clinical
mTBI.
Acknowledgements:
Supported by the Advancing a Healthier Wisconsin

Research Day 2019
Jump to Table of Contents 83
Neuroscience
Poster #
66
Abstract Title:
Feasibility and Optimization of Perfusion MRI in the Rat Cervical Spinal Cord
Presenter(s):
Briana Meyer
Authors:
Briana Meyer and Matthew Budde, PhD
Dept/Division:
Biophysics
Category:
Student
Introductions:
Current clinical management guidelines for traumatic spinal cord injury emphasize the
importance of restoring blood flow to the cord [1]. Perfusion magnetic resonance imaging (MRI)
of the brain is well-established and shown success in informing the clinical treatment of stroke [2],
yet, few studies have applied these methods to the spinal cord. Non-invasive imaging to monitor
spinal cord perfusion and hemodynamic parameters have the potential to inform the clinical care
of spinal cord injury. The purpose of this study was to evaluate the feasibility of two perfusion
MRI techniques, dynamic susceptibility contrast (DSC) and pseudo-continuous arterial spin
labeling (pCASL), and optimize their performance in the rodent spinal cord.
Methods:
MRI was performed at 9.4 tesla in healthy female Sprague-Dawley rats at the cervical level. DSC-
MRI consisted of an golden-angle radial acquisition before, during and after a bolus injection of
gadolinium-based contrast agent. Images were reconstructed using under-sampling to provide
high temporal resolution (0.5 s) and perfusion parameters were derived from the signal intensity
by time curve. PCASL MRI employed a labeling plane perpendicular to the spinal cord to tag blood
with magnetic inversion. Label duration was 0.8 s. The normalized signal difference between tag
and control images obtained 3.6 mm rostral from the labeling plane were used to estimate spinal
cord blood flow (SCBF).
Results:
Following contrast injection, a concentration-time curve was characterized in the spinal cord
tissue. Estimated mean transit time (MTT) and time to peak (TTP) was 7.6 s and 2.6 s, respectively.
PCASL labeling efficiency of 0.87 was calculated in the carotid arteries. Signal change between
pCASL control and label conditions was apparent in the spinal cord gray matter and SCBF was
estimated at 372.6 +/- 98.6 mL/100g/min (n=3).
Conclusions:
This work demonstrates that non-invasive measurements of perfusion of the rodent spinal cord is
feasible at high field using two complementary techniques: DSC and pCASL. SCBF estimates varied
between animals and further optimization of pCASL parameters is necessary before applications
to spinal cord trauma or other spinal cord injuries. The development of perfusion MRI for the
spinal cord will be useful to interrogate the role of perfusion in spinal cord trauma, aid in the
development of potential therapies, and potentially guiding appropriate medical care for SCI
patients in a clinical setting, thereby meeting several unmet experimental and clinical needs.
Reference 1:
Martin, A.R., et al (2015). Current Trauma Reports, 1(3), 169-181.
Reference 2:
Albers, G.W., et al. (2018). New England Journal of Medicine, 378(8), 708-718.
Acknowledgements:
We thank Natasha Wilkins, Matt Runquist for experimental assistance. This study was supported
by funding from the National Institutes of Neurological Disorders and Stroke (R01NS109090).

Research Day 2019
Jump to Table of Contents 84
Neuroscience
Poster #
67
Abstract Title:
MRI predictors of neurological function in a rat model of cervical spinal cord contusion injury
Presenter(s):
Seung-Yi Lee
Authors:
SeungYi Lee, Natasha Wilkins, Shekar N. Kurpad PhD, Brian D. Schmit PhD, Matt D. Budde PhD
Dept/Division:
Biophysics
Category:
Student
Introductions:
Intramedullary hemorrhage following traumatic spinal cord injury (SCI) is consistently identified as
an MRI feature associated with poorer neurological outcomes. However, it is unknown whether
hemorrhage has a causal role in increasing the degree of spinal cord damage or whether it is
merely a consequence of more severe injuries. Moreover, an unmet clinical need for SCI patient
management is a biomarker to identify those patients with recovery potential. As a first step to
evaluate imaging biomarker-guided therapeutic strategies, the study aims to investigate the
relationship between metrics derived from MRI and neurological outcomes in a rat model of
cervical contusion injury.
Methods:
Twenty Sprague-Dawley rats were used. Mild hemi-contusion spinal cord injury was produced at
C5 following hemi-laminectomy, using the New York University impactor. A 10g weight was
dropped from 25 mm onto the exposed cord. The rats underwent MRI at 1- and 30-days post
injury (dpi), using anatomic and diffusion weighted imaging. The volume of hemorrhage and
edema were quantified as T2-weighted hypo- and hyper-intensities, respectively, and axonal
injury was quantified as decreased diffusion parallel to the white matter spinal cord using a cord-
optimized filtered diffusion technique. Metrics were quantified with manual region of interest
analysis. Neurological function was assessed for locomotion by forelimb locomotor assessment
scale (FLAS).
Results:
Edema was the most prominent and consistent feature observed acutely (3.02 mm2 ±1.29). An
axonal injury occupied a smaller portion of the cord (1.44 mm2 ± 1.04). Hemorrhage after SCI had
the smallest volume (0.56 mm2 ± 0.53), but the largest inter-animal variability. At the site of
injury, edema and axonal injury area were strongly correlated to one another (R2=0.77,
p=0.0003), while hemorrhage was only weakly correlated with edema (R2=0.22, p=0.055) or
axonal injury (R2=0.24, p=0.028). Forelimb locomotor function was impaired acutely with high
variability assessed by ipsilateral FLAS score (41 ± 16; out of 64) at 2 dpi, but recovery plateaued
by 14 dpi and continued to near-normative levels (59 ± 3.6) through 4 weeks post injury. The
strongest MRI predictors of acute FLAS score at the same point in time were axonal injury area
(R2=0.59, p=0.0003), with edema having a lower correlation with FLAS (R2=0.55; p=0.0002).
Interestingly, the degree of hemorrhage was not strongly correlated with acute FLAS (R2=0.32,
p=0.0099).
Conclusions:
Axonal injury area and edema measured with MRI were stronger correlates of acute impairment
of forelimb locomotor function compared to hemorrhage. However, in this mild injury model, a
ceiling effect of recovery along with limited variability in dysfunction precluded assessment of
prognostication in SCI, which is a highly sought goal to capture the heterogeneity in human SCI.
Future studies will examine a range of injury severities in combination with therapies to foster the
development of personalized care in SCI.

Research Day 2019
Jump to Table of Contents 85
Neuroscience
Poster #
68
Abstract Title:
Acute effects of sport-related concussion on neuroactive kynurenine pathway metabolites and
their association with post-concussion mood symptoms
Presenter(s):
Morgan E. Nitta
Authors:
Timothy B. Meier, Morgan E. Nitta, Kent T. Teague, James B. Hoelzle, Lindsay D. Nelson, Michael
A. McCrea, Jonathan Savitz
Dept/Division:
Neurosurgery
Category:
Student
Introductions:
There is great interest in identifying objective biomarkers to assist in the diagnosis and prognosis of
sport-related concussion (SRC). Previous work has demonstrated that an imbalance in neuroactive
kynurenine pathway (KP) metabolites measured in serum is associated with mood dysregulation in a
variety of psychiatric diseases and potentially SRC. Here, we tested the hypothesis that neurotoxic KP
metabolites (3-hydroxykynurenine [3HK] and quinolinic acid [quinA]) are elevated relative to
neuroprotective metabolites (kynurenine acid [kynA]) following SRC and are associated with post-injury
mood symptoms.
Methods:
Blood was collected at preseason and at 6 hours, 24-48 hours, and 8, 15, and 45 days post-concussion
in high school and collegiate football players (N=63, age=18.00±1.56 years). Matched, non-injured
football players were recruited as controls and completed similar visits (N=60, age=18.22±1.71 years).
Mood symptoms were assessed using the Brief Symptom Inventory 18 (BSI-18) somatization,
depression, and anxiety subscales at each visit except at 6 hours post-injury. KP metabolites were
quantified in serum by high-performance liquid chromatography with tandem mass spectrometry,
blind to diagnosis, and subsequently natural-log transformed. Linear mixed effects models were used
to assess changes in biomarker levels and BSI-18 scores across time with the effect of group and the
interaction of group by visit, with participant modeled as a random effect. Generalized linear models
(GLM) were used to determine the relationship between KP metabolites and BSI-18 subscales in
concussed athletes, covarying preseason biomarker levels and BSI-18 scores.
Results:
SRC athletes had elevated anxiety, depression, and somatization symptoms at 24-48 hours post-injury
relative to other post-injury visits and relative to controls (ps<0.05), while somatization and depression
symptoms were still elevated relative to controls at 8 days post-concussion (ps<0.05). There was a
significant group by visit interaction for the ratio of kynA to 3HK, F(5,523)=2.48, p=0.03. Follow-up tests
showed that kynA/3HK was significantly higher in SRC at 6 hours relative to preseason and 8, 15 and 45
days post-injury as well as relative to contact controls (ps<0.05). In addition, kynA/3HK levels in SRC at
45 days post-concussion were significantly lower relative to all other visit (ps<0.05). Higher kynA/3HK
at 6 hours post-concussion predicted lower depression scores at 24-48 hours (p<0.05). This relationship
was driven by a positive association between 3HK at 6 hours post-concussion and depression scores at
24-48 hours (p<0.05).
Conclusions:
Results suggest that SRC results in an acute increase in the neuroprotective kynA to 3HK ratio that may
attenuate the severity of post-concussion depressive symptoms.
Reference 1:
Nitta, M. E., Savitz, J., Nelson, L. D., Teague, T. K., Hoelzle, J. B., McCrea, M. A., & Meier, T. B. (2019).
Acute elevation of serum inflammatory markers predicts symptom recovery after
concussion. Neurology, 10-1212.
Reference 2:
Savitz, J. (2019). The kynurenine pathway: a finger in every pie. Molecular psychiatry, 1.
Reference 3:
Singh, R., Savitz, J., Teague, T. K., Polanski, D. W., Mayer, A. R., Bellgowan, P. S., & Meier, T. B. (2016).
Mood symptoms correlate with kynurenine pathway metabolites following sports-related concussion. J
Neurol Neurosurg Psychiatry, 87(6), 670-675.
Acknowledgements:
This work supported by Defense Health Program under the Department of Defense Broad Agency
Announcement for Extramural Medical Research through (Award No. W81XWH-14-1-0561) and the
National Institute of Neurological Disorders And Stroke (R21NS099789; R01NS102225).

Research Day 2019
Jump to Table of Contents 86
Neuroscience
Poster #
69
Abstract Title:
Diffusion tensor imaging and quantitative susceptibility mapping in concussed adolescents with
and without persistent symptoms
Presenter(s):
Luisa Bohorquez-Montoya
Authors:
Luisa Bohorquez-Montoya, Lezlie Espaͱa1, Juan Liu2, Kevin Koch3, Timothy Meier1
Dept/Division:
Neurosurgery, Biomedical Engineering and Radiology
Category:
Postdoctoral Fellow
Introductions:
It is estimated that approximately 30% of pediatric concussion patients develop persistent post-
concussion symptoms (PPCS), though the exact etiology of PPCS has not been determined. We
explored the effects of concussion and PPCS in adolescents on deep gray and white matter brain
structures using diffusion tensor imaging (DTI) and quantitative susceptibility mapping (QSM).
Methods:
Concussed adolescents with (PPCS; n=28, 10 male, age = 16.09 ± 0.98) and without PPCS
(Recovered; n=15, 8 male, age = 15.93 ± 0.96) were recruited from a concussion clinic and
completed visits at least one-month post-injury. Matched adolescents without prior concussion
were recruited as healthy controls (HC; n=15, 6 male, age =16.25 ± 1.16). DTI and QSM were
collected on a 3T GE scanner. Fractional anisotropy (FA), mean diffusivity (MD) and magnetic
susceptibility were calculated in each participant using regions-of-interest (ROIs) derived from the
Harvard-Oxford and JHU-ICBM atlases, with a priori analyses focused on caudate, putamen,
pallidum, thalamus, corpus callosum, and internal capsule. Analysis of variance was used to
determine group differences in FA, MD, and susceptibility.
Results:
There were significant group differences in MD in bilateral putamen and right caudate (ps<0.05).
Follow-up tests found that MD in left and right putamen was significantly elevated in PPCS
relative to HC (ps<0.05), whereas MD in the right caudate was lower in PPCS relative to HC
(ps<0.05). No differences between groups were found in FA (ps>0.05). Groups also differed in
magnetic susceptibility in the genu and body of the corpus callosum (ps<0.05), where PPCS had
greater susceptibility relative to HC (ps<0.05). Ongoing analyses are investigating the relationships
between diffusion metrics and magnetic susceptibility in the identified ROI
Conclusions:
These pilot results suggest that DTI and QSM identify pathophysiology associated with PPCS in
adolescent patients with concussion.

Research Day 2019
Jump to Table of Contents 87
Neuroscience
Poster #
70
Abstract Title:
Loss of IL-12p40 mediates a beneficial effect on recovery after spinal cord injury.
Presenter(s):
Jose Rosas
Authors:
Jose Rosas, Nicolas Pelisch, Brandy Aperi, Kyle Stehlik, Karin Swartz, Antje Kroner
Dept/Division:
Neurosurgery, Microbiology and Immunology
Category:
Student
Introductions:
Traumatic spinal cord injury (SCI) is a relatively frequent event that imposes a massive burden on
the health, quality of life and socioeconomic situation of affected persons and their caregivers.
Both localization and extent of tissue damage in the injured cord influence the functional
outcome. Tissue damage after SCI occurs in two phases: While primary damage describes tissue
loss caused by the initial trauma, the lesion is expanded by secondary damage processes,
including inflammation, hemorrhage, edema and production of reactive oxygen species.
A more complete understanding of individual contributors to inflammatory damage is necessary
to specifically target and modify detrimental factors. Inflammation after SCI is exacerbated, with
activated microglia and monocyte-derived macrophages being the main immune cell populations
in the injured tissue.
Of particular interest are the pro-inflammatory cytokines IL-12 and IL-23, which share a subunit
(p40) that is strongly upregulated after phagocytosis of red blood cells. IL-12 and IL-23 are
expressed by a variety of cell types and have critical functions in regulating both the adaptive and
innate immune system by inducing the production of pro-inflammatory cytokines
Methods:
We used western blot for protein detection as well as immunofluorescence and Turnbull Blue
staining to assess spinal cord tissue integrity after injury. The Basso Mouse Scale (BMS) was used
to monitor locomotor recovery after injury.
Results:
First, we quantified protein expression using Western blot. IL-12p40 is significantly upregulated
24h after injury and stays upregulated throughout the observation period (28 days). The receptor
subunit IL12RΒ2 is also significantly upregulated, while IL-12RΒ1or IL-23p19, the second subunit of
IL-23, are not significantly changed.
We also utilized IL-12p40 and IL-23p19 global knockout mice and wildtype C57BL/6 controls to
quantify locomotor recovery after SCI using the Basso Mouse Scale (BMS). We observed improved
recovery in IL-12p40 deficient mice compared to wildtype mice. IL-12p40 KO mice also
demonstrate significantly more spared tissue and less iron accumulation at 28 days after SCI. In
contrast, IL-23p19 KO mice did not differ from wildtype mice regarding their locomotor scores.
In addition, we sought to identify the effect of locally applied rIL-12 on locomotor recovery and
inflammation after SCI. Our preliminary data suggest that local application of rIL-12 does not
change locomotor recovery compared to vehicle treated controls.
Conclusions:
In summary, these results suggest that the absence of IL-12p40, but not IL-23p19, mediates a
neuroprotective effect after contusion SCI, serving as a new potential therapeutic target to
ameliorate secondary damage and promote better functional recovery outcomes.
Acknowledgements:
Advancing a Healthier Wisconsin Endowment, Milwaukee Veteran's Affair Medical Center

Research Day 2019
Jump to Table of Contents 88
Neuroscience
Poster #
71
Abstract Title:
Role of Microglial CB2 Receptors in the Hyperlocomotor Effects of Cocaine
Presenter(s):
Christina Behlke
Authors:
Christina A. Behlke, Samantha L. Pollock, Jennifer L. Sterrett, Jacob W. Adelman, Alison Moe and
Cecilia J. Hillard
Dept/Division:
Pharmacology & Toxicology
Category:
Student
Introductions:
Drug addiction significantly impacts worldwide disease burden. Some drugs, like the
psychostimulant cocaine, lack effective treatments. Cocaine rapidly and robustly increases
dopamine in the brain’s reward center, causing an intense high, contributing to cocaine’s
addictiveness. Because of its ability to modulate dopamine transmission, the endocannabinoid
system is increasingly gaining interest as a possibility for pharmacological intervention in the
treatment of addiction. Two cannabinoid receptors (CB1R and CB2R) have been identified; CB1R is
abundantly expressed in the brain, and CB1R agonists, such as the cannabinoid THC, can produce
dependence. CB2R is present in peripheral immune cells and at low levels within the brain, where
cell-specific expression remains controversial. Our lab and others have shown that CB2R agonists
reduce cocaine-induced hyperlocomotion, indicating CB2R contributes certain behavioral effects.
Previous studies identified microglial cells as the primary source of CB2R in the brain. Our goal
was to test the hypothesis that CB2R agonist-induced suppression of cocaine hyperlocomotion
required microglial CB2R.
Methods:
We established a transgenic mouse line (CB2tg/tg) containing a floxed CB2R (Cnr2) gene with an
eGFP reporter. Global CB2-/- mice were created by crossing floxed mice with mice ubiquitously
expressing cre-recombinase. To examine the role of microglial CB2R in drug-related behaviors, we
crossed mice expressing cre under the control of the microglial- and macrophage-selective gene
for CX3CR1 with CB2tg/tg mice (CX3CR1-CB2-/-). To characterize the transgenic models, single-cell
suspensions were prepared from spleens of WT and all mouse lines mentioned. Fluorescence of
eGFP-expressing lymphocyte populations was quantified using flow cytometry. Locomotor activity
was measured using the open-field test. CB2R-dependent effects were determined using the
CB2R agonist JWH-133. All mice were given a dose of saline or cocaine (20mg/kg, intraperitoneal)
30-minutes after an injection of vehicle or JWH-133 (20mg/kg, intraperitoneal). Ambulation was
recorded for 45-minutes. Data was interpreted using AnyMaze software and analyzed using a 2-
way ANOVA.
Results:
Flow cytometric analysis from CB2tg/tg revealed the highest eGFP expression in B-cells and lowest
in NK-cell populations, consistent with known CB2R expression in these cell types. In WT and
global CB2-/-, eGFP was low in all measured lymphocyte populations. Microglia from CX3CR1-CB2-
/- displayed low levels of eGFP fluorescence. During the open-field test, mice expressing only cre,
CB2tg/tg, and WT all responded similarly (n=4-6/group); therefore, control data were all
combined. Data from controls showed significant effects of cocaine, JWH, and the interaction.
Sidak’s multiple comparisons test indicated a significant difference (p<0.0015) in the response to
cocaine between mice treated with vehicle versus JWH. In global CB2-/- and CX3CR1-CB2-/-,
cocaine treatment was the only significant factor affecting locomotor activity.
Conclusions:
These findings demonstrate that microglia participate in cocaine-related behaviors and that
cocaine-induced hyperlocomotion is regulated by microglial CB2R; this suggests CB2R is a
potential therapeutic target for psychostimulant abuse treatment.

Research Day 2019
Jump to Table of Contents 89
Neuroscience
Poster #
72
Abstract Title:
Prediction of Cellularity in Glioblastoma using MRI Radiomic Features
Presenter(s):
Alex Barrington
Authors:
Samuel Bobholz, Allison Lowman, Jennifer Connelly, Sean McGarry, John Bukowy, Andrew
Nencka, Alexander Barrington, Peter LaViolette
Dept/Division:
Radiology
Category:
Student
Introductions:
Recent studies of glioblastoma radiomics have found that specific features and radiomic features
of gadolinium enhanced T1-weighted MRI (T1+C) possess predictive utility regarding prognosis
and phenotype. However, there has been little research investigating a biological candidate for
the pathologically relevant information the radiomic measures are able to capture. Therefore, this
study tested the hypothesis that radiomic features of T1-weighted MR images would be predictive
of histological tissue features in glioblastoma tissue.
Methods:
Two glioblastoma patients recruited for brain donation were included in this study. The whole
brain samples were sliced axially to match T1+C clinical imaging using patient specific 3D-printed
slicing jigs. Tissue specimens were acquired from regions suspicious of tumor, H&E stained, and
registered to MR space. After registration of the histological slices to MR space, manually drawn
regions of interest (ROI) were used to highlight the areas of the tissue with relevant histological
information. The masked ROIs were also split into tiles (8 voxel by 8 voxel with 2 voxel overlap) in
order to compare the relationship between radiomic and histological features at different scales.
Pyradiomics v2.1.0 was used to generate radiomic features for each tile and each ROI, and the
voxelwise average of the extracellular fluid (ECF) and cellularity of the ROIs/tiles were calculated.
Kendalls' tau rank coefficients were used to evaluate the correlation between the histological
statistics and radiomic features using a significance threshold of p < 0.001.
Results:
The tile-based results demonstrated several histological statistics correlating with radiomic
features across feature sets, with stronger correlations in ECF than cellularity. The ROI-based
results mirrored the tile-based results, with the exception of no significant correlations between
ROI-based radiomics and cellularity observed, though several factors trended towards
significance.
Conclusions:
These results suggest that the prognostic utility of MR radiomics may be a result of its ability to
capture histologically relevant features. The absence of cellularity correlations in ROI-based
analysis could be a result of texture heterogeneity of the ROI, as well as a matter of sample size,
as the trending factors had tau coefficients similar to the tile-based results.

Research Day 2019
Jump to Table of Contents 90
Neuroscience
Poster #
73
Abstract Title:
A precise comparison of heterogeneous pathological features of glioblastoma at autopsy to T1
subtraction maps
Presenter(s):
Allison Lowman
Authors:
A Lowman, A Barrington, B Ellingson, S Bobholz, J Connelly, S McGarry, J Bukowy, A Nencka, P
LaViolette
Dept/Division:
Radiology
Category:
Research Support Staff
Introductions:
The heterogeneous nature of glioblastoma often makes it difficult to visualize subtly enhancing
infiltrative glioblastoma. To mitigate this issue, T1-weighted subtraction maps are beginning to be
adopted for determining the extent of tumor location. These maps are created by subtracting
intensity normalized T1 weighted images from T1 post-gadolinium contrast images (T1+C). Tumor
volume derived from T1 subtraction maps has been shown to predict patient prognosis and
response to therapy. This study precisely correlates large format histology acquired at autopsy to
a T1 subtraction map acquired in vivo to quantify pathological features responsible for
enhancement.
Methods:
One patient was recruited for this radiological-pathological (rad-path) study. At autopsy, the
whole brain sample was sliced axially to match the T1+C MRI scan acquired 22 days prior to death.
Large specimens suspected to contain tumor were sectioned at autopsy, embedded on large
format histology slides, H&E stained, then digitized. Each digital slide was then manually
annotated to indicate regions of necrotic treatment effect, hypercellularity with pseudopalisading
necrosis, and hypercellularity without pseudopalisading necrosis. The digital histology was then
aligned and resampled into the MRI space using custom software previously published. A T1
subtraction map was generated by first performing a gaussian normalization of the T1 and T1+C
images, linearly alignment, then performing a subtraction. Tumor regions annotated on the
pathology samples were then compared to the values within the T1 subtraction map.
Results:
A total of 8662 voxels were assessed with tissue from two large samples. Regions of
pseudopalisading necrosis co-localized with heightened enhancement on the T1 subtraction map.
The enhancement differed significantly (p<0.00001) from regions of infiltrative tumor, which
showed enhancement levels much more similar to regions without tumor present. Regions of
necrotic treatment effect enhanced subtly.
Conclusions:
Regions of pseudopalisading necrosis are more evident on T1 subtraction maps than those of
hypercellularity which are nonenhancing. Additional research is necessary to determine how well
this pattern generalizes across patient populations.
Reference 1:
LaViolette PS, Mickevicius NJ, Cochran EJ, et al. Precise ex vivo histological validation of
heightened cellularity and diffusion-restricted necrosis in regions of dark apparent diffusion
coefficient in 7 cases of high-grade glioma. Neuro Oncol. 2014;16(12):1599-1606.
Reference 2:
Nguyen HS, Milbach N, Hurrell SL, et al. Progressing Bevacizumab-Induced Diffusion Restriction Is
Associated with Coagulative Necrosis Surrounded by Viable Tumor and Decreased Overall Survival
in Patients with Recurrent Glioblastoma. AJNR Am J Neuroradiol. 2016.

Research Day 2019
Jump to Table of Contents 91
Neuroscience
Poster #
74
Abstract Title:
Comparison of MRI Radiomics and Histomic Features in Glioblastoma
Presenter(s):
Samuel Bobholz
Authors:
Samuel Bobholz, Allison Lowman, Jennifer Connelly, Sean McGarry, John Bukowy, Andrew
Nencka, Alexander Barrington, Peter LaViolette
Dept/Division:
Radiology
Category:
Student
Introductions:
Radiomic features of MR images have recently been shown to be predictive of prognosis and
phenotypic variation in glioblastoma. However, little is known about the underlying tissue
properties that manifest as macroscopic textures measurable with radiomics. This study compares
MRI derived radiomic features to large tissue samples acquired at autopsy to quantitatively
establish a histological basis.
Methods:
Two patients recruited for brain donation following treatment for glioblastoma were included in
this study. The whole brain samples were sliced in the same orientation as the axial clinical
imaging using patient specific 3D-printed slicing jigs. Large tissue specimens were acquired from
regions suspicious of tumor. H&E stained histology slides images were registered to MR space and
down-sampled to the MRI resolution. Pyradiomics v2.1.0 was used to calculate first order
statistics, gray level co-occurrence matrix features, gray level run length matrix features, gray
level size zone matrix features, neighboring gray tone difference matrix features, and gray level
dependence matrix features for both the down-sampled histology and for the T1+C image.
Features were calculated for tiles of the ROI (8 voxels by 8 voxels with 2 voxel overlap in each
direction) in addition to the whole ROI in order to observe the preservation of radiomic features
at different scales. Kendall's tau rank correlations between the histological and MR radiomic
feature were calculated.
Results:
Tile-based results showed widespread correlations between the histology and MR radiomic
features across all feature sets, with nearly all features demonstrating correlation. ROI-based
results also demonstrated several correlations between histology and MR radiomic features,
though less ubiquitously than with the tile-based results.
Conclusions:
These findings indicate that histological radiomic features of glioblastoma tissue are reflected in
the radiomic features of T1+C MRI, suggesting that the MR radiomic features capture histological
information, potentially relevant to prognostic predictions.

Research Day 2019
Jump to Table of Contents 92
Neuroscience
Poster #
75
Abstract Title:
Longitudinal Reproducibility of MR Perfusion Using the 3D pCASL with Multiple Postlabeling Delay
Presenter(s):
Alexander Cohen
Authors:
Amritpal S. Jagra, Alexander Cohen, Mohit Agarwal, Andrew S. Nencka, Timothy B. Meier, Marc R.
Lebel, Michael A. McCrea, Yang Wang
Dept/Division:
Radiology: Imaging Research Center
Category:
Research Support Staff
Introductions:
While 3D pseudocontinuous Arterial spin labeling (pCASL) is the currently recommended non-
invasive MR perfusion technique, it can be confounded by varying arterial transit times (ATT)
across the brain and with disease. In this study, a Hadamard encoding scheme was used to
acquire multiple post-labeling delays (PLD), which were used to estimate ATT and thus correct
CBF. The goal of this study was to assess longitudinal reproducibility of a Hadamard encoded 3D
pCASL sequence in a set of normal volunteers.
Methods:
Imaging was performed on 52 healthy male young adults at 4 time points (TPs) over 45 days. An
“enhanced” 3D pCASL (eASL) sequence was acquired with seven PLD (1.0-3.7s) using Hadamard
encoding. A long (3.5s) labeling block was divided into 7 sub-boluses with control and label sub-
boluses corresponding to the Hadamard matrix. Images for each delay were extracted using a
linear combination of the eight images. Additional T1-weighted anatomical images were also
acquired for registration. ATT and corrected flow (cCBF) were computed using the one-
compartment model. Uncorrected flow (unCBF) was obtained by averaging the delay images with
PLD > 1.5s. The longitudinal reproducibility was analyzed across four-time intervals: 7, 14, 30, and
45 days. Several reproducibility metrics, including within and between subject coefficient of
variation (wCV and bCV respectively), the repeatability coefficient (RC), and intraclass correlation
coefficient (ICC), were analyzed in gray matter (GM) and 17 different ROIs of functional networks
across GM.
Results:
The GM ATT wCV (3.9%) showed a longitudinal stability for ATT across the four sessions,
compared to both unCBF and cCBF. For each time interval, the wCV was lower for cCBF compared
to unCBF for all ROIs and the whole GM. For most ROIs, the ICC was higher for cCBF compared to
unCBF. In addition, the bCV values were always higher than the wCV for each time interval and
ROI.
A power analysis yielded power curves for every session that followed a near identical trend.
Specifically, for GM for every time interval, a higher sample size was needed for unCBF than cCBF.
Conclusions:
Our results suggest that eASL with multiple PLD using Hadamard encoding is a robust tool for
measuring changes in CBF and ATT over time. This MRI perfusion technique can be acquired in the
same amount of time as standard pCASL scans and can be adopted to monitor hemodynamic
information for patients with disease intervention.

Research Day 2019
Jump to Table of Contents 93
Cardiovascular & Stroke
Poster #
76
Abstract Title:
SPHINGOSINE-1-PHOSPHATE INDUCED VASODILATION OF HUMAN ARTERIOLES: ROLE OF S1P
RECEPTOR 1
Presenter(s):
Boran Katunaric
Authors:
Boran Katunaric, Mary E. Schulz, and Julie K. Freed
Dept/Division:
Anesthesiology: Cardiovascular Center
Category:
Postdoctoral Fellow
Introductions:
Tight regulation of vascular resistance is critical to maintain proper tissue perfusion. Recent data
in animal models have shown that sphingolipids, a ubiquitous class of bioactive lipid messengers,
can influence vasomotor tone via dilation or constriction. The sphingolipid sphingosine-1-
phophate (S1P) is known to bind to five known receptors (S1PR1-5), three of which (S1PR1-3) are
expressed in both endothelial as well as vascular smooth muscle cells. It has been suggested that
S1P-induced vasodilation occurs via endothelial cell S1PR1 activation. The effect of S1P on human
microvascular tone is unknown. We therefore examined the hypothesis that S1P-induced
vasodilation of human arterioles is dependent on S1PR1 activation.
Methods:
Arterioles from healthy human adipose tissue were dissected and prepared for videomicroscopy,
equilibrated and pre-constricted with endothelin-1. Changes in arteriolar luminal diameter were
recorded in response to increasing concentrations of S1P (10-12 M to 10-6) in the presence or
absence of the S1PR1 receptor antagonist W146 (10µM).
Results:
Administration of exogenous S1P induced vasodilation to a maximal dilation of 60.8%±5.0, n = 3.
(mean±SEM) at 10-7. Interestingly, vascular constriction was observed with elevated, but still
physiological levels of S1P (10-6). Vasodilation due to S1P was decreased following inhibition of
S1PR1 compared to S1P alone (8.6%±5.5, n = 2).
Conclusions:
Together these data suggest that S1P can modulate vascular tone through activation of S1PR1.

Research Day 2019
Jump to Table of Contents 94
Cardiovascular & Stroke
Poster #
77
Abstract Title:
Endothelialization of a Novel Flow Diverter Using Magnetic Capture
Presenter(s):
Harsimran S. Kalsi
Authors:
Harsimran S. Kalsi, Akankshya Shradhanjali PhD, Raphael Sacho MD, Brandon J. Tefft PhD
Dept/Division:
Biomedical Engineering
Category:
Student
Introductions:
Development of a healthy endothelium on blood contacting devices has continued to be an active
area of research, especially as the clinical demand for better blood-compatible devices grows
rapidly. Over 6 million Americans have an unruptured brain aneurysm and could benefit from a
flow diverter placement procedure. A healthy endothelium on these devices could dramatically
reduce the risks of post-implantation complications. In this preliminary study, we demonstrate
that high rates of endothelial cell capture onto a flow diverter can be facilitated via targeting of
magnetic nanoparticle-labeled cells to a novel magnetic device.
Methods:
Prior to conducting cell capture experiments, both the non-magnetic flow diverter (Pipeline,
Medtronic) and the magnetic flow diverter (custom made from 2205 stainless steel wire) were
demagnetized. These devices were then subsequently magnetized through exposure to a strong
magnetic field for 5 min, after which time a magnetometer was used to measure the retained
magnetic field strength. Porcine blood outgrowth endothelial cells (BOECs) were cultured and
magnetically labeled with superparamagnetic iron oxide nanoparticles (SPIONs) at a
concentration of 5 μl/ml. SPION labeled BOECs suspended in saline were then stained with
NucBlue and delivered to a device both with and without an external magnetic field. Fluorescence
microscopy was used to assess the relative cell capture of each condition at 40x magnification.
Results:
The non-magnetic flow diverter showed little to no cell capture regardless of whether an external
magnetic field was present or absent. Conversely, the magnetic flow diverter showed significantly
more cell capture compared to the non-magnetic device. Furthermore, cell capture to the
magnetic device may have increased slightly when an external magnetic field was present.
Conclusions:
This preliminary study demonstrates great promise in the use of magnetic nanoparticles and a
magnetic flow diverter for optimizing the blood compatibility of flow diverters through rapid
endothelialization of the device. In the future, a cell retention study (simulating pulsatile flow and
physiological shear stress) may further elucidate whether this approach may be useful in a clinical
setting.

Research Day 2019
Jump to Table of Contents 95
Cardiovascular & Stroke
Poster #
78
Abstract Title:
Dynamic contrast-enhanced near-infrared fluorescence imaging to probe altered vascular changes
in rat models
Presenter(s):
Jaidip Jagtap
Authors:
Jaidip Jagtap, Gayatri Sharma, Abdul K Parchur, Chris Hansen, Carmen Bergom, Brian Fish, Meetha
Medhora, Michael Flister, and Amit Joshi*
Dept/Division:
Biomedical Engineering
Category:
Research Support Staff
Introductions:
Wholebody near-infrared (NIR) fluorescence imaging leverages reduced tissue scattering, low
autofluorescence, and enhanced tissue penetration providing a powerful tool to noninvasively
study the vascular changes response to stimuli such as tumors and radiation injury etc. We
demonstrate the in vivo NIR imaging with a short half-life indocyanine green (ICG). The
applications involved imaging tumor impacted vascular function in consomic xenograft models
(CXM) and measuring the irradiation-induced injury in immunocompetent Wistar rats.
Methods:
NIR fluorescence imaging (Λex/Λem = 785/830 nm) was performed by injecting I.V. bolus of 1mL
ICG (400µM) in tail vein for hemovascular imaging. Sequential imaging was performed for 6
minutes at 50 ms exposure per frame with suitable rejection and bandpass filters. Then, principle
component analysis was applied on imaging data to extract the spatial information which can
segment organs of the body (e.g. lung, liver, tumor etc.). The specific methods for two examples
were: (i)For assessing host dependent tumor vascular changes, NIR imaging was performed in
CXM rats Pre-tumor and 10 days Post-tumor (MDA-MB-231), further tumor perfusion and
permeability was quantified with the aid of a 3-compartment pharmacokinetic model. (ii) To
assess impact of radiation, Wistar rats were partial body irradiatied (PBI) with 13Gy x-rays
(keeping one hind leg shielded) and NIR imaging was then performed 42 days after irradiation.
Results:
(i) In CXM rats, three compartment pharmacokinetic (PK) model was used to quantify the ICG
perfusion and permeability. It exhibits reduced perfusion rate, 0.24 ± 0.03 s-1 in SS.BN3 compared
to 0.31±0.02 s-1 in SS and increased permeability ratein SS.BN3 (and retaining more ICG at
WashOut resulting increased permeability) 0.1±0.01 s-1 as compared to 0.03±0.001 s-1 in SS
genotype rats. The variation in ICG biodistribution dynamics may be due vascular dysfunction in
SS.BN3 compared to well-developed vasculature in SS genotype rats.
(ii) Irradiated rat retained more ICG compared to rapid clearance in healthy rat during the
WashOut phase. Resistance in clearance resulted in increased permeability from radiation
induced injury in lung. Perfused isolated lung study at ex vivo confirms increased permeability
rate in radiated area from lung.
Conclusions:
Fluorescence imaging quantitatively distinguishes WashIn and WashOut rates in rats. These
studies clearly show the potential use of dynamic contrast enhanced NIR-I fluorescence imaging
to identify the differences in tumor microenvironment due to different genotypes, and measure
impact of radiation induced injury.
Reference 1:
Jagtap, Jaidip, et al. Biomedical optics express 9.2 (2018): 543-556.(DOI:10.1364/BOE.9.000543)
Reference 2:
Flister, Michael J., et al. Breast cancer research and treatment 165.1 (2017): 53-64.
(DOI:10.1007/s10549-017-4311-8)
Acknowledgements:
Amit Joshi (Rock River Cancer Research Foundation, Alliance for Healthy Wisconsin, MCW
Research Affairs Committee), Meetha Medhora (NIH/NIAID U01AI107305 & R01AI101898),
Michael Flister (NIH R01 CA193343, MCW Cancer Center)

Research Day 2019
Jump to Table of Contents 96
Cardiovascular & Stroke
Poster #
79
Abstract Title:
A Model to Study the Aortic Valve Response to Endothelial Injury
Presenter(s):
Emily Nordquist
Authors:
Emily Nordquist, Michael McDermott, Aaron Trask, Joy Lincoln
Dept/Division:
Herma Heart Institute
Category:
Student
Introductions:
Heart valves are crucial structures which maintain unidirectional blood flow. However, over 5
million people in the US are affected by heart valve dysfunction, which if left untreated can lead
to heart failure or death. Currently, surgical valve repair and replacement are the only effective
treatments, but these procedures are associated with risks. Therefore, development of non-
surgical therapeutics is critical to improve patient outcomes.
The aortic valve (AoV) predominantly contains two cell types: valve interstitial cells (VICs) and
valve endothelial cells (VECs). The VICs make up the core of the leaflet and secrete the
extracellular matrix (ECM) components required for biomechanical function, while VECs form a
protective single-layer endothelium over the leaflet surface, and molecularly communicate with
underlying VICs to regulate their phenotype. Histological studies of diseased valves have
described VEC dysfunction or denudation as an initiating step that subsequently leads to
compromised AoV function, suggesting that VECs are critical in the onset and progression of valve
disease. Despite the importance of this process, the responses of the valve following VEC
disruption are not known, and therefore development of mechanistic-based therapies to halt the
progression of AoV dysfunction is hindered.
Methods:
We have adapted a surgical murine model of VEC injury (Honda et al., 2014) using a guidewire to
damage VECs on the surface of the aortic valve. To determine the valve response to injury and
how this varies with age, surgeries were performed in young adult (4-month old) and aging (16-
month old) wild type mice. Following injury, histological and functional studies were performed.
Results:
In initial studies, we have shown that by 48 hours post-injury, healthy young adult mice positively
respond to VEC damage with increased cell proliferation and concomitant preservation of the VEC
barrier, which maintains overall AoV structure and function. However in aging mice, increased cell
proliferation is not observed, and injury results in increased permeability, structural deformation,
and AoV dysfunction by 4-week post-injury.
Conclusions:
Our data demonstrates the impact of VEC damage on the AoV and suggests that valve cell
proliferation is important to avoid the detrimental effects of injury seen in aging mice. Moving
forward, we hope to determine the fate of these proliferating cells and to uncover the molecular
basis for this injury-related proliferation.
Acknowledgements:
Kaitlyn Thatcher

Research Day 2019
Jump to Table of Contents 97
Cardiovascular & Stroke
Poster #
80
Abstract Title:
Downregulation of Fis1 in Endothelial Cells Does Not Impact Normal Endothelial Cell
Mitochondrial Bioenergetics, Metabolism, or Mitochondrial Protein Content
Presenter(s):
Mamatha Kakarla
Authors:
Mamatha Kakarla, Jingli Wang, David Trykall, Kathryn Repp, V Krishna Puppala, Sudhi Tyagi,
Benjamin Hofeld, Rong Ying, Amberly Branum, Megan Harwig, John Egner, Blake Hill and Michael
Widlansky
Dept/Division:
Medicine: Cardiovascular
Category:
Research Support Staff
Introductions:
Our prior data suggest that knockdown of Fis1 protein improves vascular endothelial health by
reversing endothelial dysfunction associated with dysglycemic conditions and reducing
endothelial inflammation and permeability of the endothelium. Fis1 is an outer mitochondrial
membrane protein that triggers mitochondrial fission when bound by dynamin-related protein-1.
Fis1 is important to mitochondrial fission process specifically under pathophysiological conditions
making Fis1 an attractive therapeutic target.
Methods:
We measured mitochondrial proteins, and mitochondrial bioenergetics in immortalized human
microvascular endothelial cells (HMEC-1) under normal (5mM), high (30mM), and low (2mM)
glucose levels and wild type HMEC-1 cells (5mM). Mitochondrial proteins expression in Fis1 siRNA
HMEC-1 cell lysates and scrambled control cell lysates were assessed under different glycemic
conditions by high throughput immunodetection WES system. The oxygen consumption rate
(OCR) and extracellular acidification rate (ECAR) in transfected cells under different glycemic
conditions were measured by Seahorse mitochondrial and glycolytic stress tests.
Results:
There were no significant differences in mitochondrial bioenergetics (OCR and ECAR; n=5,
p>0.05), and expression of other mitochondrial proteins (MFF, MFN1, MFN2, Drp1, OPA1, Cyt-c,
TOMM20, MFF, pAMPKa, POLG, P62, NDUFB8, GABARAP) between siFis1 cells and scrambled
controls in any of the glycemic conditions (n=4, p>0.05). There is significant increase in expression
of other mitochondrial proteins (MFF, MFN1, Cyt-c, TOMM20, MFF, pAMPKa, POLG, P62,
NDUFB8, GABARAP) under low glucose conditions (n=4, p<0.05) compared to normal and high
glucose conditions.
Conclusions:
Reducing the expression of Fis1 did not alter other mitochondrial proteins and mitochondrial
bioenergetics that are critical for normal physiological processes. Therapeutic potential of Fis1
knockdown is enhanced by a lack of impact on endothelial cell metabolism and other
mitochondrial protein expression.

Research Day 2019
Jump to Table of Contents 98
Cardiovascular & Stroke
Poster #
81
Abstract Title:
Lactobacillus plantarum 299v Supplementation Results in Anti-Inflammatory Changes in
Mononuclear Cell Gene Expression in Men with Stable Coronary Artery Disease Who Do Not Drink
Alcohol Daily
Presenter(s):
Benjamin C. Hofeld
Authors:
Benjamin C. Hofeld, Venkata K. Puppala, Kwang Woo Ahn, Amberly Branum, Mamatha Kakarla,
Jingli Wang, Michael J. Tanner, Elise Nelton, John Baker, Nita Salzman, Martin Hessner, and
Michael E. Widlansky
Dept/Division:
Medicine: Cardiovascular Disease
Category:
Clinical Fellows & Residents
Introductions:
We have recently shown that L plantarum 299v (Lp299v) probiotic supplementation in men with
stable CAD reduced systemic inflammation and improved vascular endothelial function. Alcohol
depletes anti-inflammatory bacteria and increases gut permeability in the intestines and may
abrogate Lp299v’s effects. We explored the impact of Lp299v supplementation in non-daily
drinkers from our cohort.
Methods:
15 non-daily drinkers with CAD consumed Lp299v (20x10^9 CFU) daily for 6 weeks (75% of pilot
study subjects). Vascular endothelial function was measured by brachial artery flow mediated
dilation (FMD). Inflammatory markers were measured pre and post-supplementation. Stool
microbiota changes were determined by 16S rRNA sequencing. A validated plasma-induced RNA
transcription assay determined RNA transcription of human mononuclear cells (HMCs) exposed to
plasma from subjects pre and post-Lp299v supplementation. Data were analyzed using paired t-
tests with false discovery rate (FDR) adjustment. We used DAVID 6.8 and Ingenuity Pathway
Analysis (IPA) to determine canonical pathways, gene clusters, and upstream regulators in HMCs
impacted by Lp299v.
Results:
Leptin, IL-8, and IL-12 decreased (135 to 111 ng/ml, p=0.002; 13.8 to 10.1 pg/ml, 0.032; 54.6 to
44.0 pg/ml; 0.042). FMD % (3.51% to 4.28%, p=0.033) and peak hyperemic shear increased (74.8
to 82.9, p=0.011). 1,443 genes were differentially expressed (‰¥1.2-fold change) in HMCs
exposed to pre- vs. post-Lp299v plasma. Gene expression favored an anti-inflammatory effect of
Lp299v (P<0.0001). IPA showed down regulation of interferon (IFN) signaling (z-score -2.82, p<
0.001) and tryptophan metabolism (z-score 2.0, p<0.001), and were confirmed by DAVID. IPA
predicted changes in expression of 127 upstream regulators which were directionally anti-
inflammatory. Some are involved IFN signaling and innate immunity. No significant differences in
OTUs were seen in stool microbiota.
Conclusions:
Lp299v supplementation in men with CAD resulted in improved endothelial function and reduced
systemic inflammation associated with reduced IFN signaling and innate immune activity. These
findings suggest an anti-inflammatory-mediated cardiovascular benefit of Lp299v
supplementation.

Research Day 2019
Jump to Table of Contents 99
Cardiovascular & Stroke
Poster #
82
Abstract Title:
Survey of antepartum women to assess barriers to sequential compression device compliance
Presenter(s):
Megan Reinhard
Authors:
Megan Reinhard; Anna Palatnik; Kathryn Flynn
Dept/Division:
Obstetrics: MFM
Category:
Student
Introductions:
Use of a sequential compression device (SCD) has been recommended for antepartum pregnant
women for venous thromboembolism prophylaxis. However, based on our prior study
(PMID=31164020) patient compliance with SCD at our institution is only at 32%. The objective of this
study was to design and pilot test a patient survey to identify barriers to SCD use among pregnant
women during antepartum admissions.
Methods:
We designed an SCD survey geared towards the obstetric population, based on a previously validated
SCD compliance survey in urology (PMID=23578129). To assess the face validity and interpretation of
each question, we conducted 8 face-to-face cognitive interviews with providers (n=3) and patients
(n=5) admitted to the antepartum floor and prescribed SCD. Results from the cognitive interviews
informed revisions to the survey. Patient-reported understanding of SCD purpose, indication for SCD
use, bother, and reasons for non-compliance with SCD were included in the paper survey. We
calculated a total bother score, which was the sum of 12 items, each rated on a 1-5 point scale, on
bothersome aspects of SCD (range of 12-60). Patient demographics and clinical characteristics,
including length of stay, were abstracted from medical records.
Results:
As of August 2019, 10 patients participated. All women reported they understood the purpose of SCD
and that the purpose was blood clot prevention. When asked about the level of importance of the
SCDs, 60% reported SCDs were important to be worn at all times unless they were walking. Only 20% of
patients reported SCDs being available the first day of their admission. Across 12 categories of
bothersome aspects of SCD, the average total bother score was 23.7 (range 12-60). 30% of patients
reported they would prefer pharmacological prophylaxis to SCD. The most common reasons women
identified as why SCDs were not worn at all times were: 1) discomfort and limiting ambulation; 2) too
hot/sweaty; and 3) they wake the patient up. The most common responses to what women believe
would make SCDs easier to use were to have a wireless/cordless device, for the device to have lighter
weight/cooler material, and for there to be better availability of nurses to assist with SCD placement.
Conclusions:
In this pilot study we examined women’s attitudes towards SCD use and identified barriers to SCD
compliance among pregnant women admitted to the antepartum floor during pregnancy. Despite high
reported understanding of the purpose of SCD among pregnant antepartum women, the perceived
importance of SCDs was suboptimal. Self-identified barriers to use centered around discomfort and
restrictive nature of the device. Patients identified fixing these barriers as well as needing more
assistance with the device as important in increasing use. Combatting these barriers may critical
increasing compliance with mechanical prophylaxis.
Reference 1:
Heit J. Venous thromboembolism: disease burden, outcomes and risk factors. Journal of Thrombosis
and Haemostasis. 2005;3(8):1611-1617. doi:10.1111/j.1538-7836.2005.01415.x
Reference 2:
ACOG Practice Bulletin No. 196: Thromboembolism in Pregnancy. Obstetrics & Gynecology.
2018;132:1611-1617. doi:10.1097/aog.0000000000002923
Reference 3:
Chen M, Palatnik A. Sequential Compression Device Compliance During Inpatient Antepartum Manage-
ment [26I]. Obstetrics & Gynecology. 2018;131:104S.doi:10.1097/01.aog.0000533452.00148.65
Acknowledgements:
We would like to thank David F. Ritsema, MD for allowing us to use his SCD survey from his 2013 study
"Sequential compression devices in postoperative urologic patients: an observational trial and survey
study on the influence of patient and hospital factors on compliance" as a template for our study.

Research Day 2019
Jump to Table of Contents 100
Cardiovascular & Stroke
Poster #
83
Abstract Title:
Structure-Function-Molecular Relationships of the Extracellular Matrix of Aortic Valves in Mouse
Models of Human Disease
Presenter(s):
Kaitlyn Thatcher
Authors:
Kaitlyn Thatcher, Jessica Fulton, Michael McDermott, Peggi Angel, Cristopher Breuer, and Joy
Lincoln
Dept/Division:
Pediatrics
Category:
Research Support Staff
Introductions:
The organization of extracellular matrix (ECM) components, such as collagens, proteoglycans, and
elastins, into three distinct layers (the fibrosa, spongiosa, and ventricularis, respectively) is
essential for maintaining proper structure and function of heart valves. Mutations in ECM
components cause connective tissue disorders, such as Marfan Syndrome, Ehlers-Danlos
Syndrome, and osteogenesis imperfecta (OI), and heart valve defects in these patients are
common. However, effective treatment options are limited to surgical valve repair or
replacement. By modeling these connective tissue disorders in mice, we aim to better
understand the molecular mechanisms leading to ECM disorganization and valve dysfunction with
the goal of developing alternative, less invasive treatment approaches.
Methods:
Mice with a frameshift mutation in the pro-alpha2 chain of collagen I (col1a2) serve as a model of
osteogenesis imperfecta murine (OIM) (The Jackson Laboratory). Homozygous OIM (OIM-/-) mice
exhibit fragile bones and skeletal deformities, and in addition we and others report significant
thickening and myxomatous features of the aortic valve (AoV) by 12 months of age, and these
structural changes are associated with functional regurgitation and left ventricle enlargement. Of
note, these phenotypes were not grossly observed at earlier time points examined. To determine
early proteomic changes associated with these late structure-function phenotypes, we performed
MALDI-IM imaging on AoVs of 6-month-old mice.
Results:
Our preliminary findings reveal substantial differences in the peptide composition of OIM-/- mice
compared to wildtype (WT); analysis of mass spectrometry data revealed that OIM-/- mice show
greater intensities on lower mass peaks, which could indicate more efficient enzymatic
degradation of the ECM due to decreased collagen crosslinking.
Conclusions:
These proteomic changes may provide insights into the early mechanisms of pathogenesis that
can be therapeutically targeted to halt progression to end stage disease, thereby avoiding
surgery.
Reference 1:
Cheek JD and Wirrig EE, Alfieri CM, James JF, and Yutzey KE. (2012) Differential activation of
valvulogenic, chondrogenic, and osteogenic pathways in mouse models of myxomatous and
calcific aortic valve disease. J Mol Cell Cardiol 52(3): 689-700
Reference 2:
Tao G, Kotick JD, and Lincoln J. (2012) Heart valve development, maintenance, and disease: the
role of endothelial cells. Curr Top Dev Biol 100, 203-232
Reference 3:
Saban J, and King D. (1996) PCR genotyping of oim mutant mice. Biotechniques 21, 190,192

Research Day 2019
Jump to Table of Contents 101
Cardiovascular & Stroke
Poster #
84
Abstract Title:
The pharmacological XPO1 antagonist KPT-330 prevents aortic valve calcification via a novel
C/EBP □ signaling pathway
Presenter(s):
Punashi Dutta
Authors:
Punashi Dutta, Karthik M. Kodigepalli, Stephanie LaHaye, J. Will Thompson, Sarah Rains, Casey
Nagel, Kaitlyn Thatcher, Robert B. Hinton and Joy Lincoln
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
Calcific aortic valve disease (CAVD) is a common disorder characterized by progressive buildup of
calcium-rich nodules on the valve surface leading to stenosis. This process is mediated by
dysregulation of valve interstitial cells (VIC) that abnormally differentiate towards an osteoblast-
like lineage and promote matrix mineralization, similar to bone. Despite widespread prevalence,
effective pharmaceutical treatments are lacking and surgical intervention remains standard
treatment with no guarantee of long-term success. Therefore, there is a critical need to develop
effective therapeutic alternatives.
Methods:
We isolated porcine aortic valve interstitial cells (pAVICs) from a healthy pig heart and used it for
all in vitro studies. We induced osteogenic conditions via the use of glass as plating tool for cells
or osteogenic media to grow cells in. Small interfering RNA (si RNA) against XPO1 was used to
target XPO1. Mass spectrometry was performed to determine proteins in the nucleus in calcified
and non-calcified conditions, in addition to KPT-treated cells. Calcification was observed via the
use of alizarin red. For in vivo studies, we used the Klotho mice (an aging mouse model that
develops valvular calcification).
Results:
Our published work has suggested that inhibiting nuclear export of XPO1-dependent proteins may
have therapeutic promise. In this study, we obtained such a drug (KPT-330) currently in Phase III
clinical trials for cancer treatment, however its therapeutic potential for CAVD has not been
examined. Using an established mouse model of CAVD (Klotho-/-), we administered KPT-330
during early stages of annular valve calcification in an established mouse model (Klotho-/-) and
show that early KPT-330 treatment of Klotho-/- prevents annular calcification in vivo (n=6).
Similarly, treatment of human and porcine aortic valve interstitial cells (pAVICs) cultured under
osteogenic stimulus at later stages is sufficient to attenuate and mitigate calcific nodule formation
in vitro. Similar to pharmacological inhibition, genetic knockdown of XPO1 in vitro also prevented
calcification. To determine the proteins targeted by KPT-330 treatment, Mass Spectrometry was
performed and suggests that KPT-330 retains C/EBP□ in the nucleus of VICs to inhibit Wnt
signaling which in turn prevents pro-osteogenic signaling and cell proliferation of VICs, theraby
preventing calcification.
Conclusions:
These studies for the first time have identified KPT-330 as a novel therapeutic drug in the
treatment of CAVD by targeting C/EBP□-Wnt signaling.

Research Day 2019
Jump to Table of Contents 102
Cardiovascular & Stroke
Poster #
85
Abstract Title:
Hyperphosphatemia-induced aortic valve calcification in the setting of chronic kidney disease
Presenter(s):
Vinal Menon
Authors:
Vinal Menon and Joy Lincoln
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
Calcific aortic valve disease (CAVD) and vascular calcification (VC) are commonly seen in chronic
kidney disease (CKD) patients. The occurrence of CAVD is around 40% in stage 3 CKD vs. 80-99% in
stage 5 CKD. Due to progressive loss of kidney function, CKD leads to elevated inorganic
phosphate (Pi) serum levels which has been shown to promote VC; mediated by phosphate
transporters PiT-1/2 in smooth muscle cells and ERK-mediated signaling to induce osteogenic
changes. However, the mechanisms of elevated Pi-induced CAVD are still unknown.
Methods:
To explore phosphate-induced CAVD in vivo, we obtained 1 month old KL+/- mice and fed them a
high-Pi (1.8%P) diet for 4 months to induce hyperphosphatemia. In parallel with the mouse
model, we obtained rats with 5/6 nephrectomy (5/6 Nx), that serve as an established model of
CKD by virtue of excision of kidney tissue and these were fed a high-Pi (1.2%P) diet.
Results:
Hyperphosphatemia was confirmed by high serum Pi levels relative to KL+/- mice on the control
diet (14.5 mg/dL vs. 9.35 mg/dL). Calcification of the aortic annulus and cusp was detected in
KL+/- mice on the high-Pi diet compared to KL+/- mice on the control diet. In Klotho (KL)+/- mice,
we show that PiT-1/2 were localized in valve endothelial cells, and treatment of porcine aortic
valve interstitial (VICs) with 5mM Pi increased PiT-1/2 expression and led to ERK-dependent
formation of calcific nodules. Treated rats exhibited significant weight loss relative to sham
groups and VC, without CAVD, was observed in all (3/3 per group) sham rats on high-Pi diet and
5/6 Nx rats on control and high-Pi diets
Conclusions:
Future studies, using these systems, are focused on delineating the mechanisms underlying CAVD
in CKD patients, particularly those on dialysis and, therefore, at high risk of undergoing valve
replacement surgery

Research Day 2019
Jump to Table of Contents 103
Cardiovascular & Stroke
Poster #
86
Abstract Title:
The Role of α-Smooth Muscle Actin in Mitral Valve Prolapse
Presenter(s):
Bailey Dye
Authors:
Bailey Dye, Karthik Kodigepalli, Michael McDermott, and Joy Lincoln
Dept/Division:
Pediatrics
Category:
Student
Introductions:
Mitral valve prolapse (MVP) affects 2-3% of the general population, with surgical valve repair or
replacement as the only effective treatment. MVP is characterized by myxomatous degeneration
of the extracellular matrix (ECM), including an overabundance of proteoglycans, such as Versican.
This is associated with abnormal expression of α-smooth muscle actin (SMA) by valve interstitial
cells (VICs), suggesting an activated phenotype. Affected leaflets progressively thicken and
biomechanically weaken, causing them to prolapse back into the atria. If left untreated, MVP can
progress to heart failure. The goal of this study is to determine the contribution of abnormal SMA-
positive cells to myxomatous degeneration, and the progression of MVP.
Methods:
Fbn1C1039G mice serve as a model of Marfan Syndrome, a connective tissue disorder often
accompanied by MVP. To address our goal, we employed immunohistochemical analysis and
immunofluorescent imaging to determine the temporal changes of the mitral valve ECM, and
SMA expression, in the Fbn1C1039G mice compared to wild type. These studies were
complemented by SMA knockdown and overexpression in vitro studies in porcine mitral valve
interstitial cells (pmVICs).
Results:
We show that in the Fbn1C1039G mice, myxomatous changes are evident by 10 weeks of age, and
mitral valves are significantly thickened with hemodynamic flow disturbances by one year.
Interestingly, abnormal SMA expression in activated VICs is observed as early as postnatal day 1
(PND1) prior to ECM changes, and quantity increases with pathogenesis. In vitro studies in pmVICs
show that SMA expression is mediated by MRTF signaling, and MRTF expression is also increased
in mitral valves from Fbn1C1039G/+ mice. Furthermore, pharmacological knockdown of SMA in
pmVICs by Latrunculin A reduced Versican, while SMA overexpression had opposing effects.
Conclusions:
Our data suggests that ectopic SMA expression in activated VICs precedes myxomatous
degeneration during early stages of disease, and is potentially causative of ECM remodeling. In
addition, we show that active MRTF signaling may underlie VIC activation in MVP. Ongoing and
future work will determine the contribution of this abnormal cell population to the progression of
MVP, and insights will be used to develop mechanistic-based therapies to halt disease
pathogenesis.

Research Day 2019
Jump to Table of Contents 104
Cardiovascular & Stroke
Poster #
87
Abstract Title:
Susceptibility of Mice Lacking Renin-b to Chronic Angiotensin II Infusion
Presenter(s):
Pablo Nakagawa
Authors:
Pablo Nakagawa, Anand Nair, Shao Yang Zhang, Ko-Ting Lu, Javier Gomez, Justin Grobe, and Curt
D. Sigmund
Dept/Division:
Physiology
Category:
Postdoctoral Fellow
Introductions:
Previous experience to various hypertensive conditions enhances the response to subsequent
hypertensive challenges and the activation of the brain renin angiotensin system (RAS) is required
for the sensitization to these hypertensive challenges. We previously showed that the brain-
specific renin alternative isoform (Ren-b) tonically inhibits the activation of the brain RAS and that
ablation of Ren-b (Ren-b KO) results in brain RAS disinhibition leading to elevated blood pressure
(BP). Retrospective analysis of five cohorts of mice indicated that Ren-b KO model exhibits a high
degree of variability in BP, which may be attributed to the susceptibility to stress. Therefore, we
hypothesized that Ren-b KO are sensitized to a hypertensive challenge such as angiotensin (Ang)
II.
Methods:
Wildtype (WT) or Ren-b KO were infused with either vehicle or Ang II (400 ng/kg/min; sc.) via
osmotic minipumps for 4 weeks.
Results:
Ang II significantly increased BP in both WT and Ren-b KO to the same degree (WT+veh: 103 vs
WT+Ang: 120 mmHg; p = 0.01 (n=10-12) and KO+veh: 104±3 vs KO+Ang: 118±5 mmHg; p = 0.03
(n=10-14)). Although the BP between Ren-b KO and WT mice was elevated equally, Ang II induced
an exaggerated suppression of plasma renin in Ren-b KO compared to WT (WT+Ang: 14.8 vs
KO+Ang: 7.2 ng/ml; p = 0. 03; n=7-9). Ren-b KO exhibited enhanced Ang II-induced dipsogenic
response (WT+Ang: 3.7 vs KO+Ang: 4.6 ml/day; p = 0. 05; n=10-12) and exhibited elevated heart
weight (WT+Ang: 4.8 vs KO±Ang: 5.2 mg/g of body weight; p = 0.03; n=10-12) concomitant with
an increased cardiac collagen type I alpha-2 mRNA expression (p = 0.03; n=7-9).
Conclusions:
Our data indicates that in the presence of Ang II, Ren-b KO exhibits higher susceptibility to
cardiovascular disease. After successive breeding and backcrossing Ren-b KO developed a milder
and more variable baseline BP elevation compared to our initial cohorts. This suggests that
epigenetic silencing or other physiological and molecular mechanisms might compensate for
some of the cardiovascular alterations driven by the genetic deletion of renin-b. Studies of a
conditional Ren-b KO model will be used to elucidate the physiological and/or pathophysiological
consequences of an acute downregulation of renin-b in adulthood.

Research Day 2019
Jump to Table of Contents 105
Cardiovascular & Stroke
Poster #
88
Abstract Title:
Magnetic Resonance Imaging for Non-Invasive Assessment of Cardiac Function in Small Animals
Presenter(s):
Micaela Young, El-Sayed H. Ibrahim
Authors:
Micaela Young, Victor Magana, Carmen Bergom, El-Sayed H. Ibrahim
Dept/Division:
Radiology
Category:
Student
Introductions:
Cardiac magnetic resonance (CMR) imaging allows for comprehensive evaluation of the heart
function by providing clinically useful parameters. Unfortunately, commercially available CMR
analysis software packages don’t provide specialized processing capabilities that may be needed
in advanced applications. In this work, we developed a simple CMR image analysis package in
Matlab for analyzing global cardiac function with features not available in commercial packages,
and used an open-source cardiac function analysis software for evaluating regional cardiac
function, and tested the techniques on CMR images of rats exposed to thoracic radiation therapy
(RT) and compared the results to control rats.
Methods:
Matlab was used to build an interactive graphical user interface that allows analyzing cine images
and measuring global cardiac function parameters, e.g. ejection fraction (EF), end-diastolic
volume (EDV), and mass, as well as provide the capability of generating masks for the heart, blood
pool, and myocardium. The developed software was used to generate masks in over 2,000 cine
and tagged images. The software was also used to measure global function parameters in 8 rats (4
RT and 4 controls) and the results were compared to those obtained using commercial analysis
software. Further, two operators used the InTag software to measure myocardial strain and tissue
motion in the same animals. Statistical analysis was used to compare global and regional cardiac
function measurements as well as results from RT and control rats.
Results:
The developed software was used to create over 2,000 myocardial masks which will be used as a
training dataset for an AI-based automatic heart segmentation algorithm in the next phase of the
study. Global function measurements were normal in all studied rats (RT vs controls): EF
(83.2±5.5% vs 67.7±4%), EDV (0.25±0.04 ml vs 0.34±0.03ml), and mass (0.56±0.12g vs
0.46±0.04g). Regional function measurements showed deteriorated function in the RT rats with
measurements significantly (P<.05) lower (than controls) in circumferential strain (septal (-
10.5±1.7% vs -15.0±2.8%), mid-ventricular (-10.6±3.8% vs -14.1±3.5%), apical (-7.5±3.5% vs -
11.9±2.3%), and overall (-9.8±2.2% vs -13.0±2.7%)) and tissue motion (anterior (4.7±0.8mm vs
2.7±0.1mm) and mid-ventricular (7.9±1.8mm vs 5.4±2.2mm)). However, the differences in radial
and longitudinal strains were not significantly difference (P>.05). Finally, Bland Altman plots
showed good inter-observer and inter-software agreements.
Conclusions:
The in-house developed software allows for analyzing global cardiac function with measurements
in agreement with commercially available packages. Further, the developed software allows for
more specialized analysis, for example generating masks of different cardiac structures. Global
function parameters, e.g. EF, were insensitive for differentiating RT from control rats; however,
regional function parameters, e.g. strain, were capable of identifying abnormal heart contractility
in the RT rats, which makes it a valuable tool for early detection of cardiac dysfunction. More rats
are being imaged to allow for comprehensive statistical analysis.
Reference 1:
Filster et al, Breast Cancer Research Treat, 165:53-64
Reference 2:
Ibrahim, Heart Mechanics MRI. CRC Press, 2017
Reference 3:
Said et al, Ann Onc, 25:276-282

Research Day 2019
Jump to Table of Contents 106
Cardiovascular & Stroke
Poster #
89
Abstract Title:
TransCarotid Artery Revascularization (TCAR): A Single-Center One Year Experience
Presenter(s):
Parag Patel, MD
Authors:
Tadi Ciszak, MD, Robert A. Hieb, MD, FSIR, Peter J. Rossi, MD, Michael Malinowski, MD, Parag J.
Patel, MD, MS, FSIR
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
TransCarotid Artery Revascularization (TCAR) utilizing the ENROUTE neuroprotection system (NPS)
is a novel approach towards carotid artery stenting (CAS). This minimally invasive approach
utilizes intra-procedure high-rate flow reversal NPS and is designed for CAS in patients who are
deemed too “high-risk” for carotid artery endarterectomy (CEA). The system has shown superior
stroke and death outcomes when compared to prior registry results from both CEA and trans-
femoral CAS. The purpose of this study is to review of both short and long-term outcomes in
patients who underwent TCAR.
Methods:
We performed an IRB approved single-center retrospective review of patients who underwent
TCAR procedures between 8/2017 and 9/2018. All interventions were performed in patients
deemed at high risk for complications from CEA, symptomatic patients with ‰¥50% stenosis, or
asymptomatic patients with ‰¥70% stenosis. A hybrid OR was utilized for all procedures and co-
staffed with a vascular surgeon (VS) and an IR. Patients were followed in clinic at 1, 6, and 12
months post procedure. Demographic data and complications were reviewed.
Results:
29 TCARs were performed on 28 patients, age range 59-85 (M:F, 19:9). Technical success rate was
(100%), with no acute device, technical, or access site complications. All lesions were successfully
crossed and 30 stents were deployed (1 lesion required two overlapping stents). One patient
underwent bilateral TCAR on separate occasions, and another patient underwent concurrent
TCAR and TVAR. One adverse outcome was reported within 30-days (ipsilateral intraparenchymal
hemorrhage), with an overall adverse-free event rate of 97%. No myocardial infarction (MI) or
death occurred. All patients remained neurologically symptom-free at their follow up, and
average time to follow up was 151 days.
Conclusions:
TCAR is a safe and novel approach to CAS utilizing cerebral flow-reversal as a means of providing
neuroprotection. This procedure requires a high technical skillset and is best performed utilizing a
multidisciplinary team with VS and IR.

Research Day 2019
Jump to Table of Contents 107
Cardiovascular & Stroke
Poster #
90
Abstract Title:
Hospital Length of Stay Predicts Mortality and Readmission Rates in Advanced Heart Failure
Presenter(s):
Johnny Shepherd
Authors:
Johnny Shepherd, Dr. David Joyce, Dr. Asim Mohammed, Dr. Sakthi Sundararajan
Dept/Division:
Surgery: Cardiothoracic
Category:
Student
Introductions:
Mechanical circulatory support can improve the outcomes of patients with advanced heart
failure. Nevertheless, the complexities surrounding patient selection often serve as a barrier to
the identification of suitable candidates. We sought to establish a simplified model for selecting
patients for advanced therapies.
Methods:
The medical records of 455 patients who were seen in Heart Failure Clinic between February 2017
and December 2018 were screened for heart failure admissions during the study interval. Those
who underwent hospital admission were stratified by length of stay (LOS). A primary endpoint of
six month mortality and a secondary endpoint of readmission within six months, were compared
between those with a short LOS (defined as < or = 72 hours) and a long LOS (>72 hours).
Results:
165 (36%) of the patients who were seen in heart failure clinic were admitted for heart failure
symptoms during the study interval. The primary endpoint was met in 31 (28%) patients in the
long LOS group, compared to 4 (7.5%) patients in the short LOS group (p< 0.01) and 16 (5.5%)
patients who were never admitted to the hospital (p< 0.00001). Of the 168 patients who were
admitted during the study interval, the secondary endpoint was met in 46 (41%) patients in the
long LOS group, compared to 14 (23%) in the short LOS group (p=.02). 7 patients were admitted
for >72 hours without subsequent readmission within 6 months, however, they were readmitted
within 6 months following an admission < or = 72 hours.
Conclusions:
Heart failure admissions of greater than 72 hours are associated with worsening outcomes with
respect to mortality and subsequent readmission. These data suggest that hospital LOS should be
considered as an important variable in identifying patients for advanced therapies.

Research Day 2019
Jump to Table of Contents 108
Cardiovascular & Stroke
Poster #
91
Abstract Title:
Detection of Seasonal Trends in National Donor Heart Availability Using the UNOS Dataset
Presenter(s):
Mohammed Kamalia
Authors:
Mohammed A. Kamalia, Adhit Ramamurthi, Nathan J. Smith, Lisa Rein, Asim Mohammed, Lyle D.
Joyce, & David L. Joyce
Dept/Division:
Surgery: Cardiothoracic Surgery
Category:
Student
Introductions:
Despite the widespread belief that organ availability surges around certain holidays and times
during the year, to date there is no empirical data to support or refute this theory. This question is
highly relevant for heart transplant candidates that have undergone LVAD implantation to
potentially guide the utilization of a patient’s 30 days of Status 3 time. We sought to identify any
probable timing issues which may be advantageous in the listing strategies for these patients.
Methods:
Annual, monthly, and daily heart donation rates were calculated from October 1987 through
March 2017 on the national level and separately for each UNOS region; monthly rates were
normalized to a 30-day period to account for differences in days of the month. Rates include all
hearts recovered for donation (<2% were not transplanted). Monthly heart donation rates were
modeled using Poisson regression including month (categorical) and a spline term for year. Daily
heart donation rates were modeled using cosinor and Poisson regression, assuming a 12-month
seasonal period; the amplitude and date of the seasonal peak were reported for each model. The
holiday effect was assessed using conditional logistic regression to compare holidays (any day
within 3-days of a holiday) and non-holidays in 30-day blocks; stratifying the data into 30-day
windows controls for seasonal effects and trends across years.
Results:
Annual heart donation rates increased in a non-linear pattern over the study period, even after
adjusting for population growth. Seasonal plots suggest a modest increase in monthly donations
in the summer months. A significant seasonal pattern was detected in the national data (Fig. 1)
and all regions except for region 1 using the cosinor analysis. The regions with the highest
amplitude were region 7 (peak: July 20th, amplitude: 13.7%) and region 6 (peak: July 4th,
amplitude: 11.1%); the amplitude is expressed as the percent change from the region-specific
midline rate to account for differences in regional populations. There was no significant difference
in the odds of heart donation when comparing holidays vs. non-holidays using the national data
(odds ratio [95% CI]: 1.00 [0.97, 1.03], p = 0.99) or in any of the regional subsets.
Conclusions:
During a 30-year interval, there was no observable correlation between organ availability and
holidays. However, in all UNOS regions except region 1, a significant seasonality effect was
observed with higher donation rates occurring during warmer weather months. These findings
may add another consideration to the strategic decision making around utilization of status 3 time
for LVAD recipients.

Research Day 2019
Jump to Table of Contents 109
Clinical
Poster #
92
Abstract Title:
Perioperative Ketorolac Administration Increases Post-tonsillectomy Bleeding In A Tertiary Pediatric
Hospital; A Quality Review Of 8582 Operations
Presenter(s):
Susan Taylor
Authors:
Susan P. Taylor, MD, MPH, Richard J. Berens, MD, George M. Hoffman
Dept/Division:
Anesthesiology: Pediatric Anesthesiology
Category:
Senior Faculty
Introductions:
Meta-analyses1,2 of perioperative nonsteroidal anti-inflammatory agents support their use for post-
tonsillectomy pain without an increased risk of bleeding. These studies and concerns for the risks
related to perioperative opioids have contributed to increased administration of ketorolac for
tonsillectomy. Because of an apparent increase in the rate of reoperation for bleeding, we
undertook a review of tonsillectomy outcomes to explore the association of ketorolac use and other
factors with post-tonsillectomy bleeding.
Methods:
Data for tonsillectomy surgery performed between 2013 and 2018 at Children’s Hospital of
Wisconsin and its Surgicenter were extracted from our electronic data warehouse for quality and
practice improvement with IRB approval. Criteria for inclusion were patients < 21 years undergoing
tonsillectomy  minor ENT procedures. Cases were excluded if the original surgical procedure was
performed elsewhere, or if the case included concurrent extensive ENT or non-ENT procedures.
Repeated tonsillectomies or reoperations for bleeding in the same patient were treated as a single
case. Demographic and process variables included age, gender, ASA-physical status, perioperative
ketorolac administration, care process track (surgicenter, day surgery, short stay, scheduled
admission), duration of surgery and anesthesia. The primary outcome was occurrence of bleeding
requiring reoperation. Association of ketorolac with postoperative bleeding was analyzed by
univariate and multivariate logistic regression, and time to bleeding, by log rank tests of equality of
survivor functions, using Stata 15.2 (StataCorp, College Station, TX).
Results:
8582 surgical procedures were included in the analysis. Demographic data and process times are
reported in Table 1. Overall, 217 (2.54%) patients returned to OR for control of tonsillar bleeding.
The proportion of patients receiving ketorolac, and the incidence of bleeding, both increased from
2013-2018 (P,0.01, test for trend). Ketorolac use was associate with in increase bleeding risk (OR
1.67, CI 1.27-2.19, p<0.001) in univariate analysis. In multivariable analysis, bleeding was associated
with perioperative ketorolac (OR 1.7) and inpatient status (OR 3.4). Approximately 25% of bleeds
occurred by 24 hours, 33% by 48 hours, and 50% by 120 hours, with no difference between groups.
Conclusions:
We report an association between perioperative administration of ketorolac and post-tonsillectomy
bleeding in a review of 8582 surgical procedures. This result contrasts with two metaanalyses in the
ENT literature that found no association between perioperatiave ketorolac and other NSAIDs and
subsequent bleeding. In multivariable analysis of our data, bleeding was associated with
perioperative ketorolac (OR 1.7) and inpatient status (OR 3.4). Both ketorolac use and bleeding
increased over time from 2013 -2018. Further research is necessary to develop effective pain control
strategies and minimize risks for the pediatric patient undergoing tonsillectomy.Further research on
nonsteroidal drug administration in the perioperative period could focus on multiple outcomes to
minimize risks associated with both opioid and non-opioid analgesics
Reference 1:
Riggin L, Ramakrishna J, Sommer DD, Koren G. A 2013 updated systematic review $ meta-analysis of
36 randomized controlled trials; no apparent effects of non steroidal anti-inflammatory agens on the
risk of bleeding after tonsillectomy. Clinical Otolaryngology 2013;38:115-29.
Reference 2:
Chan DK, Parikh SR, Perioperative ketorolac increases post-tonsillectomy hemorrhage in adults but
not children. The Laryngoscope 2014, 124:1789-93.

Research Day 2019
Jump to Table of Contents 110
Clinical
Poster #
93
Abstract Title:
Agilent V4 and V7 exome capture kits: A systematic comparison of kit performance and
implications of clinical use for CNV
Presenter(s):
Mike Andresen
Authors:
Stefano Rosati B.S. 1, Mike Andresen B.S. 1, Wendy M Demos M.S. 1, Jenica Abrudan1Ph.D. 1, Lida
Zeighami M.S. 1, Michael Zimmermann Ph.D. 1,2,3
Dept/Division:
GSPMC: Bioinformatics Research and Development Laboratory
Category:
Research Support Staff
Introductions:
Whole Exome Sequencing (WES) remains the front-line workhorse for detection of germline
inherited disease due to relative affordability, assay throughput and reasonable diagnostic rate
ranging from 13.75-57.5%
1
(case type, clinical specialty dependent). Copy number variation (CNV)
is extremely relevant in monogenic disorders, CNVs account for 4.7-35% of pathogenic variants
(case type, clinical specialty dependent)
2
. Currently, many clinical WES assays do not support
calling CNV by NGS, forcing clinicians to order and integrate results from WES and
microarray/CNV testing. One hurdle of CNV calling by NGS is the variation coverage of site target
coverage from commercially available kits. In the present study, we compare Agilent’s SureSelect
Human All Exon V4 (V4 capture) and SureSelect Human All Exon V7 (V7 capture) capture kits to
assess the viability V7 capture for calling CNVs by WES
3
.
Methods:
20 DNA libraries from 15 patients were prepped via V7 WES capture kit were sequenced on
Illumina HiSeq/NovaSeq and were compared to 15 V4 kit sequencing experiments from the same
patients performed on HiSeq. Sequencing results were run through the GSPMC bioinformatics
pipeline. Comparisons of coverage were performed using Picard tools, Samtools, and inhouse
coverage assessment tool SeqSounding. V4 and V7 sample cohort results were aggregated and
comparisons were made for depth of coverage, number of covered genes/transcripts and
coverage variability.
Results:
A comparison of the average read depth per gene showed that V7 had a lower average depth
than V4 (depth 138x, 191x resp.). V7 showed an increase in the number of genes with >84x
coverage. The number of genes below 10x was 552 for v4, and 623 for v7. A comparison of the
standard deviation of gene coverage for samples run on V4 and V7 showed a decreased standard
deviation for V7 capture at 39σ compared to the V4 capture genes at 63σ. Agilent’s V7 capture kit
also showed a decrease in the number of samples with a standard deviation >75x reads per gene
(The number of genes with a standard deviation greater than 75 was 646 for V7 and 4908 for V4).
Conclusions:
Agilent’s V7 Exome Capture kit showed a greatly reduced number of genes with >10x coverage as
well as an increase in the number of genes covered >84x (V7 = 18,656, V4= 17,917). V7 also
showed an increase in the total number of genes with coverage (V7 = 19880, V4 = 18837). V7 also
showed a decreased standard deviation of coverage per gene (V7 = 39σ, V4 = 63σ). The decrease
in number of genes with st. dev. In conjunction, these data show that the V7 exome Capture kit
covers more genes and is more consistent in the number reads per gene, showing that V7 has
greater clinical efficacy in both exome sequencing and CNV calling from the exome.
Reference 1:
Stark, Zornitza, Tiong Y. Tan, Belinda Chong, Gemma R. Brett, Patrick Yap, Maie Walsh, Alison Yeung et al. "A
prospective evaluation of whole-exome sequencing as a first-tier molecular test in infants with suspected
monogenic disorders." Genetics in Medicine 18, no. 11 (2016): 1090.
Reference 2:
Truty, Rebecca, Joshua Paul, Michael Kennemer, Stephen E. Lincoln, Eric Olivares, Robert L. Nussbaum, and
Swaroop Aradhya. "Prevalence and properties of intragenic copy-number variation in Mendelian disease
genes." Genetics in Medicine 21, no. 1 (2019): 114.
Reference 3:
Agilent Technologies, Inc. “SureSelect Human All Exon V7: Data Sheet”
https://www.agilent.com/cs/library/datasheets/public/5991-
9040EN%20SureSelect%20V7%20Datasheet.pdf.

Research Day 2019
Jump to Table of Contents 111
Clinical
Poster #
94
Abstract Title:
Duration of labor induction in nulliparous women with preeclampsia and maternal and neonatal
outcomes
Presenter(s):
Zachary Colvin
Authors:
Zachary Colvin DO, Mingen Feng MS, Amy Pan PhD, Anna Palatnik MD
Dept/Division:
Obstetrics & Gynecology: Maternal Fetal Medicine, Pediatrics
Category:
Clinical Fellows & Residents
Introductions:
Preeclampsia is one of the leading medical causes for induction of labor (IOL). However, it remains
unknown how long is it safe to continue IOL in women with preeclampsia and whether prolonged
IOL in these women is associated with increased risk of adverse obstetric outcomes. The objective
of this study was to quantify the association between IOL duration in nulliparous women with
preeclampsia and maternal and perinatal morbidity.
Methods:
This was a secondary analysis of a multicenter cohort study of 228,438 deliveries in 19 U.S.
hospitals. In this analysis we included nulliparous women ‰¥18yo with singleton gestation
diagnosed with preeclampsia and undergoing IOL for the indication of preeclampsia. Women
delivered by cesarean or with missing data of time from induction to full dilation were excluded.
Duration of IOL, defined as time from admission to delivery, was examined by 4-hr intervals from
<12h to >24h in relation to composite maternal and neonatal outcomes. The trends in
proportions of outcomes that occurred at different intervals were examined by Cochran-Armitage
trend test. Relative risks were done with <12hrs as the reference category and potential
confounders adjusted by log-binomial or Poisson regression.
Results:
A total of 2,079 women met criteria for this analysis. The median labor duration was 17.3h
(interquartile range 11.8-24.9), with 545 (26.2%) lasting <12h and 568 (27.3%) >24h. The
frequency of chorioamnionitis, composite neonatal outcome, NICU admission, 5-minute Apgar
score ‰¤ 7, neonatal respiratory distress and infection was greater with increasing labor
duration. After multivariable adjustment, duration of IOL was associated with increased risks of
maternal composite outcome after 20hrs and increased risks of neonatal composite outcome
after 24hrs.
Conclusions:
Duration of IOL for preeclampsia was associated with increased risk for maternal and neonatal
morbidity after 20h and 24h, respectively. This information should factor into decision making on
how long to continue inductions in women with preeclampsia.

Research Day 2019
Jump to Table of Contents 112
Clinical
Poster #
95
Abstract Title:
Maternal Outcomes of Pregnancies Complicated by Fetal Life Limiting or Lethal Conditions
Presenter(s):
Talia Coney
Authors:
Talia S Coney , Anna Palatnik
Dept/Division:
Obstetrics and Gynecology
Category:
Clinical Fellows & Residents
Introductions:
There is evidence that women carrying fetuses with certain life-limiting or lethal conditions have
increased morbidity. We aimed to compare maternal outcomes between pregnancies with a fetal
diagnosis of life-limiting of lethal conditions to women without such diagnoses in a contemporary
U.S. cohort.
Methods:
This was a retrospective cohort of women undergoing mid-trimester ultrasound for a fetal
anatomic survey and delivering at Froedtert and the Medical College of Wisconsin between 2005
and 2018. The primary composite outcome of hypertensive disorder of pregnancy, gestational
diabetes, cesarean delivery, third or fourth degree laceration, postpartum hemorrhage, blood
transfusion, postpartum endometritis, wound infection, hysterectomy, maternal ICU admission,
and maternal death were compared between women with and without diagnosis of fetal life-
limiting or lethal condition in 1:3 ratio, using univariable and multivariable analyses. Secondary
outcomes examined were the length of the first and the second stage of labor.
Results:
During the study period, a total of 106 women with a fetal diagnosis of life-limiting or lethal
condition were eligible for analysis. They were compared to 318 women with normal fetal
anatomic surveys. In univariable analysis, the primary composite outcome was not statistically
different between the two groups (30.2% versus 21.7%, p=0.076). The rates of cesarean delivery
and blood transfusion were higher among women with a diagnosis of fetal life-limiting or lethal
condition compared to controls (26.4% versus 15.4%, p=0.011 for cesarean delivery, and 1.9%
versus 0%, p=0.013 for blood transfusion). The secondary outcome, length of the first stage of
labor was longer among women with a diagnosis of fetal life-limiting or lethal diagnosis,
compared to controls (12h versus 6.7h, p<0.001). There was no difference in the length of the
second stage of labor. In multivariable analysis, controlling for maternal race, BMI, smoking,
induction of labor, bishop score ‰¤4 on admission, gestational age at delivery and birth weight,
the first stage of labor continued to be longer by 6.2h among women with a diagnosis of fetal life-
limiting or lethal condition, compared to controls.
Conclusions:
Women diagnosed with fetal life-limiting or lethal condition, compared to controls, had a
statistically significant longer first stage of labor, higher risk of receiving a blood transfusion, and
lower risk of developing hypertensive disorders of pregnancy. This information should be
incorporated into counseling regarding term complications of these pregnancies.
Acknowledgements:
Rachel Russel, MD candidate; Joe Galante

Research Day 2019
Jump to Table of Contents 113
Clinical
Poster #
96
Abstract Title:
State Law Designed to Decrease Post-operative Opioid Prescriptions: Is it Best for the Patient?
Presenter(s):
Esha Afreen
Authors:
Esha Afreen, BS; Zachary Colvin, DO; Anna Palatnik, MD; Erika Peterson, MD
Dept/Division:
Obstetrics and Gynecology: Maternal Fetal Medicine
Category:
Student
Introductions:
Opioids are an important part of postoperative pain control following cesarean delivery. However,
excess amounts are often prescribed, which can lead to abuse. The state of Wisconsin recently
passed new provisions to the Wisconsin Uniform Controlled Substances, which went into effect
April 1, 2017. These changes were intended to discourage providers from overprescribing opioids
by mandating a search of the prescription drug monitoring program (PDMP) data base if
prescribing opioids for > 3 days duration. The objectives of this study were to see if opioid
prescribing patterns changed after these new provisions were enacted and to see if postoperative
pain control was affected.
Methods:
A retrospective cohort study of women delivering by cesarean section from 4/2016 to 4/2018 at a
large, academic, tertiary hospital in Wisconsin was done. Women were excluded if there was no
postpartum follow-up care in the hospital system, were prescribed opioids other than
oxycodone/hydrocodone, or if additional surgical procedures were performed in the same
hospitalization. Maternal and delivery characteristics were collected. Number and total amount of
opioids prescribed at discharge, additional encounters (phone call/unscheduled visit) for
inadequate pain control, and whether extra opioids prescribed were collected. Patients delivering
the year prior to the new provision were compared those delivering the year following.
Univariable and multivariable analyses were done to examine whether there was a significant
change in prescribing patterns and health care utilization after the state provisions went into
effect.
Results:
A total of 1,316 women met criteria for analysis. There were no statistically significant differences
in characteristics between patients in two study periods. There was a significant decrease in
number (28.1 vs 22.8, p<0.001), and total amount (142.7 vs 116.7 mg, p<0.001) of opioids
prescribed at discharge in the year after the provisions were enacted. A multivariate linear
regression was performed controlling for race, labor, previous cesarean deliveries, prior opioid
use, and body mass index. Both outcomes remained statistically significant. There was no
difference in percentage of patients who had additional encounters for postpartum pain control,
(5.94 vs 4.98%, p=0.443) or additional opioid prescriptions (3.90 vs 3.60%, p=0.769).
Conclusions:
The number and amount of opioids prescribed decreased in the year following state provisions
compared to the year prior. This decrease shows the mandate has been effective at reducing
opioid prescribing while not compromising postoperative pain control after discharge. Future
mandates should be considered in other states to decrease excess opioid prescribing.

Research Day 2019
Jump to Table of Contents 114
Clinical
Poster #
97
Abstract Title:
Still feeling the effects: a citation analysis of the highly cited, retracted article on MMR vaccines
and autism
Presenter(s):
Elizabeth Suelzer, MLIS, AHIP
Authors:
Elizabeth Suelzer, MLIS, AHIP; Jennifer Deal, MA, MLIS (Advocate Aurora); Karen Hanus, MLIS,
AHIP; Barbara Ruggeri, MLIS, AHIP (Carroll University); Rita Sieracki, MLS; Elizabeth Witkowski,
MILS
Dept/Division:
Office of Research: MCW Libraries
Category:
Research Support Staff
Introductions:
In 1998, Andrew Wakefield published an article that allegedly showed a causal relationship
between the measles, mumps and rubella (MMR) vaccination and autism. Although this article
was twice retracted (Murch et al., 2004; The Editors of The, 2010), and questions arose about the
credibility of Wakefield’s data (Deer, 2011) the infamous article continues to be highly cited. This
research project analyzed the cited by references of the 1998 Wakefield article to learn more
about who cited it and how the article was cited.
Methods:
We conducted a cited reference search in Web of Science to identify literature that cited the 1998
Wakefield article. The citations and full text copy for each reference were uploaded into
Covidence where each reference was screened to determine the characteristic of the in-text
citations using an established taxonomy (Bornmann & Daniel, 2008; Leung et al, 2017) and to see
if the retractions of the Wakefield article were referenced. The screening was blinded, and
conflicts were resolved by group consensus.
Results:
A total of 1,153 citations were analyzed. Articles were not included in this study if they were not
published in English or if we were unable to find the Wakefield reference in the article text. The
most common citation characteristics were negational (72%), perfunctory (9%) and affirmational
(8%). The Wakefield article was retracted twice: a partial retraction by 10 of the 12 authors in
2004, and a full retraction in 2010. The partial retraction was referenced in 32% of the articles
published between 2004-2009. Retractions were referenced in 71% of the articles published after
2010. Since 2013, the percentage of authors who referenced the retraction is continually growing.
Conclusions:
Overwhelmingly, scholarly literature negated the findings of the 1998 Wakefield article, even
before the article was retracted. Many citing authors pointed out the methodological flaws of the
study and the small sample size. Highly cited papers are presumed to hold more scholarly weight
than less cited papers, however, this article was cited for all the wrong reasons.
A significant number of articles published after the retraction did not cite the retraction. Although
most citation styles have recommendations on how to cite retractions, not all authors follow the
recommendations. There is a need for greater vigilance in ensuring that retracted articles are
referenced properly.
Reference 1:
Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis,
and pervasive developmental disorder in children. [retracted in: The Lancet.
2010;375(9713):445.]. Lancet. 1998;351(9103):637-641
Reference 2:
The Editors of The Lancet. Retraction—Ileal-lymphoid-nodular hyperplasia, non-specific colitis,
and pervasive developmental disorder in children. [retraction of: Wakefield AJ, Murch SH,
Anthony A, et al. In: The Lancet 1998;351(9103):637-641]. The Lancet. 2010;375(9713):445.
Reference 3:
Murch SH, Anthony A, Casson DH, et al. Retraction of an interpretation. The Lancet.
2004;363(9411):750. Deer B. How the case against the MMR vaccine was fixed. 2011;342:c5347.
Acknowledgements:
This project was made possible in part by the Institute of Museum and Library Services
(RE-95-17-0025-17).

Research Day 2019
Jump to Table of Contents 115
Clinical
Poster #
98
Abstract Title:
Chronic Pelvic Pain After Sling Surgery - A case series
Presenter(s):
Satvir Kalsi
Authors:
Satvir Kalsi and Hong Wu, MD, MS
Dept/Division:
Pain Medicine and Rehabilitation
Category:
Student
Introductions:
Stress urinary incontinence (SUI) is the most common type of female incontinence and its
treatment options include surgical and non-surgical approaches. Bladder sling surgery (BSS) is
considered the preferred surgical option to treat SUI. Chronic pelvic pain following BSS is rare but
can be a serious complication. Here, we present 3 female patients who developed chronic pelvic
and groin pain after BSS.
Methods:
3 patient charts were reviewed retrospectively.
Results:
We present 3 female patients who developed chronic pelvic and groin pain after BSS involving
placement of a mesh (two transobturator and one transvaginal approach) to treat SUI. Aged 44,
43, and 49 y.o. at the time of surgery without any prior history of chronic pelvic pain, they then
presented with pelvic pain (burning in nature and worsening with position) for approximately 4
years, 10 months, or 7 months after the pain onset of each case, respectively. Conservative
management of this chronic pain showed no significant relief for all patients. Interventions such
as corticosteroids injection and radiofrequency ablation to the pudendal nerve produced pain
relief.
Conclusions:
SUI is the most common type of female incontinence and its treatment options include surgical
and non-surgical approaches. BSS is considered as a preferred surgical option to treat SUI. Chronic
pelvic pain following BSS is rare but can be a serious complication. Etiology for this could be a pre-
existing chronic pain disorder, surgical trauma and scarring, nerve entrapment related
neuropathy, and centralization of pain, etc. This pain can resist conservative treatment, can
progress or escalate, and may significantly affect patient’s quality of life. Additionally, it may
result in the development of other chronic pain conditions and psychological complications.
Our data suggest management of chronic pelvic pain following BSS can be a challenge. Pudendal
nerve block and ablation could be a novel technique to manage this pain. Additional research is
needed to identify the precise etiology of this chronic pain, deploy biomaterials or develop new
surgical techniques with better outcomes, and/or define risk factors to help prevent development
and/or halt progression of this chronic pain.

Research Day 2019
Jump to Table of Contents 116
Clinical
Poster #
99
Abstract Title:
Ultrasonographic Comparison of the Lateral Epicodyle in Manual Wheelchair-Users
Presenter(s):
Andrea Cyr, D.O.
Authors:
Andrea Cyr, D.O., Kenneth Lee, M.D., Berdale Colorado, D.O., Kristin Garlanger, D.O.
Dept/Division:
Physical Medicine and Rehabilitation
Category:
Clinical Fellows & Residents
Introductions:
Lateral epicondylosis, or “tennis elbow”, is a degenerative process related to repetitive wrist
extension, radial deviation and forearm supination that frequently results in elbow pain. Prior
study estimates that the prevalence of lateral epicondylosis in the general population is about
1.3%. Manual wheelchair-users depend on use of their upper extremities for mobility and several
studies estimate the prevalence of elbow pain at 30-35% among this population. Lateral
epicondylosis remains primarily a clinical diagnosis, however, ultrasound evaluation of the elbow
may reveal calcifications, tears, irregularity of the lateral epicondyle and thickening and
heterogeneity of the common extensor tendon, findings suggestive of lateral epicondylosis. To
our knowledge, this is the first study that seeks to determine the prevalence of clinical and
subclinical evidence of lateral epicondylosis of the dominant elbow in manual wheelchair-users
based on ultrasound assessment and physical exam.
Methods:
This is a prospective, cross-sectional study. Total of 90 participants (81 males and 9 females) who
are manual wheelchair-users were recruited at the 2018 and 2019 National Veteran Wheelchair
Games in Orlando, FL and Louisville, KY respectively. Participants completed a questionnaire on
demographics, the level of manual wheelchair use, cause of injury, and current symptoms. Each
participant received an ultrasonographic assessment and a physical exam of their dominant elbow
for evaluation of lateral epicondylosis. The dominant arm of each participant was examined using
an ultrasound machine evaluating for tendon thickening, increased vascularity and
hypoechogenicity. A standard physical exam was performed of the dominant elbow using Cozens
and Mills test.
Results:
Final analysis pending. Total of 90 participants recruited, ages 23 to 79, 9 females and 81 males.
Given present data, the prevalence of elbow pathology in manual wheelchair users is significantly
higher than able-bodied individuals. Lateral epicondylosis based on sonographic findings is nearly
4-times higher than based on physical exam alone. Comparisons will be made using odds ratios of
the pairwise differences between groups following logistic regression, adjusted for demographic
variables.
Conclusions:
Wheelchair-users depend upon increased use of their upper extremities thus are predisposed to
significant chronic joint pathology of the upper extremity. Compared to able-bodied population,
there is increased prevalence of subclinical lateral epicondylosis as determined by
ultrasonographic assessment.
Acknowledgements:
Matthew Durand, Ph.D., Moriah Iverson, M.S., Rachel Minkin, M.S., Vivian Roy, M.D., Sergey
Tarima, Ph.D
Research Day 2019
Jump to Table of Contents 117
Clinical
Poster #
100
Abstract Title:
Reducing readmissinos by standardizing discharge summary documentation
Presenter(s):
Jennifer Yacub Martin
Authors:
Jennifer Yacub Martin
Dept/Division:
Physical Medicine and Rehabilitation
Category:
Junior Faculty
Introductions:
One in five patients are readmitted to the hospital within 30 days of skilled nursing facility (SNF)
admission. Unplanned and unnecessary hospital readmissions from SNF are viewed as a deficit in
quality and value. New payment models such as bundled payment for care improvement (BPCI)
focus on penalization of these readmissions and reward for coordination of care. Given these
quality metrics and financial implications, focus should be placed on addressing these issues.
Methods:
Twelve months of 30 day readmission data was reviewed from the inpatient rehab unit at
Froedtert.
Eight unique patient encounters were identified as readmissions from SNF. Reason for
readmission was identified in the emergency department provider note and history and physical
at time of readmission. The inpatient rehab discharge summary was reviewed to check if
information related to the reason for readmission was included.
Results:
In our rehab unit, readmissions from SNF to acute medical and surgical floors were found to be
due to a variety of reasons including cranioplasties, surgical site infections, urinary tract
infections, hematomas. The average number of days on inpatient rehab unit was 17 days. The
average number of days to readmission from SNF on our unit was 13.5 days. Information missed
in the discharge summaries related to these readmissions include: anticipated surgery date,
surgical site exam at time of discharge, labs at time of discharge (CBC, BMP, UA/Culture results)
and duration of DVT prophylaxis.
Conclusions:
Unplanned readmissions from SNF can result in higher morbidity for patients and increased health
care spending. Clear communication provided in a discharge summary may assist with reducing
readmissions and therefore improved patient outcomes and reduced spending. Key information
that has been identified in readmission risk prediction models include: length of hospital stay, lab
values at time of discharge, status of medical comorbidities, accurate medication reconciliation
with duration of treatment. These data points can easily be included in a discharge summary and
provide anticipatory guidance to SNF therefore potentially avoiding readmissions.
Reference 1:
Chandra A et al. Risk of 30-day Hospital Readmission Among Patients Discharged to Skilled
Nursing Facilities: Development and Validation of a Risk-Prediction Model. JAMDA 20(2019) 444-
450.
Reference 2:
Vasilevskis E et al. Potentially Avoidable Readmissions of Patients Discharged to Post-Acute Care:
Perspectives of Hospital and Skilled Nursing Facility Staff. JAGS. Februrary 2017-Vol. 65, No.2.
Reference 3:
Finkel C and Worsowicz G. Changing Payment Models: Shifting Focus on Post Acute Crae. Missouri
Medicine. January/February 2017. 114:1. 57.
Acknowledgements:
Geoff Lamb, MD and the Scholars in Patient Safety and Quality Improvement Program

Research Day 2019
Jump to Table of Contents 118
Clinical
Poster #
101
Abstract Title:
Conservative Pain Management of Pre-Sacral Schwanomma: A Case Report
Presenter(s):
Jacob Pfeiffer
Authors:
Pfeiffer, Jacob; White, Christopher
Dept/Division:
Physical Medicine and Rehabilitation
Category:
Clinical Fellows & Residents
Introductions:
Schwannomas are usually benign tumors arising from Schwann cells of the peripheral nerve
sheath. Pre-sacral schwannomas comprise 1-5% of all schwannomas, and account for 1% of
retroperitoneal neoplasms. Pre-sacral schwannomas show very non-specific clinical features due
to their slow growth, most common presenting symptoms include abdominal pain, and
neurological deficit, but low back pain has also been reported as a presenting symptom.
Methods:
A case report was performed on 67 year old female with past medical history of hyperlipidemia,
pre-diabetes, who had new onset left low back pain. Was treated by outside provider as piriformis
syndrome, with improvement of piriformis complaints, but aggravation of new left sided low back
pain.
The patient was evaluated in outpatient PM&R clinic for 6 week history of left sided low back
pain, without associated lower extremity weakness, bowel/bladder dysfunction, or constitutional
symptoms on presentation. Initial evaluation performed by vascular surgery who obtained MRI of
the lumbar spine, which revealed a 4cm left upper pre-sacral mass. Patient underwent biopsy
which was found to be nerve sheath tumor.
Results:
She was initiated with physical therapy, and found minimal improvement over the first 2 months.
Was re-evaluated, and referred for left sacroiliac joint injection, in which she reported 50%
improvement of symptoms of left low back pain. She continued with therapy, which aggravated
new right sided sacroiliac joint pain. She was referred for bilateral SI joint injections, which she
reported alleviated 100% of her right sided back pain, and alleviated at least 60% of her left sided
back pain. During this time she continued to take meloxicam, and acetaminophen as needed for
pain, as well as home exercise program. Her need for meloxicam decreased from an average of 2
times per day to once a day after bilateral SI joint injections. Her pain scores decreased from a 6-
10/10 to a 0-4/10. Her pain has continued to be well managed with Home exercise program, and
intermittent Physical therapy refresher sessions.
Conclusions:
Non surgical management of pain with pre-sacral nerve sheath tumors is a viable option in
patients without significant neurological deficits. These treatments should be multi-factorial,
including therapy, medications and/or therapeutic injections.

Research Day 2019
Jump to Table of Contents 119
Clinical
Poster #
102
Abstract Title:
Complex Regional Pain Syndrome Management: An Evaluation of the Risks and Benefits of Spinal
Cord Stimulator Use in Pregnancy
Presenter(s):
Meagan Jozwiak
Authors:
Meagan Jozwiak MD, Hong Wu MD
Dept/Division:
Physical Medicine and Rehabilitation
Category:
Clinical Fellows & Residents
Introductions:
Spinal cord stimulators (SCS) were first introduced as pain modulators in 1967. In 1989, the
Federal Drug Administration (FDA) approved its use for nerve-related chronic pain. Clinical
indications for implantation of SCS include failed back surgery syndrome, epidural fibrosis,
arachnoiditis, ischemic limb pain, phantom limb pain, and complex regional pain syndrome
(CRPS).
CRPS is a type of chronic neuropathic pain that occurs after a trauma to an extremity, and its
treatment can be challenging given its symptomatology and unclear pathophysiology. When
multifactorial and conservative measures fail, patients may consider SCS implantation as a last
resort.
SCS has become an important treatment option for patients with CRPS. Its use has reduced pain
scores, improved quality of life, and has likely reduced the number of pain medications that would
otherwise be used. The utilization of SCS is currently not recommended in pregnancy due to lack
of safety data, and only a handful of case reports and literature reviews have been done on this
patient population.
Methods:
This 26-year-old female was diagnosed with CRPS Type I after a left knee surgery. She initially
presented with severe pain, redness, burning, and hypersensitivity to the left leg. She failed all
conservative treatments including medications, therapy, and lumbar sympathetic blocks. After the
birth of her first child, she underwent SCS implantation. The SCS brought near complete
resolution of her symptoms. When she became pregnant with her second child, she turned off her
SCS. Her CRPS symptoms intensified, but she had an otherwise normal pregnancy and safe
delivery. Her CRPS symptoms continued to be debilitating postpartum. In her third pregnancy, she
was referred by her obstetrician to our pain management clinic to discuss pre-conception
planning. She was interested in using her SCS during her third pregnancy. Her pain management
and obstetrician visits were well-documented for this pregnancy. A year after the birth of her last
child, she was contacted for a phone interview to discuss her pregnancies, the health of herself
and her children, and the functionality of her spinal cord stimulator.
Results:
The patient had two healthy, full-term pregnancies with no apparent complications after the
implantation of the SCS. She continued to have significant pain relief throughout her third
pregnancy in which she utilized her SCS, and there were no apparent complications during the
pregnancy or delivery. Her SCS remains functional to this day, and the patient and her children
continue to be healthy.
Conclusions:
This is the first reported case of a patient with CRPS who had two successful pregnancies after SCS
implantation. This self-controlled case report demonstrates that SCS implantation and utilization
can be safe and effective in pregnancy. Further research is needed to determine the safety and
efficacy of SCS in pregnancy.
Research Day 2019
Jump to Table of Contents 120
Clinical
Poster #
103
Abstract Title:
Provider level barriers to PrEP implementation in the United States: a systematic review
Presenter(s):
Benedikt Pleuhs
Authors:
Benedikt Pleuhs, Steven A. John, PhD, MPH
Dept/Division:
Psychiatry
Category:
Student
Introductions:
Increasing prescription of pre-exposure prophylaxis (PrEP) is imperative to ending the HIV
epidemic in the United States (US). The objective of this review was to identify healthcare
provider level barriers to PrEP implementation.
Methods:
The database PubMed was used to identify original studies focusing on PrEP prescription among
healthcare professionals in the US. The search terms used for this review were: “Pre-Exposure
Prophylaxis,” “PrEP,” “Preexposure Prophylaxis,” “providers,” and “physicians.” Articles were
extracted on February 15th, 2019. Titles and abstracts were reviewed to identify articles for full
text review. Studies were excluded if they took place outside of the US or did not focus on PrEP
prescription or implementation.
Results:
Six themes were identified across reviewed studies: (1) a lack of knowledge about PrEP, (2) the
presence of the Purview Paradox, (3) concerns about PrEP costs, (4) negative attitudes regarding
PrEP, (5) stigma, and (6) concerns about patient adherence.
Conclusions:
Additional work is needed to better prepare providers to prescribe and manage patients on PrEP,
optimize PrEP delivery, and reduce provider bias. Future research is needed to identify providers’
attitudes and beliefs regarding innovations in PrEP dosing (e.g., event-driven), long-acting
formulations, task-shifting, and novel strategies for PrEP prescription and maintenance care (e.g.,
home-based PrEP).

Research Day 2019
Jump to Table of Contents 121
Clinical
Poster #
104
Abstract Title:
Lithium Monitoring and Outcomes in the Perioperative Period: A Quality Improvement Project
Presenter(s):
Peter DeVries MD
Authors:
Peter DeVries MD, Claire Drom MD, Ana Navarro-Montoya MD, Njeri Wainaina MD
Dept/Division:
Psychiatry and Behavioral Medicine
Category:
Clinical Fellows & Residents
Introductions:
The perioperative period, with the associated fluid shifts between physiologic compartments,
represents a unique challenge to maintaining lithium homeostasis [Spell, 2001]. Despite the
known hazards, there is limited consensus on how to manage lithium dosing in surgical patients
[Huyse, 2006].
Methods:
For the initial phase of this quality improvement project, a 5-year chart review of adult surgical
patients receiving lithium at the time of admission was conducted. A total of 180 encounters met
inclusion criteria, with 128 unique encounters eventually being reviewed. Encounters were
stratified into planned and unplanned procedures. Adverse events were defined as lithium levels
>1.2mmol/L and/or delirium with or without the physical symptoms of toxicity.
Results:
In the planned procedure group (N=102), 35.5% were male, average age was 49.3 years, and
average lithium dose was 750mg QD. In the unplanned group (N=28), 73.1% were male, average
age was 46.2 years, and average lithium dose was 964.9mg QD. A total of 9 adverse events were
found, 6 in the planned group and 3 in the unplanned. In this group, the average age was 49.2
years, 66.7% were male, and the average lithium dose was 912.5mg QD. The average length of
admission was 17.7 days. Five patients underwent abdominal procedures and two were trauma-
related.
Conclusions:
Planned procedures represented 80% of encounters. Patients in the planned group were more
likely to be female and on lower total doses of lithium. Of the encounters reviewed, 7%
experienced an adverse event. Patients in this group were more likely to be male, on higher doses
of lithium, inpatient for longer periods of time, and undergoing an abdominal or trauma-related
procedure. Factors statistically associated with adverse events will be determined by regression
analysis and are expected to include age, lithium dose, type of procedure, and anticipated length
of stay.
To our knowledge, this project is unique in that it has characterized current practices in lithium
management in surgical inpatients and identified those at high risk of experiencing an adverse
event secondary to lithium. The next phase will be the design and implementation of a protocol
for lithium management. The envisioned protocol will provide guidelines on lithium dosing,
monitoring of serum levels, and use of interacting medications. Implementation will involve
collaboration with numerous departments, including pharmacy, perioperative medicine, and
several surgical specialties.
Reference 1:
Huyse FJ, et al. Psychotropic drugs and the perioperative period: A proposal for a guideline in
elective surgery. Psychosomatics 2006; 47:8-22.
Reference 2:
Spell NO. Stopping and restarting medications in the perioperative period. Medical Clinics of
North America 2001; 85(5): 1117-28.

Research Day 2019
Jump to Table of Contents 122
Clinical
Poster #
105
Abstract Title:
TransCarotid Artery Revascularization (TCAR): High-Risk Anatomical Lesions and Other Advantages
Over Trans-Femoral Approach
Presenter(s):
Robert Hieb, MD
Authors:
Tadi Ciszak, MD, Robert A. Hieb, MD, FSIR, Peter J. Rossi, MD, Michael Malinowski, MD, Parag J.
Patel, MD, MS, FSIR
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
TransCarotid Artery Revascularization (TCAR) utilizing the ENROUTE Neuroprotection System (Silk
Road Medical Inc, Sunnyvale, Calif) is a novel approach towards carotid artery stenting (CAS). This
minimally invasive approach utilizes intra-procedure high-rate flow reversal NPS and is designed
for CAS in patients who are deemed too "high-risk" for carotid artery endarterectomy (CEA). The
system has shown superior stroke and death outcomes when compared to prior registry results
from both CEA and trans-femoral CAS. The purpose of this study is to review of both short and
long-term outcomes in patients who underwent TCAR, and also to underscore high-risk
anatomical lesion that are made easier with TCAR over a trans-femoral approach.
Methods:
We performed an IRB approved single-center retrospective review of patients who underwent
TCAR procedures between 8/2017 and 9/2018. All interventions were performed in patients
deemed at high risk for complications from CEA, symptomatic patients with ≥50% stenosis, or
asymptomatic patients with ≥70% stenosis. A hybrid OR was utilized for all procedures and co-
staffed with a vascular surgeon (VS) and an IR. Patients were followed in clinic at 1, 6, and 12
months post procedure. Demographic data, anatomical considerations, and complications were
reviewed.
Results:
29 TCARs were performed on 28 patients, age range 59-85 (M:F, 19:9). Technical success rate was
(100%), with no acute device, technical, or access site complications. All lesions were successfully
crossed and 30 stents were deployed (1 lesion required two overlapping stents). One patient
underwent bilateral TCAR on separate occasions, and another patient underwent concurrent
TCAR and TVAR. Fifteen (15) anatomically challenging lesions were identified – 7 high carotid
bifurcations, 4 stenosis at or above C2 level, 3 long-segment lesions, and 1 tortuous ICA. One
adverse outcome was reported within 30-days (ipsilateral intraparenchymal hemorrhage), with an
overall adverse-free event rate of 97%. No myocardial infarction (MI) or death occurred. All
patients remained neurologically symptom-free at their follow up, and average time to follow up
was 151 days.
Conclusions:
TCAR is a safe and novel approach to CAS utilizing cerebral flow-reversal as a means of providing
neuroprotection. It can be used to tackle lesions deemed too “high-risk” for TF-CAS or CEA. This
procedure requires a high technical skillset and is best performed utilizing a multidisciplinary team
with VS and IR.

Research Day 2019
Jump to Table of Contents 123
Clinical
Poster #
106
Abstract Title:
Percutaneous Cryoablation for the Treatment of Extra-Abdominal Desmoid Tumors
Presenter(s):
Kaila Redifer Tremblay, MD
Authors:
K. Redifer Tremblay, W. Lea, J. Neilson, D. King, S. Tutton
Dept/Division:
Radiology: VIR
Category:
Clinical Fellows & Residents
Introductions:
Desmoid tumors are a rare form of locally invasive, benign neoplasms that develop along
aponeurotic structures with high recurrence rate after surgical resection. The purpose of this
study
was to evaluate the safety and efficacy of cryoablation for local disease control.
Methods:
A retrospective search of our single-institution database identified 23 patients with extra-
abdominal desmoid tumors who were treated with percutaneous cryoablation as both de novo
(61% pts) and salvage (39% pts) treatment in 28 sessions between 2014 and 2018. Mean lesion
diameter was 7.0 cm, ranging from 1.1 - 14.0 cm. 48% of patients were treated with the goal of
complete ablation, while 52% were treated for palliative debulking. Patient age ranged from 16 to
77 years. Tumors were treated in the abdominal wall, chest wall, shoulder girdle, upper extremity,
hip girdle, lower extremity, and head and neck. Imaging was evaluated for baseline tumor size,
MR characteristics, and enhancing tumor volume.
Results:
Technical success was achieved in 100% of patients. 90% of patients who were symptomatic on
presentation showed clinical improvement following ablation. One patient suffered a major
procedural complication consisting of significant neuropraxia. The average imaging follow-up was
14.6 months (SD +/- 10.9). Of 11 patients with follow-up imaging at 12 months, the enhancing
tumor volume showed either complete response (CR) or partial response (PR) in all patients (CR
27%, PR 73%), and the total lesion volume showed either CR or PR in 9 of 11 patients. No
treatments demonstrated rapid post-ablation growth or track seeding. Three patients underwent
repeat cryoablation for either residual or progressive disease.
Conclusions:
Cryoablation for desmoid tumors demonstrates a high degree of symptom improvement and local
tumor control on early follow-up imaging with relatively few side effects. Study limitations include
variable follow-up, small sample size, and the retrospective nature of this case series; however,
further studies should be pursued as these data provide promising results.

Research Day 2019
Jump to Table of Contents 124
Clinical
Poster #
107
Abstract Title:
Correlation between right artial pressures as measured by echocardiography (ECHO) versus direct
right heart pressure measurements in patients undergoing transjugular intrahepatic
portosystemic shunt(TIPS) placement
Presenter(s):
William Rilling, MD
Authors:
David Sarver, Matthew Mohorek, Kia Saeian, William Rilling, Sarah White, Eric Hohenwalter
Dept/Division:
Radiology: VIR
Category:
Senior Faculty
Introductions:
The purpose of this study was to investigate the correlation between right atrial pressures as
measured by echocardiography (ECHO) versus direct right heart pressure measurements in
patients undergoing transjugular intrahepatic portosystemic shunt (TIPS) placement. Pre-TIPS
right heart pressure may serve as a valuable prognostic indicator since patients with an elevated
baseline right atrial pressure are more prone to post-TIPS heart failure
Methods:
This is a single center, IRB approved, retrospective study evaluating all patients who underwent
TIPS from 1997 to 2017. Demographic data was collected, as well as diagnosis and indication for
TIPS, elective vs. emergent TIPS placement, pre-TIPS MELD score, pre-TIPS ECHO, and pre and
post TIPS intra-operative direct right atrial pressure measurements. A mean and standard
deviation of the absolute difference between measurements obtained by echocardiography and
right heart catheterization was obtained.
Results:
392 patients underwent TIPS placement over the 20 year period. Of those, 113 had pre-TIPS ECHO
and pre-TIPS direct right atrial pressure measurements. The study group was 56% male, 44%
female, with a mean age of 56 ± 9.8 years. The average calculated MELD score was 13.6 ± 5.9.
70% of patients were treated electively and the remaining 30% underwent emergent treatment.
The mean and standard deviation absolute difference between measurements obtained by ECHO
and direct right atrial pressure measurements was 8.1 ± 5.3 mmHg.
Conclusions:
ECHO measurements in patients undergoing evaluation for TIPS placement should be viewed with
caution. Correlation of cardiac status with direct measurements of right heart pressures during
TIPS placement remains imperative to accurately evaluate patient’s risk for post TIPS cardiac
complications.

Research Day 2019
Jump to Table of Contents 125
Clinical
Poster #
NOT PRESENTING
Abstract Title:
Expectations of Critical Radiology Result Communication
Presenter(s):
Zeeshan Qazi
Authors:
Zeeshan Qazi, Robert Treat, and Stacy D. O'Connor
Dept/Division:
Radiology
Category:
Student
Introductions:
Timely communication of critical results is a nationally patient safety concern and the division of
these results into 3 levels of urgency is accepted. However, little data exists comparing radiologist
and referring provider expectations regarding which imaging findings fall into which category of
critical results and how these results should be communicated.
Methods:
An anonymous survey asked radiologists and referring providers if ten findings were critical
results and, if so, what level. Preferred method of communication for each level, appropriateness
of the number of critical results called by radiologists, and level of difficulty in reaching someone
were also assessed. χ2 test compared the distribution of level category assignment for the
findings as well as communication preferences. A word cloud tool was used to analyze free text
comments for recurrent themes.
Results:
19% (124/658) of providers responded. The distribution of level of urgency differed between
radiologists and referring providers for intrabdominal abscess (p = .019), pulmonary nodule (p =
.02) and solid renal mass (p = .002). Although distribution for DVT was similar for the 2 groups,
overall 65/123 (52%) chose Level 2 and 53/123 (43%) chose Level 1. Among specialties,
emergency medicine had the most findings classified as level 1 with the highest proportion. Pager
was the preferred method of communication for level 1 53/123 (43%) and level 2 64/119 (54%)
critical results. E-mail is preferred for level 3 64/119 (54%) and for non-critical findings 56/110
(51%). Radiologists were the only specialists that reported many/too many critical results are
called 5/32 (16%) and that reaching someone in regard to a critical result is very difficult 2/18
(11%). Themes in free-text responses demonstrated a desire to use the EHR for communication
and for alerting providers of critical results prior to patients reading their reports.
Conclusions:
Differences between and amongst radiologists and referring providers were found in
categorization of findings as critical results. Referring providers, especially emergency medicine,
are more likely to choose higher levels of urgency. Radiologists and referring providers have
differing expectations for critical results communication, creating opportunities for
interdisciplinary consensus building and education.
Acknowledgements:
Biostatistics Consulting Service - Division of Biostatistics

Research Day 2019
Jump to Table of Contents 126
Basic Science
Poster #
108
Abstract Title:
Modeling the Kinetics and Regulation of NADPH Oxidase 2 Assembly and Activation Facilitating
Electron Flow and Superoxide Generation
Presenter(s):
Shima Sadri
Authors:
Shima Sadri, Namrata Tomar, Said H. Audi, Allen W. Cowley Jr, Ranjan K. Dash
Dept/Division:
Biomedical Engineering
Category:
Student
Introductions:
Reactive oxygen species (ROS) play a crucial role in key physiological processes, including
regulation of cell signaling cascades. However, ROS overproduction leads to oxidative stress,
which plays a critical role in cell injury/death, premature aging, and pathogenesis of several
diseases. Members of the NADPH oxidase (NOX) family comprising of membrane and cytosolic
components are known to be the major non-mitochondrial sources of ROS in most mammalian
cells. NOX2 is the most widely expressed and well-studied NOX isoform. NOX2 is activated upon
assembly of its membrane-bound subunits gp91phox and p22phox with the cytosolic subunits
p40phox, p47phox, p67phox, and Rac facilitating electron flow and ROS production. Specifically,
upon NOX2 assembly and activation, electrons are transferred from substrate NADPH to
molecular O2 through different redox centers of NOX2 complex resulting in oxidized NADP+ and
reduced O2-. (superoxide) as a ROS product. Yet, there is a lack of a mechanistic and quantitative
understanding of the kinetics and regulation of the assembly of NOX2 subunits and their relative
contributions towards NOX2 activation and ROS production.
Methods:
A mechanistic computational model was developed to describe NOX2 assembly, activation,
electron flow, and ROS production. The model incorporates our hypothesized “random rapid
equilibrium binding mechanism” for NOX2 assembly and activation, regulations by guanine
nucleotides (GTP, GDP), and mutual binding enhancements between individual cytosolic subunits
(p40phox, p47phox, p67phox, Rac). The model uses diverse published data, all of which use cell-
free reconstituted NOX2 activation system, to estimate the unknown kinetic model parameters
using a hybrid Markov Chain Monte Carlo (MCMC) simulation approach and the built-in “fmincon”
optimization algorithm in MATLAB.
Results:
: The proposed model shows that NOX2 is differentially activated and regulated by p40phox,
p47phox, p67phox, and Rac subunits. In addition, the model shows that the assembly of NOX2
subunits is regulated by GTP, GDP, and other cytosolic subunits. Particularly, the model can
describe enhancements in the binding affinities of p47phox, p67phox and Rac subunits by GTP,
reductions in the binding affinities of the same cytosolic subunits by GDP, mutual binding
enhancement between p47phox, p67phox and Rac subunits, and enhancement in the binding
affinity of p47phox by p40phox. The NOX2 reaction flux and regulations are characterized by two
sets of parameters for two different NOX2 assembly and activation experimental system based on
five sets of independently published experimental data.
Conclusions:
The proposed model provides the first quantitative and integrated understanding of the kinetics
and regulation of NOX2 assembly and activation, and the importance of these processes in
facilitating electron flow and ROS production. The model, which can simulate diverse published
experimental data, also serves as a mechanistic and quantitative framework for investigating the
critical role of NOX2-mediated ROS production in regulating diverse cellular mechanisms under
physiological and pathophysiological conditions.

Research Day 2019
Jump to Table of Contents 127
Basic Science
Poster #
109
Abstract Title:
Genomic profiling for Personalized Medicine - technologies and services offered by the GSPMC
Presenter(s):
Jamie Wendt-Andre
Authors:
Jaime Wendt Andrae, Stefano Rosati, Wendy Demos, Kathryn Stoll, Charles Salmonson, Amy
Bauer, Ashley Steger, Brandon Smith, Shivani Kapoor, Rebecca Tyler, Kevin Havens, Ulrike Kappes,
Raul Urrutia, Gunter Scharer, Honey Reddi, Donna Hoeffler, Annette Foshey.
Dept/Division:
GSPMC
Category:
Research Support Staff
Introductions:
Personalized Medicine offers customized options for the treatment and management of disease
using individualized genomic profiling. Genomic profiling can be tailored to the specific need of
the patient, e.g. for tailored treatment in oncology (pharmacogenetics), or for the diagnosis of
rare, and undiagnosed hereditary diseases,. The mission of the GSPMC is to harness the power of
genomics to better understand, prevent, detect, and treat disease with high accuracy. Towards
this end, the GSPMC has established a clinical laboratory that houses state-of-the-art molecular
technologies, including whole genome and exome sequencing for hereditary disorders and an
variety of assays on multiple platforms for molecular oncology testing.
Methods:
Under the umbrella of the Precision Medicine Initiative (PMI) at MCW, the GSPMC has
consolidated 3 laboratories across campus under one roof to offer a consolidated one-stop-shop
for genomic profiling in molecular oncology and inherited disorders addressing the needs of
clinicians on campus, patients, and researchers.
Results:
The GSPMC offers clinical whole genome and whole exome sequencing that can also be used to
report on customized, disease specific gene panels for inherited disorders. In fact, as part of the
Human and Molecular Genetics Center, GSPMC was the first laboratory in the United States to
offer WGS as a diagnostic test. The oncology portfolio includes histology services and targeted
next generation sequencing panels for precision medicine. The Center houses a number of high
throughput platforms such as the NovaSeq, HiSeq, MiSeq Ion S5 prime and 10X single cell for
Next-Generation sequencing services as well as the Biocartis Idylla for hotspot mutation
evaluation and the ABI 3730 and 3500 for Sanger sequencing. Customized bioinformatics support
is offered by the Bioinformatics and Data Analysis group for clinical and research needs. All
services are available to clinicians and researchers alike, e.g. in the context of projects, grant
applications, clinical trials, and collaborations.
Conclusions:
The new GSPMC services include an expanded menu of assays and clinical tests that are
competitively priced and customizable. The Center is determined to change the practice of
medicine, optimize data-driven healthcare, and to ensure a lifetime of tailored care to each
individual. These services can be utilized to investigate how environmental factors, drugs and
gene variations impact gene expression, as well as to define the clinical impact of genetic variants
associated with human development and disease.
Reference 1:
Vogenberg, FR et al. Personalized Medicine. Part 1: Evolution and Development into Theranostics
P T. 2010.35:10, 560-562
Reference 2:
Borad and LoRusso. Twenty-First Century Precision Medicine in Oncology: Genomic Profiling in
Patients With Cancer. Mayo Clinic Proceedings. 92:10, 1583-1591.

Research Day 2019
Jump to Table of Contents 128
Basic Science
Poster #
110
Abstract Title:
Aurora Kinase B-phosphorylated HP1a Functions in Chromosomal Instability
Presenter(s):
Angela Mathison
Authors:
Monique M. Williams, Angela J. Mathison, Trent Christensen, Patricia T. Greipp, Darlene L.
Knutson, Eric W. Klee, Michael T. Zimmermann, Juan Iovanna, Gwen A. Lomberk, Raul A. Urrutia
Dept/Division:
GSPMC, Surgery
Category:
Junior Faculty
Introductions:
Members of the Heterochromatin Protein 1 (HP1) family of conserved non-histone chromatin
proteins, first discovered in Drosophila melanogaster, were originally noted for their role in
heterochromatin-mediated gene silencing. Mammalian genomes encode three HP1 proteins;
HP1a (CBX5), HP1b (CBX1), and HP1g (CBX3). These proteins work as epigenetic regulators and
readers of the histone 3 lysine 9 dimethyl (H3K9me2) and trimethyl (H3K9me3) marks.
Heterochromatin Protein 1a (HP1a) associates with members of the chromosome passenger
complex (CPC) during mitosis, at centromeres where it is required for full Aurora Kinase B
(AURKB) activity. Conversely, recent reports have identified AURKB as the major kinase
responsible for phosphorylation of HP1a at Serine 92 (S92) during mitosis.
Methods:
The current study was designed to better understand the functional role of this
posttranslationally modified form of HP1a. With phosphorylation specific antibodies, the
intracellular localization of HP1a was studied at various stages of cell cycle and in localization with
other centromere markers, AURKB, inner centromere protein (INCENP) and centromere protein A
(CENPA). Localization could be perturbed by the inhibition of AURKB activity through hesperidin
or gene knockdown. To evaluate effects of HP1 on chromosomal stability, fluorescent in situ
hybridization (FISH) spreads and DAPI stained mitotic cells were evaluated for chromosomal
abnormalities upon HP1a knockdown and rescue with non-phosphorylatable mutants of HP1a.
Results:
We find that S92-phosphorylated HP1a is generated in cells at early prophase, localizes to
centromeres, and associates with regulators of chromosome stability, such as INCENP. In mouse
embryonic fibroblasts, HP1a knockout alone or reconstituted with a non-phosphorylatable (S92A)
HP1a mutant results in mitotic chromosomal instability characterized by the formation of
anaphase/telophase chromatin bridges and micronuclei. These effects are rescued by exogenous
expression of wild type HP1a or a phosphomimetic (S92D) variant.
Conclusions:
In this study, we extend investigations on the role of HP1a as an effector of mitotic kinase
pathways and demonstrate that this AURKB-modified target localizes to the centromere
kinetochore complex. This suggests a role in maintaining mitotic fidelity. We find that loss of HP1a
leads to chromosomal instability, which is dependent on its AURKB-mediated phosphorylation.
This knowledge underscores the importance of chromatin proteins as mediators of chromosomal
stability downstream of pro-oncogenic pathways, such as AURKB.

Research Day 2019
Jump to Table of Contents 129
Basic Science
Poster #
111
Abstract Title:
Precision Medicine Approaches in Pancreatic Cancer Revealed New Therapeutic Targets Derived
from Tumor-Stroma Cross-Talk
Presenter(s):
Raul Urrutia
Authors:
Angela Mathison, Gwen Lomberk, Ezequiel Calvo, Nelson Dusetti, Juan Iovanna, Raul Urrutia
Dept/Division:
GSPMC, Surgery
Category:
Senior Faculty
Introductions:
Preclinical models based on patient-derived xenografts have remarkable specificity in
distinguishing transformed human tumor cells from non-transformed murine stromal cells
computationally. While pancreatic ductal adenocarcinoma (PDAC) is the fourth leading cause of
cancer-related deaths, few integrative genomic, epigenomic, and transcriptomic studies have
been conducted. This is mainly due to difficulty in obtaining an appropriate series of PDAC tumor
samples. Another critical issue is the high proportion of non-transformed stromal cells infiltrating
the tumor, which greatly hinders the analysis of carcinogenic-specific processes.
Methods:
We obtained 29 PDAC xenografts from either resectable or non-resectable patients (surgery and
endoscopic ultrasound-guided fine-needle aspirate, respectively). Patient-derived xenografts
(PDXs) are progressively appearing as a prime approach for much-needed preclinical studies and,
in particular, to characterize drug efficacy. A major advantage of PDXs is that tumor cells preserve
their complex 3D organization by being embedded in an active microenvironment with an
elaborate and dynamic cellular composition. PDXs were used to generate genomic, epigenomic,
and transcriptomic profiles. In order to accurately analyze bulk xenograft samples, we developed
a methodology that we termed SMAP (simultaneous mapping for patient-derived xenograft),
which uses both the human and mouse genomes to distinguish reads from the tumor and stromal
compartment, respectively.
Results:
Extensive multi-omic profiling revealed two subtypes with distinct clinical outcomes. These
subtypes uncovered specific alterations in DNA methylation and transcription as well as in
signaling pathways involved in tumor-stromal cross-talk. The analysis of these pathways indicates
therapeutic opportunities for targeting both compartments and their interactions. In particular,
we show that inhibiting NPC1L1 with Ezetimibe, a clinically available drug, might be an efficient
approach for treating pancreatic cancers.
Conclusions:
In conclusion, the data presented in this work reveal that PDX is a suitable model for preclinical
studies, representing the diversity of the primary cancers in which the stroma is reconstituted.
This multi-omic analysis uncovers the complex and diverse interplay between PDAC tumors and
the stroma and demonstrates the pivotal role of xenografts in drug discovery and targeted
therapeutics for patients with PDAC.

Research Day 2019
Jump to Table of Contents 130
Basic Science
Poster #
112
Abstract Title:
Work at the Precision Medicine Simulation Unit Identifies a Novel, Alternative Spliced Isoform of
the Cancer-Associated Epigenomic Regulator, HP1y
Presenter(s):
Thiago Milech De Assuncao
Authors:
Angela Mathison, Thiago Milech De Assuncao, Nikkita R. Dsouza, Monique Williams, Michael T.
Zimmermann, Gwen Lomberk, and Raul Urrutia
Dept/Division:
GSPMC, Surgery
Category:
Research Support Staff
Introductions:
HP1 is a cancer-associated chromatin protein, which was first identified as a major component of
heterochromatin. HP1 is highly conserved from S. pombe to mammals, in which three isoforms
exist; HP1α, HP1Β, and HP1y. Three HP1 isoforms in mammals are similar in amino-acid
sequences and structural organization, but functionally distinct. The structure of HP1 proteins
includes an N-terminal chromodomain (CD), followed by a linker region, and then a C-terminal
chromoshadow domain (CSD). By reading the H3K9Me3 mark through their CD, HP1 proteins play
a significant role in the epigenetics of cancer-associated processes, including cell proliferation,
differentiation, chromosomal stability, and DNA repair.
Methods:
Here we describe and characterize a novel short isoform of HP1y, containing only the CD. To
consider expression of this isoform, RNA-Seq was performed in Pancreatic ductal adenocarcinoma
cells (PDAC) and protein levels confirmed by Western blot and immunofluorescence. Additionally,
transcript expression was surveyed across cohorts of human tissues using a commercial human
total RNA panel and using the GTEx reference dataset. Molecular modelling of the sHP1y
structure was performed using MODELLER.
Results:
Analyses of RNA-Seq experiments from PDAC reveal the existence of a novel short HP1y isoform,
named here sHP1y, generated by alternative splicing. The translation of this protein in PDAC cells
was confirmed by western blot analyses, using a newly developed antibody. This alternatively-
spliced isoform is composed of 101 residues and lacks the C-terminal chromoshadow domain
(CSD), which is required for dimerization and heterodimerization. qPCR analyses demonstrate that
the transcript is expressed and widely present across normal human tissues as well as various
cancer cell types. Using publicly available RNA-Seq data, we confirmed sHP1y expression in the
majority of human tissues and cancer types. Immunofluorescence microscopy confirms that the
novel sHP1y isoform, localizes to the nucleus. Fold recognition, order-to-disorder calculations,
homology-based molecular modeling, docking, and molecular dynamic simulations show that the
sHP1y displays an IDR-CD-IDR domain organization. Modeling and molecular dynamics
simulations predict that this isoform retains its ability to bind the H3K9Me3 mark.
Conclusions:
We infer that alternative splicing of the HP1y gene gives rise to different histone code readers,
which have distinct structural and molecular properties to likely function in both overlapping and
divergent manners. Thus, our data supports the notion that, due to the existence of functionally
different isoforms, the regulation of HP1y-mediated functions is more complex than previously
anticipated.

Research Day 2019
Jump to Table of Contents 131
Basic Science
Poster #
113
Abstract Title:
The Histone 9 Methyl Transferase, G9a, is a Direct regulator of the cell cycle regulator, Cdkn1A
(p21) During KRAS-Mediated PDAC Initiation
Presenter(s):
Tim Stodola
Authors:
Angela Mathison, Thiago Milech de Assuncao, Guillermo Urrutia, Ann Salmonson, Nelson Dusetti,
Tim Stodola, Romica Kerketta, Juan Iovanna, Raul Urrutia, Gwen Lomberk
Dept/Division:
GSPMC, Surgery
Category:
Postdoctoral Fellow
Introductions:
Pancreatic ductal adenocarcinoma (PDAC) ranks third in cancer caused deaths and is almost
universally fatal, with the annual number of deaths equivalent to the number of newly diagnosed
cases. While genetic aberrations contribute to PDAC development and early progression, specific
epigenomic landscapes are responsible for the acquisition of tumor heterogeneity. Following
recent evidence that the H3K9me pathway is altered in pancreatic cancer1, we here test the ability
of G9a, a major Histone Methyl Transferase, to regulate transcriptional repression, mediate
oncogenic KRAS-induced cell growth, and initiate PDAC.
Methods:
Studies on the expression, localization, and function for G9a and its complex partners, were
performed in genetically engineered cells and animal models. Pancreatic lesions were identified
and characterized by histopathology and immunohistochemistry with an indepth analysis of acinar
to ductal metaplasia in 3D cultures. Molecular analyses were performed using Western blots, and
immunofluorescence staining with senescence measured by b-gal, apoptosis by TUNNEL, and
proliferation by Ki67 staining. Global and pathway specific gene expression changes were tested by
RNA-Seq, qPCR arrays in the control and G9a knockout pancreas. Finally, chromatin
immunoprecipitation (ChIP) assays were utilized to monitor the promoter occupancy of G9a and its
H3K9Me2 mark.
Results:
KRASG12D induces the protein levels of G9a and its partners, GLP and WIS, which further stimulate
the formation of their complex. Interestingly, conditional, pancreas-specific G9a KO 1- significantly
reduced H3K9me2 levels, 2- antagonizes oncogenic KRAS-mediated ADM and PanIN formation as
well as 3- abolishes the gene signature characteristic of PDAC initiation. RNA-Seq and qPCR arrays
data showed that G9a inactivation establishes a transcriptional profile antagonistic to cell growth
via cell cycle regulators and checkpoint pathways. Histopathological analyses, TUNEL, and RNA-Seq
of the G9a knockout model demonstrate that the lack of initiation occurs via the induction of
apoptosis and an upregulation of p21, a cyclin-dependent kinase inhibitor that facilitates cell cycle
arrest in response to DNA damage. Increased levels of p21 protein are also observed in pancreatic
lysates from the combination G9a knockout and KRASG12D overexpression as compared to control
mice. This effect (p21 upregulation) is recapitulated in vitro by pharmacological inhibition or siRNA-
mediated knockdown of G9a in cells with oncogenic KRAS and leads to cell death. Furthermore, we
find G9a and its mark, H3K9Me2 occupy the p21 promoter, demonstrating that G9a directly
regulates this gene in response to KRAS signaling.
Conclusions:
Combined, this data describes a KRAS-G9a-P21 pathway and alteration of the epigenetic landscape
that is necessary for PDAC initiation and cell survival. Targeting these components defines a novel
mechanism, which because of the availability of new G9a pharmacological inhibitors, open
opportunities for designing futuretherapeutic intervention to fight this dismal disease.

Research Day 2019
Jump to Table of Contents 132
Basic Science
Poster #
114
Abstract Title:
Genomic variation in PDAC-predisposing genes identified using the MCW germline exome panel
Presenter(s):
Jennifer Geurts
Authors:
Michael T. Zimmermann, Susan Tsai, Jenica L. Abrudan, Wendy Demos, Michael Tschannen,
Jennifer Geurts, Angela Mathison, Gwen Lomberk, Douglas Evans, Raul Urrutia
Dept/Division:
GSPMC
Category:
Junior Faculty
Introductions:
Milwaukee has a 17% higher incidence of Pancreatic Ductal Adenocarcinoma (PDAC) than the rest
of USA. PDAC remains one of the deadliest forms of cancer, yet molecular and genetic causes
shared by patients remain elusive. Germline susceptibility, in particular genetic variants in DNA
repair genes, have a clear mechanistic link to pancreatic cancer development, but few patients
have a pathogenic variant in one of these genes, limiting their clinical impact. Here we
investigated 53 PDAC risk alleles in the germline of patients with pancreatic cancer, to better
understand the genetic risk factors and potential genetic modulators of disease. Currently, few of
the germline genomic variants in these genes are known to be pathogenic, leaving a significant
number classified as variants of unknown significance (VUS), which are not able to be used in
patient care. Thus, it is of significant interest and clinical value to identify which VUS are likely to
have a disease relevance.
Methods:
Peripheral blood mononuclear cells were isolated and DNA extracted from 537 patients in our
PDAC biobank. GSPMC developed a novel 53 gene PDAC Germline AmpliSeq panel, targeting
genes with known roles across DNA damage repair, matrix reorganization, and pancreatitis risk.
The patient cohort was sequenced across the panel with 2x300bp paired-end reads on the
Illumina MiSeq platform and targeted a median of 300x coverage. Variants were identified and
annotated across the Human Gene Mutation Database (HGMD), ClinVar, Catalogue Of Somatic
Mutations In Cancer (COSMIC), The Cancer Genome Atlas (TCGA), and Genome Aggregation
Database (gnomAD). We used snpEff to annotate the protein coding effect of each variant.
Results:
This cohort was analyzed from a unique perspective that combines annotations of prior
observations from both germline and somatic contexts. Most variants, 67%, detected in our
cohort were novel VUS, with no annotation in any of the 4 disease databases used, highlighting
the underlying genetic diversity and need to sequence each patient. For this cohort, all patients
have VUS in the sequenced genes, with an average of 16 previously reported and 2 novel VUS per
patient respectively. Interestingly, variants (VUS or pathogenic) were not limited to one per gene
- many genes have multiple VUS per patient. For example, ATM has 20 patients with 6 or more
VUS; the implications of concurrent VUS are unstudied. Finally, we identified germline diseases
associated with pathogenic variants and subdivide out cancer and cancer risk syndromes.
Conclusions:
Classifying and determining the impact of patient VUS is of significant relevance for improving
cancer screening, genetic counseling, and in some cases therapy. Nearly all patients in our cohort
have a VUS in a DNA repair gene. We are optimistic that future bioinformatic-based and
functional validation experiments will help to shed further light into the true pathogenicity
potential of these variants and if a subset of them can be identified as likely pathogenic, then a
greater fraction of patients will directly benefit from genomics testing.

Research Day 2019
Jump to Table of Contents 133
Basic Science
Poster #
115
Abstract Title:
Proteomics, RNA-Seq, ATAC-Seq, RRBS, and Multi-parametric ChIP-Seq Intergration Reveal the
Early Epigenomic Landscape of Oncogenic Kras Signaling
Presenter(s):
Romica Kerketta
Authors:
Romica Kerketta, Angela Mathison, Thiago Milech De Assuncao, Tim Stodola, Lida Zheighami,
Jenica Abrudan, Wendy Demos, Michael Zimmermann, Gwen Lomberk, Raul Urrutia
Dept/Division:
GSPMC
Category:
Research Support Staff
Introductions:
Pancreatic ductal adenocarcinoma (PDAC) develops through accumulation of genetic alterations,
with the KRAS oncogene being the earliest genetic mutation found, which drives the progression
of preneoplastic pancreatic intraepithelial neoplasia (PanIN) lesions into carcinoma. Direct
targeting of KRAS has been clinically unsuccessful and the downstream impact that the
constitutive activation of KRAS has on chromatin remains unknown. Thus, to identify chromatin
events downstream of oncogenic KRAS which can be clinically targeted, we investigated the
earliest changes at the transcriptomic and epigenomic levels that occur following activation.
Methods:
Our in vitro pancreatic cell model was derived from a genetically engineered mouse, carrying a
doxycycline-inducible KRASG12D transgene. At different time points following doxycycline
treatment, western blot was used to evaluate levels of oncogenic KRAS and broad alterations in
the epigenetic landscape. Subsequently, RNA, cross-linked chromatin and DNA were isolated for
next generation sequencing (NGS). The epigenetic landscape was assessed through transcriptomic
sequencing (RNA-seq) for gene expression, chromatin immunoprecipitation sequencing (ChIP-seq)
with histone marks to assess active and silenced chromatin, and reduced representation bisulfite
sequencing (RRBS) for DNA methylation. After sequencing, advanced bioinformatics tools were
used to process, integrate and analyze relationships among signaling pathways and the epigenetic
landscape. Proteomic changes were also interrogated using a cancer signaling array.
Results:
Induction of oncogenic KRAS was confirmed by western blot using a G12D specific antibody. RNA-
seq data indicated that following KRAS induction, genes involved in the regulation of epithelial to
mesenchymal transition (EMT) and metabolic pathways were downregulated, while genes
involved in KRAS signaling and cellular proliferation were upregulated. ChIP-seq revealed that
KRAS activation was correlated with an increase in the deposition of histone marks associated
with enhancers/super-enhancers (H3K27ac and H3K4me1), activated promoters (H3K4me3), and
an increase in regions silenced by polycomb (H3K27me3). Integration of RNA-seq and ChIP-seq
data demonstrated that up- or down-regulated genes also had corresponding alterations of the
H3K27ac and H3K4me3 activating histone marks near their promoters. DNA methylation levels of
several CpG islands were also altered following KRAS induction. Proteomic arrays highlight the
upregulated activity of genes involved in cell cycle and PI3K-Akt-mTOR signaling.
Conclusions:
Based on our results, exposure to oncogenic KRAS induced pancreatic cells to acquire a more
epithelial-like phenotype with increased proliferation, which coincided with changes in the
transcriptome, proteome and epigenome. RRBS demonstrated that KRAS induction shifts the
differentially methylated regions across the genome. Through genomic mapping of histone
modifications, we observed a marked increase in active enhancers and super-enhancers, as
measured by H3K27ac and H3K4me1 peaks, implicating histone acetyltransferases as downstream
epigenetic modulators of the KRAS signaling pathway. These enzymes may therefore serve as
potential drug therapy targets in future studies to disrupt KRAS mediated oncogenesis pathways
and mitigate the progression of PDAC.

Research Day 2019
Jump to Table of Contents 134
Basic Science
Poster #
116
Abstract Title:
Developing surface-based scores for interpreting genomic variants
Presenter(s):
Nikita R. Dsouza
Authors:
Nikita R. Dsouza, Swarnendu Tripathi, Raul Urrutia, Michael T. Zimmermann
Dept/Division:
GSPMC
Category:
Research Support Staff
Introductions:
Interpreting genetic variants usually begins by identifying how they affect protein-coding
sequences, but rarely is the 3D protein molecule considered in clinical assessment. We are
establishing methods to assess clinical variants using 3D approaches. Many properties of the 3D
protein molecule are dictated by its surface. Surface properties affect how proteins interact with
each other, biologic membranes, and small molecules, but may also affect stability. Algorithms
have been developed to calculate surface properties. We are using these methods to develop a
method to statistically assess changes in surface properties due to genomic variants.
Methods:
The study included protein that have an overall effect like Thermophilic versus Mesophilic
proteins, down to variants having a focal effect on surface properties like genomic variants or
Post-Translational Modifications (PTMs). We used experimental structures obtained from RCSB’s
Protein Data bank and computational metagenesis using FoldX. We developed an approach using
available tools to calculate the electrostatic potential for the surface. We evaluated the change
using multiple statistical tests to see if the surface changes were significant and to evaluate the
performance characteristics of each statistical test.
Results:
The evaluation for the surface potential distribution showed that the distribution for the
thermophilic and mesophilic differed from each other and had a significant p-values using
quantile-based tests, but not using tests based on detecting mean differences. Some variants in
the genes used in the study had a significant effect whereas some were similar to the WT which
was used as a control. The statistical methods help evaluate the surface potential change when
there is an overall change and they are used as a reference to measure the difference in the
potential when a genomic variant leads to a focal change. We found that statistical tests were
more sensitive when applied to regions of the protein centered on the altered site. When protein
dynamics are included, we were able to identify changes to protein surface properties that are far
away from the genomic variant, yet have allosteric effects.
Conclusions:
The method developed can help us determine the effect of a genomic variant on the encoded
protein. Statistical significance can be measured through multiple statistical tests, but the most
sensitive approach has to be tailored to each protein. This study demonstrates that small changes
in amino acid sequences can affect the electrostatic distribution of the protein surface.
Reference 1:
Zimmermann, M. T., Urrutia, R., Oliver, G. R., Blackburn, P. R., Cousin, M. A., Bozeck, N. J., & Klee,
E. W. (2017). Molecular modeling and molecular dynamic simulation of the effects of variants in
the TGFBR2 kinase domain as a paradigm for interpretation of variants obtained by next
generation sequencing. Plos One, 12(2). doi:10.1371/journal.pone.0170822
Reference 2:
Zimmermann, M. T., Urrutia, R., Cousin, M. A., Oliver, G. R., & Klee, E. W. (2018). Assessing Human
Genetic Variations in Glucose Transporter SLC2A10 and Their Role in Altering Structural and
Functional Properties. Frontiers in Genetics, 9. doi:10.3389/fgene.2018.00276

Research Day 2019
Jump to Table of Contents 135
Basic Science
Poster #
117
Abstract Title:
NOS1-derived nitric oxide regulates NFκB activation and macrophage polarization
Presenter(s):
Diego Rodrigues Coelho
Authors:
Diego Rodrigues Coelho, Veronica Paviani, Benjamin N. Gantner, Marcelo G. Bonini
Dept/Division:
Medicine: Endocrinology
Category:
Postdoctoral Fellow
Introductions:
At the molecular level, macrophage immune activation is directed in large part by the nuclear
translocation and assembly of nuclear factor κB (NFκB) into functionally distinct transcription
factors. While the canonic p65/p50 NFκB heterodimer is required for the expression of pro-
inflammatory genes, other configurations such as p50 homodimers and p65 homodimers may
have alternative functions in inflammation resolution. Our group described that NOS1-derived
nitric oxide (NO) is essential in the regulation of pro-inflammatory gene expression leading to the
hypothesis that NO formed in the nucleus regulates the assembly and gene targeting of NFκB-
family of transcription factors.
Methods:
Bone marrow-derived macrophages (BMDM) were isolated from nitric NOS1-/- mice, and
activated with LPS. The nuclear localization of both p65 and p50 was evaluated by
immunofluorescence microscopy in different time points after LPS stimulus. We also monitored
the nuclear translocation of GFP-labeled p65 in BMDM. To analyze the expression of NFκB target
genes, mRNA was purified and quantified by qPCR.
Results:
Our results with NOS1-/- BMDM indicated that in the absence of nuclear NO the stoichiometry of
p65/p50 in the nucleus is lost during early hours of LPS-induced activation, compared to WT cells.
By tracking GFP-labeled p65 in real time, we found p65 moves in and out of the nucleus during
the polarization process of WT macrophages, but in NOS1-/- cells nuclear p65 gradually increases
inside the nuclear compartment. Interestingly these different kinetic patterns of p65 and p50
translocation reflected in the differential downregulation of several but not all pro-inflammatory
cytokines. Among the most differentially expressed cytokines were IL1Β and IL6, which are
markers of pro-inflammatory M1 polarization and critical mediators of the acute phase
inflammatory and adaptive immune responses.
Conclusions:
Hence, results so far suggest the novel concept that NOS1-derived NO produced in the nucleus of
macrophages acts as a pacemaker synchronizing rhythms of p65 and p50 dynamics, assembly and
transcriptional activity during inflammation.

Research Day 2019
Jump to Table of Contents 136
Basic Science
Poster #
118
Abstract Title:
Use of chemogenetic systems and biosensors to generate and sense H2O2 within organelles in
live cells: implications for epigenetics and cell biology
Presenter(s):
Flavio Romero Palma
Authors:
Flavio Romero Palma; Marcelo G Bonini
Dept/Division:
Medicine: Endocrinology
Category:
Postdoctoral Fellow
Introductions:
Reactive oxygen species (ROS) are highly reactive molecules mainly generated as metabolic by-
products from a number of cellular pathways. Historically, redox signaling has been studied in the
cytoplasmic context, since this compartment contains the organelles that are the major sources of
ROS. Although some species could act by regulating transcription factors and nuclear genes, ROS
generation and their effects in the nucleus are still not well known for basic nuclear processes, as
well as for proliferation and epigenetics. Therefore, the aim of our work is to investigate how the
production of nuclear H2O2 affects cell cycle and drives epigenetic changes.
Methods:
We coupled a NLS-D-amino acid oxidase (DAAO), a H2O2-generator chemogenetic system, with
NLS-roGFP2-Orp1, a redox biosensor, to respectively produce and sense H2O2 in the nucleus of
MCF10A ER-Src cells. After treatment with different concentrations of D-Alanine, we determined
the redox state of the nucleus by using Confocal Microscopy. We assessed the expression levels of
genes related to nucleosome and chromatin structure by using qPCR and verified the levels of
Histone 3 PTMs (H3K4Me3, H3K9Ac, H3k9Me3, H3k14Ac, H3k27Ac and H3k27Me3). Finally, we
used a Fast FUCCI (Fluorescence Ubiquitination-based Cell Cycle Indicator) to monitor the cell
cycle and we tested the cellular proliferation by performing growth curves and wound healing
assays.
Results:
Our results show that the nuclear-generated H2O2 is dependent on the concentration of D-
Alanine. H2O2 affected the expression of H2B, H4 and H3 variants (H3.1, H3.2 and H3.3) with a
possible role of H3’s cysteine and methionine residues in the chromatin architecture. Nuclear-
produced H2O2 differently affected H3 PTMs according to the type of modification observed,
concentration of D-Alanine and time after treatment. H2O2 promoted cell proliferation and
shortened cell cycle.
Conclusions:
Nuclear generated H2O2 seems to have effects in the regulation of chromatin organization and
epigenetic markers. Redox changes in the nucleus possibly have a role on key pathways that
regulate cell cycle and proliferation.

Research Day 2019
Jump to Table of Contents 137
Basic Science
Poster #
119
Abstract Title:
Effect of ROS in the mitochondrial metabolic changes that promote macrophage polarization
Presenter(s):
Veronica Paviani
Authors:
Veronica Paviani, Diego R. Coelho, Flavio R. Palma, Benjamin N. Gantner and Marcelo G. Bonini.
Dept/Division:
Medicine: Endocrinology
Category:
Postdoctoral Fellow
Introductions:
Macrophages are innate immune cells capable of assuming different phenotypes that can either
activate (referred as M1) or resolve (referred as M2) inflammation. Inflammatory M1
macrophages have been reported to display glycolytic metabolism while M2 macrophages show
vigorous respiratory activity. Though the central idea in the field is that the mode of metabolism
shapes the kind of inflammatory response macrophages mount, little is known about the
molecular mechanisms involved. Our laboratory hypothesized that reactive oxygen species (ROS)
and not a specific form of metabolism regulates macrophage polarization due to their capacity to
activate multiple redox sensitive pathways rapidly and simultaneously. Hence, our main goal was
to determine if mitochondrial reactive oxygen species (ROS) regulate inflammatory gene
expression in LPS-activated macrophages.
Methods:
Firstly, bone marrow derivate macrophages (BMDM) were pre-incubated or not with some
mitochondria scavengers (EUK-8, EUK-134 and Mito-Q) and activated with LPS (100 ng/mL) in
different time points. The proinflammatory and anti-inflammatory cytokines were analyzed by
qPCR. The redox state of the mitochondria was monitored by confocal fluorescence using BMDM
from mice that express the H2O2 sensor: Mito-orp-roGFP. And the effect of ROS in the
metabolism was performed by Seahorse using Mito stress and ATP rate assays
Results:
Our results show that LPS increases the expression of M1-type proinflammatory factors including
IL1□, IL6, NOS2, INFΒ, TNFα and IL12. Some of these cytokines showed a decrease of expression
when the macrophages were pre-incubated with mitochondrial ROS scavengers such as EUK134.
Confocal microscopy imaging of the mitochondrial ROS sensor (Mito-Orp1-roGFP2) confirmed the
production of mitochondrial H2O2 when the macrophages were activated by LPS. Extracellular
flow analysis (Seahorse) showed that although BMDM macrophages display glycolytic metabolism
when activated with LPS, EUK134 promotes aerobic respiration and reduces glycolysis.
Conclusions:
Taken together, the data suggest mitochondrial ROS direct the expression of a subset of
inflammatory genes and indicate that there are ROS-regulated and ROS-independent sets of
genes that control macrophage polarization.
Reference 1:
Chao He and A Brent Carter. The Metabolic Prospective and Redox Regulation of Macrophage
Polarization. J Clin Cell Immunol. Vol. 6(6), 2015
Reference 2:
Kent Langston, Munehiko Shibata and Tiffany Horng. Metabolism Supports Macrophage
Activation. Frontiers in Immunology. Vol. 8 (61), 2017
Reference 3:
Mirza Saqib Baig, Sofia V. Zaichick, Mao Mao,Andre L. de Abreu, Farnaz R. Bakhshi, Peter C. Hart,
Uzma Saqib, Jing Deng, Saurabh Chatterjee, Michelle L. Block, Stephen M. Vogel, Asrar B. Malik,
Marcia E.L. Consolaro, John W. Christman, Richard D. Minshall, Benjamin N. Gantner, and Marcelo
G. Bonini. NOS1-derived nitric oxide promotes NF-kB transcriptional activity through inhibition of
suppressor of cytokine signaling-1. J. Exp. Med. 2015 Vol. 212 (10), 2015
Research Day 2019
Jump to Table of Contents 138
Basic Science
Poster #
120
Abstract Title:
Role of endothelial YAP1/TAZ signaling in lung regeneration
Presenter(s):
Kathryn Hendee
Authors:
Kathryn Hendee, Megan Muyleart, Akiko Mammoto, and Tadanori Mammoto
Dept/Division:
Pediatrics
Category:
Postdoctoral Fellow
Introductions:
Angiogenesis, the formation of new blood capillaries, plays a key role in organ development,
homeostasis and regeneration. We have reported that angiogenesis is stimulated during
regenerative lung growth after unilateral pneumonectomy (PNX). In addition to chemical factors,
mechanical forces play important roles in endothelial cell (EC) growth and differentiation. It is
known that mechanical forces change during regenerative lung growth after PNX. The
mechanosensitive transcriptional co-activators, Yes-associated protein (YAP1) and transcriptional
co-activator with PDZ-binding motif (TAZ), control angiogenesis.
However, the mechanosensitive mechanism by which endothelial YAP1/TAZ signaling controls
angiogenesis during regenerative lung growth remains unclear.
Methods:
We use a unilateral PNX model and VE-cadherin-specific Yap1 knockout mice to characterize the
role of endothelial YAP1 in angiogenesis and regenerative lung growth. To examine the effects of
mechanical forces changed after PNX, we use silicone prosthesis insertion and one lobar
pulmonary artery ligation in combination with PNX.
Results:
Knockdown of endothelial YAP1 suppresses compensatory lung growth after unilateral PNX in
adult mice. Parenchyma deformation due to expansion of the remaining lobes and increases in
alveolar microvascular perfusion of the remaining lobes after PNX play key roles in the post-PNX
lung growth. Insertion of silicone prosthesis to replace an excised lobe prevents post-PNX lung
growth and decreases YAP1/TAZ expression. Ligation of one lobar pulmonary artery after PNX
stimulates compensatory growth of the remaining non-occluded lung lobes. To analyze the effects
of endothelial YAP1 on angiogenesis and epithelial morphogenesis during regenerative lung
growth, we implanted fibrin gel on the mouse lung after PNX and found that knockdown of
endothelial YAP1 inhibits angiogenesis and alveolar epithelial cell recruitment into hydrogel
implanted on the mouse lung.
Conclusions:
These results suggest that changes in mechanical forces after PNX contribute to regenerative lung
growth through endothelial YAP1/TAZ signaling and modulation of endothelial YAP1/TAZ could be
novel interventions for the improvement of the strategies for lung regeneration.

Research Day 2019
Jump to Table of Contents 139
Basic Science
Poster #
121
Abstract Title:
Effects of age-dependent changes in cell size on endothelial cell growth through YAP1
Presenter(s):
Megan Muyleart
Authors:
Megan Muyleart, Kathryn Hendee, Tadanori Mammoto, and Akiko Mammoto
Dept/Division:
Pediatrics
Category:
Research Support Staff
Introductions:
The aging population is rapidly growing. Aging is associated with impaired angiogenesis -the
growth of new blood capillaries- and contributes to the increased susceptibility to various
diseases. Thus, in order to develop more efficient therapies for aging-associated diseases, we
need to understand the mechanisms by which aging impairs angiogenesis. In addition to soluble
angiogenic factors, biophysical factors such as changes in cell size and geometry control
endothelial cell (EC) growth and differentiation. A Hippo signaling transducer, Yes-associated
protein (YAP1), acts as a mechanosensitive transcriptional co-activator and controls angiogenesis
and organ regeneration.
Methods:
We use silver nitrate staining and immunocytochemical analysis to measure the EC size in blood
vessels ex vivo and in vitro. To directly examine the effects of cell size on YAP1 activity and EC
proliferation and senescence, we use the microcontact printing system and culture young vs. aged
ECs on each island.
Results:
We have found that pulmonary artery ECs in aged mice are significantly larger than those in young
mice. Aged human adipose tissue ECs are also larger than those in young adults. A major focal
adhesion protein, paxillin, distributes at the distal ends of actin stress fibers in young ECs, while
paxillin is localized along the actin fibers in the cytoplasm in aged ECs. The levels of YAP1 decrease
and EC senescence is induced in aged ECs. The activity of CDC42, which controls actin
cytoskeleton structures, is also higher in aged ECs compared to that in young ECs. To analyze
whether age-related changes in EC size control YAP1 activity and EC senescence, we cultured ECs
on the microcontact-printed substrates consisting of square fibronectin-coated single-cell sized
islands. When we culture aged human adipose ECs on large islands of size comparable to aged EC,
YAP1 is excluded from the nucleus and EC proliferation is attenuated. Reduction of the aged EC
size by culturing on smaller islands restores YAP1 nuclear localization, decreases Cdc42 activity,
and inhibits EC senescence. Stimulation of YAP1 or inhibition of Cdc42 activity in aged ECs also
restores blood vessel formation. These results suggest that age-dependent increases in EC size
stimulate aged EC senescence through CDC42-YAP1 signaling.
Conclusions:
Modulation of EC size and/or Cdc42 and YAP1 activity will reverse age-related decline in
angiogenesis and will lead to the development of promising strategies for age-dependent
diseases.

Research Day 2019
Jump to Table of Contents 140
Basic Science
Poster #
122
Abstract Title:
Growth Phase and Osmotic Stress Drive Subcellular Localization of Enterococcus faecalis
OGIRF_11271, a Conserved Protein Involved in Cell Envelope Integrity
Presenter(s):
Kevin Jennings
Authors:
Kevin Jennings, Ismael Banla, Christopher Kristich, Nita Salzman
Dept/Division:
Pediatrics, Microbiology/Immunology
Category:
Student
Introductions:
Enterococcus faecalis (EF) is a Gram-positive commensal that acts opportunistically in
immunocompromised hosts and contributes to nosocomial infections. EF readily colonizes the GI
tract and is intrinsically resistant to broad-spectrum cephalosporins. IreK is a transmembrane
kinase that promotes cell envelope integrity in EF. Deletion of ireK in EF impairs antimicrobial
resistance, cell envelope integrity, and intestinal colonization. We previously described two
proteins [OG1RF_11271 (271) and OG1RF_11272 (272)] that act antagonistically to IreK. The 271-
272 protein pair is conserved among all enterococci, yet their functions remain unknown. 271
and 272’s detrimental actions on cell envelope integrity are only apparent in IreK-deficient
mutants but the mechanism by which IreK suppresses the activity of these two proteins is
unknown.
Methods:
To investigate the function and regulation of 271 and 272, we determined their cellular
localization by fractionation. Cell lysates of wild-type, delta-ï„ireK, delta-ï„271, and delta-ï„272
were separated into membrane and cytoplasmic cellular fractions by ultracentrifugation. Purified
fractions were analyzed via western blot and band intensities for 271 and 272 were quantified via
the LiCor Odyssey system and software.
Results:
We found that, while 272 remains cytoplasmic under all conditions tested, 271 localizes
predominantly to the cytoplasm during exponential phase, but redistributes to the membrane
during stationary phase. This shift in localization during the growth phase transition was not
dependent on the presence or absence of IreK or 272. Interestingly, when EF cells are suspended
in water for 24 hours (simulating osmotic stress), 271 evenly distributes between cytoplasm and
membrane in the wild-type strain but localizes exclusively to the cytoplasm in the ireK deficient
strain.
Conclusions:
Since 271 localization during normal growth is not impacted by ireK deletion, we can conclude
that IreK is not responsible for regulating 271’s localization under these circumstances. However,
the fact that IreK is important for proper 271 localization under osmotic stress suggests some
level of regulation. Presumably, ireK mutants would suffer greater deficits when hypertonic to
their surroundings. Suspending these mutants in water may drive physiological changes that
subsequently alter the regulation of 271 localization. Regardless, these data suggest that osmotic
stress may be an important condition for studying the roles of IreK, 271 and 272 in EF. Defining
the molecular mechanisms of 271/272 regulation will contribute to a better understanding EF cell
envelope biology and may provide novel therapeutic targets for controlling antibiotic resistant EF
infections.

Research Day 2019
Jump to Table of Contents 141
Basic Science
Poster #
123
Abstract Title:
Insights of the role of FOXC1 gene in ocular development using a double foxc1a/foxc1b knockout
zebrafish line
Presenter(s):
Jesus J Ferre-Fernandez
Authors:
Jesus J Ferre-Fernandez, Elena Sorokina, Sanaa Muheisen, Samuel Thompson, Elena V Semina.
Dept/Division:
Pediatrics: Developmental Biology
Category:
Postdoctoral Fellow
Introductions:
The gene forkhead box C1 (FOXC1) encodes a forkhead/winged helix transcription factor involved
in embryonic development. Mutations in FOXC1 cause developmental eye disorders like Axenfeld-
Rieger syndrome type 3 or anterior segment dysgenesis, usually following an autosomal dominant
inheritance pattern. Some patients also present other non-ocular defects like cardiac and
craniofacial abnormalities. There are two zebrafish orthologous genes, foxc1a and foxc1b. Both
zebrafish genes demonstrate evolutionary conservation with the human ortholog, especially in
the forkhead and activation domains. The lack of foxc1a in zebrafish produces defects in
somitogenesis, heart and craniofacial region. In this study we use the zebrafish as an animal
model to further study the role of FOXC1 in the eye development.
Methods:
Using CRISPRs we generated single foxc1a and foxc1b knockout zebrafish lines, carrying p.[D71*]
and p.[A86Dfs*30] alleles correspondingly, and used them to obtain foxc1a/foxc1b double
knockout embryos (D-KO). Both foxc1 mutations are predicted to produce complete loss-of-
function alleles because of an early truncation affecting the forkhead and C-terminal domains.
Results:
foxc1a-/- homozygous embryos showed anomalies in blood flow, microphthalmia and periocular
edema, as well as embryonic lethality, while heterozygous foxc1a+/- and heterozygous or
homozygous foxc1b embryos did not display any visible phenotype and survived to adulthood. To
further evaluate foxc1a/b dosage requirements and to generate D-KO embryos, we raised adults
carrying heterozygous foxc1a and homozygous foxc1b alleles. The foxc1a+/-;foxc1b-/- fish
demonstrated reduced survival, craniofacial, skeletal and ocular defects, thus displaying a
dominant phenotype for the foxc1a mutation in foxc1b-deficient background and exposing a role
of foxc1b in the development/maintenance of the affected structures. Embryos with deficiency
for a single (foxc1a) or both (foxc1 D-KO) genes were examined by histology and showed similar
ocular defects; also, analysis of eye vasculature was performed using Tg(fli1a-GFP)/foxc1a+/-
animals and showed severe abnormalities. To identify downstream effects of foxc1 deficiency, D-
KO eye samples were collected at different developmental stages, RNAseq was performed and
results will be presented.
Conclusions:
Our data show that foxc1 is necessary for the proper eye development in zebrafish and that the
developed zebrafish lines serve as a suitable model for FOXC1-related human ocular disease.
Research Day 2019
Jump to Table of Contents 142
Basic Science
Poster #
124
Abstract Title:
Succinate acts through tuft cells to stimulate Paneth cell secretion
Presenter(s):
Lisa Fraser
Authors:
Lisa Fraser, Joseph Rouse, Michael Hayward, Jennifer Ziegelbauer, Nita Salzman
Dept/Division:
Pediatrics: Gastroenterology
Category:
Postdoctoral Fellow
Introductions:
The intestinal epithelium is a single cell layer that is involved in nutrient absorption as well as
protection. In addition to providing a physical barrier, specialized cell types such as tuft cells and
Paneth cells detect and respond to the external environment by secreting a variety of products.
Succinate is a metabolite of both the tricarboxylic acid cycle and microbial propionate synthesis,
and is detected by tuft cells. Succinate detection by tuft cells results in a type 2 immune response
via Il-13 production from type 2 innate lymphoid cells (ILC2s). Il-13 has also been shown to lead to
Paneth cell degranulation and release of antimicrobial peptides like lysozyme, suggesting that the
tuft cell - ILC2 circuit may play a role in AMP secretion from Paneth cells.
Methods:
Axenic or conventionally colonized male C57BL/6J mice were given ad libitum access to water
either untreated of containing 100mM disodium succinate for seven days. On day 7, mice were
euthanized, and the distal small intestinal tissues and luminal contents were collected for RNA
and protein isolation. As a positive control for Paneth cell secretion, mice were injected with
carbachol (axenic, 5ug; conventionally colonized, 10ug) and euthanized after 10 minutes, tissues
and contents were collected as above. Lysozyme abundance and secretion was assessed by
western blot of distal small intestinal tissues and luminal contents. Tuft cell abundance was
assessed by detection of DCLK1 transcript using quantitative RT-PCR.
Results:
Addition of 100mM succinate in drinking water was sufficient to stimulate an increase in lysozyme
secretion in small intestine of both axenic and conventionally colonized mice when compared to
untreated mice. Conversely, lysozyme abundance was decreased in distal small intestinal tissues
of succinate treated animals. Treatment with dietary succinate led to an increase in DCLK1
transcript compared to untreated animals, which is indicative of an increase in tuft cell numbers.
Conclusions:
We demonstrated that administration of succinate resulted in an increase in lysozyme secretion
in the small intestine of mice. Since the receptor for succinate is specifically expressed in tuft cells,
this work indicates that lysozyme secretion in response to succinate occurs through a tuft cell -
Paneth cell circuit. These findings suggest a novel mechanism for the sensing of microbial
products in the gut, thus driving an epithelial antimicrobial host response. Further studies are
needed to identify and characterize the mechanisms involved in this interaction.

Research Day 2019
Jump to Table of Contents 143
Basic Science
Poster #
125
Abstract Title:
SMA-Like Phenotype in a Mouse Model of Acid Ceramidase Deficiency
Presenter(s):
Murtaza S Nagree
Authors:
Murtaza S Nagree, Carissa Ahrenhoerster, Matthew D. Budde, and Jeffrey A Medin
Dept/Division:
Pediatrics: Hem/Onc
Category:
Student
Introductions:
Acid ceramidase (ACDase) is a lysosomal enzyme that catabolizes the sphingolipid ceramide.
ACDase deficiency leads to Farber disease (FD; OMIM#228000), in which ceramide accumulates in
numerous tissues. ACDase deficiency can also lead to a different disorder, Spinal Muscular
Atrophy with Progressive Myoclonic Epilepsy (SMA-PME; OMIM#159950). SMA-PME patients
experience a loss of spinal motor neurons resulting in progressive loss of muscle function and
muscular atrophy. This may be followed by the onset of myoclonic seizures that increase in
frequency. SMA-PME patients eventually succumb to respiratory insufficiency. While a few mouse
models of ACDase-deficiency exist, there have been no reports of these mice having a SMA-PME-
like phenotype.
Methods:
Our lab previously “˜knocked-in’ a mutation associated with FD, p.P361>R, into mice. These mice
display a phenotype that mimics FD presentation in patients, including hepatosplenomegaly. An
additional two mouse lines were generated for these present studies. The first features an
ACDase mutation, p.T41>A, previously reported in a patient with mild SMA, introduced into
C57BL/6J mice using Cas9-sgRNA. The second, referred to as attenuated p.P361>R, was generated
by removing an incidental transgenic element from the parent line, followed by 9 generations of
backcrossing to C57BL/6J. Both lines of mice were bred as heterozygotes. Sphingolipids were
measured using mass spectrometry. Histological staining was done on representative serial
sections of fixed and paraffin embedded tissues as indicated, and conclusions verified by a
pathologist. Molecular biology assays were conducted using standard methods.
Results:
Mice homozygous for the p.T41>A mutation were followed up to 21 months of age with no gross
physical or behavioral abnormalities noted. No significant accumulation of ceramide was
measurable by mass spectrometry or identified by EM. Conversely, the FD-like phenotype in
homozygous p.P361>R mice, following backcrossing into C57BL/6J, was attenuated compared to
the parent strain. Attenuated p.P361>R mice live longer than the parent line, and display a later-
onset of phenotype with progressive loss of hind limb function. This lower-limb dysfunction is
typified by hind limb atrophy, kyphosis, persistent tremor, and urinary incontinence - this
phenotype is more reminiscent of SMA than FD. These mice also displayed multiple large
vacuolated lesions in their spinal cords with dramatically reduced myelin staining. We did not find
gross changes in brain cortex nor cerebellum, or observe Purkinje cell loss, however, although
small regions in the arbor vitae appeared to have reduced myelin.
Conclusions:
The p.T41>A mutation in ACDase that leads to SMA in humans appears to have no effect in mice.
Conversely, the p.P361>R mutation in ACDase capable of causing FD in humans can lead to both
Farber-like and SMA-like phenotypes in mice, highlighting strain differences and/or a discrepancy
between human and mouse ACDase. SMA-like phenotypes in homozygous p.P361>R mice appear
to be a result of spinal cord lesions that likely perturb the function of affected neurons, similar to
that described in SMA-PME patients. We plan to study the pattern of occurrence of spinal cord
lesions using MRI, then characterize them by histopathology. Our mice are a valuable model to
study mechanisms of, and test treatment for, ACDase deficiency-related SMA.
Acknowledgements:
CHW Histology and Imaging Cores, WashU Metabolomics Core, Geurts Lab

Research Day 2019
Jump to Table of Contents 144
Basic Science
Poster #
126
Abstract Title:
Administration of pegylated-human growth factors (PEG-HGF) and lisinopril for mitigation of
acute radiation syndrome
Presenter(s):
Tessa Miller
Authors:
Tessa Miller, Tracy Gasperetti, Jayashree Narayanan, Elizabeth R. Jacobs, George N. Cox, Christie
M. Orschell, Brian Fish, Meetha Medhora
Dept/Division:
Radiation Oncology
Category:
Research Support Staff
Introductions:
People will be exposed to radiation in the event of a nuclear attack, radiological accident, or in
preparation for bone marrow transplantation. Depending on the dose, severe early damage
occurs within the bone marrow. Without transplantation or intervention, individuals will develop
Acute Radiation Syndrome (ARS) resulting in a fatal hematopoietic injury. We have developed a
total body irradiation (TBI) model in rats to test medical countermeasures for ARS including
hematopoietic response and the delayed effects of acute radiation exposure (DEARE). PEG-HGF is
a combination of the pegylated-hematopoietic growth factors G-CSF, GM-CSF, and IL11. Growth
factors are used in the clinic to aid recovery of white blood cells after radio- or chemo-therapy.
PEG-HGF works by stimulating production of bone marrow hematopoietic progenitors, the
precursors of all blood elements. Lisinopril and captopril are angiotensin-converting enzyme (ACE)
inhibitors and are used to treat hypertension and vascular dysfunction. In mice, captopril
improves red blood cell recovery after TBI. Our previous research has found that lisinopril is an
effective mitigator of DEARE in a rat model. While pegylated hematopoietic growth factors (PEG-
HGF) or captopril have been shown to mitigate ARS after radiation in mice, the agents were not
effective in rats.
Aim: To mitigate ARS in a rat model by combining PEG-HGF and lisinopril.
Methods:
30 rats were irradiated with 7.5 Gy TBI and randomized into 5 groups (6 rats/group): 1) control 2)
vehicle 3) PEG-HGF 4) lisinopril + vehicle and 5) PEG-HGF + lisinopril. PEG-HGF (2.75 mL/kg) and
the vehicle were administered 24 hours post-irradiation via subcutaneous injection, and lisinopril
(24mg/m^2/day) was given in drinking water starting 7 days after radiation. Blood was harvested
for blood counts at days 10, 18, 25, and on termination at 30 days post-irradiation. The brain,
sternum, and femurs were harvested for histology and cell counts.
Results:
PEG-HGF or lisinopril alone did not enhance survival after TBI. Lisinopril and PEG-HGF in
combination effectively mitigated ARS compared to the vehicle alone (p=0.01). Analysis of blood
and bone marrow cells and histology are ongoing to investigate the mechanism of mitigation by
the combined therapy.
Conclusions:
Combining two classes of drugs, hematopoietic growth factors and ACE inhibitors, led to
enhanced survival of rats through ARS. These results suggest synergistic mechanisms of action for
each drug type.
Acknowledgements:
Grants: NIAID U01AI107305 and R01AI101898

Research Day 2019
Jump to Table of Contents 145
Basic Science
Poster #
127
Abstract Title:
Advancing a rat model of leg-out partial-body irradiation for testing mitigators of ARS and DEARE
under the FDA Animal Rule
Presenter(s):
Tracy Gasperetti
Authors:
Tracy Gasperetti, Brian L. Fish, Abdul Parchur, Jayashree Narayanan, Dana Scholler, Amit Joshi,
Thomas J. MacVittie, Barry Hart, Meetha Medhora
Dept/Division:
Radiation Oncology
Category:
Research Support Staff
Introductions:
After a radiological or terrorist attack, victims will experience various degrees of acute radiation
syndrome (ARS) and delayed effects of acute radiation exposure (DEARE) depending on the dose
and volume of body irradiated. We developed a model to mimic a large single dose of radiation
with partial-body shielding and simple supportive care in rats maintained on a high antioxidant
diet (Teklad 8604: isoflavones 350-650 mg/kg). This model demonstrated survival of ARS injuries
to the gastro-intestinal tract (GI) and hematopoietic system to permit investigation of DEARE,
lung, heart and kidney injuries.
Methods:
Two weeks prior to irradiation, adult male and female WAG/RijCmcr rats were placed on a Teklad
2018 diet containing 150-250 mg/kg isoflavones. Rats received 13 Gy leg-out partial-body
irradiation (leg-out PBI) at 12 weeks of age with 5-8% bone marrow sparing or were maintained as
unirradiated controls. All rats received supportive care consisting of antibiotics (days 2-21) and
subcutaneous hydration (d2-10) to mitigate acute gastrointestinal morbidity. ARS endpoints
included morbidity to d30, total blood counts (d1-d42), and body weight. DEARE endpoints
included breathing rates (d28-84), weekly computed tomography (CT) of the thorax (d28-d84) to
identify pneumonitis, blood urea nitrogen (BUN) levels after d90 to identify nephropathy and
morbidity to d120.
Results:
After 13 Gy leg-out PBI, the neutrophil count reached a nadir between 6-10 days post irradiation
and returned to normal levels by 15 days. Female rats decreased in body weight during ARS-GI
and started to gain weight 10 days after irradiation. A second decrease in body weight occurred at
7 weeks post irradiation during pneumonitis. The time course of breathing intervals, CT, BUN
levels and survival are being evaluated.
Conclusions:
We are optimizing our rat model of high dose (13 Gy) leg-out partial-body irradiation which
exhibits multiple sequelae including ARS and DEARE, to be used for testing countermeasures
under the FDA Animal Rule.
Acknowledgements:
HHSN272201800012C (BH), U01AI133594 (MM) and the Dept. of Radiation Oncology, MCW.

Research Day 2019
Jump to Table of Contents 146
Basic Science
Poster #
128
Abstract Title:
A Framework of Automatic Contour Quality Validation for MRI-Guided Online Adaptive Radiation
Therapy
Presenter(s):
Ying Zhang
Authors:
Ying Zhang, Frank Ceballos, Ergun Ahunbay, X. Allen Li
Dept/Division:
Radiation Oncology
Category:
Clinical Fellows & Residents
Introductions:
Rapid and accurate segmentation is essential for online adaptive radiation therapy (OART). This
study aims to develop a framework to automatically evaluate contour quality using quantitative
MRI texture and shape features for MRI-guided OART.
Methods:
The framework includes: (1) pre-processing images, (2) extracting texture and shape features on a
slice-by-slice basis in the contours to be checked and feature changes between 4-mm inner/outer
shells and a core region, (3) ranking all the features using a recursive feature elimination method
and selecting top-ranked features, and (4) building and testing supervised classification models
for contour validation. A variety of contours of the pancreatic-head generated on 22 sets of T1-
weighted non-contrast MRIs of 11 patients was utilized to demonstrate the framework. Three sets
of contours were created: (1) ground truth, (2) auto-generated contour using deformable image
registration, and (3) modified contour from that in (2). The contour on a slice from set #2 or 3 was
labeled as accurate if Dice similarity coefficient ‰¥ 0.85, mean distance to agreement ‰¤1.5
mm, and 95% of distance to agreement ‰¤ 5 mm, as compared to the ground truth. A total of
754 accurate and 650 inaccurate contour slices were used, where 80% of these contour slices
were used for the model training and 20% for testing.
Results:
A total of 132 features were extracted from each slice and ranked. The top-ranked 30 features
were selected for model building where 12 different classification models were trained and
compared. The best performing model yielded average sensitivity of 91% and specificity of 89%
on the testing data after 5-fold cross-validation.
Conclusions:
The newly-developed framework can automatically identify accurate and inaccurate contours on
a slice-by-slice basis on MRI with high sensitivity and specificity, thus, can be implemented for
quick contour check in MRI-guided OART.

MCW Research Overview
Jump to Table of Contents 147
MCW Research Overview: Funding
Research Grant Awards Over $1M: August 2018 – July 2019
Principal Investigator
Project
Sponsor
Total*
Brian Volkman, PhD
800 MHz NMR Spectrometer for Southeast
Wisconsin
National Institutes of Health:
Office of the Director
$2.0M
Melinda Dwinell
Hybrid Rat Diversity Program
NIH Office of the Director (R24)
$3.1M
Amy Drendel, DO
The Effect of Emergency Department and
After-Emergency Department Analgesic
Treatment on Pediatric Long Bone
Fracture Outcomes
National Institute on Minority
Health and Health Disparities
$2.9M
Leonard Egede, MD
Rebekah Walker, PhD
Lowering the Impact of Food insecurity in
African American Adults with Type 2
Diabetes Mellitus (LIFT-DM)
National Institute on Minority
Health and Health Disparities
$3.2M
Qing-Song Liu, PhD
Mechanistic studies of cAMP effectors in
cocaine addiction
National Institute on Drug Abuse
$1.8M
Jeffrey Binder, MD
Concept Representation in the Human
Brain
National Institute on Deafness
and other Communication
Disorders
$3.0M
Matthew Budde, PhD
Noninvasive Spinal Cord Perfusion
Techniques with MRI
National Institute of
Neurological Disorders and
Stroke
$1.7M
Cheryl Stucky, PhD
Nociceptive Mechanisms Underlying Sickle
Cell Pain
National Institute Of
Neurological Disorders and
Stroke
$3.0M
Lindsay Nelson, PhD
Improving Patient Classification and
Outcome Measurement in Traumatic Brain
Injury (TBI)
National Institute of
Neurological Disorders and
Stroke
$3.0M
Michael McCrea, MD
Yang Wang, MD
Effects of Head Impact Exposure During
Contact Sport on Middle School and High
School Athletes
National Institute of
Neurological Disorders and
Stroke
$2.9M
Laura Glasman, PhD
Regular HIV Testing and HIV Prevention
Among At-Risk Latino Men in the
Heartland
National Institute of Mental
Health
$2.7M
Sang Lee, PhD
Molecular Mechanisms of GABAergic
Synapse Modulation by TAFA
National Institute of Mental
Health
$1.9M

MCW Research Overview
Jump to Table of Contents 148
Principal Investigator
Project
Sponsor
Total*
Adriano Marchese, PhD
Role of beta-arrestins in chemokine
receptor signaling
National Institute of General
Medical Sciences
$1.3M
Blake Hill, PhD
Fis1 Regulation of Mitochondrial Fission
National Institute of General
Medical Sciences
$1.4M
Brian Smith, PhD
Discovering and Exploiting Selectivity
within Tandem Bromodomains
National Institute of General
Medical Sciences
$1.9M
John McCorvy, PhD
Molecular Mechanisms of G protein-
coupled Receptor Biased Signaling
National Institute of General
Medical Sciences
$1.9M
Xiaowen Bai, MD, PhD
IncRNAs and Anesthetic-Induced
Developmental Neurotoxicity
National Institute of General
Medical Sciences
$1.3M
Marcelo Bonini, PhD
Environmental Arsenic in the Subtype
Specification of Breast Cancer
National Institute of
Environmental Health Sciences
$1.8M
Brian Smith, PhD
Biochemical mechanisms of beta cell
protection through bromodomain
inhibition
National Institute of Diabetes
and Digestive and Kidney
Diseases
$1.9M
John Corbett, PhD
Biochemical Mechanism of Beta-Cell
Destruction
National Institute of Diabetes
and Digestive and Kidney
Diseases
$1.2M
Jyoti Sengupta, PhD
Banani Banerjee, PhD
Patrick Sanvanson, MD
Neuromolecular Mechanisms of Chronic
Pelvic Pain in Neonatally-induced Cystitis
National Institute of Diabetes
and Digestive and Kidney
Diseases
$2.4M
Leonard Egede, MD
HOME DM-BAT: Home-based Diabetes-
Modified Behavioral Activation Treatment
for Low Income Seniors with T2DM
National Institute of Diabetes
and Digestive and Kidney
Diseases
$3.3M
Leonard Egede, MD
Financial Incentives And Nurse Coaching
to Enhance Diabetes Outcomes - FINANCE-
DM
National Institute of Diabetes
and Digestive and Kidney
Diseases
$3.3M
Christopher Kristich, PhD
Intrinsic cephalosporin resistance in
enterococci
National Institute of Allergy and
Infectious Diseases
$1.5M
Melinda Dwinell, PhD
Mary Shimoyama, PhD
Dissemination and Coordinating Center for
the SCGE Consortium
National Human Genome
Research Institute
$15.0M

MCW Research Overview
Jump to Table of Contents 149
Principal Investigator
Project
Sponsor
Total*
Akiko Mammoto, PhD
Tadanori Mammoto, MD,
PhD
Role of endothelial Twist1 in vascular
remodeling in pulmonary hypertension
National Heart, Lung, and Blood
Institute
$1.2M
Curt Sigmund, PhD
PPARG-dependent Mechanisms Control
Endothelial-Smooth Muscle Coordination,
Arterial Pressure, Vasomotor Function and
Arterial Stiffness
National Heart, Lung, and Blood
Institute
$6.5M
Girija Konduri, MD
Liver Kinase B1 signaling in persistent
pulmonary hypertension of the newborn
National Heart, Lung, and Blood
Institute
$1.6M
Mary Shimoyama, PhD
Rat Genome Database, Years 20 – 23
National Heart, Lung, and Blood
Institute
$8.6M
Roy Silverstein, MD
ERK5 and CD36 link oxidative stress to
platelet dysfunction and ischemic injury
National Heart, Lung, and Blood
Institute
$2.5M
Amanda Brandow, DO
Investigating the role of the microbiome
and inflammation in acute and chronic
pain in patients with sickle cell disease
National Heart, Lung and Blood
Institute
$3.7M
Andrey Sorokin, PhD
Role of p66Shc in Regulation of
Microvascular Reactivity of Renal Blood
Vessels
National Heart, Lung and Blood
Institute
$1.6M
Caitlin O’Meara, PhD
IL13 - A Novel Therapeutic Factor for
Cardiac Regeneration
National Heart, Lung and Blood
Institute
$1.9M
Carmen Bergom, MD
Genetic Modifiers of Radiation Therapy-
Induced Cardiotoxicity
National Heart, Lung and Blood
Institute
$2.3M
Curt Sigmund, PhD
Genetic and Signaling Mechanisms in the
Central Regulation of Blood
National Heart, Lung and Blood
Institute
$7.4M
David Brousseau, MD
Julie Panepinto, MD, MSPH
Implementation of evidence-based care
for the acute treatment of sickle cell
disease pain
National Heart, Lung and Blood
Institute
$1.1M
Michael Widlansky, MD
Impact of L. plantarum 299v
Supplementation on Endothelial Function
and Systemic Inflammation
National Heart, Lung and Blood
Institute
$2.9M
Nicole Lohr, MD
Small molecule NO precursors as a
bioactive source of NO in vasodilation and
angiogenesis
National Heart, Lung and Blood
Institute
$2.2M
Parameswaran Hari, MD
Shawn Jobe, MD
David Allen Wilcox, PhD
A Phase I Clinical Trial Testing Feasibility of
Hematopoietic Stem Cell Gene Therapy
Using Platelet Factor VIII to Safely Improve
Hemostasis for Severe Hemophilia A with
Inhibitory Antibodies
National Heart, Lung and Blood
Institute
$8.2M

MCW Research Overview
Jump to Table of Contents 150
Principal Investigator
Project
Sponsor
Total*
Qizhen Shi, MD, PhD
Platelet-derived FVIII Gene Therapy of
Hemophilia A
National Heart, Lung and Blood
Institute
$2.0M
Tadanori Mammoto, MD,
PhD
Akiko Mammoto, MD, PHD
The role of YAP1 in angiogenesis during
organ regeneration
National Heart, Lung and Blood
Institute
$1.5M
William Drobyski, MD
Inflammatory Cytokine Networks in
Gastrointestinal Tract Graft Versus Host
Disease
National Heart, Lung and Blood
Institute
$2.0M
Daniel Lipinski, DPHIL
Vascular Gene Delivery and Early Disease
Biomarkers in Diabetic Retinopathy
National Eye Institute
$1.8M
Iris Kassem, MD, PhD
Diagnosis and Predictive Value of the
Ocular Manifestations of Fabry Disease
National Eye Institute
$2.7M
Joseph Besharse, PhD
Brian Link, PhD
RPE Signaling in Ocular Health and Disease
National Eye Institute
$1.8M
Joseph Carroll, PhD
Developing Cone-Dominant Retinal
Disease Models as a Resource for
Translational Vision Research
National Eye Institute
$6.3M
Michael Dwinell, PhD
Biased chemokine receptor signaling in
cancer progression
National Cancer Institute
$2.0M
Alan Nyitray, PhD
Determining the accuracy of self- and
partner anal exams for detecting anal
abnormalities
National Cancer Institute
$3.2M
Ann Nattinger, MD
Can regionalization improve outcomes
and reduce disparities related to breast
cancer care? An Evaluation of the NY
Medicaid regionalization experiment
National Cancer Institute
$1.1M
Balaraman Kalyanaraman,
PhD
Ming You, MD
Chemoprevention of lung cancer by
targeting lonidamine to mitochondria
National Cancer Institute
$1.9M
Marcelo Bonini, PhD
MnSOD Acetylation Promotes Cancer
Stem Cell Phenotypes in Breast Cancer
National Cancer Institute
$1.8M
Mary Horowitz, MD
Immuno-Oncology Translation Network
(IOTN): Cellular Immunotherapy Data
Resource (CIDR)
National Cancer Institute
$8.5M
Mary Horowitz, MD
A Data Resource for Analyzing Blood and
Marrow Transplants (CIBMTR)
National Cancer Institute
$17.7M
William H Bradley, MD
Timothy S Fenske, MD
Elizabeth M Gore, MD
James P Thomas, MD, PhD
Tina Yen, MD, MS
Stuart Wong, MD
MCW NCTN Lead Academic Participating
Site
National Cancer Institute
$4.2M

MCW Research Overview
Jump to Table of Contents 151
Principal Investigator
Project
Sponsor
Total*
John Baker, PhD
Defining the relationship between
simulated weightlessness and space
radiation on cardiovascular disease
NASA
$1.5M
Julie Raaum, DNP
ANE Nurse Practitioner Residency
Program
Health Resources and Services
Administration
$1.7M
Matthew Durand, PhD
Allison Hyngstrom, PhD
Ischemic Conditioning and Improved
Motor Function Post Stroke
Eunice Kennedy Shriver National
Institute of Child Health &
Human Development
$2.1M
Frank Pintar, PhD
Automated Vehicle Occupant Kinematics
Department of Transportation
$1.1M
Michael McCrea, PhD
Cumulative and persistent intermediate
effects of concussion and head impact
exposure in CARE Consortium Military
Service Academy members and NCAA
Athletes
Department of Defense
$4.0M
Danny Thomas, MD, MPH
Active Injury Management (AIM) after
Pediatric Concussion
Center for Disease Control
$2.2M
*Projected Cumulative Awards rounded to the nearest hundred-thousand

MCW Research Overview
Jump to Table of Contents 152
National Institutes of
Health
$89.8M
33%
Other Federal
Agencies
$31.3M
11%
MCW Institutional
Support in FY18
$74.3M
27%
Other External
Sponsors
$78.8M
29%
MCW Overall Research Funding FY19
July 1 2018 - June 30 2019
Source: Business Information "Grants Cube" as of 8/27/2019
Prepared by the Office of Research on 8/27/2019
$274.3M in Total Costs expended in Research, Teaching, Training and Related Purposes
in FY19 which lead to improve patient care and health outcomes.

MCW Research Overview
Jump to Table of Contents 154
MCW Research Overview: Publications
*As of August 16, 2019
Source: Science Citation Index and Social Sciences Citation Index
Top Quartile: The top tier journals list is comprised of journals that are in the top quartile of biomedical fields from the
most recent three editions of Journal Citation Reports and journals in niche areas suggested by MCW faculty for inclusion.
559
568
617
560
958
63.2%
919
61.8%
914
59.7%
1,163
67.5%
0
200
400
600
800
1,000
1,200
1,400
1,600
1,800
2,000
FY2015-2016 FY2016-2017 FY2017-2018 FY2018-2019*
MCW Total Annual Publications with Top Quartile Division
Publications not in top journals Publications in top quartile journals
1,517
1,487
1,531
1,723

MCW Research Overview
Jump to Table of Contents 155
High Impact Publications: FY19
The following articles were published in FY19 by MCW authors in a journal with a 2018 impact factor or 20 or
greater. (MCW authors’ names are in bold.)
1. Bell EH, Zhang PX, Fisher BJ, Macdonald DR, McElroy JP, Lesser GJ, Fleming J, Chakraborty AR, Liu ZY,
Becker AP, Fabian D, Aldape KD, Ashby LS, Werner-Wasik M, Walker EM, et al. Association of MGMT
Promoter Methylation Status With Survival Outcomes in Patients With High-Risk Glioma Treated With
Radiotherapy and Temozolomide An Analysis From the NRG Oncology/RTOG 0424 Trial. Jama Oncology.
2018;4(10):1405-1409.
2. Bentley AR, Sung YJ, Brown MR, Winkler TW, Kraja AT, Ntalla I, Schwander K, Chasman DI, Lim E, Deng X,
Guo XQ, Liu JM, Lu YC, Cheng CY, Sim X, et al. Multi-ancestry genome-wide gene-smoking interaction study
of 387,272 individuals identifies new loci associated with serum lipids. Nature Genetics. 2019;51(4):636-+.
3. Bergl PA. At Baseline. New England Journal of Medicine. 2019;380(19):1792-1793.
4. Bruner DW, Pugh SL, Lee WR, Hall WA, Dignam JJ, Low D, Swanson GP, Shah AB, Malone S, Michalski JM,
Dayes IS, Seaward SA, Nguyen PL, Pisansky TM, Chen Y, et al. Quality of Life in Patients With Low-Risk
Prostate Cancer Treated With Hypofractionated vs Conventional Radiotherapy A Phase 3 Randomized
Clinical Trial. Jama Oncology. 2019;5(5):664-670.
5. Burke MJ. Allogeneic Hematopoietic Cell Transplantation Provides No Benefit for Patients With
Hypodiploid Acute Lymphoblastic Leukemia. Journal of Clinical Oncology. 2019;37(10):763-+.
6. Comerota AJ, Kearon C, Gu CS, Julian JA, Goldhaber SZ, Kahn SR, Jaff MR, Razavi MK, Kindzelski AL, Bashir
R, Patel P, Sharafuddin M, Sichlau MJ, Saad WE, Assi Z, et al. Endovascular Thrombus Removal for Acute
Iliofemoral Deep Vein Thrombosis Analysis From a Stratified Multicenter Randomized Trial. Circulation.
2019;139(9):1162-1173.
7. Dignam JJ, Hamstra DA, Lepor H, Grignon D, Brereton H, Currey A, Rosenthal S, Zeitzer KL, Venkatesan VM,
Horwitz EM, Pisansky TM, Sandler HM. Time Interval to Biochemical Failure as a Surrogate End Point in
Locally Advanced Prostate Cancer: Analysis of Randomized Trial NRG/RTOG 9202. Journal of Clinical
Oncology. 2019;37(3):213-+.
8. Gao P, Xia JH, Sipeky C, Dong XM, Zhang Q, Yang YH, Zhang P, Cruz SP, Zhang K, Zhu J, Lee HM, Suleman S,
Giannareas N, Liu S, Tammela TLJ, et al. Biology and Clinical Implications of the 19q13 Aggressive Prostate
Cancer Susceptibility Locus. Cell. 2018;174(3):576-+.
9. Gerson JN, Handorf E, Villa D, Gerrie AS, Chapani P, Li S, Medeiros LJ, Wang MI, Cohen JB, Calzada O,
Churnetski MC, Hill BT, Sawalha Y, Hernandez-Ilizaliturri FJ, Kothari S, et al. Survival Outcomes of Younger
Patients With Mantle Cell Lymphoma Treated in the Rituximab Era. Journal of Clinical Oncology.
2019;37(6):471-+.
10. Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, Papp KA, Sofen H, Puig L, Foley P,
Ohtsuki M, Flack M, Geng ZQ, Gu YH, Valdes JM, et al. Efficacy and safety of risankizumab in moderate-to-
severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-
controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392(10148):650-661.

MCW Research Overview
Jump to Table of Contents 156
11. Hlubocky FJ, Sachs GA, Larson ER, Nimeiri HS, Cella D, Wroblewski KE, Ratain MJ, Peppercorn JM,
Daugherty CK. Do Patients With Advanced Cancer Have the Ability to Make Informed Decisions for
Participation in Phase I Clinical Trials? Journal of Clinical Oncology. 2018;36(24):2483-+.
12. Huang LH, Zinselmeyer BH, Chang CH, Saunders BT, Elvington A, Baba O, Broekelmann TJ, Qi LN, Rueve JS,
Swartz MA, Kim BS, Mecham RP, Wiig H, Thomas MJ, Sorci-Thomas MG, et al. Interleukin-17 Drives
Interstitial Entrapment of Tissue Lipoproteins in Experimental Psoriasis. Cell Metabolism. 2019;29(2):475-
+.
13. Hyams JS, Thomas SD, Gotman N, Haberman Y, Karns R, Schirmer M, Mo A, Mack DR, Boyle B, Griffiths
AM, LeLeiko NS, Sauer CG, Keljo DJ, Markowitz J, Baker SS, et al. Clinical and biological predictors of
response to standardised paediatric colitis therapy (PROTECT): a multicentre inception cohort study.
Lancet. 2019;393(10182):1708-1720.
14. Johansson LC, Stauch B, McCorvy JD, Han GW, Patel N, Huang XP, Batyuk A, Gati C, Slocum ST, Li CF,
Grandner JM, Hao SM, Olsen RHJ, Tribo AR, Zaare S, et al. XFEL structures of the human MT2 melatonin
receptor reveal the basis of subtype selectivity. Nature. 2019;569(7755):289-+.
15. Kanate AS, Kumar A, Dreger P, Dreyling M, Le Gouill S, Corradini P, Bredeson C, Fenske TS, Smith SM,
Sureda A, Moskowitz A, Friedberg JW, Inwards DJ, Herrera AF, Kharfan-Dabaja MA, et al. Maintenance
Therapies for Hodgkin and Non-HodgEn Lymphomas After Autologous Transplantation A Consensus
Project of ASBMT, CIBMTR, and the Lymphoma Working Party of EBMT. Jama Oncology. 2019;5(5):715-
722.
16. Lee J, Yesilkanal AE, Wynne JP, Frankenberger C, Liu J, Yan JL, Elbaz M, Rabe DC, Rustandy FD, Tiwari P,
Grossman EA, Hart PC, Kang C, Sanderson SM, Andrade J, et al. Effective breast cancer combination
therapy targeting BACH1 and mitochondrial metabolism. Nature. 2019;568(7751):254-+.
17. McGuire DK, Alexander JH, Johansen OE, Perkovic V, Rosenstock J, Cooper ME, Wanner C, Kahn SE, Toto
RD, Zinman B, Baanstra D, Pfarr E, Schnaidt S, Meinicke T, George JT, et al. Linagliptin Effects on Heart
Failure and Related Outcomes in Individuals With Type 2 Diabetes Mellitus at High Cardiovascular and
Renal Risk in CARMELINA. Circulation. 2019;139(3):351-361.
18. Moore K, Colombo N, Scambia G, Kim BG, Oaknin A, Friedlander M, Lisyanskaya A, Floquet A, Leary A,
Sonke GS, Gourley C, Banerjee S, Oza A, Gonzalez-Martin A, Aghajanian C, et al. Maintenance Olaparib in
Patients with Newly Diagnosed Advanced Ovarian Cancer. New England Journal of Medicine.
2018;379(26):2495-2505.
19. Morgan SC, Hoffman K, Loblaw DA, Buyyounouski MK, Patton C, Barocas D, Bentzen S, Chang M,
Efstathiou J, Greany P, Halvorsen P, Koontz BF, Lawton C, Leyrer CM, Lin D, et al. Hypofractionated
Radiation Therapy for Localized Prostate Cancer: An ASTRO, ASCO, and AUA Evidence-Based Guideline.
Journal of Clinical Oncology. 2018;36(34):3411-+.
20. Murillo OD, Thistlethwaite W, Rozowsky J, Subramanian SL, Lucero R, Shah N, Jackson AR, Srinivasan S,
Chung A, Laurent CD, Kitchen RR, Galeev T, Warrell J, Diao JA, Welsh JA, et al. exRNA Atlas Analysis Reveals
Distinct Extracellular RNA Cargo Types and Their Carriers Present across Human Biofluids. Cell.
2019;177(2):463-+.
21. Ortiz A, Gui J, Zahedi F, Yu PF, Cho C, Bhattacharya S, Carbone CJ, Yu QJ, Katlinski KV, Katlinskaya YV,
Handa S, Haas V, Volk SW, Brice AK, Wals K, et al. An Interferon-Driven Oxysterol-Based Defense against
Tumor-Derived Extracellular Vesicles. Cancer Cell. 2019;35(1):33-+.

MCW Research Overview
Jump to Table of Contents 157
22. Owen DL, Mahmud SA, Sjaastad LE, Williams JB, Spanier JA, Simeonov DR, Ruscher R, Huang WS, Proekt I,
Miller CN, Hekim C, Jeschke JC, Aggarwal P, Broeckel U, LaRue RS, et al. Thymic regulatory T cells arise via
two distinct developmental programs. Nature Immunology. 2019;20(2):195-+.
23. Papp K, Gordon K, Thaci D, Morita A, Gooderham M, Foley P, Girgis IG, Kundu S, Banerjee S. Phase 2 Trial
of Selective Tyrosine Kinase 2 Inhibition in Psoriasis. New England Journal of Medicine. 2018;379(14):1313-
1321.
24. Petersdorf EW, Stevenson P, Malkki M, Strong RK, Spellman SR, Haagenson MD, Horowitz MM, Gooley T,
Wang T. Patient HLA Germline Variation and Transplant Survivorship. Journal of Clinical Oncology.
2018;36(24):2524-+.
25. Roach M, Moughan J, Lawton CAF, Dicker AP, Zeitzer KL, Gore EM, Kwok Y, Seider MJ, Hsu IC, Hartford AC,
Horwitz EM, Yamoah K, Jones CU, Michalski JM, Lee WR, et al. Sequence of hormonal therapy and
radiotherapy field size in unfavourable, localised prostate cancer (NRG/RTOG 9413): long-term results of a
randomised, phase 3 trial. Lancet Oncology. 2018;19(11):1504-1515.
26. Rosenblum AM, Rosenblum AL. An Unusual Occurrence of Dual Tachycardia. Jama Internal Medicine.
2018;178(8):1113-1114.
27. Rosenstock J, Perkovic V, Johansen OE, Cooper ME, Kahn SE, Marx N, Alexander JH, Pencina M, Toto RD,
Wanner C, Zinman B, Woerle HJ, Baanstra D, Pfarr E, Schnaidt S, et al. Effect of Linagliptin vs Placebo on
Major Cardiovascular Events in Adults With Type 2 Diabetes and High Cardiovascular and Renal Risk The
CARMELINA Randomized Clinical Trial. Jama-Journal of the American Medical Association. 2019;321(1):69-
79.
28. Shalev AY, Gevonden M, Ratanatharathorn A, Laska E, van der Mei WF, Qi W, Lowe S, Lai BS, Bryant RA,
Delahanty D, Matsuoka YJ, Olff M, Schnyder U, Seedat S, deRoon-Cassini TA, et al. Estimating the risk of
PTSD in recent trauma survivors: results of the International Consortium to Predict PTSD (ICPP). World
Psychiatry. 2019;18(1):77-87.
29. Sherman SK, Lange JJ, Dahdaleh FS, Rajeev R, Gamblin TC, Polite BN, Turaga KK. Cost-effectiveness of
Maintenance Capecitabine and Bevacizumab for Metastatic Colorectal Cancer. Jama Oncology.
2019;5(2):236-242.
30. Shuen AY, Lanni S, Panigrahi GB, Edwards M, Yu L, Campbell BB, Mandel A, Zhang C, Zhukova N, Alharbi M,
Bernstein M, Bowers DC, Carroll S, Cole KA, Constantini S, et al. Functional Repair Assay for the Diagnosis
of Constitutional Mismatch Repair Deficiency From Non-Neoplastic Tissue. Journal of Clinical Oncology.
2019;37(6):461-+.
31. Stadtmauer EA, Pasquini MC, Blackwell B, Hari P, Bashey A, Devine S, Efebera Y, Ganguly S, Gasparetto C,
Geller N, Horowitz MM, Koreth J, Knust K, Landau H, Brunstein C, et al. Autologous Transplantation,
Consolidation, and Maintenance Therapy in Multiple Myeloma: Results of the BMT CTN 0702 Trial. Journal
of Clinical Oncology. 2019;37(7):589-+.
32. Stadtmueller BM, Bridges MD, Dam KM, Lerch MT, Huey-Tubman KE, Hubbell WL, Bjorkman PJ. DEER
Spectroscopy Measurements Reveal Multiple Conformations of HIV-1 SOSIP Envelopes that Show
Similarities with Envelopes on Native Virions. Immunity. 2018;49(2):235-+.
33. Stauch B, Johansson LC, McCorvy JD, Patel N, Han GW, Huang XP, Gati C, Batyuk A, Slocum ST, Ishchenko
A, Brehm W, White TA, Michaelian N, Madsen C, Zhu L, et al. Structural basis of ligand recognition at the
human MT1 melatonin receptor. Nature. 2019;569(7755):284-+.

MCW Research Overview
Jump to Table of Contents 158
34. Sun A, Hu C, Wong SJ, Gore E, Videtic G, Dutta S, Suntharalingam M, Chen Y, Gaspar LE, Choy H.
Prophylactic Cranial Irradiation vs Observation in Patients With Locally Advanced Non-Small Cell Lung
Cancer: A Long-term Update of the NRG Oncology/RTOG 0214 Phase 3 Randomized Clinical Trial. Jama
Oncology. 2019;5(6):847-855.
35. Timmerman RD, Paulus R, Pass HI, Gore EM, Edelman MJ, Galvin J, Straube WL, Nedzi LA, McGarry RC,
Robinson CG, Schiff PB, Chang G, Loo BW, Bradley JD, Choy H. Stereotactic Body Radiation Therapy for
Operable Early-Stage Lung Cancer Findings From the NRG Oncology RTOG 0618 Trial. Jama Oncology.
2018;4(9):1263-1266.
36. Volk A, Liang KW, Suraneni P, Li XY, Zhao JY, Bulic M, Marshall S, Pulakanti K, Malinge S, Taub J, Ge YB, Rao
S, Bartom E, Shilatifard A, Crispino JD. A CHAF1B-Dependent Molecular Switch in Hematopoiesis and
Leukemia Pathogenesis. Cancer Cell. 2018;34(5):707-+.
37. Wang HE, Schmicker RH, Daya MR, Stephens SW, Idris AH, Carlson JN, Colella MR, Herren H, Hansen M,
Richmond NJ, Puyana JCJ, Aufderheide T, Gray RE, Gray PC, Verkest M, et al. Effect of a Strategy of Initial
Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital
Cardiac Arrest A Randomized Clinical Trial. Jama-Journal of the American Medical Association.
2018;320(8):769-778.
38. Wang TS, Sosa JA. Thyroid surgery for differentiated thyroid cancer - recent advances and future
directions. Nature Reviews Endocrinology. 2018;14(11):670-683.
39. Wingler LM, Elgeti M, Hilger D, Latorraca NR, Lerch MT, Staus DP, Dror RO, Kobilka BK, Hubbell WL,
Lefkowitz RJ. Angiotensin Analogs with Divergent Bias Stabilize Distinct Receptor Conformations. Cell.
2019;176(3):468-+.
40. Wolfe GI, Kaminski HJ, Aban IB, Minisman G, Kuo HC, Marx A, Strobel P, Mazia C, Oger J, Cea JG,
Heckmann JM, Evoli A, Nix W, Ciafaloni E, Antonini G, et al. Long-term effect of thymectomy plus
prednisone versus prednisone alone in patients with non-thymomatous myasthenia gravis: 2-year
extension of the MGTX randomised trial. Lancet Neurology. 2019;18(3):259-268.
41. Yannopoulos D, Bartos JA, Aufderheide TP, Callaway CW, Deo R, Garcia S, Halperin HR, Kern KB,
Kudenchuk PJ, Neumar RW, Raveendran G, Amer Heart A, Emergency Cardiovasc Care C. The Evolving Role
of the Cardiac Catheterization Laboratory in the Management of Patients With Out-of-Hospital Cardiac
Arrest A Scientific Statement From the American Heart Association. Circulation. 2019;139(12):E530-E552.
42. Zenati MA, Bhatt DL, Bakaeen FG, Stock EM, Biswas K, Gaziano JM, Kelly RF, Tseng EE, Bitondo J, Quin JA,
Almassi GH, Haime M, Hattler B, DeMatt E, Scrymgeour A, et al. Randomized Trial of Endoscopic or Open
Vein-Graft Harvesting for Coronary-Artery Bypass. New England Journal of Medicine. 2019;380(2):132-141.
43. Zhao Y, Rafatian N, Feric NT, Cox BJ, Aschar-Sobbi R, Wang EY, Aggarwal P, Zhang B, Conant G, Ronaldson-
Bouchard K, Pahnke A, Protze S, Lee JH, Huyer LD, Jekic D, et al. A Platform for Generation of Chamber-
Specific Cardiac Tissues and Disease Modeling. Cell. 2019;176(4):913-+.

MCW Research Overview
Jump to Table of Contents 159
Society for Research Excellence
The Office of Research is pleased to host the MCW Society for Research Excellence, a
new collective of select MCW faculty with a demonstrated commitment to discovery,
mentorship, leadership, and advancement in research.
Mission: To foster, promote and recognize excellence across MCW in all types of
research and discovery.
Members of the SRE are characterized by such experience as:
• Sustained research leadership leading to high impact discoveries or findings
• History of serving as an effective mentor for trainees and/or junior faculty
• National recognition for research, such as high visibility publications, national
or international leadership roles, and/or receipt of awards
• MCW full time or full professional effort appointment for at least 5 years
2017 (Inaugural Membership)
Tom Aufderheide, MD
Emergency Medicine
Joseph T. Barbieri, PhD
Microbiology and Immunology
Allen W. Cowley, Jr., PhD
Physiology
Nancy M. Dahms, PhD
Biochemistry
Mary M. Horowitz, MD
Medicine: Hematology and Oncology
Balaraman Kalyanaraman, PhD
Biophysics
Jeffrey A. Kelly, PhD
Psychiatry and Behavioral Medicine
Purushottam (Prakash) W. Laud, PhD
Institute for Health & Equity
Julie A. Panepinto, MD
Pediatrics: Hematology & Oncology
Frank A. Pintar, PhD
Neurosurgery
Nita H. Salzman, MD, PhD
Pediatrics: Gastroenterology
Roy L. Silverstein, MD
Medicine: Hematology & Oncology
2018
David D. Gutterman, MD
Medicine: Cardiology
Elizabeth R. Jacobs, MD
Medicine: Pulmonary
Jeffrey R. Binder, MD
Neurology
Jenifer Coburn, PhD
Medicine: Infectious Diseases
John A. Corbett, PhD
Biochemistry
John D. Imig, PhD
Pharmacology & Toxicology
Joseph J. Carroll, PhD
Ophthalmology
2019
William R. Drobyski, MD
Medicine: Hematology & Oncology
Cecilia J. Hillard, PhD
Pharmacology & Toxicology
Quinn H. Hogan, MD
Anesthesiology
Mingyu Liang, MD, PhD
Physiology
Ann B. Nattinger, MD
Medicine: General Internal Medicine
Daisy Sahoo, PhD
Medicine: Endocrinology
Reza Shaker, MD
Medicine: Gastroenterology
Cheryl L. Stucky, PhD
Cell Biology, Neurobiology & Anatomy

MCW Research Overview
Jump to Table of Contents 160
About the Office of Research
Our Mission: The Office of Research is an integrated resource for facilitating scientific discovery through administrative
support of investigators, education and training, and ensuring regulatory compliance.
What do we do?
Our department is comprised of 9 specialized units that oversee research. Virtually every MCW researcher interacts with
our office in some way...
• Wet and dry lab space assignments
• Grant submission and management
• Human and animal research safety and compliance
• Formalized regulatory and safety approvals
• Electronic research systems training and maintenance
• Data and literary resource access
• Intellectual property guidance and assurance
We continuously look for new ways to improve the research experience! You can contact a member of our administrative
team via email: research@mcw.edu.
Office of Research Leadership: Administration
Ann B. Nattinger, MD, MPH, MACP
Associate Provost for Research
Professor of Medicine
Lady Riders Professor of Breast Cancer Research
Dr. Ann Nattinger stepped into the role of Senior Associate Provost for Research in October
2015. Prior to this appointment, Dr. Nattinger served as Division Chief of General Internal
Medicine for 15 years. A major proponent of research in academic medicine, in 2001 Dr.
Nattinger also founded the Center for Patient Care and Outcomes Research (now known as
CAPS) and served as Center Director for 16 years.
Dr. Nattinger is a nationally recognized cancer health services researcher, focusing on breast cancer treatment,
survivorship and outcomes. Her research has been funded by the National Institutes of Health, the Department
of Defense and the American Cancer Society. She has authored or co-authored more than 170 scientific papers,
abstracts and book chapters. Among Dr. Nattinger’s many accomplishments, she received the esteemed
designation as a “Master” of medicine from the American College of Physicians. Additionally, Dr. Nattinger
received the Distinguished Service Award in 2012, MCW’s highest faculty and staff honor.

MCW Research Overview
Jump to Table of Contents 161
Cecilia J. Hillard, PhD
Associate Dean for Research
Professor of Pharmacology and Toxicology
Director, Neurosciences Research Center
Dr. Cecilia Hillard was named Associate Dean for Research in November 2015 after serving as co-
Interim Senior Associate Dean for Research. Additionally, Dr. Hillard has served as director of the
Neuroscience Research Center since its inception in 2010. She was also Inaugural Director of the
Neuroscience Graduate Training Program from 1996-2010.
As a highly active researcher, Dr. Hillard’s laboratory is primarily focused on the pharmacology and biochemistry
of the cannabinoids and endocannabinoids. Her significant bibliography and frequent invitations to present attest
to her reputation as a leader in her field. Dr. Hillard is an MCW graduate and a true advocate for the Basic Sciences.
Frequently named an Outstanding Medical Student Teacher, Dr. Hillard takes an active role in training and
mentorship, receiving MCW’s highest honor, the Distinguished Service Award, in 2011.
Marja T. Nevalainen, MD, PhD
Assistant Dean for Research
Professor of Pathology
Associate Director of Education, Cancer Center
Dr. Nevalainen is an internationally recognized prostate cancer researcher. Her work has been
funded by the NIH’s National Cancer Institute, the Department of Defense, the American Cancer
Society, and several industry sponsors. Many patents and licensing agreements have been
developed in the Nevalainen Lab. She is frequently invited to speak to international audiences, including the
Gordon Conferences, the Endocrine Society and the European Association of Urological Research. Her work has
appeared in the Journal of Clinical Oncology, Journal of Clinical Investigation, Clinical Cancer Research, Nature
Urology, Cancer Research and Molecular Cancer Therapeutics, and she has been a long time Senior Editor for
Elsevier's Journal of Biochemistry and Cell Biology, and Editorial Board Member for the American Journal of
Pathology and The Prostate. A passionate educator, Dr. Nevalainen has mentored dozens of students and is an
important leader in the MCW Cancer Center’s education programs. Dr. Nevalainen has served in a number of grant
review panels including NCI, American Cancer Society and DOD Prostate Cancer Integration Panel over multiple
years.
Lisa R. Henk, MS
Chief Administrator for Research Operations
Lisa Henk joined the Office of Research leadership team in January, 2016 as Chief Administrator
for Research Operations. Prior to this appointment, Lisa served a dual role as Administrator for
the Department of Pharmacology and Toxicology and the Neurosciences Research Center for
four years. She also served as Interim Business Administrator for the Human and Molecular
Genetics Center for much of 2015. Since 2008, Lisa has been an important leader in Basic Science
Administration at MCW.
In her role as Chief Administrator, Lisa provides operational leadership for Office of Research functions. She works
closely with each of the department’s nine units to facilitate development, enhance efficiency, and provide the
best possible experience for researchers and staff. Lisa maintains a focus on both the immediate needs and long-
term objectives of MCW research.

MCW Research Overview
Jump to Table of Contents 162
Office of Research Leadership: Units
Grants & Contracts Office
Support submission of high quality, competitive & compliant funding
proposals
Training and educational resources for federal, state, and local procedures
Assistance and troubleshooting through rigorous application process
(414) 955-8563
mcw.edu/grants-and-contracts-office
April A. Haverty, MPE, JD
Director
Grants & Contracts Office
Human Research Protection Program
Oversight of the Institutional Review Board (IRB) and human subject
research
Navigating investigators & study staff through IRB processes
Ensuring safe, compliant & ethical treatment of human research subjects
IRBoffice@mcw.edu
(414) 955-8422
mcw.edu/hrpp
David Clark, PhD
Director
Human Research Protection
Program/IRB Office
Professor
Office of Technology Development
Protect invention & intellectual property for MCW
Invention disclosure: Intake & support
Discovery development & evaluation
Commercialization: Promotion, patenting, licensing & start-ups
(414) 955-4362
mcw.edu/Technology-Development
Kevin Boggs, MBA, PhD
Director
Office of Technology
Development

MCW Research Overview
Jump to Table of Contents 163
Research Systems
Guide investigators through MCW web-based research systems,
eBridge & OnCore
Registration, training, and help desk/support
ResSysTrain@mcw.edu
Help-ebridge@mcw.edu
(414) 955-8476
mcw.edu/research-systems-training.htm
Debbie Scott, PhD
Enterprise Research Applications
Manager
MCW Libraries
Provide MCW research faculty/staff with medical information
services & resources
Management of print, electronic, and web-based resources
Literary search, access & availability assistance
Topical research support & training
(414) 955-8302
(414) 367-9629 (text)
mcw.edu/libraries
Ellen Sayed, MLS, MAcc
Director, MCW Libraries
Biomedical Resource Center
Compliant laboratory animal facility: Research animal housing &
care
Facility management, safety & access
Support of data collection & transfer
BRCadmin@mcw.edu
(414) 955-4209
(414) 603-1591 (emergency pager)
Infoscope.mcw.edu/brc
Joseph D. Thulin, DVM, MS, DACLAM
Director, Biomedical Resource Center
Associate Professor

MCW Research Overview
Jump to Table of Contents 164
Institutional Animal Care & Use Committee Office
Oversight of the Institutional Animal Care and Use Committee &
animal research program
Federal & organizational compliance
Animal Use Application submission, review & management
Audit of facilities, programs & regulations
Complaint investigation & incident response
IACUCadmin@mcw.edu
(414) 955-8084
Infoscope.mcw.edu/iacuc
Sandra L. Jensen, MS, RLATG, CPIA
Institutional Animal Care & Use
Committee Office and Safety
Committees Manager
Office of Radiation Safety
Ensure safe and compliant use of radiation & radioactive materials
Monitor radioactive material inventory, use, treatment, and disposal
Regulate safe use, report incidents & respond to emergencies
RadSafety@mcw.edu
(414) 955-4347
mcw.edu/radiation-safety
Todd Senglaub, MHP
Radiation Safety Officer
Safety Committees
MRI Safety
MRIresearch@mcw.edu

MCW Research Overview
Jump to Table of Contents 166
Cancer Center
MCWCC is the only academic cancer research center in Southeastern Wisconsin, a distinct region
that includes large underserved minority populations with significant disparities in cancer
incidence, mortality and outcomes. The MCWCC serves over 2 million residents in a seven-
county area, providing the people of Southeastern Wisconsin with access to nationally
recognized physician scientists, the latest research-driven treatments, and over 200 cancer
clinical trials. The heart of our service area is the city of Milwaukee, the most segregated urban
area and 9
th
-poorest city in the U.S., with 30% of residents living at or below the poverty line.
The nearest cancer centers are in Madison and Chicago, 75-90 miles away, making MCWCC the
only academic cancer center accessible to these underserved populations. One of MCWCC’s top
priorities is to address and eliminate cancer disparities in Southeastern Wisconsin, and we are lucky to have a 47-member
Community Advisory Board to help direct efforts in this area.
MCWCC has over 250 faculty research and clinical members from five institutions and 24 MCW departments who are aligned
within three established Research Programs; Cancer Biology, Hematologic Malignancies & Immunotherapy and Cancer
Control & Outcomes. The MCWCC provides members with access to shared research resources – labs, cores, equipment,
data, and expertise. These resources are critical to successful cancer research but not usually available to individual
researchers because of cost, complexity or lack of space. Some of these resources are labs and equipment; some resources
are expertise, knowledge, or access to data. The MCWCC provides eight shared research resources; Bioenergetics, Biomedical
Imaging, Biostatistics, Clinical & Translational Research Laboratory, Flow Cytometry, Lymphocyte Propagation Lab,
Observational Methods, and Tissue Bank. Helping to direct the science of the MCWCC are thirteen Faculty Research
Committees that focus on disease-specific clinical research, in addition to external, internal and community advisory boards.
MCWCC physician scientists treat over 4,000 new cancer cases each year. There are over 200 cancer clinical trials underway,
with our researchers funded by over $35 million in peer-reviewed cancer research grants. The clinical cancer programs are
housed in the Clinical Cancer Center, where care is delivered in this 340,000 square feet building dedicated to cancer services.
This state-of-the-art ambulatory care facility houses multidisciplinary clinics, diagnostic and treatment imaging facilities,
operating rooms, the Quality of Life Center, and Breast Care Center. Designated clinical research facilities provide dedicated
space for research coordinators, biosampling, and processing, and a Translational Research Unit designed just for patients
participating in early phase I/II cancer clinical trials.
An important part of the MCW Cancer Center is the Nicholas Family Foundation Translational Research Unit (TRU). The TRU
is a space devoted to early-phase investigator initiated cancer research trials, one of only a few in the nation with the
capability to conduct early phase cancer clinical trials in dedicated space with experienced research staff. The TRU was built
to accommodate complex and novel cancer treatments and support pharmacokinetic and pharmacodynamic research. The
TRU encompasses 4,700 sq ft of space, with 13 infusion bays and a sub-waiting area with room for 2 patients. The TRU is
staffed with 10 experienced chemotherapy infusion nurses who have received additional training in the care of patients on
early-phase clinical trials. The location within the Clinical Cancer Center provides nearby access to the resources of the entire
center, including a dedicated research pharmacy, full laboratory, day hospital and 76-bed dedicated inpatient oncology space.
MCWCC is the only center in the state and region to have this type of dedicated unit, making it a unique resource for patients
throughout the upper Midwest.
To learn more, visit the MCWCC website at www.mcw.edu/cancercenter

MCW Research Overview
Jump to Table of Contents 167
Cancer Center Redox & Bioenergetics Shared Resource
The Medical College of Wisconsin Cancer Center (MCWCC) Redox and Bioenergetics Shared Resource (RBSR) was established
in 2012, as part of the cancer biology research program, to provide state-of-the-art instrumentation, cutting-edge techniques,
and sophisticated expertise dedicated to investigating cancer cell metabolism and redox signaling.
The mission of the RBSR is to enable researchers to assess cellular bioenergetics, metabolism, reactive oxygen species (ROS)
generation, and intracellular redox status. The RBSR provides an environment for education and training in research on oxy-
radicals, cellular redox, and bioenergetic status. The resource supports and guides investigators in the development of
anticancer treatments, based on the redox
profiling of cancer cell and bioenergetic
status. The RBSR is directed by Balaraman
Kalyanaraman, PhD, with oversight by an
advisory committee responsible for reviewing
all services provided by the resource.
The RBSR offers services and instrumentation
to assess many aspects of redox signaling and
metabolic function in cancer cells (Figure 1).
These include 1) detection of superoxide
radical anion, hydrogen peroxide, and
peroxynitrite; 2) the redox status of key
cytosolic and mitochondrial antioxidant
proteins including peroxiredoxins and
thioredoxins; 3) mitochondrial respiration
and glycolytic function; 4) analysis of
metabolic intermediates; and 5) identification
of altered metabolism using stable isotope-
based metabolite flux analysis.
The five main goals of the MCWCC RBSR are to 1) investigate cancer cell metabolism and redox signaling, and understand
how cancer cells exploit metabolic pathways for survival, proliferation, differentiation, and drug resistance; 2) provide a
better understanding of the bioenergetic pathways and oxidant production in cancer cells cultured under normoxic and
hypoxic microenvironments; 3) develop new, rigorous, and cost-effective assays to measure the production of ROS, redox,
and bioenergetic status in cancer cells in vitro and in tumors in vivo; 4) develop new redox- and metabolism-based strategies
for inhibiting cancer cell progression and metastasis and promoting cancer prevention and therapy; and 5) promote increased
collaboration in cancer metabolism research between basic scientists and clinical researchers at MCW.
The RBSR labs are centrally located for MCW cancer researchers at Froedtert Hospital, MCW, and the Blood Research
Institute, on the second floor of the MACC Fund Research Center (MFRC, Room 2013), in the Department of Biophysics.
The resources and facilities of the RBSR have been utilized in numerous grants, including program project grants, over the
past decade, and more than 40 research publications have utilized the RBSR facility. Examples of recent papers published by
the RBSR staff include [1–5].
Figure 1. The RBSR promotes the understanding of cancer cell
bioenergetics, metabolism, ROS, and redox signaling, which are
central to several areas of cancer research.

MCW Research Overview
Jump to Table of Contents 168
For more information, contact Jacek Zielonka, PhD (955-4789 or jzielonk@mcw.edu), or visit the RBSR website
(https://www.mcw.edu/departments/redox-and-bioenergetics-shared-resource).
1. Cheng G, Zielonka J, Hardy M, Ouari O, Chitambar CR, Dwinell MB, Kalyanaraman B. Synergistic Inhibition of Tumor
Cell Proliferation by Metformin and Mito-Metformin in the Presence of Iron Chelators. Oncotarget.
2019;10(37):3518-3532.
2. Zielonka J, Zielonka M, Cheng G, Hardy M, Kalyanaraman B. High-Throughput Screening of NOX Inhibitors.
Methods Mol Biol. 2019;1982:429-446.
3. Zielonka J, Zielonka M, Kalyanaraman B. HPLC-Based Monitoring of Oxidation of Hydroethidine for the Detection of
NADPH Oxidase-Derived Superoxide Radical Anion. Methods Mol Biol. 2019;1982:243-258.
4. Cheng G, Zhang Q, Pan J, Lee Y, Ouari O, Hardy M, Zielonka M, Myers CR, Zielonka J, Weh K, Chang AC, Chen G,
Kresty L, Kalyanaraman B, You M. Targeting Lonidamine to Mitochondria Mitigates Lung Tumorigenesis and Brain
Metastasis. Nat Commun. 2019;10(1):2205.
5. Kalyanaraman B, Cheng G, Zielonka J, Bennett B. Low-Temperature EPR Spectroscopy as a Probe-Free Technique
for Monitoring Oxidants Formed in Tumor Cells and Tissues: Implications in Drug Resistance and OXPHOS-Targeted
Therapies. Cell Biochem Biophys. 2019;77(1):89-98.

MCW Research Overview
Jump to Table of Contents 169
Cardiovascular Center
The Cardiovascular Center (CVC), founded in 1992 at the Medical College of Wisconsin (MCW), is
at the forefront of scientific discovery in cardiovascular health and disease. Over 36,000 square
feet of space is dedicated to the center’s laboratories, offices, conference rooms, and equipment
cores primarily located on the fourth floors of the Health Research Center (HRC) and Medical
Education Building (MEB). The CVC is staffed by full- and part-time personnel who maintain core
equipment, coordinate academic research, funding, and community outreach initiatives, and
provide support to the more than 160 CVC members from 21 departments and institutes on the
Milwaukee Regional Medical Campus.
The CVC’s mission is to improve cardiovascular health in southeast Wisconsin and beyond through cutting-edge research,
cost-efficient and high-quality healthcare delivery, rigorous training of the next generation of cardiovascular scientists, and
engaging the community to eliminate disparities in health outcomes.
At the CVC, an emphasis is placed on collaborative, multidisciplinary research centered around our faculty’s expertise in
thematic areas of research called Signature Programs and Affinity Groups, which are:
Signature Programs: Cross-Cutting Affinity Groups:
Atherosclerosis, Thrombosis & Vascular Biology Cardio-Oncology
Cardiac Biology & Heart Failure Prevention
Hypertension Redox Biology & Medicine
Precision Cardiovascular Medicine
The CVC is directed by Ivor Benjamin, MD, Professor of Medicine at Froedtert Hospital and MCW, and 2018-2019 President
of the American Heart Association, who has over 25 years of experience and expertise leading cardiovascular clinical and
research programs. David Gutterman, MD, the Senior Associate Director of the CVC and Northwestern Mutual Professor in
Cardiology, also brings more than 25 years of experience including 8 years as Senior Associate Dean for Research with broad
responsibility over research development and infrastructure. Moreover, as a green center, the CVC is also guided by an
external scientific advisory board, internal scientific advisory board, institutional leadership, and a CVC advisory board.
Along with its exceptional leadership, the CVC receives extensive institutional support in addition to a $4 million grant from
the Advancing a Healthier Wisconsin Research and Educational Endowment Program, and from philanthropic gifts by the A.
O. Smith Foundation, the Michael H. Keelan, Jr., MD, Cardiovascular Research Fund through the Greater Milwaukee
Foundation, and the Cullen Family Healthy Heart Research Program, among others. In 2017, the CVC was awarded a $1.6
million postdoctoral training grant from the National Heart, Lung, and Blood Institute, one of only five T32 postdoctoral
training programs on campus.
The CVC offers its primary members and their trainees access to core facilities including microscopy, imaging, other core
equipment, free biostatistical support, a quarterly newsletter, conference rooms for meetings and presentations, eligibility
for CVC grant awards, and promotion and sponsorship of the CVC Seminar Series and the Lunch and Learn Seminar Series,
which are held on an almost weekly basis during the regular school year in the CVC’s main conference room on the fourth
floor of the HRC.
Last year, the members of the CVC were awarded more than $77 million in total funding, with $30 million being funded by
the National Heart, Lung, and Blood Institute of the National Institutes of Health. More than 50 trainees were mentored and
465 scientific articles were published in peer-reviewed journals.
For more information, visit our webpage: http://www.mcw.edu/Cardiovascular-Center.htm

MCW Research Overview
Jump to Table of Contents 170
Center for Advancing Population Science
The Center for Advancing Population Science
(CAPS) (formerly Patient Care and Outcomes
Research (PCOR)) is proud to support the MCW
Research Day. CAPS mission is to develop, test, and
implement innovative strategies that transform
healthcare and optimize quality, value, and cost.
CAPS is comprised of a diverse group of investigators, supported by dedicated staff, with a wide range of clinical backgrounds
and areas of research expertise. CAPS Investigators are focused on becoming a global leader in healthcare transformation
through innovative research to improve the health of diverse populations and geographic regions. Center faculty range in
backgrounds of clinical training including internal medicine, surgical disciplines, pediatrics, physical medicine and
rehabilitation, emergency medicine and hematology-oncology, as well as economics, epidemiology, human factors, and
biostatistics. The research approaches used are broad and include survey methods, secondary analysis of existing large
databases, and the design and implementation of interventions to improve the delivery of health care. With an
interdisciplinary perspective, we can design studies that will translate innovative research to care that makes a difference in
patients’ lives. In addition to implementing innovative research projects, CAPS faculty are dedicated to mentoring medical
students, residents, graduate, undergraduate and high school students to foster the next generation of health services
researchers and innovators.
Areas of research focus for the center include:
• Health Systems Research, particularly related to the most effective ways to organize, finance, and deliver care, as
well as the translation and implementation of research findings into everyday clinical practice.
• Health Disparities, focusing on increasing the awareness of health disparities in the populations and communities
we engage in research and considering the impact of interventions on disparities.
• Community Engagement, focused on engaging communities in research through identifying relevant issues to the
community, conducting research in collaboration with communities, and evaluating and sharing results with the
community.
• Cancer control, particularly related to breast cancer therapy and survivorship issues;
• Cancer outcomes, understanding ways in which outcomes may vary for underserved populations, and ways to
ameliorate these disparities;
• Cardiovascular outcomes, including projects designed to improve care for hypertension, diabetes and obesity;
• Surgical care outcomes, involving outcomes related to breast and spine surgery;
• Patient-physician communication and medical decision making, including such diverse populations as pediatric
and adult ICU patients and veterans;
• Patient safety, consisting of issues related to shift handoffs, resident training, inpatient documentation and the
role of hospitalists;
• Fertility issues, including decision-making by patients seeking care for fertility problems and the expansion and
validation of a sexual function measure,
• Use of the electronic medical record (EMR), especially as it relates to communication between the doctor and
patient, and;
• Measurement of patient-reported outcomes, including health-related quality of life, with applications in both
research and clinical care.
For more information about CAPS, please visit: https://www.mcw.edu/Center-for-Advancing-Population-Science-CAPS.htm

MCW Research Overview
Jump to Table of Contents 171
Center for Biomedical Mass Spectrometry Research
Scope & Mission
The Center for Biomedical Mass Spectrometry Research, founded in 2017 at the Medical College of Wisconsin (MCW), is a
collaborative research hub for scientific discovery. We integrate state-of-the-art instrumentation, innovative methodologies,
advanced bioinformatics, and unique expertise to promote basic, translational, and clinical research programs. Our goals are
to catalyze interdisciplinary research, foster technology development, and provide education regarding the applications of
mass spectrometry in biomedical research. Our technologies and expertise are applied to targeted and untargeted analyses
of biological molecules including: identification, characterization, and quantification of peptides, proteins, metabolites, and
small molecules. With more than 50 established project workflows to choose from, we work together with investigators in a
flexible and collaborative model, to apply the most advance methods available in an individualized approach. Ultimately, the
MS Center is well-equipped with state-of-the-art instrumentation and recognized expertise that collectively provide a
competitive edge for investigators at MCW and partner institutions. To learn more, visit our website to learn more about our
capabilities. All projects begin with a consultation with MS Center experts.
To schedule your free consultation, please visit our website!

MCW Research Overview
Jump to Table of Contents 172
Center for Healthy Communities and Research
(Department of Family and Community Medicine)
The Center for Healthy Communities and Research (CHCR) was established to meet the growing need for rigorous scholarship,
teaching, and engagement to address health care gaps and advance health equity for underserved and vulnerable
populations. The CHCR is an integral part of the department, closely aligned with its affiliated family medicine residency
programs and MCW regional campuses. The CHCR is driven by three core commitments that are cornerstones for its work:
partnerships, education, and research.
CHCR faculty have a diversity of backgrounds, including sociology, psychology, adult education, anthropology, medicine, and
public health. The CHCR also houses strong expertise in qualitative research methods. The CHCR has built a regional and
national reputation for research in these areas, with faculty serving as principal or co-investigator roles for numerous internal
and extramurally funded awards (over $4.3M and $2.8M respectively) since 2016.
The CHCR has the following major areas of research activity:
• Health Equity and Disparities, examining from a critical sociological perspective the mechanisms by which social
institutions perpetuate disparities.
• Mental Health, prioritizing the study of trauma among military veterans, and resilience, peer mentoring, and the
influence of behavioral health on physical health outcomes.
• Physical Activity and Nutrition, focusing on inadequate food access, increasing physical activity in schools, and
innovative utilization of farmers’ markets for healthy food options.
CHCR faculty and staff develop, implement and evaluate educational courses across the continuum of medical education,
graduate and post graduate education. This includes support and sponsorship of primary care research training through the
Academic Fellowship in Primary Care Research. CHCR faculty and post-doctoral fellows teach and mentor medical students
each summer supported by a National Research Service Award from the National Institute on Aging. CHCR faculty also mentor
students in MCW’s Scholarly Pathways program on longitudinal research and service learning projects.
For more information about the CHCR, please visit: www.mcw.edu/chcr
For more information about the Academic Fellowship in Primary Care Research, please visit: https://www.mcw.edu/Family-
Medicine/Primary-Care-Research.htm

MCW Research Overview
Jump to Table of Contents 173
Center for Imaging Research
Our Mission:
The mission of the Center for Imaging Research (CIR) is to unite basic and clinical scientists of various disciplines to further
the development and application of imaging in health and disease.
Investigators from institutions across the Midwest utilize the resources available within the MCW CIR. Our state of the art
facilities and technical support infrastructure provide users with tools required to perform basic and clinical imaging research
studies.
Investigative projects at the CIR span a wide variety of disease states and topics of technological development.
Services Offered:
The CIR maintains 4 research-dedicated MRI systems, including a 3.0T GE Healthcare Discovery MR750 located in the
Froedtert Pavilion, the newest generation 3.0T GE Healthcare Signa Premier located in the MRI annex to the MACC Fund
Building, a 7.0T GE Healthcare MR950 located in the MRI annex, and a pre-clinical 9.4T Bruker Biospec located in the MRI
annex.
The CIR is structured to enable the use of MRI in a broad range of research studies. Support is available from staff and faculty
level physicists on a fee-for-service model. This support can be used to protocol experiments, develop novel image
acquisitions, and assist in image analysis. For pre-clinical work, an animal “drop-off” service is available to aid in the
preparation and handling of small animals in imaging studies. With these services, the goal of the CIR is to lower the “barrier
to entry” for imaging studies. Ultimately, researchers with questions that can be answered with MRI can use the services of
the CIR to tailor an imaging experiment and understand its outcome.
The CIR has an imaging study pilot award funding opportunity. Renewable $5,000 awards are available, and are reviewed and
awarded on a rolling basis. Funds from these awards are available for study setup, general physics support, data analysis, and
imaging expenses. For application details, please see the CIR webpage: www.mcw.edu/CIR.
The following imaging equipment is dedicated for research use and is available to all funded researchers associated with the
MCW CIR:
• GE Healthcare Advantage Workstation with VolumeShare 7.0
• GE Healthcare Discovery MR750 3T MRI
• GE Healthcare Signa Premier 3T MRI
• GE Healthcare Discovery MR950 7T MRI
• Bruker 20cm 9.4T pre-Clinical MRI
Contact Us:
Center for Imaging Research
Medical College of Wisconsin
8701 Watertown Plank Road
Milwaukee, WI 53226
414-955-4663

MCW Research Overview
Jump to Table of Contents 174
Center for Immunology
The Center for Immunology under the Directorship of Dr. Michael Dwinell, was established in 2018 and built on a strong
decade-long informal group known as the Committee on Immunology that spanned investigators at the Medical College of
Wisconsin (MCW), the Children’s Research Institute and Versiti, Blood Research Institute.
The Center for Immunology combines expertise in basic and clinical immunology to accomplish two goals across MCW:
• Integrate immunological resources around emerging needs in clinical care that will constitute the personalized
healthcare of tomorrow
• Coordinate immunological research investment capacity by coordinating Center communications and interactions
The comprehensive Center for Immunology will coordinate the resources, investments and research strengths in
immunology to build additional capacity in basic and translational research to enhance patient care and strengthen MCW’s
connection to the community.
To achieve these goals the Center for Immunology will empower clinicians and basic scientists to collaborate in translational
research, to understand immune pathology and pathophysiology, and to develop individualized and effective treatments
for our patients. Congruent with these translational goals the Center will streamline the education of tomorrow’s physicians
so that they are conversant in the use of immune-based therapies and confident in initiating cutting-edge trials with new
therapies.

MCW Research Overview
Jump to Table of Contents 175
The Center for Infectious Disease Research
The mission of the Center for Infectious Disease Research (CIDR), is to enhance research efforts that focus on understanding
the molecular mechanisms of pathogenesis related to infection with all types of microorganisms, viruses, fungi or parasites.
These efforts also include programs to define host factors contributing to disease resistance or susceptibility, host recognition
of foreign materials and the innate and adaptive immune responses following exposure to infectious organisms. Overall, the
long-term goals are to integrate basic and translational research for the development of new therapeutics, vaccines and
diagnostic tests.
CIDR was established in 2002 as the Center for Bioterrorism and Infectious Diseases (CBID) under the leadership of Dr. Dara
Frank, Founding Director. Dr. Frank established a core of highly successful investigators whose research focuses on bacterial
pathogens, viral pathogens, and parasites. Dr. Frank also established the highly interactive and collaborative nature and
culture of CIDR that persists today. CBID was also dedicated to the set up and maintenance of a state of the art Biosafety
Level 3 laboratory and development of a select agent research program. Select agents are those of particular concern from
the standpoint of potential use as biological weapons. The name of the Center was changed in 2010 to reflect broadening
appreciation for the importance of infectious diseases that are caused by organisms that would be difficult to weaponize.
CIDR remains dedicated to fostering collaboration that will lead to new insights into a number of infectious diseases. These
insights are essential to formulating strategies to combat infectious diseases, including vaccines and new therapeutic
approaches guided by comprehensive understanding of the pathogenic mechanisms of bacteria, parasites, and viruses.
Please visit the CIDR website at https://www.mcw.edu/Center-for-Infectious-Disease-Research-CIDR.htm to learn more
about who we are and what we do.

MCW Research Overview
Jump to Table of Contents 176
Center for International Blood & Marrow Transplant Research
The Center for International Blood and Marrow Transplant Research (CIBMTR)
collaborates with the worldwide scientific community to advance the fields of
hematopoietic cell transplantation (HCT) and cellular therapy (CT). A research
collaboration between MCW and the National Marrow Donor Program/Be The
Match, the CIBMTR facilitates important clinical research to increase survival and
enrich the quality of life for thousands of patients.
The CIBMTR’s research arises from a base of collaborative scientific and statistical expertise, a network of >400 centers across
the globe, a clinical database containing information from >530,000 patients, and a biospecimen repository containing
>140,000 samples. Information from the database, and the support provided by the CIBMTR Coordinating Center to analyze
it, have led to the successful completion of hundreds of studies that have significantly impacted clinical practice worldwide.
At any given time, the CIBMTR has >200 observational studies and >10 prospective studies ongoing. Since inception, the
organization has published >1,300 articles and chapters in scientific publications. In 2018, the CIBMTR generated 109
publications and presented 76 abstracts at national and international conferences.
The CIBMTR has six major areas of research activity:
• Clinical Outcomes. Fifteen international Scientific Working Committees oversee most of the CIBMTR’s clinical outcomes
research. Each committee focuses on a specific disease, use of HCT or cellular therapy, or complication of therapy. They
utilize the CIBMTR’s clinical database to answer clinically important questions in a timely manner.
• Clinical Trials. The CIBMTR supports prospective research to evaluate new transplant and cellular therapies. The Blood
and Marrow Transplant Clinical Trials Network conducts multicenter Phase II and III national trials. The Resource for
Clinical Investigations in Blood and Marrow Transplantation supports Phase I-III trials, providing investigator support
services, survey research, and clinical study management.
• Immunobiology. The CIBMTR maintains a repository of paired tissue samples (from donors and recipients, related and
unrelated) used in studying the genetic, cellular, and immunologic factors that influence the outcomes of transplantation
and cellular therapy.
• Health Services. The CIBMTR facilitates studies regarding economic and health-related cost analyses, disparities in and
barriers to access, treatment decision making and support, health care utilization, quality and value of care, and survey
research.
• Bioinformatics. The CIBMTR analyzes genetic data, particularly the major histocompatibility complex; research activities
include improving the transplant match algorithm and data standards as well as conducting donor registry modeling
• Statistical Methodology. In conjunction with the MCW Division of Biostatistics, the CIBMTR Coordinating Center not only
provides advice and statistical consultation to researchers writing proposals and developing protocols for HCT and
cellular therapy studies but also investigates new statistical approaches and techniques for analyzing their data.
The CIBMTR serves as the data repository for the Stem Cell Therapeutic Outcomes Database for HRSA’s C.W. Bill Young Cell
Transplantation Program. As such, it collects data for all allogeneic HCTs performed in the US and, worldwide, any HCTs
performed with products procured through the Program. The goal is to make blood and marrow transplants available to all
who need them and to increase the safety and effectiveness of HCT.
.

MCW Research Overview
Jump to Table of Contents 177
Center for Microbiome Research
What Do We Do?
The Center for Microbiome Research (CMR) facilitates collaborative research, provides specialized research resources, and
promotes education. A microbiome is defined as the totality of microorganisms and their collective genetic material present
in or on the human body or in another environment. This ecological community consists of bacteria, viruses, fungi, yeasts,
and protozoa. Each body site has a distinct microbiome, but the vast majority of the microbiota reside in the GI tract. The
precise composition of a physiological microbiome is affected by host diet, age, genetics, exposure to drugs, and other
environmental factors. Disrupted microbiomes have been correlated with a number of disease states including obesity,
diabetes, asthma, eczema, heart disease, celiac disease, colitis, neuropsychiatric disorders, and some cancers.
Benefits:
• Collaboration with MCW, CHW & BRI investigators
• Gnotobiotic Core Facility (GCF) resource
• Training and assistance in biota-focused sample collection,
processing & sequence coordination
• Invited speaker seminar series, journal club, & bioinformatics
workshops
Microbiome-Focused Services Offered
• Consultation: Study Design & Funding Applications
• Sample Collection & Processing specific to microbial targets
• Gnotobiotic Core Facility: Axenic and gnotobiotic rodent husbandry & experiments, including choice of isolators or
iso-caging as appropriate for your study.
• Bioinformatics & Biostatistics support and training
Contact Us:
Nita Salzman, MD, PhD Mary Holtz, PhD
Center Director Program Manager
CRI Wing, TBRC, 3
rd
floor bay, #C3368; Email for an appointment
https://www.mcw.edu/Center-for-Microbiome-Research.htm

MCW Research Overview
Jump to Table of Contents 178
Center for Neurotrauma Research
(Department of Neurosurgery)
The Medical College of Wisconsin recently launched the Center for Neurotrauma Research (CNTR) with the Department of
Neurosurgery. The CNTR’s multidimensional mission is to advance the science of neurological trauma and related diseases,
enhance the translation of brain and spinal trauma research into clinical care innovations, foster the professional
development of future scientists, and improve the health of communities throughout the region and state. Within MCW, the
CNTR functions as a collaborative hub for neurotrauma research and will create a synergistic collaboration with other MCW
Centers such as the Comprehensive Injury Center, Neuroscience Research Center and the Center for Imaging Research.
The CNTR builds upon the successful track record of the neurotrauma research program in the Department of Neurosurgery
spanning more than 25 years, including dramatic growth over the past 10 years. The creation of the CNTR reflects MCW’s
scientific progress in this field and the program’s current standing in the international neurotrauma research community.
The CNTR is co-directed by Shekar Kurpad, MD, Sanford J. Larson Professor and Chair of Neurosurgery; and Michael McCrea,
PhD, Professor of Neurosurgery, Eminent Scholar, Vice Chair of Research and Director of Brain Injury Research.
Spinal Cord Injury Research
Spinal Cord Injury (SCI) is a relatively frequent event, with estimates suggesting that 12,500 new cases of SCI occur every year
in the US alone. In the US, approximately 276,000 persons live with SCI, which has a huge impact on their lives and families,
as well as tremendous socioeconomic and medical costs. Additionally, approximately 500,000 persons in the US are living
with non-traumatic SCI, brought on by degenerative diseases, tumors, and other causes.
The current theme in SCI research is interdisciplinary cooperation with a strong emphasis on a multi-pronged solution to
increase functional recovery. The Department of Neurosurgery is conducting research in diagnostic, interventional, and
therapeutic areas of SCI. Our researchers are examining Diffusion Tensor MR Imaging of traumatic SCI and of cervical
myelopathy, giving clinicians more information about prognosis at earlier time points. We are investigating the mechanisms
that contribute to secondary tissue damage tissue damage following SCI with the aim to reduce this damage and thereby
improve functional outcome. The Department of Neurosurgery is also involved in clinical trials investigating stem cell
intervention in SCI patients.
Traumatic Brain Injury Research
Traumatic Brain Injury (TBI) is a significant public health problem with national estimates of TBI in the United States range
anywhere from 1.4 million to 4 million brain injuries per year, depending on the study and methods used to define and include
cases. About 75% of TBIs that occur each year are concussions or other forms of mild traumatic brain injury (mTBI). The Brain
Injury Research Program was established in the Department of Neurosurgery in 2011 and focuses on investigating the acute
and chronic effects of traumatic brain injury (TBI). With funding from the Department of Defense, National Collegiate Athletic
Association, the National Institutes of Health and other sources, current research employs basic and applied methods to study
civilian, military and sport-related brain injury. Ongoing projects focus on understanding individual differences in TBI
recovery, refining TBI outcome measurement, investigation of advanced multi-modal MRI techniques, identifying the acute
effects of mTBI on brain biochemistry and physiology using blood biomarkers, and determining the short- and long-term
effects of mTBI. The Brain Injury Research Program is also involved in various large scale national efforts to study TBI, such
as the NCAA-DOD CARE Consortium, TRACK-TBI, and the TBI Endpoints Development Initiative.

MCW Research Overview
Jump to Table of Contents 179
Head and Spine Biomechanics
One of the longest running research programs in the Department of Neurosurgery has focused on head and spine
biomechanics, with emphasis on trauma and disease. This research area brings together engineering scientists specializing
in biomechanics and neurosurgeons to determine how the spine and the head-neck complex are compromised in traumatic
events and through disease progression. Current efforts in this area include: examination of spinal trauma in underbody
military vehicle blast events, development of lumbar spine injury criteria in vehicle and other types of crashes, comparison
of available artificial cervical discs and their viability in active military personnel, investigation of head supported mass and
the effects of wearing advanced combat helmets for prolonged periods of time, and the development of spine injury criteria
for female military personnel.
Patient Specific Modeling
Surgical Intervention in the spine to optimize neurologic function has a measurable effect on the biomechanics of the spine
with possible neurologic sequelae. In general, current intervention and treatment plans are based on rough estimates of
outcomes, primarily based on results of clinical trials. One explanation for variation in outcome is differences in local anatomy
between patients. Personalized finite element (PFE) modeling is the development of accurate computer models that use
patient specific data. Researchers in Neurosurgery are working to develop and validate a clinician friendly tool that can
perform patient specific pre-clinical evaluations to aid with the treatment planning process.

MCW Research Overview
Jump to Table of Contents 180
Center of Systems Molecular Medicine (CoSMM)
The CoSMM is a research center in the Department of Physiology at the Medical College of Wisconsin. The mission of the
CoSMM is to develop and apply systems molecular approaches to improve the understanding and treatment of human
disease. The primary function of the CoSMM is to serve as an intellectual incubator for research and project development.
The current areas of focus at the CoSMM are regulatory RNA, epigenomics and related translational research.
The CoSMM currently has 24 member laboratories led by faculty with primary or secondary appointments in the Department
of Physiology. CoSMM members collaborate with more than 10 institutes, departments or divisions at MCW in studies
related to CoSMM’s areas of focus, sharing our expertise with investigators across MCW.
CoSMM members have published dozens of studies on regulatory RNA, epigenomics and related translational research.
Examples of notable publications in CoSMM’s areas of focus since 2018 are listed below (CoSMM member faculty shown in
bold font).
1. Chuppa S, Liang M, Liu P, Liu Y, Casati M, Cowley AW, Patullo L, Kriegel AJ. MicroRNA-21 regulates peroxisome
proliferator-activated receptor alpha, a molecular mechanism of cardiac pathology in Cardiorenal Syndrome Type
4. Kidney Int. 2018 Feb; 93(2): 375-389.
2. Widlansky ME, Jensen DM, Wang J, Liu Y, Geurts AM, Kriegel AJ, Liu P, Ying R, Zhang G, Casati M, Chu C, Malik M,
Branum A, Tanner MJ, Tyagi S, Usa K, Liang M. miR-29 contributes to normal endothelial function and can restore
it in cardiometabolic disorders. EMBO Mol Med. 2018 Mar; 10(3): e8046.
3. Sun X, Han Y, Zhou L, Chen E, Lu B, Liu Y, Pan X, Cowley AW Jr, Liang M, Wu Q, Lu Y, Liu P. A comprehensive
evaluation of alignment software for reduced representation bisulfite sequencing data. Bioinformatics. 2018 Aug
15;34(16):2715-2723.
4. Liu Y, Usa K, Wang F, Liu P, Geurts AM, Li J, Williams AM, Regner KR, Kong Y, Liu H, Nie J, Liang M. MicroRNA-214-
3p in the Kidney Contributes to the Development of Hypertension. J Am Soc Nephrol. 2018 Oct;29(10):2518-2528.
5. Han Y, Yang J, Qian X, Cheng WC, Liu SH, Hua X, Zhou L, Yang Y, Wu Q, Liu P, Lu Y. DriverML: a machine learning
algorithm for identifying driver genes in cancer sequencing studies. Nucleic Acids Res. 2019 May 7;47(8):e45.
Visit our website for more information: http://cosmm.org/

MCW Research Overview
Jump to Table of Contents 181
Children’s Research Institute
Children’s Research Institute represents the investment of Children’s Hospital of
Wisconsin in pediatric research. The Children's Research Institute (CRI) advances state-
of-the-art pediatric health care through translational research programs designed to
find life-saving discoveries, interventions and cures for the diseases that affect children.
Additionally, our researchers are studying ways to improve the quality of life for
children living with chronic diseases. Investigators are involved in nearly 1,000 active clinical research studies, and pediatric
researchers have over $27 million in extramural funding.
The CRI currently has numerous cores and shared services to help pediatric investigators, including:
• BioBank and Analytical Tissue Core
• Histology
• Confocal Imaging
• Flow Cytometry
• Pediatric Translational Research Unit
• Quantitative Health Sciences (Biostatistics)
• Grants Development Office
For more information on the cores and how their capabilities can enhance your research, contact Bill Sweeney at 955-5773.
Children’s Research Institute is organized in Research Units to promote team science. Research Unit Leaders are charged with
strategically growing and advancing science in their disciplines through programmatic development and collaborative efforts.
The CRI Research Units are:
• Developmental Genetics & Genomics
• Infection, Inflammation and Immunity
• Vascular Biology & Hematology
• Patient-Centered Research.
Examples of research awards for ongoing CRI investigations include:
• Ulrich Broeckel, MD, professor of Pediatrics at MCW and a research unit leader of the CRI was awarded a $2.5 million
dollar NIH grant entitled “Genetics of Cardiomyocyte and Cardiac Matrix Interaction”
• Amy Drendel, DO, professor of Pediatrics at MCW and CRI member was awarded a $2.9 million dollar NIH grant entitled
“The Effect of Emergency Department and After-Emergency Department Analgesic Treatment on Pediatric Long Bone
Fracture Outcomes”
• Martin Hessner, PhD, professor of pediatrics at MCW and a research unit leader of the CRI was awarded a $1 million
dollar grant from the Juvenile Diabetes Research Foundation entitled “Prediction of Post-onset Partial Remission
Duration in New Onset Type 1 Diabetes”
• Julie Panepinto, MD MSPH, professor of Pediatrics at MCW and research unit leader of the CRI received a $2.7 million
dollar NIH grant “Midwest Child Patient Reported Outcomes Consortium”
• Nita Salzman MD, PhD, professor of Pediatrics at MCW and research unit leader of the CRI received a $2.0 million dollar
NIH award entitled “Intestinal Enterococcal Dynamics; Modeling Host-Commensal and Host-Pathogen Interactions”
• Janette Strasburger, MD, professor of pediatrics at MCW and CRI member received a $2.4 million dollar NIH award titled
“Fetal Electrophysiologic Abnormalities in High-risk Pregnancies Associated with Fetal Demise”
Children’s Research Institute researchers have also received recent funding from several national foundations including
American Diabetes Association, American Cancer Society, American Heart Association, Cystic Fibrosis Foundation, Lillian
Goldman Charitable Trust and the W.M. Keck Foundation.

MCW Research Overview
Jump to Table of Contents 182
Clinical & Translational Science Institute
The Clinical & Translational Science institute of Southeast Wisconsin (CTSI) is dedicated to transforming the biomedical
research enterprise in southeast Wisconsin to advance patient care and education. The 8 member organizations, the Medical
College of Wisconsin, Marquette University, the Milwaukee School of Engineering, University of Wisconsin-Milwaukee the
BloodCenter of Wisconsin, Children’s Hospital and Health System, Froedtert Hospital, and the Clement J. Zablocki VA Medical
Center, create a borderless, synergistic research enterprise that accelerates the translation of research discoveries into new,
innovative medical treatments.
The CTSI serves as a nexus for services that support clinical and translational research, including:
▪ The Faculty Collaboration Database fosters collaboration between the CTSI member institutions through detailed
faculty profiles.
▪ Biomedical Informatics supports the collection and management of data from CTSI supported protocols, offers
image de-identification services, and is the clearinghouse for access to clinical data through the data warehouse.
▪ Statistical support for investigators on study design, data management, data entry, and statistical software usage
and analysis
▪ Cores Search – A centralized database of core facilities and technical expertise available at MCW and partnering
institutions
▪ Clinical Trials Office (CTO) – The MCW CTO is a central resource available to investigators to facilitate
implementation of clinical studies and trials. The CTO operates at MCW, CHW and at our partner institutions in
Greater Milwaukee area to provide fully trained study coordinators who assist with all aspects of clinical trial
implementation, including but not limited to, IRB submissions, budget and contract negotiations, recruitment of
patients into trials and any other activity required for completion of research protocols. We also provide
assistance with IND/IDE applications, study monitoring and audit, OnCore implementation and educational
programs such as BootCamp for new research staff.
▪ Translational Research Units (TRUs) – CTSI has three TRUs: the Adult TRU at Froedtert Hospital, a Pediatric TRU at
Children’s Hospital of Wisconsin, and an Adult/Geriatric TRU at the VA Hospital. Research support includes nursing
care for research participants, Boinutrition and Body Composition Cores, Exercise Physiology Lab, Pediatric
Echocardiography Core Lab, Sleep Lab, and a Translational Cardiac and Vascular Function Unit.
▪ CTSI’s website serves as our virtual portal. All information related to our mission, from educational to funding
opportunities and clinical research resources to workshops and conferences is located on the site. Membership is
required to access CTSI resources. Please join: ctsi.mcw.edu/join
The CTSI supports and promotes efforts to enhance multidisciplinary collaborations within our institution and with others,
including:
▪ Collaboration consortia with UWM, MU and MSOE to focus on administrative, informatics, educational, and
project/program initiatives
▪ Virtual Community with online tools for investigator collaboration (web conferencing, group document sharing,
virtual white board, instant messaging, etc.)
▪ Common IRB – one set of forms and one meeting for multi-site studies with area academic collaborators (MU,
UWM, MSOE)
▪ Shared research facilities, staff, other resources

MCW Research Overview
Jump to Table of Contents 183
▪ Infrastructure for promoting translational research that includes the community as active partners (community
based physicians, advocacy groups)
The CTSI funds innovative, multidisciplinary programs that advance clinical and translational research, including:
▪ Clinical and Translational Pilot Grants for collaborative teams of researchers
▪ Core support for facilities conducting research in novel methodologies
▪ Infrastructure support for services that promote clinical and translational research
▪ Support for the enhancement of technology transfer services and expertise
▪ Co-funding grant opportunities with Advancing a Healthier Wisconsin
The CTSI provides training opportunities that will prepare individuals to function effectively on multidisciplinary research
teams:
▪ Mentored Clinical and Translational Research Awards (KL2)
▪ MS degree in Clinical and Translational Sciences
▪ PhD in Basic and Translational Science
▪ PhD and MS in Clinical and Translational Rehabilitation Health Science at Marquette University, Jointly sponsored
with CTSI
▪ Clinical Research Scholars Program
▪ Lecture series on Grant Preparation, Biostatistics, and Collaborative IRB Training Initiative (CITI)
▪ Workshops on training human research team members on basic knowledge necessary to conduct research safely,
ethically, and efficiently
For more information about CTSI, please visit our website at https://ctsi.mcw.edu/

MCW Research Overview
Jump to Table of Contents 184
Comprehensive Injury Center
The mission of the Comprehensive Injury Center (CIC) is to create a platform to engage campus and community partners in
the advancement of injury control and prevention science. The CIC will build on the history of the Injury Research Center as
well as the strengths of our faculty and staff who work in many sectors across campus to advance all four missions of the
Medical College of Wisconsin with a focus on injury control and prevention.
The goals of the CIC are to:
• Advance injury prevention and control science by facilitating, conducting, and disseminating interdisciplinary injury
prevention and control research that makes new discoveries in injury prevention, acute care, and rehabilitation;
• Catalyze, leverage, and advance the value of our Level I Trauma Centers by translating research into clinical
practice by partnering with faculty and staff to advance the care and rehabilitation of the injured patient through
discovery, translation, and training, as well as contribute to efforts to maintain national and state-level trauma
verification, which require advanced care and sustained research and prevention efforts;
• Utilize and leverage our campus resources including our experienced faculty and staff to train the next generation
of injury prevention and control researchers, practitioners, and educators by developing, implementing, and
evaluating multi-disciplinary educational opportunities; and
• Strengthen injury prevention and control practice by engaging our community through strong partnerships that
facilitate, translate, and disseminate evidence-based programs and policies.
The CIC will serve as the convening body for ongoing injury prevention and control work at our two Level I Trauma Centers,
the Medical College of Wisconsin, and the VA Medical Center, facilitating interdepartmental partnerships and providing a
platform for collaboration. This will enhance both the breadth and depth of the advances that can be made by leveraging
talent and investments that exist across this campus as well as become a beacon for attracting new talent and investments
to our campus.

MCW Research Overview
Jump to Table of Contents 185
Drug Discovery Center
The primary focus of the Drug Discovery Center is to facilitate and accelerate drug discovery and the translation of new
basic discoveries in to therapies to improve human health. Research expertise at the center will provide resources,
knowledge, and services to complete the drug development process from target validation, drug design, and drug delivery
to clinical application.
• Discovery to Clinic
• Collaborations
• Funding opportunity guidance
• Non-GLP PK and Tox studies
• Small Molecule modification & design
• CMC and Process development
Center’s Signature Program
One step at a time in Multistep process
Mission: To facilitate and accelerate therapeutics & drug discovery by translation of ne basic discoveries into therapies.
TAP’s Services:
• Providing internal project based funding opportunities
• Facilitating collaborations (internal & external)
• Independent scientific review and guidance
• I.P. disclosure assistance
• Project execution
For more information or discussion contact:
Dr. Ranjit Verma, r[email protected], (414) 955 -5743
Dr. John Imig, jdimig@mcw.edu, (414) 955 -4834

MCW Research Overview
Jump to Table of Contents 186
Genomic Sciences & Precision Medicine Center
Since 2017, the MCW genomics center has
continued its transformation into the Genomic
Sciences & Precision Medicine Center (GSPMC)—
a robust family of specialized yet interconnected
Precision Medicine Laboratories with the Mission
to prevent, diagnose, and treat diseases, as well as improve the wellness of our patients and the community
through scientific investigations and their rapid translation to the medical practice. All efforts strive to achieve the
Center’s Vision to provide educational, clinical, and research support infrastructure to the Milwaukee Regional
Medical Center, establishing MCW and its partnering health care providers as the premier Precision Medicine
provider in the state of Wisconsin and one of the top in the nation. Core to realizing this vision is the critical role
of research, wherein the GSPMC will arm MCW researchers with the advanced science necessary to increase
funding and establish the Institution as a national leader in Precision Medicine research.
Modernized Precision Medicine Laboratories to Enable Research and Clinical Practice:
The GSPMC’s Precision Medicine Laboratories (PML) boast over 40 precisely-recruited, expertly-trained
laboratory leadership and staff, who enable an expansive and diverse menu of services with over 300 clinical,
translational, and basic science research assays and, through the constant evaluation, reconstruction, and
maximization of infrastructure, equipment, technology, and project management, have created a capacity of over
3 million samples a year. Continuous development of assays, methods, and services is an ongoing, Center-wide
effort. Presently focusing these development efforts on research-enabling assays and services in the areas of
genomics, epigenomics, pharmacogenomics, microbiome, data science, and undiagnosed and rare diseases, these
offerings are scheduled to be fully developed by 2022. In FY19 alone, GSPMC completed nearly 400 projects for
56 different PI’s in 18 different MCW departments, and the number of projects completed in FY20 is expected to
increase significantly.
The aggressive development and offering of services require the following matrix of Precision Medicine
Laboratories and Units:
▪ Germline Sequencing Laboratory
▪ Somatic Molecular Oncology Precision Medicine Laboratory
▪ Epigenomic Laboratory
▪ Research and Development Laboratory
▪ Bioinformatics Research & Development Laboratory
▪ Functional Validation Laboratory
▪ Precision Medicine Simulation Unit for New Methods of Interpretation of Genomic Information
Robust Bioinformatic and Data Modeling Research, Development, and Services:
In order to expand the reach of its services and collaborative network, the GSPMC continues to grow its
bioinformatics workforce, with 5 active recruitments alongside a present headcount of 15 (6 PhD-level, 4 Masters-
level, and 2 Bachelors-level bioinformaticians as well as 2 IT managers and 1 software engineer). This engine of
Bioinformatics is at the heart of these “connector” service lines that are enhancing research, translation, and
patient care.

MCW Research Overview
Jump to Table of Contents 187
Services:
The GSPMC offers whole exome and genome sequencing as well as many additional services, including RNA-Seq,
ChIP-Seq, RRBS, and 10x Genomics Single Cell sequencing. In the field of precision diagnostics and therapeutics,
the PML offers assays in pediatric and adult solid tumors, liquid biopsies, and myeloid diseases. The Center also
provides robust bioinformatics, quality control, and validation for all assays and will work with investigators to
develop custom research and translational sequencing analysis.
Facilities:
The GSPMC occupies a 20,000 square foot facility on the 5th floor of MCW’s Health Research Center. These
facilities have modern design, state-of-the-art equipment, and expert personnel to allow the efficient
implementation of next generation sequencing methodologies to Cancer Genomics, Non-Cancer Clinical
Genomics, Pharmacogenomics, Epigenomics, Molecular Pathology, and Rare Diseases.
Our Technology:

MCW Research Overview
Jump to Table of Contents 188
Institute for Health & Equity
Biostatistics Consulting Service
The Division of Biostatistics is part of the Institute for Health and Equity at the Medical
College of Wisconsin. The Division’s faculty, staff, and students are dedicated to providing
basic biostatistical support for biomedical researchers. The Division focuses on three
missions: Methodologic research into novel techniques for analyzing biomedical data,
Collaborative research with biomedical researchers such as through the Biostatistics
Consulting Service, and Education including a PhD program in Biostatistics and other training opportunities.
Research Accomplishments & Activities:
In 2017, the Division of Biostatistics helped bring in over $152 million dollars to the Medical College of Wisconsin from various
grants they were included on. In calendar year 2017, the Division published 14 methodological papers that appeared in the
statistical literature either online or in print. The Biostatistics Consulting Service collaborated on 430 projects which resulted
in 73 Publications. Of those 430 projects, 70 were grant preparation.
Research Support Services Available:
The Biostatistics Consulting Service can handle projects requiring expertise in any area of statistic, such as:
Useful Links:
Division of Biostatistics websites
Biostatistics Faculty
Biostatistics MCW YouTube Page
Methodological Research Areas
Survival Analysis
Clinical Trials
Bayesian Methodology
Image Analysis
Multiple Comparisons
Statistical Modeling
Big Data Methods
Statistical Genetics/
Bioinformatics
Precision Medicine
Collaborative Research Areas
CIBMTR
PCOR
Genomic Sciences and
Precision Medicne Center
(GSPMC)
Cardiovascular Center (CVC)
Dept of Orthopedic
Surgery
Dept of Medicine
Cancer Center (CC)
•Sample size determination
•Grant proposal preparation
•Assistance with study design
•Help with funding proposals
•Modeling
•Randomization
•Design of clinical trials
•Analysis of experimental data
•Statistical graphics
•Interpretation of results
•Help with data management
•Assistance with manuscripts
Pediatric Emergency
Medicine
Dept of Hematology /
Oncology
Dept of Phys Med &
Rehabilitation
Froedtert Hospital
Pharmacy
Dept of Surgery

MCW Research Overview
Jump to Table of Contents 189
Center for Bioethics and Medical Humanities
The Center for Bioethics and Medical Humanities (CBMH) has pursued a variety of interdisciplinary research and scholarly
activities since its establishment in the early 1980s. This commitment to research and scholarship continues today and will
be a part of the CBMH’s future endeavors. Past research activities and scholarship by CBMH faculty have addressed a wide
range of bioethics issues, including discovery and dissemination of new knowledge and best practices for addressing and
managing the ethical concerns raised in research and clinical application of new genetic technologies; patient refusal of
recommended treatment in the emergency department; responses to law enforcement demands of health care personnel,
comparing clinical consent and research consent; political authority in a bioterror emergency; vaccination and objection; and,
disabling cardiac devices.
Currently, CBMH faculty are engaged in research aimed at developing a conceptual framework for health equity, analyzing
ethical implications of contributing factors and interventions to address health disparities, constructing a flexible curriculum
for community engaged research as an alternative to CITI training and also creating simple, strong consent translation
policies; examining the attitudes and personal expectations concerning psychiatric advance directives of stakeholders; and,
examining the ethical, legal/regulatory and social issues arising from the use of neuroimaging biomarkers as a new diagnostic
tool for Alzheimer’s Disease in asymptomatic individuals.
CBMH faculty provide research ethics consultation services to investigators before, during, and after engaging in research
activities. CBMH faculty and staff also serve as members and leaders of a number of Froedtert and the Medical College of
Wisconsin institutional review boards.
Faculty Scholarly Expertise
• Arthur R. Derse, MD, JD, Professor and Director – Informed consent; decision making capacity; medical futility;
ethics in emergency medicine; legal issues in end of life care; ethics and humanities in medical education; health
care ethics committees and ethics case consultation.
• Mary Homan, MA, MSHCE, DrPH, Assistant Professor – Pediatric ethics; public health ethics; social justice;
vulnerable populations; health equity.
• Fabrice Jotterand, PhD, MA, Associate Professor – Neuroethics; ethical issues in psychiatry and mental health; the
use of neurotechnologies in psychiatry; medical professionalism; neurotechnologies and human identity; and
bioethics and moral/political philosophy (justice and health care).
• Cynthiane Morgenweck, MD, MA, Associate Professor – Ethical issues and the surgical experience; informed
consent; clinical trials and placebo surgery; treatment limitation during procedures, including use of cardiac
devices; spirituality in medicine; and ethics case consultation.
• Ryan Spellecy, PhD, Professor – Research ethics and scientific integrity; community engaged research ethics,
informed consent in research; advance directives; psychiatric advance directives; ethics and mental health care;
pediatric ethics; exception from informed consent in emergency research.
• Julia A. Uihlein, MA, Assistant Professor – Humanities in medical education; ethical issues in pediatrics

MCW Research Overview
Jump to Table of Contents 190
Division of Epidemiology
The Division of Epidemiology is comprised of five faculty members, four postdoctoral fellows and twelve staff members.
Members of the Division engage in a wide variety of research and education activities and collaborate with a multitude of
internal and external partners, both locally and globally.
Laura Cassidy, MS, PhD
Dr. Cassidy concentrates much of her research on pediatric trauma. She directs the Epidemiology Data Resource Center. Dr.
Cassidy partners with many researches across MCW and assists with sampling, survey design, and registry development.
Kirsten Beyer, MPH, PHD, MS
Dr. Beyer’s current research focuses on the impacts of neighborhood environmental characteristics such as residential racial
segregation and green space on cancer outcomes, particularly through pathways that include stress, time spent outdoors,
social interaction, and food and physical activity behaviors. Dr. Beyer’s work includes disease mapping, social and spatial
epidemiology, and mixed methods approaches that aim to identify spatial patterns of disease and injury and understand the
complex human-environment processes that create them. Her goal is to conduct research that leads to the development of
community-based interventions and policies to reduce health disparities. Her primary research project (NIH R01CA214805)
is focused on the contemporary problems of institutional racism and residential racial segregation, and investigates whether
these social structures contribute to the magnitude of racial and ethnic breast cancer survival disparities. The project uses a
community engaged research framework that draws upon existing partnerships with community organizations in Milwaukee,
WI, which often tops the list of America’s most segregated cities.
Mallory O'Brien, MS, PhD
Dr. Mallory O’Brien is the Founding Director of the Milwaukee Homicide Review Commission (MHRC) and DataShare, an
integrated data system for Milwaukee, linking public health, public safety and education data to improve the lives of
Milwaukee residents. Dr. O’Brien participates in death reviews and conducts trainings across the country on these reviews.
She is working on a variety of research projects on violence prevention and firearm use funded by both federal agencies and
private foundations. Dr. O’Brien is using her extensive experience to partner with the State of WI to develop opioid overdose
reviews and sexual assault reviews.
Matt Dellinger, MS, PhD
Dr. Dellinger has collaborated with ITCM and ITFAP on fish consumption outreach since 2004 and is a recognized researcher
in the Great Lakes region. He a co-investigator and active member of the Great Lakes Native American Research Center for
Health (GLNARCH) Community Scientific Advisory Committee and the Bemidji Area Environmental Public Health Advisory
Committee. He has worked extensively with Native American youth education programs through digital storytelling and art,
combining academic research and cultural perspectives. His current initiatives include: digital storytelling as a tool for
exposure reduction to toxic chemicals (NIH R21 11765725), GLNARCH outreach, and adapting mobile technology to improve
environmental health literacy. He was recently award an R01 through NIEHS entitled “Gigiigooinaan (Our Fish): A New
Advisory to Promote Anishinaabe Health and Wellness”

MCW Research Overview
Jump to Table of Contents 191
Community Health Division Research
Full-time Research Faculty
• Jessica Olson, PhD, MPH, Assistant Professor: research expertise in breast neoplasms, microRNAs, cardiovascular
diseases, women’s health, and healthcare disparities
• John Meurer, MD, MBA, Professor, Director of the Institute for Health & Equity, and Co-Director of the Primary
Care Research Fellowship: research expertise in early childhood development systems improvement
Recent Publications
More than a Conversation: the Power of Bringing Scientists and the Community Together to Change Perceptions About
Cancer. (Olson J, Svoboda-Newman S, Gardner-Volle K, McNally M, Fabian E, Maurana C) J Cancer Educ 2019 Jun;34(3):571-
576
Serum S100A8/A9 and S100A12 Levels in Children With Polyarticular Forms of Juvenile Idiopathic Arthritis: Relationship to
Maintenance of Clinically Inactive Disease During Anti-Tumor Necrosis Factor Therapy and Occurrence of Disease Flare After
Discontinuation of Therapy. (Hinze CH, Foell D, Johnson AL, Spalding SJ, Gottlieb BS, Morris PW, Kimura Y, Onel K, Li SC,
Grom AA, Taylor J, Brunner HI, Huggins JL, Nocton JJ, Haines KA, Edelheit BS, Shishov M, Jung LK, Williams CB, Tesher MS,
Costanzo DM, Zemel LS, Dare JA, Passo MH, Ede KC, Olson JC, … Lovell DJ) Arthritis Rheumatol 2019 Mar;71(3):451-459
Community Breast Health Education for Immigrants and Refugees: Lessons Learned in Outreach Efforts to Reduce Cancer
Disparities. (Kamaraju S, Olson J, DeNomie M, Visotcky A, Banerjee A, Asan O, Tavares E, Rao A, LaCroix M, Krause K,
Neuner J, Stolley M) J Cancer Educ 2018 Aug 09
Fatty Acids in Ten Species of Fish Commonly Consumed by the Anishinaabe of the Upper Great Lakes.(Dellinger MJ, Olson
J, Holub B, Ripley MP) J Great Lakes Res 2018 Jun;44(3):521-526
Precision Medicine and Precision Public Health: Academic Education and Community Engagement. (Meurer JR, Whittle JC,
Lamb KM, Kosasih MA, Dwinell MR, Urrutia RA) Am J Prev Med 2019 Aug;57(2):286-289
Student Leadership Development Initiative: A Pilot for a Sustainable, Replicable Model for Incorporating Leadership into
Medical Education. (Idso JM, Helmen ZM, Hueston WJ, Meurer JR) WMJ 2019 Apr;118(1):39-41
Non-parametric recurrent events analysis with BART and an application to the hospital admissions of patients with
diabetes. (Sparapani RA, Rein LE, Tarima SS, Jackson TA, Meurer JR) Biostatistics 2018 Jul 28

MCW Research Overview
Jump to Table of Contents 192
National Biomedical EPR Center
Founding Director: James S. Hyde, PhD
Current Director: Candice S. Klug, PhD
The National Biomedical Electron Paramagnetic Resonance (EPR) Center at MCW is the largest EPR facility in the nation. The
National Institutes of Health (NIH) has made an enormous investment in EPR research at MCW over the past four decades.
Most significantly, the NIH funded the EPR Center as a P41 Research Resource for more than 40 years to develop “the most
extensive and advanced biomedical-oriented EPR facility in the world, with a complete range of EPR equipment, an
engineering/development staff capable of steadily and significantly advancing the state-of-the-art technology for biomedical
applications of EPR spectroscopy, and a scientific staff with broad experience across many fields.”
EPR spectroscopy is a critically important technique in biomedical research. The fundamental power of EPR is its unique ability
to detect unpaired electrons, either naturally occurring or engineered through site-specific labeling, in complex biological
environments and its wide-ranging applicability to biomedically important areas of research such as structural biology,
metalloproteins, redox biology, and rational drug design. EPR is also ideally suited to dynamic studies as the wide array of
EPR technologies that have been developed at MCW and elsewhere span the entire picosecond to millisecond timescale of
protein motion. EPR also provides detailed structural information on proteins, from helical rocking modes and loop
fluctuations to large-scale tertiary rearrangements and protein-protein and protein-ligand interactions. In comparison with
other biophysical approaches such as NMR (nuclear magnetic resonance) and fluorescence-based methods, EPR has distinct
advantages in its ability to directly detect an unpaired electron attached to a protein in any environment, including
macromolecular complexes, membrane proteins in their native lipid environments, distinct populations of protein states
exchanging on the microsecond timescale, and on limited samples using short acquisition times. EPR technology also is central
to characterizing metalloprotein structure and function, is a gold standard for the detection of biological free radicals in redox
biology, and is a powerful method to reveal free radical and metalloprotein signatures in tumor and tissue samples as a
diagnostic tool.
An impressive array of custom-built and commercial instrumentation is housed within the National Biomedical EPR Center in
the Department of Biophysics at MCW. Our resources and expertise are available to scientists at MCW, regionally, nationally,
and internationally. To take advantage of our instrumentation resources or collaborate with our faculty and engineers, learn
more on our website: https://www.mcw.edu/departments/national-biomedical-epr-center.

MCW Research Overview
Jump to Table of Contents 193
Neuroscience Research Center
The mission of the Neuroscience Research Center (NRC)
is to facilitate the discovery and translation of new
knowledge in the neurosciences, with a focus on
discoveries that will improve the health of the
communities served by our clinical programs.
Overall Goals:
1. Impactful research. The NRC is made up of outstanding biomedical scientists who are experts in neuroscience knowledge,
and are carrying out research projects that are supported by extramural funding and have the potential to improve the health
of the communities we serve.
2. Leverage resources through collaboration. NRC scientists are engaging in collaborative research projects that bring
scientists with complementary expertise and interests together, promoting collegiality, sharing of data and ideas, and raising
the caliber of research of all participants.
3. Provide support. NRC members have access to high quality support staff, seed funding, statistical support, equipment and
expertise to carry out their research.
How does this help me?
As part of our strategic initiatives, the NRC hosts seminars, data sharing events, research in progress and symposia, all with
the goal of providing MCW faculty, students, staff and fellows up-to-date knowledge and connecting members for the
purposes of collaboration.
The NRC has established a Rodent Behavioral Core that is available to all MCW investigators. The core is equipped with
apparati and software for the measurement of simple and complex rodent behaviors using tests such as the elevated plus
maze, open field, radial arm mazes, prepulse inhibition, and fear conditioning.
The NRC also runs a Microscopy Core with Multiphoton Microscope services and a Leica Sp8 Confocal Microscope. More
information and the ability to book our equipment is available on iLab.
Please visit our Intranet area on Infoscope for details on our cores, grant opportunities and membership:
https://infoscope.mcw.edu/NRC-Intranet.htm
If you are interested in becoming a member of the NRC and receiving email updates of seminars, events and grant
opportunities, please contact Betsy Wriedt at ewriedt@mcw.edu.

MCW Research Overview
Jump to Table of Contents 194
Research Computing Center
The Research Computing Center (RCC) provides the infrastructure and campus-wide access to high performance computing
(HPC) resources required for computationally-intensive biomedical research. RCC is institutionally supported and available to
all MCW students, staff, and faculty. RCC services and operations are governed by representatives of the MCW Faculty in
partnership with RCC leadership.
Services
HPC:
RCC maintains a Linux-based HPC cluster ideal for both massively parallel and high throughput workloads.
• 50 nodes
• 1200 cores
• 44 GPUs
• 10TB of memory
• Infiniband Interconnect
Storage:
RCC also provides petascale data storage to support both data-intensive computing and long-term retention.
• High-performance parallel file system
• Long-term storage for completed projects
• 10GigE interconnect
Consulting:
RCC provides consulting services for users, groups, and projects regarding a variety of research computing related topics.
• Training on HPC systems
• Software installation and setup
• End-user support and trouble-shooting
• Grant assistance and boilerplate language
• Consulting on IT needs of computational research projects
Staff and Facilities:
RCC has full-time dedicated staff with extensive experience in system administration and computational research. All
hardware is housed in professionally managed MCW datacenters. RCC also collaborates with and is supported by MCW’s
excellent central IT teams.
• 2 Datacenters
o Redundant power and cooling
o Biometric access control
• Professional staff
o Experience in research computing, system administration, network, and security

MCW Research Overview
Jump to Table of Contents 195
Crash Injury Research Engineering Network
Narrative: The CIREN center contributes to the National Highway
Traffic Safety Administration’s (NHTSA) mission to prevent and
reduce deaths, injuries and economic losses resulting from motor
vehicle travel on our nation’s roadways. The CIREN Center at
MCW is one of seven national centers. It conducts crash injury
research collecting and analyzing relevant data in the interest of
public health. Real-world crashes are investigated to further the following objectives: Reconstruct and understand crash
and injury causation, improve prognosis and treatment for crash trauma patients, reduce time of recovery and treatment
costs, simulate crash scenarios in laboratory environment, disseminate data to industry, regulatory, and public agencies,
develop strategies to reduce fatalities and injuries in automobile accidents, provide information to improve public
infrastructure to reduce accidents, develop and disseminate safety messages to the public and train health care providers in
vehicular safety and associated care.
Available Equipment: FARO 3D LIDAR scanner
Contact:
Dale Halloway
Program manager
(414) 384-2000 x47171

MCW Research Overview
Jump to Table of Contents 196
Versiti Blood Research Institute
From its beginning in 1947, Versiti (formerly known as BloodCenter of
Wisconsin), has supported basic, translational, and clinical research to
advance patient care. Research at Versiti today excels in Thrombosis,
Hemostasis and Vascular Biology, Immunobiology, Transfusion Medicine,
and Stem Cell Biology. Research activities are housed primarily in the Blood
Research Institute (BRI) on the Milwaukee Regional Medical Center (MRMC)
adjacent to the Medical College of Wisconsin (MCW), an 87,000 sq. ft.
facility. The BRI is home to 34 investigators and more than 120 research staff, including fellows, graduate students,
technologists, and administrative personnel. Total extramural funding for research in 2018 was $16.1 million, including a
Training Grant in Transfusion Medicine, currently in its 40
th
year, which provides stipends for outstanding postdoctoral fellows
engaged in NIH-funded research.
BRI research in Thrombosis, Hemostasis and Vascular Biology focuses on the cellular and molecular mechanisms of normal
blood clotting, pathological thrombosis and event impacting the integrity of vascular and blood vessel development. Studies
have given rise to a number of important breakthroughs in understanding mechanisms of the regulation of blood clotting.
The work of our clinical investigators has led to improved outcomes for patients with blood-related diseases including Sickle
Cell Disease, Hemophilia, and von Willebrand Disease. Research in Transfusion Medicine focuses on immune responses to
transfused blood and the underlying immunologic mechanisms as well as practices related to blood storage and safety.
Currently, investigators in this area focus on the basic biology and clinical implications of a wide range of transfusion-related
issues. Historically, Versiti research in Immunobiology focused on understanding the mechanisms involved in
antibody/antigen recognition. Versiti investigators played an important role in the first allogeneic bone marrow transplant
performed at Children’s Hospital of Wisconsin and the creation of the national marrow donor program. Today, BRI
investigators are exploring the immune system in a variety of areas, including neuro-immunology, T- and B-cell development
and regulation and the development of cell-based immunotherapies targeted to malignant hematopoietic and solid tumors.
The Translational Glycomics Center focuses on the important and understudied role sugars play in the biology and
pathobiology of various blood cells. The Translational GlycOmics K12 Program, part of the National Career Development
Consortium for Excellence in Glycosciences, trains emerging generations of researchers to pursue basic and applied
glycobiology research. Stem Cell Biology is the newest and fastest-growing area of research at the BRI with studies focused
on transcriptional and epigenetic regulation of stem cells and normal/malignant hematopoiesis biology.
In addition to its research laboratories, the BRI maintains 12 state-of-the-art Core Laboratories within the BRI, which provide
cutting-edge technology and expertise to BRI investigators and others on the MRMC campus. Core Labs include Biophysics,
Histology, Hybridoma, Microscopic Imaging, Molecular Biology, Protein Chemistry, Viral Vector, Thrombosis, and Flow
Cytometry. The Cores are supported by a PhD-level Director, who oversees a staff of experienced, cross-trained technologists
available for consultation with researchers on experimental design and data analysis related to products and services
provided by the Core Labs. In addition, the BRI provides expertise in Transgenic Mouse production and maintenance and in
Gene Editing and Bioinformatics. Finally, the BRI houses a fully staffed Clinical Trials Research Office.

MCW Research Overview
Jump to Table of Contents 197
Biochemistry
The research interests of our faculty span a broad spectrum of biochemistry ranging from cell and developmental biology to
structural biology. The unifying theme defining us is an interest in biological processes at the molecular level. The department
is home to state of the art facilities and instruments for X-ray crystallography, NMR spectroscopy, mass spectrometry,
fluorescence microscopy, to name just a few. A collaborative and collegial atmosphere makes the Biochemistry Department
an ideal place to do science and train for a wide variety of biomedical science careers.
Research Facilities
BIAcore 3000 Instrument: The BIAcore 3000 instrument integrates surface plasmon resonance (SPR) technology with a
microfluidics system to monitor molecular interactions in real time at concentrations ranging from pM to mM. This label-free
technology can detect a wide range of molecular masses from 180Da to >1000kDa. The high sensitivity and high through-put
capabilities allows for the detection of drug-protein, hormone-protein, protein-protein, DNA-protein, carbohydrate-protein,
and lipid-protein interactions. The ability to interface with mass spectrometers provides discovery-based research in
proteomic studies. For more information about SPR technology, theory, and applications, please see the attached BIAcore
presentation (PDF).
The BIAcore 3000 instrument is housed in the Department of Biochemistry and is available to all Medical College of Wisconsin
faculty and staff who have been trained and demonstrate the ability to use microfluidic-based instrumentation. Training and
consultation are available on an appointment basis.
For more information contact:
Nancy Dahms, PhD
(414) 955-4698 | [email protected]
Biomolecular NMR at MCW: 600 MHz NMR spectrometer.
Cryoplatform is visible to the left of the magnet, RF
console and workstation to the right. The NMR Facility is
an interdepartmental research service unit located in the
Biochemistry Department. High-field NMR spectroscopy is
a powerful technique for the study of biomolecular
structure and dynamics. The facility provides service for
routine 1D and 2D NMR methods, and can also provide
consultation and collaborative assistance with the
acquisition and analysis of multidimensional, multinuclear
protein NMR spectra. The facility operates two Bruker 600
MHz and one 500 MHz NMR spectrometers, each
equipped with 1H/13C/15N cryoprobes for enhanced
sensitivity in biomolecular applications. In addition, a
Bruker 300 MHz NMR spectrometer is available for routine
analytical NMR of small molecules. For some long-term projects, the facility provides training for instrument operation and
data analysis to investigators and research personnel. The facility operates on a fee-for-service basis and is open to faculty of
the Medical College of Wisconsin and outside researchers.
Brian Volkman, PhD
[email protected] | (414) 955-8400
Francis Peterson, PhD

MCW Research Overview
Jump to Table of Contents 198
MCW Research Overview: Basic Science Departments
Macromolecular X-Ray Crystallography Facility
Automated Crystallization Systems: Hamilton (left) and Phoenix crystallizers (right)
In-house X-ray Diffraction Laboratory (left) and Graphics Workstations (right)
The department houses state-of-the-art instrumentation dedicated to Structural Biology research. The facility includes
chromatographic systems for protein purification, an in-house X-ray diffraction core and an automated crystallization system
for high-throughput screening and optimization. High-end computer workstations have been set up for 3-D graphic
visualization and crystallographic analysis.
The X-ray facility is located on the second floor of the Translational Biomedical Research Center (TBRC). The facility houses
an X-ray diffraction system consisting of a Rigaku R-AXIS IV++ image plate detector system and MicroMax 007 generator
equipped with Osmic confocal mirrors and an X-treme crystal cryocooler. The crystallization system includes a Hamilton STAR
for solution making and a Phoenix equipped with a CrysCam for nanoliter crystallization and visualization. A fully automatic
crystal incubator/imager (crystallization hotel) will soon be added to enhance throughput capacity.
The facility is open to faculty members of the Medical College of Wisconsin. Various levels of training are available and
collaborative arrangements can be made to scientists both inside and outside of the MCW community.
Jianhua Fu, PhD
[email protected] | (414) 955-5849
Jung-Ja Kim, PhD
[email protected] | (414) 955-8479

MCW Research Overview
Jump to Table of Contents 199
Shared Research Instrumentation
The Biochemistry Department maintains several instruments for isolation and physical characterization of biomolecules and
detection of their interactions. All are located on the second floor of the TBRC and include:
Jasco J-710 Circular dichroism spectropolarimeter
The Jasco J-710 circular dichroism (CD) spectropolarimeter is equipped with a thermally regulated sample compartment.
Monitoring of the far-UV and/or near-UV CD spectra can provide valuable information about the secondary structure,
thermal stability, or conformational state of a protein.
Contact: Nolan Kennedy, n[email protected]
Photon Technologies Inc. QuantaMaster™ spectrofluorometer
The QuantaMaster™ spectrofluorometer is outfitted with dual excitation and emission monochromators for high sensitivity,
a thermally regulated sample compartment, and Glan Thompson polarizers for fluorescence anisotropy measurements. The
instrument is suitable for emission/excitation scanning experiments, fluorescence experiments requiring synchronous
scanning of the excitation and emission monochromators, time based fluorescence measurements, fluorescence resonance
energy transfer experiments and fluorescence anisotropy measurements.
Contact: Francis Peterson, fpeterso@mcw.edu | Davin Jensen, djensen@mcw.edu
MicroCal VP - Isothermal Titration Calorimetry
The MicroCal VP-ITC is capable of measuring heat evolution as little as 0.4 nanoJ/sec. This instrument is suitable for the
studies of protein-ligand and protein-protein interactions and provides the biochemists with reliable measurements of
binding constants in the range of 10
3
-10
9
M
-1
as well as the enthalpy and stoichiometry of interactions. ITC is a preferred
technique to demonstrate the interaction between newly discovered binding partners in vitro.
Contact: Brian Smith, brismith@mcw.edu
Perseptive Biosystems Voyager DE-Pro MALDI mass spectrometer
The matrix-assisted laser desorption ionization (MALDI) mass spectrometer is used for routine mass determination of
peptides, proteins and other macromolecules.
Contact: Davin Jensen, [email protected]
Promega Maxwell-16 robot
This benchtop instrument provides fast automation of routine DNA, RNA or protein extractions resulting in reproducible
yields and purity. Parallel multi-channel operation permit automated purification of milligram yields of up to 16 different
recombinant proteins in less than one hour.
Contact: Davin Jensen, [email protected]
Molecular Devices Flexstation 3 microplate reader
This benchtop instrument is a 5-mode microplate reader for use in a wide range of biochemical- and cell-based assays for
basic research and drug discovery. This instrument is equipped with an 8-channel pipettor for 96-well-based assays based
on absorbance, fluorescence intensity, fluorescence polarization, luminescence, and time-resolved fluorescence assays. It
has high-efficiency tunable monochromator optics and a dedicated photomultiplier tube for luminescence assays.
Contact: Chad Koplinski, ckoplinski@mcw.edu | Francis Peterson, fpeterso@mcw.edu
MCW Research Overview
Jump to Table of Contents 200
Biochemistry Program in Chemical Biology
The Program in Chemical Biology (PCB) provides resources in structure-based drug
design, protein production, and organic synthesis to the MCW community for chemical
biology and medicinal chemistry projects. The PCB is a valuable resource for faculty
throughout the MCW research environment, supporting projects from the departments
of Biochemistry, Biophysics, Cell Biology, Medicine, Microbiology and Immunology,
Pharmacology and Toxicology, and Pediatrics. Collaborating centers and programs include
the Cardiovascular Center, Cancer Center, Center for Infectious Disease Research,
Genomic Sciences & Precision Medicine Center, National Biomedical EPR Center,
Neuroscience Research Center, Research Computing Center, and Redox Biology Program. Different focus groups within the
PCB meet weekly to discuss the progress of active projects and evaluate new collaborative opportunities. The PCB
encourages investigators interested in the development and use of small molecules for basic and translational research to
take advantage of its capabilities which include:
• Small-molecule library screening using NMR and other biophysical techniques
• Recombinant protein expression and purification
• Organic synthesis
• Computational docking and homology modeling of proteins and small-molecule:protein interactions
For more information or discussion contact:
Dr. Brian Volkman, Director ([email protected], (414) 955-8400)
Dr. Brian Smith, Associate Director (bris[email protected], (414) 955-5669)

MCW Research Overview
Jump to Table of Contents 201
Biomedical Engineering
The Joint Biomedical Engineering Department (Joint Department) between Marquette University and the Medical College of
Wisconsin provides a unique opportunity to grow southeast Wisconsin’s biomedical engineering capabilities and reputation.
Biomedical engineering is a multidisciplinary approach to improving health care by integrating education, research, patient
care, and industry. The Joint Department presents many opportunities, investments and returns for various stakeholders
including students, faculty, institutional and college leaders, donors, investors and industry partners.
Our mission is to serve our institutions, our community, and the world by applying engineering approaches to solving critical
unmet medical needs.
Clinical Collaborations
Help us to apply our newly developed technologies and discoveries so they can be used in clinical decision making. Clinical
collaborators include:
• Versiti
• Otolaryngology-MCW
• Radiology-MCW
• Ophthalmology-MCW
• Physical Medicine and Rehabilitation-MCW
• Neurology-MCW
• Neurosurgery-MCW
• Herma Heart Center & the Pediatric Genetics Groups at Children’s Hospital of WI
• VA Medical Center
Imaging
Departmental research groups develop imaging systems or applications that cover many different modalities such as:
• CT
• Micro CT
• SPECT
• Fluoroscopy
• MRI and fMRI
Applications include imaging brain function and lung cellular activity
Analytics, Informatics & Software Engineering
Biomedical engineers work at the interface between computer and software engineering and the biomedical computational
sciences. They conduct computational research, innovation and visualization in the areas of genomics, other areas of
molecular sciences, and neuroscience
Crash Injury & Research Engineering Network
Real-world crashes are investigated to further the following objectives:
• Reconstruct and understand causation
• Improve prognosis and treatment for crash trauma patients
• Reduce time of recovery and treatment costs
• Disseminate data to industry, regulatory, and public agencies
• Develop strategies to reduce fatalities and injuries in automobile crashes
• Provide information to improve public infrastructure

MCW Research Overview
Jump to Table of Contents 202
Neurosystems & Neurorehabilitation
These research groups focus on the brain, nervous system, and motor control. They study aspects of neuroscience and
neuromuscular control as they relate to normal function and in conditions like stroke rehabilitation and multiple sclerosis.
Orthopaedics & Orthopaedic Rehabilitation
Researchers in this area study human motion and musculoskeletal physiology as it relates to human health and disease. They
also perform clinical research in the areas of orthopaedic surgery and physical medicine and rehabilitation using biomedical
engineering analysis methods, modeling, and instrumentation. This area also includes innovative prosthetic design and
analysis to reduce crashes, develop and disseminate safety messages to the public, and train health care providers in vehicular
safety and associated care.
Computational Biology & Systems Biology
Biomedical engineering specializes in understanding complex, interacting systems using the tools of Systems Biology.
Integrating protein and metabolic function from molecule to the whole person involves many sophisticated models of how
biological systems work and how computational science can be used to better understand them. Systems Biology
incorporates computational models of huge networks of proteins, molecules, and genes to identify how they work together
and allows our faculty and students to work in a broad array of new and exciting areas. Our faculty use a systems approach
to study cardiovascular, pulmonary, neurological and skeletal biological diseases.
Cardiovascular & Pulmonary
Investigators in this area use high performance computing and modeling, as well as imaging to study the mechanical and
physiological aspects of vascular and respiratory function to fight:
• Heart disease
• Hypertension
• Diabetes
• acute lung injury
Medical Device Innovation
Medical devices are at the heart of biomedical engineering. Innovations from our faculty and students have ranged from
instruments to computer algorithms. Our group works closely with physicians and research scientists to translate ideas into
devices.
GOALS:
• Develop new, highly innovative and translational programmatic areas of international excellence through
collaboration with our partner institutions.
• Support entrepreneurial and industry activities that result in bringing biomedical engineering innovations to
market
• Create seed funding to support developmental research using technological innovation to solve unmet clinical
needs both globally and in our own community
Our faculty, staff, and students continuously strive to further advance the Joint Department’s mission and enhance the impact
of our discoveries and technology developments. Through their dedication and effort, the Joint Department will continue to
contribute to scientific advances in biomedical research and explore clinical applications at the Medical College of Wisconsin
and Marquette University.

MCW Research Overview
Jump to Table of Contents 203
Biophysics
The Department of Biophysics at MCW is dedicated to excellence in research and
graduate and postdoctoral training. The research interests of our faculty are broadly
based, with strong, innovative research programs in electronic paramagnetic
resonance (EPR), redox, and magnetic resonance (MR) physics and brain imaging.
The Department of Biophysics has state-of-the-art facilities and equipment geared
toward these programs. The department houses chemical and biochemical labs, two
tissue culture labs, an engineering complex, a microwave lab, five EPR spectroscopy
labs, and a machine shop.
EPR Research
The National Biomedical EPR Center at MCW is the most extensive EPR facility in the
nation. It was supported by an NIH P41 research resource award from 1976 to 2019.
The research conducted within the EPR Center includes technological innovation and
application of new techniques to biological problems. The main areas of research are
spin labeling of proteins and lipids, structural and conformational changes of
proteins, redox changes at the active site of metallo-proteins, and oxidants and free
radical formation in tumorigenesis and tumor progression and in drug resistance in
cancer. The EPR Center houses an array of internally developed and commercial EPR
instrumentation, a specialized engineering/development staff capable of steadily
and significantly advancing the state-of-the-art technology for biomedical
applications of EPR spectroscopy, and a scientific staff with broad expertise.
Redox Research
Scientists in the Department of Biophysics are internationally recognized for their expertise and contribution to the field of
free radical and redox biology. The main research focus is on establishing the role of free radicals and oxidants in
pathophysiological conditions (e.g., in cardiovascular diseases, neurodegeneration, and cancer) and in normal cell function.
The department provides an environment for development of novel, rigorous chemical probes and assays for monitoring the
generation of free radicals in cells (in vitro) and in animals (in vivo). These include fluorogenic and bioluminescent probes,
EPR spin traps and probe-free assays (e.g., redox immunoblotting [peroxiredoxins, thioredoxins] and low-temperature EPR
studies of the redox status of cellular protein metal centers). Ongoing collaborative work within MCW (e.g., Cardiovascular
Center, Cancer Center) and with other institutions utilizes these assays to understand role of oxidants in cardiovascular
diseases (e.g., stroke, ischemia-reperfusion), neurodegeneration (e.g., Parkinson Disease), and cancer (e.g., cancer cell
proliferation, chemoprevention, and chemotherapy).
MR Physics & Brain Imaging Research
MCW Biophysics scientists have been engaged in MRI/functional MRI (fMRI) research for more than 25 years, publishing the
first paper on fMRI in 1992 and on resting-state fMRI in 1995. The widely used fMRI software program AFNI (Analysis of
Functional NeuroImages) was developed in Biophysics in 1994. Imaging technology development has been a hallmark in
Biophysics, beginning with the introduction of the local gradient coil for fMRI; the current emphasis is on applications to
neurological and psychiatric disorders (e.g., early disease detection, precision disease prevention, prediction of disease

MCW Research Overview
Jump to Table of Contents 204
development, and assessment of treatment efficacy in Alzheimer’s disease research). Strong interdisciplinary collaborations
exist, centering on chronic pain mechanisms, psychiatric depression, and other fields in neuroscience.
Biophysics Graduate Program
The Biophysics Graduate Program features two primary areas of research: Magnetic Resonance Imaging and Molecular
Biophysics. Our program is designed to assist young scientists in developing the research skills they need to thrive in academic
and clinical settings. The Magnetic Resonance Imaging track places emphasis on MRI and MRS (magnetic resonance
spectroscopy); fMRI of the human brain is an active research area (neuroscience, contrast mechanisms, technical
development). The Molecular Biophysics track encompasses the investigation, detection, and use of free radicals and
paramagnetic metal ions in biological systems using EPR spectroscopy. Students with more of a physical background may
specialize in EPR instrumentation.
Centers
The Department of Biophysics is home to the Free Radical Research Center, National Biomedical EPR Center, Redox and
Bioenergetics Shared Resource, and Redox Biology Program.
More Information
For more information about the department of Biophysics, visit our website.
(http://www.mcw.edu/departments/biophysics.htm).

MCW Research Overview
Jump to Table of Contents 205
Cell Biology, Neurobiology, and Anatomy
Cell Biology, Neurobiology & Anatomy (CBNA) is one of the six Basic Science Research departments at MCW. CBNA faculty
members and graduate trainees conduct fundamental research in the areas of cell biology, developmental biology and
neuroscience, with expertise covering the brain, gastrointestinal tract, liver, retina and heart. Our Department is home to the
Cell & Developmental Biology graduate training program as well as the Neuroscience Graduate program, and we prioritize
the ability of our trainees to gain experience to a variety of cutting-edge methods from single molecule to whole organism
assays and present their results at national meetings.
CBNA’s traditional focus on developmental pathway mechanisms caused it to evolve a major emphasis on stem cell biology,
and its potential for regenerative medicine, during the past decade. CBNA is home to MCW’s Program in Regenerative
Medicine and Stem Cell Biology, which utilizes pluripotent stem cells to study pathways of normal development and disease.
The Department has current expertise in neural, gastrointestinal, liver, and cardiovascular stem cell models.
CBNA faculty members also play an essential role in the Medical School’s Discovery Curriculum courses, including the first
year Clinical Human Anatomy, Medical Neuroscience and Molecules to Cells courses, as well as several second-year courses.
In 2018, we are delighted to welcome several new Faculty to MCW, who will enhance collaborative projects across our basic
and clinical enterprise, and bring new technologies and capabilities to campus For further information, please visit our
department website: http://www.mcw.edu/cellbiology.htm

MCW Research Overview
Jump to Table of Contents 206
Microbiology & Immunology
Faculty research spans a broad range of interests including, viral and bacterial infection and pathogenesis, inflammation and
immunology, enzymology and metabolism, molecular genetics, and signaling and gene expression. Our faculty address
questions at the cellular and molecular level, using contemporary technology and approaches where more than 30-faculty
serve as graduate student research mentors. Many graduates of our Program conduct postdoctoral studies and then serve
as faculty at academic medical centers or scientists in research institutes, industry, and government.
Microbiology & Immunology
Departmental bacteriologists study a variety of organisms and topics, which include the identification and characterization
of the delivery, trafficking and function of bacterial toxins that target key cellular processes of the eukaryotic host. Toxins
under study include the botulinum and tetanus neurotoxins, and the ExoS and ExoU type-III effectors encoded by
Pseudomonas aeruginosa. A variety of genetic, cell biological, biochemical, and structural approaches support the study of
the biological functions of these toxins. Moreover, the toxins themselves and delivery machinery are components of potential
vaccines. Faculty research interests also address intrinsic antibiotic resistance in Gram-positive bacteria such as E. faecalis
where one major areas of study is a kinase/phosphatase system that mediates resistance to the cephalosporin family of
antibiotics. Other faculty study host-pathogen interactions of spirochetes.
Departmental virologists study different research topics on members of the herpesvirus family. These topics include studies
on the immune evasions encoded by human herpesvirus 6 and 7, host/ human cytomegalovirus interactions, using a
combination of virology and mass spectrometry. MHV68, a mouse pathogen which is similar to the KSHV and EBV viruses that
infect humans is also studied to understand the host DNA damage response and the interferon system to infection, and in
how these viruses cause hematological malignancies.
Departmental immunologists address various aspects of the immune system. These topics include the study of chemokines,
which are chemotactic cytokines that can affect the homing of various cell types to different organs. This work focuses on
how the expression of chemokines and chemokine receptors affects tumor progression and metastasis; pancreatic cancer
and other high-risk malignancies are a particular focus. Other studies address how the immune system combats infections by
bacteria that establish granulomatous lesions, as seen in tuberculosis. These studies address the role of the cytokine IL12 and
its cognate receptor. Departmental molecular geneticists’ study various aspects of gene expression and fundamental cell
biology. These studies focus on how differential mRNA splicing and polyadenylation regulate gene expression and modulate
viral and cellular behavior, while other studies address mRNA localization, and the role of localization on cell fate, and studies
essential cellular proteins that regulate mitochondrial protein import and lipid composition.
Center for Immunology
The Center for Immunology Program consists of a highly collaborative and integrated group of scientists from the Medical
College of Wisconsin, Blood Research Institute and Children’s Research Institute whose goal is to promote immunological
education and research on campus at both the basic and clinical level. the Center for Immunology is composed of research
laboratories focused on the immunological aspects of autoimmunity, infectious disease, allergy, immunodeficiency and
cancer and is forging new links to physician colleagues at Froedtert Hospital and the Children’s Hospital of Wisconsin.
Graduate research training in immunology is offered through the Microbiology and Immunology graduate program. The
Immunology Group sponsors a number of campus wide events offering additional training in immunology including a weekly
journal club and Work-in-Progress. Immunology focused research seminars are available on campus through weekly Dept. of
Microbiology and Immunology, Blood Research Institute and the Children’s Research Institute seminar series. Now in its 12th
year, the Immunology Group hosts an annual Immunology Scientific Retreat. The Center for Immunology held its inaugural
retreat at Miller Park in March 2019 and will host its Retreat in Spring of 2020.

MCW Research Overview
Jump to Table of Contents 207
Faculty Research Expertise:
John Kirby, PhD: Chairman, major areas of research focus on signal transduction in diverse bacteria ranging from soil dwelling
spore formers (Bacillus subtilis and Myxococcus xanthus) to biofilm forming pathogens, to microbial communities in the gut.
Dr. Kirby is actively investigating interactions between M. xanthus and B. subtilis as a model for predator-prey interactions in
vivo, primarily to assess the role of production of specialized metabolites, similar to antibiotics, on both sides of the predator-
prey equation. Additionally, he has been examining the role of xenobiotics (antipsychotics, antihypertensives and antibiotics)
for their capacity to disrupt the gut microbiota with deleterious consequences on metabolism.
Joseph Barbieri, PhD: research involves the study of bacterial toxins. Several families of bacterial toxins are under
investigation: botulinum and tetanus neurotoxins; Certhrax, an ADP-ribosylating exotoxin from Bacillus cereus; and ExoS, a
type III cytotoxin of Pseudomonas aeruginosa. Dr. Barbieri is also the Director for the Medical Scientist Training Program
(MSTP).
Kenneth Brockman, PhD: Dr. Brockman’s research is focused on understanding bacterial-host interactions within the human
airways, with an emphasis on understanding the microbial regulatory mechanisms that underlie chronic diseases, such as
otitis media and exacerbations of lung disease. One area of specific interest seeks to elucidate the role of the phase variable
regulon (phasevarion) of nontypeable Haemophilus influenzae during disease. His lab utilizes a range of in vitro assays and
experimental disease models to determine bacterial genes required for persistence and define their specific roles in
pathogenesis in order to develop improved preventative and therapeutic strategies to combat infection and disease.
Weiguo Cui, PhD: The main goal of his research in the lab is to elucidate how TCR and cytokine signaling and their downstream
transcriptional programs regulate pathogen-specific T cells to proliferate, differentiate into either short-lived effector cells or
long-lived memory cells.
Bonnie Dittel, PhD: One goal of Dr. Dittel’s research program is to investigate the cellular and molecular mechanisms involved
in the regulation of the autoimmune immune response. Broadly, they are studying how the immune system regulates
inflammation associated with the central nervous system autoimmune disease multiple sclerosis (MS). These studies are
largely conducted using the animal model of MS experimental autoimmune encephalomyelitis (EAE). Specific areas of interest
are regulatory mechanisms of B cells, immune-mediated neuronal damage and myeloperoxidase as a therapeutic target in
CNS autoimmunity.
Michael Dwinell, PhD: Research in the Dwinell laboratory seeks to define the role for extracellular mediators in the
progression and metastasis of solid and hematological cancers. Additional studies are examining the role for metabolic
reprogramming to influence tumor progression and exploring new mitochondria-targeted compounds as inhibitors of cancer
progression. Human and murine 2D and 3D cell culture systems and preclinical models are being used to investigate the
cellular, biochemical, and metabolic signaling pathways that regulate cellular proliferation, programmed cell death and
motility in inflammation and cancer.
Dara Frank, PhD: Dr. Frank’s laboratory focuses on type III secretion systems (T3SS) and their effectors with specific emphasis
on pathogens that inject patatin-like phospholipases causing severe lung pathology. P. aeruginosa and several other bacterial
genera encode orthologous patatin-like PLA2 effectors that are highly toxic to eukaryotic cells. The founding member of this
family is ExoU, which we have shown requires a noncovalent interaction with ubiquitin (Ub) or ubiquitylated proteins to
express membrane destructive activity. Other than acting as overt toxins, the biological function of this family of enzymes is
unclear. The mechanism of Ub-mediated activation has not been solved. Further, while there are crystal structures
representing the inactive form of ExoU and a closely related ortholog, structural changes that result in activation are
unknown. Understanding the mechanism of activation could lead to the development of therapeutics for a broad spectrum
of organisms. To understand the structural changes that occur during membrane and ubiquitin association, we are using
biophysical (continuous wave EPR and double electron-electron resonance), biochemical (mutagenesis and enzymology) and
computational approaches (molecular dynamics and modeling).

MCW Research Overview
Jump to Table of Contents 208
Jack Gorski, PhD: Dr. Gorski is interested in understanding the molecular basis of T cell immunity in man, focusing on
polymorphism and variability within this system. Work in his lab has involved one to many to one mapping of the principle
components of the system: the MHC, antigen peptide, and TCR. He has been interested in the biophysics of binding of multiple
peptides to a single class II MHC molecule, as well as the ability of a single peptide to bind multiple class II MHC. Similarly, he
has a strong interest in the biophysics of many TCR interacting with a single peptide-MHC complex as well as the T cell cross-
reactivity (one TCR binding many peptide-MHC complexes).
Amy Hudson, PhD: The Hudson lab is interested in how viruses escape detection by the immune system. As a response to
selective pressures exerted by the host immune system, many viruses have developed an equally complex set of immune-
evasive strategies. Perhaps most interesting is the array of unique strategies that viruses employ to interfere with the
presentation of viral antigens on the surface of host cells for recognition by cytotoxic T lymphocytes.
Nikki Johnston, PhD: Dr. Johnston’s research laboratory measures pepsin, as a diagnostic biomarker for reflux and aspiration,
in clinical tissue and secretion samples from patients with diseases of the upper airway, investigates the effects of nonacid
pepsin on the airway using in vitro and in vivo models and the molecular signaling pathways through which nonacid pepsin
elicits cell damage. In addition to investigating the role of pepsin in reflux-attributed inflammatory disease, her group has
highlighted a potential role for refluxed pepsin in carcinogenesis of the laryngopharynx and for local acid and pepsin
production in Barret’s esophagus and its progression to esophageal adenocarcinoma. Her research team is currently
investigating the mechanism by which pepsin causes inflammation and promotes carcinogenesis. Her team is also leading a
drug discovery program to develop a therapeutic for reflux disease which specifically targets pepsin. They have developed
high throughput screening assays, identified a FDA approved drug which also inhibits pepsin, and developed a mouse model
to test the efficacy of these drugs for pepsin-mediated laryngeal inflammation in vivo. This work will pave the way for a
clinical trial for a much-needed medical therapy for patients with airway reflux using a faster repurposing approach and allow
us to provide proof of concept that a pepsin inhibitor will be effective for patients with airway reflux and thus de-risk the
development of new compositions of matter, perhaps more potent with optimized formulation for local delivery by nasal
spray.
Christopher Kristich, PhD: Dr. Kristich uses genetic, molecular, biochemical, and genomic experimental approaches to
understand (1) the mechanisms by which Gram-positive bacteria sense internal and external stimuli (the input), (2) how these
signaling systems control cellular processes in response to environmental conditions (signal processing); and (3) the
biochemical mechanisms of antimicrobial resistance and gut colonization (the output). His goal is to understand all aspects
of the sensory process: to define the signals that are sensed, to understand the signal transduction processes mechanistically,
to identify the corresponding physiological or behavioral output, and to elucidate how that output – the product of the signal
transduction processes – enhances the ability of the bacteria to survive and proliferate in their natural settings. He
approaches problems of bacterial signal transduction in the context of basic bacterial physiology, host-microbe interactions,
and microbial pathogenesis, with the goal of understanding how fundamental bacterial signaling processes serve to shape
the outcome of interactions with human hosts and the environment.
Robert Lochhead, PhD: Dr. Lochhead is an immunologist studying the pathogenesis of Lyme arthritis, which is caused by
infection with the tick-borne pathogen Borrelia burgdorferi. He conducted his postdoctoral fellowship at Massachusetts
General Hospital and Harvard Medical School with Dr. Allen Steere where he studied inflammatory synovitis in patients with
Lyme arthritis. In 2018 he accepted a faculty position at MCW in the Department of Microbiology & Immunology. His research
focuses on understanding how bacterial infections may trigger immune dysregulation, arthritis, and autoimmunity, and he is
involved in developing and testing a safe and effective Lyme disease vaccine for use in humans.
Mark McNally, PhD: Dr. McNally’s laboratory uses molecular, genetic, biochemical, and cell biological approaches to study
post-transcriptional mechanisms of gene regulation, including RNA splicing and polyadenylation control. One area of focus
uses the simple retrovirus, Rous sarcoma virus (RSV), to understand the role of RNA processing in the virus life cycle. He is
also exploiting antisense oligonucleotide technologies to alter RNA splicing as an approach to develop a breast cancer
therapeutic.

MCW Research Overview
Jump to Table of Contents 209
Michelle Riehle, PhD: Dr. Riehle’s laboratory uses genetic, molecular, biochemical, genomic and computational experimental
approaches to understand (1) malaria resistance mechanisms and factors that naturally segregate in the wild mosquito vector
(2) the role of non-coding genetic variation in the mosquito immune response and resistance to Plasmodium falciparum, the
eukaryotic malaria parasite and (3) the role of the mosquito prokaryotic and eukaryotic microbiomes in shaping mosquito
immune responses and Plasmodium infection outcome. The overall goal of her laboratory is to understand in totality existing
natural mechanisms of Plasmodium resistance in the mosquito vector that have been molded through evolutionary time and
to harness these mechanisms for vector and malaria control.
Vera Tarakanova, PhD: Dr. Tarakanova’s current research focuses on gammaherpesviruses. Gammaherpesviruses infect a
majority of adult population worldwide; this virus infection is never cleared. Importantly, gammaherpesviruses drive the
development of several malignancies, including lymphomas. While it is clear that not every infected human will develop virus-
driven lymphoma, the risk factors for viral lymphomagenesis remain poorly defined and it is next to impossible to predict
individual’s risk of developing gammaherpesvirus-driven cancer. Her research group utilizes a mouse gammaherpesvirus-68
(MHV68) model to study the entire spectrum of virus-host interactions: molecular mechanisms using cultures of primary
immune cells --chronic infection of an intact host-- animal models of viral lymphomagenesis.
Scott Terhune, PhD: Dr. Terhune’s laboratory is interested in determining the underlying molecular mechanisms of human
cytomegalovirus protein function during infection. Our current projects focus on defining how viral proteins manipulate
cellular processes early during infection to construct a permissive cellular environment for replication. He accomplishes his
goal by combining targeted proteomics and viral genetic manipulations with basic approaches in cellular and molecular
biology.
Demin Wang, PhD: Dr. Wang’s research focuses on identifying and functionally characterizing signaling pathways and
transcriptional regulators that control B cell development from hematopoietic stem cells (HSCs) and B cell function. His
studies aim to understand the molecular mechanisms underlying immunodeficiency and autoimmune diseases, including
heparin-induced thrombocytopenia (HIT). His research uses mouse models and human patient samples, and employs multiple
cutting-edge approaches, such as targeted gene disruption, transgenic, bone marrow transplantation and high-throughput
DNA/RNA sequencing technologies.
Tom Zahrt, PhD: Dr. Zahrt’s laboratory uses a combination of genetic, molecular, biochemical, and proteomic approaches,
along with various in vitro and in vivo model systems of infection, to understand the mechanisms by which two intracellular
respiratory pathogens, Mycobacterium tuberculosis and Francisella tularensis, persist and/or cause disease within the lungs
of infected individuals.

MCW Research Overview
Jump to Table of Contents 210
Pharmacology and Toxicology
The Department of Pharmacology and Toxicology at the Medical College of Wisconsin is dedicated to quality in research,
graduate and postdoctoral training and medical education. The research interests of our faculty are broadly based in
cardiovascular pharmacology, neuropharmacology, cancer pharmacology, toxicology and molecular pharmacology. The
research programs in the Department of Pharmacology and Toxicology are also multidisciplinary in nature and have strong
associations with researchers of other basic science and clinical departments. In addition, our faculty members collaborate
on research projects both nationally and internationally. The specific areas of research interest include:
Cardiovascular Pharmacology: The cardiovascular research focuses on the heart, kidney, and vascular biology. Emphasis
is on molecular, signal transduction, immunological, cellular and in vivo approaches to understanding heart failure, cardiac
ischemia-reperfusion injury, endothelial regulators of vascular tone, lipoprotein regulation, renal injury and mechanisms
of hypertension.
Neuropharmacology: The neuropharmacology research involves studies of drugs of abuse and molecular mechanisms
that underlie learning, memory and behavior. Cellular, molecular, imaging, optigenetics and in vivo approaches are used
to address the mechanisms by which addictive drugs, including cannabinoids, cocaine, ethyl alcohol and opiates, affect
the brain; the roles of endocannabinoid signaling in stress-related disorders; and molecular mechanisms controlling
memory.
Cancer Pharmacology: Basic mechanism regulating cancer cell growth and metastasis, chemoprevention and
chemotherapy are studied. Emphasis is placed on identifying genes altered in cancer, regulation of cellular oxidant
mechanisms, role of small molecular weight GTPases in cancer and immune mechanism regulating tumor growth. Studies
to develop new treatment involve vaccines, antisense oligonucleotides, repurposing of existing drugs and combination
therapies for chemoresistance.
The Drug Discovery Center is housed within the Department of Pharmacology and Toxicology. The primary focus of the Drug
Discovery Center is to facilitate and accelerate drug discovery and the translation of new basic discoveries into therapies to
improve human health. Research expertise in the Center will provide resources, knowledge, and services to complete the
drug development process from target validation, drug design, and drug delivery to clinical application.
The Center for Disease Prevention Research is a Pharmacology and Toxicology department-based center focusing on basic,
translational, and clinical research for the prevention of major chronic diseases including cancer, neurologic diseases, cardiac
diseases, gastrointestinal disorders and type 2 diabetes. In collaboration with hospital partners, the Center is establishing
new clinical platforms such as an Integrative Medicine Clinic, where patients are provided access to conventional,
complementary and alternative medicine therapies, and opportunities to participate in disease prevention clinical trials.
The MCW Shared Mass Spectrometry (MSMS) Facility – MSMS Facility is a research service unit managed by the Department
of Pharmacology and Toxicology. The facility provides service and consultation for research projects requiring mass
spectrometric analysis (fundamental, identification and quantitation) of a variety of compounds. The primary focus is on
small molecules such as drugs, hormones, chemical intermediates and cellular metabolites. The facility operates on a fee for
service basis and is open for faculty of the Medical College of Wisconsin and outside researchers. State-of-the-art mass
spectrometers with different configurations and 27 years of experience and expertise meet researchers’ needs for sample
analysis.

MCW Research Overview
Jump to Table of Contents 211
There is also a long history of quality graduate education in the Department of Pharmacology and Toxicology at the Medical
College of Wisconsin. Our graduates are successful scientists in universities, pharmaceutical companies and government. The
size of the program encourages the development of a close working relationship between students and faculty. In addition,
every effort is made to optimize and tailor training programs to meet individual student needs in preparation for successful
careers in pharmacology and toxicology. Our doctoral program provides diverse research opportunities in the areas of
cardiovascular pharmacology, molecular pharmacology, molecular toxicology, behavioral pharmacology, neuropharmacology
and cancer pharmacology. An emphasis is placed on cellular and molecular pharmacology and signal transduction and using
in vivo models of disease. The primary objective of our program is to provide students with the academic background, state-
of-the-art scientific approaches and professional development opportunities that are necessary to investigate and solve the
important biological and biomedical problems for a successful biomedical research career in the 2000's.

MCW Research Overview
Jump to Table of Contents 212
Physiology
The Department of Physiology is dedicated to quality in three main areas: research, graduate and postdoctoral training and
medical education. The interests of our faculty are broadly based, with strong emphasis on cardiovascular, renal, metabolic
and respiratory physiology, physiological genomics, proteomics and computational biology, epigenomics, and related
translational research. The research programs in this department are multidisciplinary in nature with strong associations
with researchers in other basic science and clinical departments. The department is tightly integrated with several Research
Centers on the MCW campus including the Cardiovascular Center, Genomic Sciences and Precision Medicine Center, Center
of Systems Molecular Medicine, and Neuroscience Research Center. We are also closely aligned with the Marquette
University and Medical College of Wisconsin Department of Biomedical Engineering.
There is a long history of quality graduate education in the Department of Physiology. Our graduates are successful scientists
in universities, pharmaceutical companies and government. The size of our program encourages the development of close
working relationships between students and faculty. Additionally, the Department has established the Master's in Medical
Physiology (MMP) Program to improve a college graduate’s academic record for application to medical schools. Every effort
is made to optimize and tailor our training programs to meet individual student needs in preparation for successful careers.
The basic support for projects and programs in the department is provided by the Research Services Cores (RSC). The RSC
facilities is serviced by a group of professional engineers, computer programmers, systems analysts, histologists, and animal
technicians who provide infrastructure support to the research programs in the department of Physiology and other
researchers at MCW. The main areas are: Chronic Monitoring Facilities (provide equipment, computer hardware and
software, and service and support necessary for short term or continuous 24-hour-a-day measurement of hemodynamic
variables from research animals in their home cages); Computer Core (an integrated computer environment to support
research and other needs with specialized software, printers, and access to dedicated servers for online storage); Biochemical
Core Service Center (provides a broad range of assays for biochemical measurements); and Microscopy and Image Processing
Core (offers a broad range of imaging options as well as consultations and training).
Physiology is the home of two NIH Program Project Grants studying Blood Pressure Regulation; a Dissemination and
Coordinating Center for a Somatic Cell Genome Editing (SCGE) Program; a Hybrid Rat Diversity Panel (HRDP) Program; and a
T32 pre-doctoral training grant on Integrated Physiology Training: Molecular to Organism. Department trainees are the
recipients of numerous training grants from the NIH and American Heart Association, among other agencies.
Summary of Department of Physiology faculty research programs:
Allen W. Cowley, Jr., PhD.: Research in the Cowley laboratory is dedicated to advancing our understanding of the
physiological and genetic mechanisms that determine blood pressure in normal and hypertensive states with a specific
interest in the role of the kidney. Research is currently focused on two major areas of research: 1) the role of the mTOR
pathway and oxidative stress in the regulation of kidney function and blood pressure salt-sensitivity; 2) mechanisms whereby
positionally cloned gene associated with blood pressure salt-sensitivity called Pappa2 influences kidney development and
function.
• Kumar V, Wollner C, Kurth T, Bukowy J, Cowley Jr AW. Inhibition of Mammalian Target of Rapamycin complex 1
Attenuates Salt-Induced Hypertension and Kidney Injury in Dahl Salt-Sensitive Rats. Hypertension 70: 813-821, 2017.
• Kumar V, Evans LC, Kurth T, Yang C, Wollner C, Nasci V, Zheleznova NN, Bukowy J, Dayton A, Cowley Jr. AW.
Therapeutic Suppression of mTOR (Mammalian Target of Rapamycin) Signaling Prevents and Reverses Salt-Induced
Hypertension and Kidney Injury in Dahl Salt-Sensitive Rats. Hypertension 73: 630-639, 2019.
• Cowley AW Jr, Yang C, Kumar V, Lazar J, Jacob H, Geurts A, Liu P, Dayton A, Kurth T, Liang M. Pappa2 is linked to salt-
sensitive hypertension in Dahl S Rats. Physiol Genomics 48: 62-72, 2016.

MCW Research Overview
Jump to Table of Contents 213
Melinda R. Dwinell, PhD: Dr. Dwinell’s major focus is on the development of research resources for the scientific community.
Current projects focus on 1) the development of the 96 strain Hybrid Rat Diversity Panel to be used to detect genetic loci
associated with complex traits, 2) the establishment of the Somatic Cell Genome Editing (SCGE) Dissemination and
Coordinating Center for the SCGE Consortium and 3) the development of Sry transgenic rats to study the phenotypic
differences between males and females through isolation of differences in sex chromosomes and gonadal hormones.
• Smith JR, Bolton ER, Dwinell MR. The Rat: A Model Used in Biomedical Research. Methods Mol Biol 2018:1-41, 2019.
• Meurer JR, Whittle JC, Lamb KM, Kosasih MA, Dwinell MR, Urrutia RA. Precision Medicine and Precision Public
Health: Academic Education and Community Engagement. Am J Prev Med 57:286-289, 2019.
• Shimoyama M, Smith JR, Bryda E, Kuramato T, Saba L, Dwinell M. Rat Genome and Model Resources. ILAR 58:42-
58, 2017.
Aron Geurts, PhD: Dr. Guerts pioneers cutting edge genetic engineering technologies in stem cells and whole animals to
model human cardiovascular diseases including heart disease, hypertension, type 1 diabetes, and more. His lab is strongly
motivated by the challenges of understanding how genetic variation affects human disease and developing novel disease
models primarily in rats and human stem cells. He is considered an expert in genetic engineering, especially gene editing of
rodent genomes and was awarded a prestigious New Innovator Award from the Office of the Director of the National
Institutes of Health in 2011 for his efforts to advance genetic engineering technology.
• Geurts AM, et al. Knockout rats via embryo microinjection of zinc-finger nucleases. Science 325:433, 2009.
• Endres BT, et al. Mutation of Plekha7 attenuates salt-sensitive hypertension in the rat. Proc Natl Acad Sci USA 111:
12817-12822, 2014.
• Mitzelfelt KA, et al. Efficient Precision Genome Editing in iPSCs via Genetic Co-targeting with Selection. Stem Cell
Reports 8: 491-499, 2017.
Justin L. Grobe, PhD: The Grobe laboratory focuses on the cross-talk between obesity and hypertension, through dissection
of the hypothalamic circuitry that mediates integrative control of blood pressure and resting energy expenditure. In addition,
their work on hypothalamic contributions to blood pressure control has provided exciting new insights into the severely
underserved hypertensive cardiovascular disorder of pregnancy, preeclampsia. Further, they are developing novel
technologies to assess resting energy expenditure in vivo provides unique opportunities to understand the contribution of
the gut microbiota to whole-organism energy homeostasis.
• Claflin KE, Sandgren JA, Lambertz AM, Weidemann BJ, Littlejohn NK, Burnett CM, Pearson NA, Morgan DA, Gibson-
Corley KN, Rahmouni K, Grobe JL. Angiotensin AT1A receptors on leptin receptor-expressing cells control resting
metabolism. J Clin Invest 127:1414-1424, 2017.
• Sandgren JA, Deng G, Linggonegoro DW, Scroggins SM, Perschbacher KJ, Nair AR, Nishimura TE, Zhang SY, Agbor LN,
Wu J, Keen HL, Naber MC, Pearson NA, Zimmerman KA, Weiss RM, Bowdler NC, Usachev YM, Santillan DA, Potthoff
MJ, Pierce GL, Gibson-Corley KN, Sigmund CD, Santillan MK, Grobe JL. Arginine vasopressin infusion is sufficient to
model clinical features of preeclampsia in mice. JCI Insight 3:e99403, 2018.
• Soto JE, Burnett CML, Ten Eyck P, Abel ED, Grobe JL. Comparison of the Effects of High-Fat Diet on Energy Flux in
Mice Using Two Multiplexed Metabolic Phenotyping Systems. Obesity 27:793-802, 2019.
Matthew R. Hodges, PhD: Dr. Hodges is focused on the neural mechanisms that control breathing during health and in animal
models of human disease. He and his research team are specifically focused on the role of brainstem serotoninergic neurons
as key regulators of breathing and global pH homeostasis, and how their dysfunction may contribute to unexpected death
during development (SIDS) or seizure disorders (SUDEP). Through a strong multidisciplinary approach, he and his
collaborators also are currently focused on how opioids such as fentanyl suppress ventilation, and are developing novel
strategies and drugs for reversing these negative effects.
• Mouradian GC Jr., Alvarez-Argote S, Gorzek R, Thuku G, Michkalkiewiz T, Wong-Riley MTT, Konduri GC, Hodges MR.
Acute and chronic changes in the control of breathing in a rat model of bronchopulmonary dysplasia. Am J Physiol
Lung Cell Mol Physiol 316: L506-L518, 2019.
• Burgraff NJ, Neumueller SE, Buchholz K, Hodges MR, Pan P, Forster HV. Glutamate receptor plasticity in brainstem
respiratory nuclei following chronic hypercapnia in goats. Physiol Rep, 7: e14035, 2019.
• Puissant MM, Muere C, Levchenko V, Manis AD, Martino P, Forster HV, Palygin O, Staruschenko A, Hodges MR.
Genetic mutation of Kcnj16 identifies Kir5.1-containing channels as key regulators of acute and chronic pH
homeostasis. FASEB J 33:5067-5075, 2019.

MCW Research Overview
Jump to Table of Contents 214
Alison J. Kriegel, PhD: Dr. Kriegel’s research program is centered on understanding how alterations in microRNAs (miRNAs),
protein coding genes, and metabolism influence cardiorenal syndrome, cardiovascular disease, and kidney disease
progression. She often blends discovery-based next-generation technologies with classical physiology and molecular biology
techniques to study these complex problems, with the goal of identifying novel translational interventions and/or therapies.
• Chuppa S, Liang M, Liu P, Liu Y, Casati MC, Cowley AW, Patullo L, Kriegel AJ. MicroRNA-21 regulates peroxisome
proliferator-activated receptor alpha, a molecular mechanism of cardiac pathology in Cardiorenal Syndrome Type 4.
Kidney International 93:375-389, 2018.
• Kriegel AJ, Terhune SS, Greene AS, Noon KR, Pereckas MS, Liang M. Isomer-specific effect of microRNA miR-29b on
nuclear morphology. J Biol Chem 293:14080-14088, 2018.
• Nasci VL, Chuppa S, Griswold L, Goodreau KA, Dash RK, Kriegel AJ. miR-21-5p regulates mitochondrial respiration
and lipid content in H9C2 cells. Am J Physiol Heart Circ Physiol 316:H710-H721, 2019.
Anne E. Kwitek, PhD: Dr. Kwitek’s major research focus involves understanding the genetic susceptibility to complex human
diseases, with a focus on obesity, hypertension, and cardiometabolic disease. The approach involves integrating genetics,
genomics, and other ‘omics’ approaches to identify genes and mechanisms leading to complex disease using rat models and
human populations. Her studies also involve how genomic variation affects and is affected by environmental stimuli to
influence susceptibility to cardiovascular disease and metabolic syndrome.
• Mansilla AM, Sompallae RR, Nishimura CJ, Kwitek AE, Kimble MJ, Armstrong ME, Campbell CA, Smith RJ, Thomas CP,
Targeted Broad-Based Genetic Testing by Next Generation Sequencing Informs Diagnosis and Facilitates
Management in Patients with Kidney Diseases. Nephrology Dialysis Transplantation (in press) 2019.
• Ma MCJ, Pettus JM, Jakoubek JA, Mennie AK, Kwitek AE, Contribution of Independent and Pleiotropic Genetic Effects
in the Metabolic Syndrome in a Hypertensive Rat. PLoS One 12:e0182650, 2017.
• Wang J, Ma MCJ, Mennie AK, Pettus JM, Xu Y, Lin L, Traxler MG, Jakoubek J, Atanur SS, Aitman TJ, Xing Y, Kwitek AE,
Systems Biology with high-throughput sequencing revealed genetic mechanisms underlying the metabolic syndrome
in the Lyon Hypertensive Rat. Circ Cardiovasc Genet 8:316-326, 2015.
Mingyu Liang, PhD: The current work in Mingyu Liang’s laboratory focuses on three areas: regulatory RNA, cellular
metabolism, and precision medicine and epigenomics, as they relate to hypertension and cardiovascular and kidney diseases.
Dr. Liang uses a multidisciplinary, translational research platform to integrate human research with animal and cell model
research using approaches of physiology, genetics, biochemistry, molecular biology, genome editing, and big data analysis.
• Xue H, Geurts AM, Usa K, Wang F, Lin Y, Phillips J, Henderson L, Baker MA, Tian Z, Liang M. Fumarase Overexpression
Abolishes Hypertension Attributable to endothelial NO synthase Haploinsufficiency in Dahl Salt-Sensitive Rats.
Hypertension 74:313-322, 2019.
• Liang M. Epigenetic Mechanisms and Hypertension. Hypertension 72:1244-1254, 2018.
• Widlansky ME, Jensen DM, Wang J, Liu Y, Geurts AM, Kriegel AJ, Liu P, Ying R, Zhang G, Casati M, Chu C, Malik M,
Branum A, Tanner MJ, Tyagi S, Usa K, Liang M. miR-29 contributes to normal endothelial function and can restore it
in cardiometabolic disorders. EMBO Mol Med 10: e8046, 2018.
Julian H. Lombard, PhD: The Lombard laboratory is currently investigating the mechanisms by which vascular dysfunction
develops during chronic exposure to sub-physiological levels of angiotensin II, either as a result of a high salt diet or due to
genetic factors, such as those encountered in humans with low renin hypertension. They found that chronic exposure to low
levels of angiotensin II in the blood leads to oxidative stress and severe impairment of endothelium-dependent and
endothelium-independent mechanisms of vascular relaxation and to a reduced density of microvessels that supply oxygen
and nutrients to the tissues. To investigate these questions, they are employing novel rat genetic models including knockouts
of the master antioxidant and cell-protective transcription factor (NRF2); the Mas1 receptor for angiotensin (1-7), and the
AT1A receptor for angiotensin II.
• Priestley JR, Kautenburg K, Casati M, Endres BT, Geurts AM, and Lombard JH. The NRF2 knockout rat: A new animal
model to study endothelial dysfunction, oxidant stress, and microvascular rarefaction. Am J Physiol Heart Circulatory
Physiology 310:H478-H487, 2016.
• Raffai G and Lombard JH. Angiotensin (1-7) selectively induces relaxation and modulates endothelium-dependent
dilation in mesenteric arteries of salt-fed rats. J Vasc Res 53:105-118, 2016.
• Allen LA, Schmidt JR, Thompson CT, Carlson BE, Beard DA, and Lombard JH. High salt diet impairs cerebral blood
flow regulation via salt-induced angiotensin II suppression. Microcirculation 26:e12518, 2019.

MCW Research Overview
Jump to Table of Contents 215
Caitlin O’Meara: Dr. O’Meara’s research is focused on understanding the cell biology of heart regeneration and
cardiomyocyte cell cycle activity. They use pro-cardiac regenerative models such as neonatal mice and zebrafish to identify
pathways and molecules that facilitate successful cardiac regeneration. The ultimate goal of this research is to develop new
therapeutic targets for promoting cardiac healing in the adult heart following injury such as myocardial infarction.
• Wodsedalek DJ, Paddock SJ, Wan TC, Auchampach JA, Kenarsary A, Tsaih SW, Flister MJ, O'Meara CC. IL13 Promotes
in vivo neonatal cardiomyocyte cell cycle activity and heart regeneration Am J Physiol Heart Circ Physiol 316:H24-
H34, 2019.
• Flinn MA, Jeffery BE, O'Meara CC, Link BA. Yap is required for scar formation but not myocyte proliferation during
heart regeneration in zebrafish. Cardiovasc Res 115:570-577, 2019.
• O'Meara CC, Wamstad JA, Gladstone RA, Fomovsky GM, Butty VL, Shrikumar A, Gannon JB, Boyer LA, Lee RT.
Transcriptional reversion of cardiac myocyte fate during mammalian cardiac regeneration. Circ Res 116:804-815,
2015.
Curt D. Sigmund, PhD: Dr. Sigmund’s major areas of research focus on 1) the mechanism by which the central nervous system
and the brain renin-angiotensin system controls fluid balance, blood pressure and metabolism, and 2) vascular mechanisms
of blood pressure regulation by the transcription factor PPAR-gamma, and its downstream effectors Cullin-3/RhoBTB1. He
investigates these pathways using a combination of molecular biological, genetic and physiological approaches including the
generation of unique transgenic and gene targeted mouse models.
• Mukohda M, Fang S, Wu J, Agbor LN, Nair AR, Ibeawuchi SC, Hu C, Liu X, Lu KT, Guo DF, Davis DR, Keen HL, Quelle
FW, Sigmund CD. RhoBTB1 protects against hypertension and arterial stiffness by restraining phosphodiesterase 5
activity. J Clin Invest 130:2318-2332, 2019.
• Agbor LN, Nair AR, Wu J, Lu KT, Davis DR, Keen HL, Quelle FW, McCormick JA, Singer JD, Sigmund CD. Conditional
deletion of smooth muscle Cullin-3 causes severe progressive hypertension. JCI Insight 5: e129793, 2019.
• Nair AR, Silva SD Jr, Agbor LN, Wu J, Nakagawa P, Mukohda M, Lu KT, Sandgren JA, Pierce GL, Santillan MK, Grobe
JL, Sigmund CD. Endothelial PPARγ (Peroxisome Proliferator-Activated Receptor-γ) Protects From Angiotensin II-
Induced Endothelial Dysfunction in Adult Offspring Born From Pregnancies Complicated by Hypertension.
Hypertension 74:173-183, 2019.
Alexander Staruschenko, PhD.: Dr. Staruschenko’s research is focused on understanding the mechanisms regulating ion
channels activity and electrolyte homeostasis, respectively, in the control of blood pressure and various kidney diseases. His
technical expertise is very broad and he applies in the laboratory physiological, biophysical, genetic, and microscopy methods
to address unresolved questions regarding the regulation of renal transport processes in hypertension and kidney diseases.
• Ilatovskaya DV, Levchenko V, Pavlov TS, Isaeva E, Klemens CA, Johnson J, Liu P, Kriegel AJ, Staruschenko A. Salt-
deficient diet exacerbates cystogenesis in ARPKD via epithelial sodium channel (ENaC). EBioMedicine 40: 663-674,
2019.
• Palygin O, Ilatovskaya DV, Levchenko V, Klemens CA, Dissanayake L, Williams AM, Pavlov TS, Staruschenko A.
Characterization of purinergic receptor expression in ARPKD cystic epithelia. Purinergic Signaling 14: 485-497, 2018.
• Ilatovskaya DV, Blass G, Palygin O, Levchenko V, Pavlov TS, Grzybowski M, Winsor K, Shuyskiy LS, Geurts A, Cowley
AW Jr, Birnbaumer L, Staruschenko A. A NOX4/TRPC6 pathway in podocyte calcium regulation and renal damage in
diabetic kidney disease. Journal of the American Society of Nephrology 29: 1917-1927, 2018.

MCW Research Overview
Jump to Table of Contents 216
Anethesiology
Departmental faculty members direct research teams at Zablocki VA Medical Center and the MCW campus labs, where we
investigate a wide range of topics relevant to anesthesiology. These programs not only contribute fundamental new
knowledge to the foundational basic science of anesthesia, but are also engaged in developing new therapies. Support for
these labs, totaling $3,900,000 this past year, comes from the NIH, Veterans Administration, Advancing a Healthier Wisconsin,
commercial affiliations, and internal departmental and MCW support. Research education is a key element in our research
division, with participation by medical, graduate, and post-doctoral students. Our current projects are described below.
Amadou Camara, PhD studies the role of mitochondrial dysfunction in disease, particularly in ischemic heart disease,
neurodegenerative diseases, diabetes and aging, with a focus on mitochondrial calcium handling and their regulation or
reactive oxygen species, using a broad range of experimental approaches.
Caron Dean-Bernhoft, PhD performs research that is based in systems physiology, primarily the neurobiology of stress
conditions. Recent research focus is on central neuronal circuitry at the interface of sympatho-sensory responses.
Julie Freed, MD, PhD uses physiological and pharmacological approaches to explore the regulation of microcirculation with
particular interests in endothelial dysfunction, the coronary microcirculation, vasoplegia, endothelium-derived extracellular
vesicles, and the role of ceramide signaling.
Quinn Hogan, MD examines mechanisms of chronic pain at the molecular and cellular level, and applies this in developing
novel therapies for chronic pain. Additional studies involve coordination of autonomic activity and pain, and strategies to
avoid loss of brain connectivity with sensory systems after injury.
Wai-Meng Kwok, PhD is focused on the modulation of ion channel proteins. His major areas of interest are investigating
the roles of ion channels in mitochondrial dysfunction, and electrophysiological characterization of cardiomyocytes derived
from induced pluripotent stem cells.
Bin Pan, PhD explores the organization of brain function at the network and synaptic level, focusing on the links between
depression and pain, and the role of cannabinoid signaling in the control of these pathways.
Christopher Pawela, PhD investigates brain plasticity in neurological injury and disease using MRI. His current work focuses
on the effect of chronic hypertension on neurovascular structure/function, brain reorganization after peripheral nerve
injury/repair, and the physiologic basis of neuroimaging signals.
David Stowe, MD, PhD studies molecular aspects of mitochondrial channels and transporters involved in cell stress, and
liver mitochondrial bioenergetics during ischemia/reperfusion during transplantation.
Astrid Stucke, MD examines the central mechanisms regulating breathing at the neuronal and network level. Her current
focus is on the effect sites of opioids and potential differences between young and adult animals, which is of importance for
perioperative patient care.
David Warltier, MD, PhD is an expert in the area of anesthetic effects on the circulation and heart function, with a current
focus on the potential use of novel hemoglobin-based oxygen carriers (HBOCs) in the treatment of shock.
Dorothee Weihrauch, DVM, PhD studies coronary collateral growth and impaired angiogenesis in diabetes using
techniques such as protein analysis, proliferation assays, migration assays on cultured cells as well as histology and
immunohistochemistry.
Hongwei Yu, MD is an expert in molecular genetic techniques for controlling gene expression and signaling interactions,
which he uses to design novel treatments for chronic pain, including arthritic and neuropathic etiologies.
Edward Zuperku, PhD studies the brainstem networks that control breathing, including the neurophysiology and
pharmacology of respiratory neurons, the relevant pharmacology of agents that modulate respiratory control, and the
effect of opioids and anesthetics on respiratory neurons and breathing patterns.

MCW Research Overview
Jump to Table of Contents 217
Dermatology
The Department of Dermatology at the Medical College of Wisconsin has a deep commitment to expanding the understanding
of the physiology of the skin and new and novel treatments through research. Our faculty provide comprehensive and
specialty clinical care in skin cancer and inflammatory diseases, first class cutaneous surgery and dermatopathology, and one
of the most vital and important sections of pediatric dermatology, both nationally and internationally.
Our research portfolio includes projects with fellows, residents, medical students, and other collaborating researchers from
numerous renowned institutions.
Studies involving Departmental Faculty in the immediate past and current academic years include the following:
1. Protocol; Risankizumab verse Secukinumab for Subjects with Moderate to Severe Plaque Psoriasis (Kenneth
Gordon, MD)
2. A multicenter, single-arm, open label, study to assess the usability of the risankizumab autoinjector combination
product in Adult Patients with Moderate to Severe Plaque Psoriasis (Kenneth Gordon, MD)
3. A 24-week Multicenter, Randomized, Double-Blind Parallel-Group Study Comparing the Efficacy and Safety of
Ixekizumab to Guselkumab in Patients with Moderate to Severe Plaque Psoriasis (Kenneth Gordon, MD)
4. A Pilot Study of a Single, Easily Measurable Outcome for Psoriasis in Pediatric and Adult Patients (Kenneth Gordon,
MD)
5. A Multi-Center, Randomized, Double-Blind, Placebo- and Active Comparator-Controlled Phase 3 Study with
Randomized Withdrawal and Retreatment to Evaluate the Efficacy and Safety of BMS-986165 in Subjects with
Moderate-to-Severe Plaque Psoriasis (Kenneth Gordon, MD)
6. Efficacy, Safety and Pharmacokinetics of Topical Timolol in Infants with Infantile Hemangioma (Kristen Holland,
MD)
7. Multicenter Phenotype-Genotype analysis of Vascular Overgrowth Syndromes ( Dawn Siegel, MD)
8. A proposal to support Melanoma Research at MCW (Kara Walton, MD).
9. Regeneron Pharmaceuticals, Clinical Trial PROSE R668-AD-1762 (Keri Chaney, MD)
10. A prospective observational survey study to determine and compare patient centered and physician assessed
outcomes in Hidradenitis Suppurativa. (Olayemi Sokumbi, MD)
11. Development and Validation of a Gene Expression Assay to Predict the Risk of Recurrence Disease in Cutaneous
Squamous Cell Carcinoma. (Julia Kasprzak, MD).
12. Analysis of Whole Genome Sequencing Data from an Infantile Hemangioma Syndrome Cohort. (Dawn Siegel, MD)
13. Genomic Analysis of a Cohort with Infantile Hemangiomas Associated with Multi-Organ structural birth defects
(Dawn Siegel, MD)
14. SID Mid-Career Award (Dawn Siegel, MD)
15. A PHASE 3, MULTI-CENTER, RANDOMIZED, DOUBLE- BLIND, PLACEBO-CONTROLLED STUDY TO ASSESS THE
EFFICACY AND SAFETY OF APREMILAST IN PEDIATRIC SUBJECTS FROM 6 THROUGH 17 YEARS OF AGE WITH
MODERATE TO SEVERE PLAQUE PSORIASIS (Kristen Holland, MD)
16. A Phase 3, Randomized, Double-Blind, Placebo-Controlled, Multi-Center Study Investigating the Efficacy and Safety
of PF-04965842 Co-Administered with Background Medicated Topical Therapy in Adolescent Participants 12 to <18
Years of Age with Moderate to Severe Atopic Dermatitis (Kristen Holland, MD)
17. A PHASE 3 MULTI-CENTER, LONG-TERM EXTENSION STUDY INVESTIGATING THE EFFICACY AND SAFETY OF PF-
04965842, WITH OR WITHOUT TOPICAL MEDICATIONS, ADMINISTERED TO SUBJECTS AGED 12 YEARS AND OLDER
WITH MODERATE TO SEVERE ATOPIC DERMATITIS (Kristen Holland, MD)

MCW Research Overview
Jump to Table of Contents 218
Emergency Medicine
The Department of Emergency Medicine at the Medical College of Wisconsin has a robust research portfolio and is at the
forefront of emergency medicine research. The Department is one of the top 30 National Institutes of Health (NIH) funded
emergency medicine departments in the country. Our faculty members are recognized nationally and internationally as
leaders in emergency medicine research, and the department participates in the NIH sponsored Strategies to Innovate
Emergency Care Clinical Trials Network (SIREN) and the HRSA sponsored Pediatric Emergency Care Applied Research Network.
Our faculty has published hundreds of publications in the peer reviewed literature on a variety of topics ranging from disaster
medicine to cardiovascular care and we are considered leaders in prehospital care research.
Our research portfolio includes numerous projects with fellows, residents, graduate and medical students. Our clinical
research laboratory includes a 43 bed state of the art emergency department that treats over 70,000 patients per year and
serves as the only adult level 1 trauma center in Southeastern Wisconsin. We work closely with the county EMS system to
conduct both prehospital clinical trials and observational research that utilizes their medical record database which covers
over a decade of EMS responses. We also work with numerous governmental and non-governmental organizations at the
state, regional, and national levels to study injury rates and patterns, as well as treatment. We have international research
relationships in China, Belize, and other countries. The Department’s Research Director is a PhD epidemiologist with 20 years
of emergency medicine research experience. The department also has a Research Manager, who works with the Director to
assist faculty and students in all aspects of research. We also have Research Assistants stationed in the emergency depart 7
days a week/16 hours per day who identify and enroll research subjects.
The Department of Emergency Medicine provides numerous opportunities to engage in cutting-edge research.

MCW Research Overview
Jump to Table of Contents 219
Medicine
The Department of Medicine is nationally and internationally known for research and scholarship. Department of Medicine
faculty members are active in numerous clinical trials and are primary or collaborating investigators on a number of NIH,
Foundation and Industry grants. In total, the Department has over $35,000,000 in annual research funding, with all Divisions
represented. Research efforts are based at the Medical College of Wisconsin campus, the Blood Research Institute/Versiti,
and the Clement J. Zablocki VA Medical Center. Through investments and active recruitments, the Department continues to
be poised for significant growth in research during the next several years.
Department of Medicine faculty members, spread across 10 Divisions, are actively pursuing numerous interdepartmental
translational research projects and training opportunities, including in the Clinical Translational Research Institute (CTSI), the
MCW Cancer Center, Cardiovascular Research Center, the Genomic Sciences and Precision Medical Center (GSPMC) and the
Center for Advancing Population Science (CAPS). The TOPS Obesity Center, in partnership with the Division of Endocrinology,
is exploring the causes and treatment of obesity. The Center for International Blood and Marrow Transplantation, housed in
the Division of Hematology/Oncology, is internationally known as a leader of outcomes research as well as a coordinating
center for multi-center clinical trials.
These are just a few examples of the types of research activities taking place in the Department. To learn more about these
and other research activities, please visit the Department Website (http://www.mcw.edu/Medicine/Research.htm) or our
individual Division pages and click on “Research”.
Division of Cardiovascular Medicine
The Division of Cardiovascular Medicine maintains signicant basic research programs with the purpose of generang and
tesng new hypotheses in the eld of Cardiovascular Medicine and Physiology. Our physicians and invesgators
collaborate with many basic and clinical departments in order to advance MCW’s mission “to discover and translate new
knowledge in the biomedical sciences”.
The research conducted by many of our investigators has national and international recognition. We are the recipients of
funding through the NIH (including eight active R01s), American Heart Association, American Diabetes Association, and the
Veterans Health Administration. Many of our investigators developed local collaborations through successful funding
through the regional CTSI. Our research has been published in Circulation, Circulation Research, American Journal of
Physiology, Journal of the American College of Cardiology, EMBO Molecular Medicine, Free Radical Biology and
Medicine,PLOS One, Journal of Molecular and Cellular Physiology, Hypertension. Our areas of interest include atrial
fibrillation, redox biology (nitric oxide and free radical), muscular dystrophy related cardiomyopathy, diabetes; hypertensive
disease, congestive heart failure; endothelial dysfunction; peripheral arterial disease and wound management
Acve research-intensive faculty members include:
• Andreas Beyer, PhD studies the metabolic effects of aging, hyperglycemia, and oxidative stress on the
peripheral microcirculation.
• Ivor Benjamin, MD is interested in the genetic etiology of atrial fibrillation and the use of induced pluripotent
stem cells in a dish, for modeling disease.
• David Gutterman, MD examines the effect of atherosclerosis and diabetes on the coronary microcirculation.
• Jacquelyn Kulinski, MD is interested in understanding the physiological mechanisms between sedentary
behavior and endothelial dysfunction. Physiology of endothelial dysfunction in gestational diseases.
• Nicole Lohr, MD, PhD studies the mechanisms of cellular nitric oxide production and the effect of red light
on vasodilation. Physiology of endothelial dysfunction in gestational diseases.
• Jennifer Strande, MD, PhD has research interests focused on the mechanisms underlying the cardiomyopathy
of muscular dystrophy.
MCW Research Overview
Jump to Table of Contents 220
• Michael Widlansky, MD has efforts focused on the relationship between altered mitochondrial bioenergetics
and endothelial dysfunction. In addition, he studies the impact probiotic supplementation on vascular
endothelial function in humans with coronary artery disease.
• David Zhang, MD, PhD seeks to identify cellular mechanisms by which the endothelium regulates blood vessel
tone in both normal physiological conditions and disease states, such as ischemic heart disease and
hypertension.
In addition, the division boasts a robust clinical trials portfolio, including over 20 clinical trials involving all aspects of
cardiovascular care including advanced structural heart disease, electrophysiology, advanced heart failure, and secondary
prevention of cardiovascular events. In addition, the clinical trials group supports multiple investigator initiates human
translational research studies with the goal of eventually applying knowledge from these initial studies to improve the
health of our patients.
Division of Endocrinology & Molecular Medicine
The Division of Endocrinology and Molecular Medicine has continued to maintain a high level of research and scholarly
activity. Several of our current full-time faculty are currently involved in our clinical or basic-science research programs. We
collaborate with many basic and other clinical departments in order to advance the research mission.
Marcelo Bonini, PhD – Professor of Medicine, is interested in determining how changes to the electrochemical potential of
the nucleus changes the chromatin epigenetic landscape, the interaction of transcription factors with co-regulators and
genomic loci, and how these events regulate gene transcription involved in breast cancer progression and inflammatory
diseases. His laboratory is currently funded by multiple grants from the NIH, DOD, and MCW Cancer Center.
Zeljko Bosnjak, PhD – Professor of Medicine, is interested in fundamental insight into the mechanisms responsible for greater
susceptibility of diabetic hearts to ischemia-reperfusion injury using both patient-derived cardiomyocytes and diabetic
animals. In addition, he is also performing translational studies to identify biomarkers involved in anesthetic-induced
neurotoxicity in children and cardiotoxicity of breast cancer chemotherapeutic agents. His laboratory is currently funded by
the NIH.
Ty Carroll, MD – Clinical Assistant Professor of Medicine, is interested in novel tools to diagnose and treat Cushing syndrome.
He is currently a co-investigator of multiple clinical trials for treatment of Cushing syndrome.
Carol Everson, PhD – Professor of Medicine, is investigating the ways in which long-term sleep deficiency is physically harmful
and increases morbidity and mortality. The laboratory has shown that long-term sleep deficiency in the animal model results
in unique metabolic, immune, and hormonal abnormalities. Current studies are investigating the mediation of arrested bone
formation and osteoporotic processes resulting from chronic sleep deficiency. Other organ systems—liver, lung, and
intestine—show increased DNA damage; this provides potential biological linkage to epidemiological findings of cancer risk
associated with chronic sleep deficiency. In a third area of concentration, sleep and sleep restriction, as well as other agents
that affect cerebral blood flow and metabolism, are being studied as interventions in mild concussive injury. The interventions
represent practical and low-cost means amenable to field implementation to improve outcomes from concussive injury,
determined by changes to brain functional connectivity, hormone status, and behavior.
James Findling, MD – Clinical Professor of Medicine and Surgery, is interested in novel tools to diagnose and treat Cushing
syndrome. He discovered the importance of inferior petrosal sinus sampling for the differential diagnosis of Cushing
syndrome and introduced late-night salivary cortisol as a simple screening test for Cushing syndrome. He is currently the PI
of clinical trials for treatment and diagnosis of Cushing syndrome.

MCW Research Overview
Jump to Table of Contents 221
Benjamin Gantner – Assistant Professor of Medicine, is interested in studying different types of inflammatory responses to
understand how they impact the decisions of innate immune cells (e.g. macrophages and neutrophils) to injure surrounding
host tissue. The lab uses microscopic observation of cells in living animals (i.e. intravital imaging) and in vitro culture systems
to study the intracellular processes, intercellular communications, and behavioral responses of immune cells during bacterial
infection and cancer.
Chenxia He, PhD – Assistant Professor of Medicine, is interested in the role of SOD2 as a new regulator of gene transcription
in the cell nucleus in the progression of breast cancer stemness and metastasis. Her research is currently funded by Research
Affairs Committee.
Srividya (Vidya) Kidambi, MD – Associate Professor of Medicine, is interested in the role of adiposity distribution, microRNA,
and resting metabolic rate in obesity pathogenesis, epigenetic modifications in chronic diseases such as hypertension &
cardiovascular outcomes, and circulating gut microbiome products. Her research is funded by AHA, AHW, and CTSI. In
addition, she is PI for multiple clinical trials for treatment of obesity, diabetes, and metabolic syndrome.
Paul Knudson, MD – Associate Professor of Medicine, is interested in evaluating outcomes of inpatient diabetes
management team and factors affecting readmission rates of patients with diabetes. He is also a co-investigator of a clinical
trial evaluating hypertriglyceridemia.
Theodore Kotchen, MD – Professor Emeritus, is primarily on mechanisms and complications of hypertension. He is currently
exploring the role of epigenetic modifications on cardiovascular outcomes. His research is funded by the AHA.
Hershel Raff, PhD – Professor of Medicine, is interested in two main research areas of interest. His basic research on the
hypothalamic-pituitary-adrenal axis focuses on the short- and long-term consequences of neonatal hypoxia. His clinical
research focuses on the development of diagnostic endocrine tests and, in particular, using the measurement of salivary
cortisol to evaluate the hypothalamic-pituitary-adrenal axis in a variety of human stress models.
Daisy Sahoo, PhD, Professor of Medicine, is interested in the role of scavenger receptors in cardiovascular disease, diabetes
and obesity. Specifically, she relies on state-of-the-art biophysical techniques to understand how the structural organization
of SR-BI, the most physiologically relevant HDL receptor, facilitates HDL-cholesterol delivery to the liver for disposal. In other
studies, she is trying to define the underlying mechanisms by which PCPE2, an extracellular matrix protein, facilitates the
cholesterol transport functions of SR-BI in adipocytes. She is also interested in unraveling how oxidative modifications
transform cardio-protective HDL into an atherogenic particle. Dr. Sahoo is currently funded by the NIH and the University of
Chicago Diabetes Research Training Center.
Jenna Sarvaideo, DO, Assistant Professor of Medicine, is interested in optimal hormonal treatments of transgender patients
in line with her clinical interests. She has received funding from the Endocrine Society and Faculty Development Grant from
the Department of Medicine. She was accepted into Clinical Research Scholars program for 2019. In addition, she is serving
as a co-investigator for multiple clinical trials evaluating treatments of type 2 diabetes and obesity.
Mary Sorci-Thomas, PhD, Professor of Medicine, is interested in examining the role of SR-BI and PCPE2 in adipose tissue lipid
metabolism using a newly developed adipose tissue specific PCPE2 knockout mice and inducible adipose tissue specific PCPE2
knockout mice. Her other research is focused on molecular mechanisms involved in high density lipoprotein apo A-I-mediated
protection against the progression of heart disease. She is currently funded by the NIH.
Division of Gastroenterology & Hepatology
As part of the Department of Medicine at the Medical College of Wisconsin, the Division of Gastroenterology and Hepatology
contributes to the MCW Research mission in several ways, spanning a variety of interests. The Division’s active clinical,
translational, and basic science research program involves gastroenterologists, hepatologists, advanced practice providers,
research scientists, research fellows, post-doctoral fellows, and a myriad of MCW medical students and Department of
Medicine residents. Our division places special emphasis on teaching and mentorship, as well as partnerships throughout the

MCW Research Overview
Jump to Table of Contents 222
College. Basic, clinical, and translational research efforts are heavily supported by several successfully funded NIH awards, as
well as internal funding from the Clinical and Translational Science Institute (CTSI) and Digestive Disease Center (DDC). During
the 2018-2019 academic year, the Division of Gastroenterology and Hepatology has been involved in research
spanningesophageal motility, IBD diseases including moderately to severely active Crohn’s disease or ulcerative colitis, Cyclic
Vomiting Syndrome, hepatic encephalopathy and esophageal obstruction caused by intrinsic or extrinsic malignancies,
refractory benign esophageal strictures or fistulas/perforations/leaks, and cystitis. This has resulted in many local, national,
and international oral presentations and publications of articles and manuscripts. Below is a short highlight of some of our
recent accomplishments:
Dr. Reza Shaker, Division Chief, collaborated with Dr. Nita Salzman from the Division of Gastroenterology in the Department
of Pediatrics, co-principal investigator, to successfully recruit a new fellow for the fourth year of hisNIH Training Grant (T32)
award. This grant allows for research intense training of 2 fellows each year in the area ofgastroenterology, while still allowing
for clinical exposure and training.
Dr. Banani Banerjee, Dr. Patrick Sanvanson and Dr. Jyoti Sengupta successfully submitted a competitive renewalof their R01
grant submission titled “Neuoromolecular Mechanisms of Chronic Pelvic Pain in Neonatally-induced Cystitis”.
Dr. Bidyut Medda received a seed grant from the DDC for his proposal entitled "Esophago-Cardiovascular Reflexes Following
Acute and Chronic Esophageal Acid Exposure in Rats".
Dr. Ivan Lang received a seed grant from the DDC for his proposal entitled "Development of an Animal Model for the Study
of Human Sleep Disorders of Airway Production".
Dr. Achuthan Souria received a seed grant from the DDC for his proposal entitled "Enteral Nutrition and Inflammation
Response in Obese Alcoholic Hepatitis".•In May, 2019, our Division presented a total of 23 posters and 6 presentations at
Digestive Disease Week in SanDiego.
Our ongoing clinical research studies in the Division currently include trials that assess the efficacy and safety of new
medications and devices. They also assess new dosing regimens for currently approved medications. We currently have a
total of thirty two active clinical trials in our Division. This includes twenty nine active IBD clinical trials (two by Dr. Beniwal-
Patel, one by Dr. Amir Patel, four by Dr. Daniel Stein, twenty two by Dr. Andres Yarur), two active hepatology clinical trials
(one by Dr. Kia Saeian, one by Dr. Achuthan Sourianarayanane), one motility clinical trial (Dr. Reza Shaker). We are in the
process of starting two new clinical trials including one hepatology clinical trial by Dr. Aiman Ghufran and a pancreatic cancer
clinical trial by Dr. Kulwinder Dua. Overall, we are working with ten different pharmaceutical and device companies. Our
Division maintains our industry sponsored trials while continuously identifying and engaging in new drug and device trials for
the future. The Division of Gastroenterology and Hepatology’s philosophy has always been strongly rooted in MCW’s
Research mission, as we believe this is the essential element to the advancement of medicine and innovation of patient-
centered care.
Division of General Internal Medicine
The Division of General Internal Medicine (GIM) has an active and nationally recognized research program focused on
conducting innovative clinical and outcomes research. Research efforts by GIM are based at the Medical College of Wisconsin
campus, the Clement J. Zablocki VA Medical Center, and in the local Milwaukee community. Research infrastructure includes
affinity groups focused on building research capacity and mentoring faculty interested in research, statistical and design
support to provide consultation and analysis for unfunded projects, and research conferences in collaboration with the MCW
Center for Advancing Population Science (CAPS). Faculty in GIM are actively involved in dissemination of their work through
peer-reviewed publications and participation in national and international conferences, including the Society of General
Internal Medicine (SGIM) and the Society of Hospital Medicine (SHM). Faculty also conduct collaborative work with other
Divisions, Departments, and the College of Pharmacy within MCW and local institutions.

MCW Research Overview
Jump to Table of Contents 223
Over the past 6 months, GIM has been awarded 4 large National Institute of Health (NIH) R01 grants to add to extensive local
and national funding. Faculty in GIM incorporate a variety of research designs into their research including randomized
controlled trials, community-engaged research, use of large administrative and clinical databases, and health systems based
quasi-experimental research. GIM research faculty have expertise in both quantitative and qualitative research, community
based participatory research, program evaluation, cost-effectiveness analysis, and implementation science. Research topics
range from evaluating policy changes at the national level like the impact of Medicaid regionalization on disparities in breast
cancer care, testing novel interventions to improve chronic care such as financial incentives for improving glycemic control,
addressing social determinants of health such as food insecurity, and recruiting participants for a national effort to expand
the future of precision medicine.
Division of Geriatrics & Gerontology
The Division of Geriatrics & Gerontology is engaged in a variety of clinical and educational research areas, which are intended
to advance patient care and innovate/optimize geriatrics education.
Over the years, the Division has had a series of awards to support its efforts in Geriatrics Education; including funding from
the National Institute of Aging-NIA (The Geriatric Medicine Academic Career Award), the Health Services and Resources
Administration, The Department of Veterans Affairs, the Hartford Foundation and AAMC as well as the Society of General
Internal Medicine, and 10 years of funding from the Reynolds Foundation for innovative geriatrics training. These awards
have sparked program and faculty development in the areas of undergraduate, graduate and continuing medical education.
For decades there has been funding for the Division from the Health Resources and Services Administration (HRSA) through
a subcontract with Marquette University for the Wisconsin Geriatric Education Center. In July 2015, funding was competitively
renewed for a new HRSA program: The Geriatrics Workforce Enhancement Program (GWEP). One focus of this award is
continuing professional development using geriatrics though the Part IV Maintenance of Certification (MOC) process targeting
primary care providers at MCW as well as other GWEP affiliates (UW and Aurora). Another focus has been the maintenance
and expansion of MCW’s Geriatrics Fast Facts, a repository of brief, to-the-point summaries of a discrete clinical problem.
Funding for this HRSA award was extended through June 30, 2019.
The Division maintains a variety of clinical research interest areas. These include: geriatrics syndromes (falls, delirium, urinary
incontinence); quality improvement studies; community home nursing care; hospice/end-of-life care; patient perceptions
and self-management of chronic illnesses such as diabetes and congestive heart failure; application of technology for
improving patient self-management and health behaviors; musculoskeletal conditions in aging; aging and immune function;
multi-morbidity and frailty. Active, cross-disciplinary collaborations are addressing minority health disparities and obesity,
Latino elders with dementia and their caregivers, physical activity and aging, and risks and potential interventions to address
unplanned, post-surgical hospital readmissions. These research initiatives have been funded through the National Institutes
of Health, the Agency for Healthcare Research and Quality (AHRQ), Veteran’s Health Administration, and the Healthier
Wisconsin Partnership Program, among others.
The Division participates in the MCW NIA T-35 award that supports 10 undergraduate medical students in summer research
each year including the summer of 2019. Most recently, the division has been working with CTSI on the development of an
interdisciplinary Ensemble addressing multi-drug resistant organisms and the interfaces between acute and long-term care
facilities.
Division of Hematology and Oncology
Building a robust clinical and laboratory research program is a primary mission of the Division of Hematology and
Oncology. Under the leadership of Parameswaran Hari, MD, MS, Division Chief, Dr. Mehdi Hamadani, Director of Blood and
Marrow Transplant (BMT) and Cellular Therapy Program, and, Drs. Ehab Atallah, James Thomas, Joshua Field and Wendy

MCW Research Overview
Jump to Table of Contents 224
Peltier, Section Heads of Hematologic Malignancies, Solid Tumor Oncology, Benign Hematology and Palliative Care,
respectively, the Division has been successful in creating a climate conducive to research and to developing high-quality,
nationally recognized research programs. Below is a summary of the research interests and activities that occur throughout
the Division.
Sameem Abedin, MD’s clinical and research interests are in the treatment of patients with myeloid malignancies including
acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), as well as Graft-versus-host disease after allogeneic
HCT. He is developing clinical trials for patients with relapsed AML, with a goal of investigating methods to improve disease
related outcomes. He additionally is developing trials related to GVHD.
Abdel Alqwasmi, MD’s research interests include breast cancer.
Ehab Atallah, MD’s primary interest is in the treatment of patients with leukemia, myelodysplastic syndromes (MDS) and
myeloproliferative disorders with special emphases on the treatment of patients with chronic myelogenous leukemia (CML).
He is co-Principal Investigator (PI) with Dr. Kathryn Flynn, MD on an R01 from the National Cancer Institute (NCI) to evaluate
stopping tyrosine kinase inhibitors in patients with CML who are in complete molecular remission. In addition, he is currently
the administrative director of the Jean Khoury Cure CML consortium (HJKC3) which is housed at MCW.
Lisa Baumann Kreuziger, MD, MS is a clinical and translational researcher with a focus in thrombosis. She has an interest in
device and cancer-associated thrombosis. She started the US network for venous thromboembolism research (VENUS,
https://www.htrs.org/HTRS/Research/Endorsed-Studies/VENUS-VTE-Network). Additionally, she is the institutional PI for
cancer-associated thrombosis trials. Lastly, she works in collaboration with Alan Mast, MD, PhD, in the Recipient Epidemiology
and Donor evaluation program (REDS-IVP) to understand outcomes of patients receiving transfusion for hematologic
conditions. Dr. Baumann Kreuziger also developed a study to evaluate a mechanism of how blood clots form in left ventricular
assist devices that is funded through a pilot grant from the CTSI. She works in collaboration with Alan Mast, MD, PhD, to
complete the biomarker studies involved in her clinical trials and understand the clinical implications of tissue factor pathway
inhibitor.
Alexandria Bear, MD’s research interests include experiential learning and development of end of life communication
workshops.
Juliana Perez Botero, MD’s research interest is in diagnosis and treatment of patients with inherited and acquired platelet
disorders, specifically genotype-phenotype correlation in patients with inherited disorders of platelet number and/or
function, development of new laboratory assays to evaluate platelet function and novel treatments of patients with immune
thrombocytopenia.
John Burfeind, MD's research interest includes enrolling patients with genitourinary malignancies in clinical trials.
Additionally, he has a significant role in the development of the Community Cancer Network, serving as the liaison between
the Division of Hematology and Oncology and the Cancer Care Network.
Kathryn Bylow MD's research interest is in the treatment of genitourinary malignancies. She has a long-standing research
interest in geriatric oncology and the long-term effects of cancer therapies. She is currently studying nutritional methods to
forestall the loss of muscle mass seen in men treated with anti-androgen therapy in prostate cancer.
Karen Carlson, MD, PhD’s research focus is on hematopoiesis. Using a novel mouse model system, she has identified a
requisite component of the early lymphopoietic niche. She is now working to elucidate the biochemical regulation of this
niche and its spatial localization within the bone marrow. Her research activities provide information about the basic biology
of the hematopoietic stem cell and early lymphocyte developmental environment and characterize new targets for niche-
directed therapy. Her long-term goal is to identify novel targets for the treatment of bone marrow failure syndromes and
hematopoietic malignancies. Dr. Carlson is the recipient of a K08 mentored career development award from the National
Heart Lung and Blood Institute.
John Charlson, MD's research interests are focused on the care of patients with sarcoma and young adult cancer patients.
Current efforts include chemotherapy clinical trials, evaluation of several potential biomarkers of treatment response, and
cancer care process improvement.

MCW Research Overview
Jump to Table of Contents 225
Lubna Chaudhary, MD, MS’s primary research interest is to better understand the biology of breast cancer tumors, as well
as different hormone receptors and how they impact patient outcomes. She is working to identify new drug therapies to
overcome cancer cell growth. Her investigator initiated clinical trial assessing neoadjuvant endocrine therapy and tumor
molecular changes in patients with breast cancer was the recipient of funding from the Rock River Foundation and the MCW
Cancer Center in 2017. Another investigator initiated clinical trial assessing the role of PD-1 inhibition in breast cancer patients
undergoing neoadjuvant chemotherapy was recently funded by a CTSI KL-2 grant funded by Advancing a Healthier Wisconsin
Research and Education Program (AHW REP).
Xiao Chen, MD, PhD’s research focuses on the role of micronutrients in regulating GVHD. His lab is investigating how vitamin
A and vitamin D affect GVHD risk after allogeneic stem cell transplantation using animal models. He is also investigating how
to target nuclear receptors including retinoic acid receptor and vitamin D receptor to mitigate GVHD.
Yee Chung Cheng, MD’s research interest is in the development of clinical trials focusing on the investigative use of
chemotherapy and/or novel therapy in high risk breast cancer cases such as triple negative breast cancer or inflammatory
breast cancer particularly in the pre-operative setting.
Saurabh Chhabra, MD, MS is a BMT-trained clinician with interest in BMT and high-risk multiple myeloma. His current
research interests include clinical trials for drug development in the areas of plasma cell neoplasms and improving outcomes
of allogeneic hematopoietic cell transplantation. He is the Principal Investigator (PI) for an Investigator-Initiated study
evaluating the utility of anti-IL-6 monoclonal antibody tocilizumab for prevention of Graft-versus-Host Disease (GVHD) in
patients receiving allogeneic transplant for hematologic malignancy. He is also involved in the BMT CTN studies, as the site PI
of CTN 1501 (evaluating role of sirolimus for treatment of standard-risk GVHD after allogeneic transplant) and as a protocol
team member of the CTN 1801 study (examining impact of gut microbiome on transplant outcomes). He is also the site PI for
a number of phase I and II clinical trials for treatment of newly diagnosed and relapsed/refractory multiple myeloma. He is
also actively involved with transplant registry (Center for International Blood and Marrow Transplant Research; CIBMTR)
studies, as Scientific Director of Regimen-Related Toxicity Working Committee.
Christopher Chitambar, MD’s research focuses on the role of iron and iron proteins in tumor growth and the development
of novel metallodrugs to target tumor iron homeostasis and mitochondrial function in non-Hodgkin's lymphoma and brain
tumors. He also studies the role of mitochondrial dysfunction in the development of fatigue in patients with early stage breast
cancer receiving adjuvant chemotherapy.
Binod Dhakal, MD, MS’s Binod Dhakal, MD, MS’s research focuses on multiple myeloma and related plasma cell disorders.
He completed two early phase studies in multiple myeloma: one looking at the novel drug combination in the management
of relapsed/refractory multiple myeloma and the other on the pharmacokinetics of new Melphalan both of which were
published. He has secured funding for 2 more early phase studies: one looking at the novel induction therapy in multiple
myeloma patients with renal injury, and that also evaluates the role of novel biomarker for renal recovery. The other study is
an entirely new drug targeting PIM kinase with the study evaluating a dual role of anti-myeloma and bone protective effect.
He was awarded a pilot grant from American Cancer Society to explore the role of micro-RNA in multiple myeloma bone
disease and the results looking promising to be tested in a larger setting. Additionally, in collaboration with investigator from
University of Wisconsin Madison/UCSD, he was awarded a prestigious Translational Research Program grant from Leukemia
and Lymphoma Society to explore the role of matrikines in the immune regulation of myeloma. This concept is being
investigated prospectively through a nationally conducted multi-center BMT CTN study.
William Drobyski, MD’s laboratory evaluates multiple aspects of the immunobiology of allogeneic HCT with particular
emphasis on Graft-versus-Host Disease (GVHD) biology. By employing murine models of stem cell transplantation, this
research aims to understand the interplay between the inflammatory and regulatory arms of the immune system and how
they impact the severity of GVHD. Dr. Drobyski has been continuously funded by NIH for this work since 1991. He currently
has two NIH grants that are directed at understanding the pathophysiology of GVHD and is particularly interested in
developing new approaches for the prevention of this disease in the gastrointestinal tract which is the major site of morbidity
in patients. He also has an interest in the translation of pre-clinical studies into the clinic to attenuate GVHD in patients.
Anita D’Souza, MD, MS is an Associate Professor of Medicine with a research focus in plasma cell disorders including multiple
myeloma and amyloidosis. She is the Scientific Director of the Plasma Cell Disorders and Adult Solid Tumors working

MCW Research Overview
Jump to Table of Contents 226
committee of the CIBMTR. In addition to conducting clinical trials, she also leads efforts to study quality of life and patient-
reported outcomes in these diseases. She mentors multiple trainees on research projects in this area.
Mary Eapen, MD, MS's research is in alternative donor and grafts for allogeneic HCT for acute leukemia and non-malignant
diseases.
Timothy Fenske, MD, MS’s clinical and research interests focus on the care of patients with lymphoma. He has a strong
interest in refining the use of hematopoietic cell transplantation (HCT) as a treatment for lymphoma. He is a co-chair of the
Lymphoma Working Committee of the Center for International Blood and Marrow Transplant Research (CIBMTR). He is the
co-chair of a national (Intergroup) trial evaluating the use of maintenance therapy with ibrutinib to prevent recurrence of
diffuse large B-cell lymphoma after autologous HCT. He is also the national Principal Investigator for an Intergroup trial
evaluating a deep sequencing minimal residual disease assay to help direct therapy for mantle cell lymphoma patients in first
remission.
Joshua Field, MD’s research program focuses on of clinical studies in adults with sickle cell disease. Particular areas of interest
include acute and chronic pain, pulmonary complications, transfusion, and therapeutic studies.
Patrick Foy, MD's current research focuses on management of bleeding in patients with hereditary hemorrhagic
telangiectasia with therapy designed to decrease blood vessel growth (VEGF inhibition). Dr. Foy also assists in ongoing clinical
trials in hemophilia and thrombosis. He also is actively engaged in educational research designed to improve teaching of
medical students, residents, and fellows in hematology and oncology.
Kenneth Friedman, MD is a clinical laboratory investigator who is involved with numerous clinical trials with several academic
institutions, Industry and the NIH investigating the role of diagnostic laboratory hemostasis and thrombosis testing in the
evaluation of patient cohorts.
Ben George, MD's research focus is on pancreatic and gastro-esophageal cancers. He is interested in experimental
therapeutics, specifically, clinical trials targeting putative molecular mechanisms involved in the development and
progression of gastrointestinal malignancies. Dr. George chairs the Molecular Tumor Board - a monthly meeting that analyzes
genomic alterations in tumors to identify appropriate targeted treatment options. Further, he represents Froedtert and
Medical College of Wisconsin at the Precision Medicine Exchange Consortium, of which MCW is a founding member. The goal
of the consortium is to pool clinically annotated molecular data among member institutions and use that information to
develop clinical trials aimed at actionable genomic alterations. He is the institutional Principal Investigator on several clinical
trials in both Pancreatic and Gastro-esophageal Cancers.
Thomas Giever, DO, MBA’s main research interests are enrolling patients on genitourinary clinical trials. Additionally, building
a robust general oncology clinical trial portfolio at the Drexel Town Square Health Center Cancer Center within the Froedtert
Community Cancer Network and Division of Hematology and Oncology.
Jonathan Gully, MD is interested in the culture of palliative care, specifically, better integration of palliative care into medical
student education. He is in the final stages of testing a palliative care app to augment educational efforts, with the hope of
getting insights into how students and resident’s interface with technology at bedside.
Guru Subramanian Guru Murthy, MD’s clinical and research interests focus on the outcomes of patients with leukemia and
stem cell transplantation. He conducts retrospective and prospective clinical studies in patients with leukemia and stem cell
transplantation with a goal of improving disease related outcomes"
Mehdi Hamadani, MD’s research interest includes lymphoma, GVHD, and alternative donor transplantation. He is the
Scientific Director of the CIBMTR’s Lymphoma Working Committee, and the Medical Director of MCW BMT and Cell Therapy
Program. He has investigated the role of immunomodulation with HMG-CoA reductase inhibitors and TNF-alpha blockers for
preventing acute GVHD as well as the role of the novel proteasome inhibitor MLN9708 in preventing chronic GVHD. As part
of BMT CTN’s Data Coordinating Center, Dr. Hamadani is intricately involving in the development and conduct of several
cooperative group trials looking at prevention and treatment of GVHD, and mitigation of post-transplant relapse-risk in acute
leukemias.

MCW Research Overview
Jump to Table of Contents 227
Parameswaran Hari, MD conducts clinical research evaluating novel therapies for plasma cell disorders including myeloma
and amyloidosis as well as novel approaches for transplantation. He is the Scientific Director of the CIBMTR’s Plasma Cell
Disorder Working Committee and co-Chair of multiple national trials for multiple myeloma. He is also an investigator on
several novel drug phase I and II trials in multiple myeloma several of which have led to FDA approval. In addition, he has
projects in development for translational applications of cell-based therapeutics in malignancies, spinal cord injury,
hemophilia and other immune therapies.
Mary Horowitz, MD, MS leads two international programs to evaluate and improve outcomes of hematopoietic stem cell
transplantation (HCT): the CIBMTR (described separately), funded by the NCI, NHLBI and NIAID and the Blood and Marrow
Transplant Clinical Trials Network (BMT CTN), funded by NHLBI and NCI. The CIBMTR maintains a large outcomes registry
compiling data on HCT recipients in more than 350 centers in more than 40 countries. The BMT CTN conducts large
multicenter trials and enrolls patients from more than 100 centers in the US, Canada, France and Germany. In 2018, Dr.
Horowitz received an additional grant from the NCI to establish a Cellular Immunotherapy Data Resource, which collects data
on outcome of non-transplant cellular therapies for cancer.
Siegfried Janz, MD’s primary research interest concerns neoplasms of terminally differentiated, immunoglobulin producing
B-lymphocytes called plasma cells. Relying in part on gene-insertion mice that mimic different fine structures of the human
MYC-activating t (8;14) (q24;q32) translocation, he recapitulates important features of human plasma cell myeloma (multiple
myeloma) in single and compound transgenic mice. His laboratory takes advantage of mouse models of this sort to elucidate
mechanisms of neoplastic plasma cell development and evaluate new approaches to myeloma treatment and prevention.
The long-term goal of Dr. Janz’s work, which is supported by NCI grants and other external revenue streams, is to improve
the outcome of patients with myeloma and related blood cancers. To that end, he collaborates with fellow investigators from
HemOnc, the Department of Medicine and the MCW Cancer Center.
Bryon Johnson, PhD conducts basic/translational research on adoptive T cell immunotherapies for both hematologic
malignancies and solid tumors. He is also Director of the BMT Cell Therapy Laboratories, which processes hematopoietic
progenitor cells and immune cells for the MCW Blood and Marrow Transplant Program and participates in the development
of novel immune cell therapies for patients with cancers and other diseases. The labs also provide some immune monitoring
services for investigators involved in immunotherapy clinical trials.
Sailaja Kamaraju, MD has research interest in breast cancer and more specifically, how breast cancer mortality rates can be
reduced in vulnerable, and underserved populations through community-based initiatives, for which she has received several
Susan G. Komen grants. She works with Patient Centered Outcomes Research (PCOR) evaluating cancer treatment related
toxicities and cancer survivorship disparities.
Deepak Kilari, MD's research focuses on genitourinary cancers, including early phase and translational trials. Dr. Kilari and
his collaborators are also studying how copper transport proteins play an important role in the sensitivity of cancer cells to
platinum-based chemotherapy, as well as the role of exosomes micro RNAs in predicting treatment responses in men with
prostate cancer. He is also the Principal investigator of a phase 2 study looking at the role of upfront enzalutamide and
dutasteride for elderly men with systemic prostate cancer. He is actively involved in outcomes research at the Clement J
Zablocki VA Medical Center.
Walter Longo, MD is interested in alpha/beta depletion with haploidentical donors to lessen complications of GVH but
preserve graft versus tumor. He is also interested in CAR-T for lymphoma, myeloma, CLL and other hematologic malignancies.
Subramaniam Malarkannan, PhD's research interests include signaling cascades that regulate the development and
functions of human Natural Killer cells (NK) patients with malignancies, inherited diseases and infections, and developing
translational models to improve the anti-tumor efficacy of human NK cells. His team uses cellular, biochemical, and
transcriptomic (single-cell RNA-seq) approaches. Research in his laboratory is supported by NCI, NIH, MACC Fund, Nicholas
Family Foundation, and Gardetto Family Endowed Chair.
Sean Marks, MD's research interest is in Palliative Care Education among physicians in training, prognostication, and
psychological issues at the end of life.

MCW Research Overview
Jump to Table of Contents 228
Smitha Menon, MD’s research interest is in the role of novel agents and targeted therapy in the treatment of lung cancer.
She is the PI of multiple clinical trials.
Laura Michaelis, MD's research interests are in the care of patients with acute and chronic leukemias. She conducts research
on novel agents in the treatment of these diseases and in ways to better manage the side effects and toxicities of therapies.
She is the primary investigator of a national clinical trial being developed to test low-intensity therapy for older individuals
who have acute myeloid leukemia.
Prabhas Mittal, MD's research interests are in clinical trials, specifically cooperative group clinical trials and drug
development.
Ariel Nelson Primary research interests include genitourinary malignancies, immunotherapy and novel therapeutic and
combination clinical trials.
Marcelo Pasquini, MD, MS research focus on applications of cellular therapies for the treatment of cancer. Dr. Pasquini
oversees two large post-marketing studies to evaluate the efficacy and safety of commercial CAR T cells in a real-world setting.
His research also focuses on transplants and cellular therapies for the treatment of multiple myeloma, acute leukemia, and
lymphoma.
Wendy Peltier, MD's research interests include quality improvement models for ‘upstream’ palliative care in cancer and
advanced heart failure and creating models for inpatient hospice in the ICU setting. She also serves on the Kern Faculty Pillar,
with interest in educational programs that support Caring and Character in end-of-life care.
Katherine Recka, MD has research interests in palliative care education and bioethics. She has led quality improvement
initiatives based upon key program data obtained from the quarterly, nationwide Department of Veteran’s Affairs (VA) family
bereaved survey. Her program has been selected to help other VA programs lead similar initiatives to enhance end-of-life
care in the veteran population.
Mary Rhodes, MD’s research interests include identification of language and cultural barriers to quality palliative care
services. She is particularly interested in the impact of limited English language proficiency on communication with patients
with serious illness.
Kimberly Ridolfi, MD's research interests include treatment of solid tumors, survivorship, and quality care of our veterans.
Research in Matthew Riese, MD, PhD’s lab focuses on understanding how T cells are affected by the tumor
microenvironment, and how they can be manipulated to overcome the inhibitory mediators present within that environment.
Dr. Riese’s laboratory focuses on diacylglycerol kinases, proteins that serve as intracellular brakes to dampen T cell activity,
and PECAM-1, a cell adhesion protein that is required for efficient TGF-beta signaling in T cells.
Paul Ritch, MD’s clinical research focus includes patients with gastrointestinal malignancies with particular interest in
pancreatic cancer. He is part of a multidisciplinary research team conducting multimodality clinical trials in patients with early
stage disease and is involved in protocols evaluating new strategies and novel agents targeting pancreatic cancer cells and
tumor stroma and extracellular matrix in advanced disease.
J. Douglas Rizzo, MD, MS’s research interest is in late effects after transplantation, quality of life, and financial impacts upon
patients. He also performs the annual center specific outcomes analysis for US transplant centers and has an interest in
hospital outcomes reporting.
Lyndsey Runaas, MD’s research interests include improving outcomes for patients undergoing allogeneic bone marrow
transplant. Specifically, this includes understanding and preventing graft-versus-host disease, studying the role of the
intestinal microbiome in bone marrow transplant, and trying to optimize communication between patients with advanced
hematologic malignancies and their providers. She hopes to continue to foster a translational and collaborative research
career incorporating both qualitative and quantitative methods to improve the outcomes of patients with advanced
hematologic malignancies.

MCW Research Overview
Jump to Table of Contents 229
Wael Saber, MD, MS conducts clinical research evaluating outcomes of autologous and allogeneic HCT. He is the Scientific
Director of the CIBMTR’s Chronic Leukemia, Acute Leukemia, and Health Services & International Issues Committees. His
research primarily focuses on patients with MDS and on issues related to cost-effectiveness and access to HCT care. He is the
protocol officer for a national clinical trial comparing transplantation to non-transplant therapies among older MDS patients
(BMT CTN 1102). He is a co-principal investigator of an ancillary R01 grant to evaluate the cost-effectiveness of these two
treatment approaches among older MDS patients participating in BMT CTN 1102.
Nirav Shah, MD MSHP’s research interests includes lymphoid malignancies, cellular and immunotherapy, and bone marrow
transplant. He is leading the internal CAR-T cell trial for non-Hodgkin lymphoma at MCW and is working on developing new
treatment regimens for patients with relapsed hematological malignancies.
Bronwen Shaw, MD, PhD has an interest in health-related quality of life and survivorship issues in patients who undergo
hematopoietic cell transplantation (HCT). She is especially interested in the ability of patient reported outcome (PRO)
collection to predict patient experience and clinical outcomes. She also has an interest in hematopoietic cell donors, both in
terms of their experience and in terms of determining factors which help to select the best donor for an individual patient.
Roy Silverstein, MD’s lab focuses on platelet and macrophage biology as they relate to common vascular diseases, including
atherosclerosis and arterial thrombosis. Dr. Silverstein’s work centers on a cell signaling system mediated by the type 2
scavenger receptor CD36. As a receptor for long chain fatty acids CD36 mediates cellular metabolism in many cell types,
including tumor stem cells and tumor infiltrating macrophages. As a pattern recognition receptor on macrophages and
platelets for numerous “danger signals,” including oxidized low-density lipoprotein (oxLDL), glycated proteins, cell-derived
extracellular vesicles and bacterial cell wall components, CD36 mediates innate immune responses that contribute to
inflammation, thrombosis and atherogenesis.
Liza Thiel, MD, MS’s research interest is in Palliative Care Education in the community setting.
James Thomas, MD, PhD's research interest is in oncology drug development and the role of reactive oxygen species in cancer
development and treatment.
Jonathan Thompson, MD, MS has interest in clinical and translational research related to thoracic malignancies, particularly
regarding the use of immunotherapy and novel agents for the treatment of lung cancer. Recently, he has focused on the
impact of the microbiome on immunotherapy outcomes in non-small cell lung cancer.
The laboratory of Li-Shu Wang, PD is investigating the ability and mechanisms of active metabolites from black raspberries
(BRBs) to influence colon and pancreatic cancer immunology through epigenetic modifications. The results from animal
models of both cancer types indicate that the berries dampen tumor-induced immune suppressive microenvironment by
decreasing CD11b+ myeloid cells and boosting CD8+ T-cell and natural killer cells. In an effort to translate these findings from
laboratory to clinical use, Dr. Wang is collaborating with Dr. Ehab Atallah on the effects of black raspberries on DNA
methylation in patients with myelodysplastic syndrome (MDS). This trial was awarded the Kurtis Froedtert CTO Seed Grant in
January 2017. The aim of this clinical trial is to evaluate the hypomethylating properties of BRBs in patients with MDS monthly
for 12 weeks of BRB supplementation.
Jo Weis, PhD's research interests include psychological phenomena at the end-of-life including anticipatory grief and post-
traumatic symptomatology.
Gilbert White, MD’s research focuses on the role that blood platelets play in heart disease and strokes. Specifically, he is
using genetic and proteomic approaches to study the intracellular signaling pathways that mediate integrin activation, a key
event in platelet aggregation. The overall goal of his work is to understand the signaling processes in order to identify
druggable targets that will more safely and effectively modulate platelets. Rap1b is a small GTPase in platelets that has
features of a bidirectional regulator of integrin activation. His current work is aimed at understanding the mechanism of rap1b
action.
Krista Wiger, MD's research interests are in maintaining resiliency among practitioners as well as exploring quality
improvement opportunities and hospital readmissions issues specific to inpatient oncology.
MCW Research Overview
Jump to Table of Contents 230
Stuart Wong, MD conducts clinical research evaluating novel therapies for head and neck cancer, and in particular, agents
that are used concurrently with radiation therapy. His research efforts include NCI funded clinical trials. His research also
focuses on national patterns of care for head and neck cancer treatment, and mitigation of toxicity from head and neck cancer
treatment, and cancer prevention. Dr. Wong is the lead investigator for the Lead Academic Participating Site (LAPS) of the
NCI’s National Clinical Trial Network at MCW. MCW is one of the top 32 institutions in the country to receive a LAPS award.
He also received an RO1 NIH grant with Ming You, MD. PhD, to study a new agent in patients with oral cancer.
Fenlu Zhu, PhD’s research interest has been focusing on immunotherapy especially preclinical process development and
validations; large-scale cGMP manufacturing of cellular products including patient cell purification, expansion, transduction
and formulation; product characterization and release testing; technology transfer from research bench to clinical
production; quality control, FDA regulations and FACT accreditations; SOP preparation and investigational new drug (IND)
applications; immune monitoring and correlative studies pre and after cellular therapy infusion. Related to this area, cellular
therapy products have been manufactured under cGMP for clinical trials including multi-specific (EBV, CMV and Adenovirus)
cytotoxic T lymphocytes (CTL) in G-Rex system and CD20_CD19 dual chimeric antigen receptor (CAR) T cells using CliniMACS
Prodigy Device for the treatment of B cell malignancies.
Division of Infectious Diseases
The Division of Infectious Diseases is involved in multidisciplinary and collaborative research efforts with internal and external
partners. Faculty are engaged in a variety of clinical research trials conducted in collaboration with research networks and
industry sponsored trials. Several HIV treatment, HIV prevention, and Influenza Phase III drug trials and network trials are in
active enrollment and will determine the safety and effectiveness of various new treatments. The Division also conducts
studies in infection control and hospital epidemiology. In close collaboration with the MCW Center for AIDS Intervention
Research (CAIR), the Division’s behavioral and community research is supported by several key institutions including the
National Institute of Mental Health, National Institute on Aging, Centers for Disease Control and Prevention, and the
Wisconsin AIDS/HIV program. Division faculty work closely with CAIR to develop, conduct, and evaluate new interventions to
prevent HIV among individuals most vulnerable to the disease. Several ongoing laboratory-based research projects headed
by key members of the Infectious Diseases division. In addition, other research is aimed at addressing international health
issues.
Primary research investigators include:
Dr. Bilal Abid’s research interest intersects in areas of both Oncology and Infectious Diseases. He heads projects dealing with
immunotherapy, cytokine release syndrome, CAR T-cells, malaria, as well as the gut microbiome. He analyses haploHCT
patients at MCW to study the association between CRS and infections. He spearheads a study in genomic profiling of a case
of tumor hyper progression with pre-existing Li Fraumeni Syndrome that spans across both the Division of Infectious Diseases
and Hematology and Oncology.
Dr. Sol Aldrete is currently working on project in which the Retrospective observational study of patients who received BCG
vaccination seeking to identify patient factors associated with Mycobacterium bovis infection after instillation of the vaccine
for bladder cancer. This is a study in the VA along with Dr. Gundacker. Second project is looking at HIV Preexposure
prophylaxis initiation and retention in care at an HIV health care system in Wisconsin.
Dr. Jenifer Coburn’s research interests focus on pathogenic spirochetes, a group of bacteria that are able to cause persistent,
disseminated infections in immunocompetent animals, including humans. The Coburn lab is currently working with Borrelia
burgdorferi, which is maintained in a tick-animal cycle in nature. They also work with another pathogenic spirochete,
Leptospira interrogans. Leptospires are maintained in infected animals in nature but can also survive in water and mud. The
focus of the work with both Borrelia and Leptospira is to identify and then test the biologic significance of bacterial proteins
that help the bacteria bind to mammalian cell surface receptors, to identify the mammalian cell surface receptors recognized
by the bacteria, and ultimately the biological and pathologic significance of the bacterial-mammalian receptor interaction.

MCW Research Overview
Jump to Table of Contents 231
Dr. Carlos Figueroa-Castro's projects include implementation of telemedicine consultation solutions in the inpatient setting,
and its impact in patient's outcomes; use of open-source statistical software (RStudio) to perform analytics of electronic hand
hygiene monitoring; and to study the correlation between data management organization strategies and infection prevention
program effectiveness.
Dr. Michael Frank is currently conducting two large NIH-funded clinical trials in individuals with HIV infection. The first is as
an affiliate of the International Network for Strategic Initiatives in Global HIV Trials (INSIGHT), the START trial (Strategic Timing
of Anti-Retroviral Treatment), which is answering the question of the optimal timing of initiation of antiretroviral therapy
(ART) with regard to morbidity and mortality among HIV-1 infected patients. The second is the Randomized Trial to Prevent
Vascular Events in HIV (REPRIEVE) trial through the AIDS Clinical Trials Group, which is examining whether use of an HMG-
CoA reductase inhibitor improves outcomes in HIV-positive patients who are at low or moderate risk of cardiovascular events.
Dr. Jamie Green’s research clinical and research interest are in the areas of infections of immunocompromised hosts including
leukemia, lymphoma, stem cell and solid organ transplant. Past projects included immune reconstitution after stem cell
transplant and herpesviruses (cytomegalovirus and human herpesvirus 6) as well as infections in heart or lung transplant
recipients. Currently she is pursuing projects that aim to improve overutilization of antibiotics in neutropenic patients with
leukemia, lymphoma or stem cell transplant, and creations of a comprehensive dataset on infections in heart and lung
transplant recipients; specifically, to evaluate those who have an active infection at the time of transplant.
Dr. Michael Kron is leading an NIH-funded collaborative study investigating compounds that might be useful in treating
human filiarial diseases, which infect millions of persons. In collaboration with an international network of laboratories, the
researchers are working to identify novel chemical scaffolds that inhibit recombinant parasite aminoacyl-tRNA synthetase
(AARS) and predict the structure using computer modeling. Under an exploratory grant from the Fogarty International Center
of NIH, research has also focused on the natural products and biodiversity issues of terrestrial and marine organisms in the
Philippines. He also collaborates with the Viral Oncogenesis group at the US National Cancer Institute who are looking at the
relationship between certain HHV8 genotypes and IgE levels. In a project that evolved from time as a US State Department
Senior Science Advisor, and in collaboration with WHO mental health, he analyzed data in Global Mental Health in the 21
countries of APEC (Asia Pacific Economic Cooperation).He lead an MCW based project in collaboration with the Molecular
Parasitology Research Unit, Queensland, Australia, comparing DNA sequence of parasite DNA extracted from a kidney-liver
transplant recipient and mitochondrial DNA databases in order to determine the species of parasite and the country where
our patient became infected.
Dr. Sheran Mahatme is involved in a variety of quality improvement and clinical research projects at ZVAMC. She has
partnered with Allergy/Immunology, Emergency Medicine, and ID Pharmacy in reassessing beta lactam allergy listings and
has supported ID Pharmacy in conjunction with Geriatric Medicine and Nursing in developing an algorithm to reduce the
acquisition and unnecessary antimicrobial use in asymptomatic bacteriuria. Dr. Mahatme has worked with Inpatient Internal
Medicine, Radiology and Nursing to initiate a Venous Access Team to provide a standardization process for long term venous
access placement and has collaborated with ID Pharmacy in assisting the Department of Surgery’s reassessment and update
of antimicrobial surgical prophylaxis. She has spearheaded implementation of the ANNIE Program on a local level to improve
the medical adherence, retention and linkage of care of people living with HIV and those on pre-exposure prophylaxis. Finally,
Dr. Mahatme is involved in two clinical studies, one looking at developing an improved interferon release gamma assay using
specific T cell stimulation for the detection of M. tuberculosis, and the second as a site co-investigator for a National VA
Cooperative Study assessing the optimal treatment for recurrent C. difficile infection by comparing the efficacy of oral
Vancomycin, oral Vancomycin (taper and pulse) and Fidaxomicin.
Dr. Silvia Munoz-Price’s research deals with the horizontal transmission of organisms within the healthcare environment.
This includes initial acquisition and development of infections with multidrug resistant organisms, microbiota disruption,
antibiotic exposures, environmental contamination, and hand hygiene. Dr. Munoz-Price is also conducting clinical trials
looking at prevention of Clostridium difficile colitis in patients colonized with C. difficile. Additional topics of interest include
analyses of time dependent variables (i.e. antibiotics) and quality and patient safety indicators, such as hospital readmissions.

MCW Research Overview
Jump to Table of Contents 232
All activities are performed in close collaboration with the Enterprise Infection Control Departments, the Antibiotic
Stewardship teams, the Quality Department and the Clinical Microbiology Laboratory. Using an array of approaches and data
collection, research is focused on reducing the spread of infection among medical and surgical patients within the hospital
environment.
Dr. Andrew Petroll’s research interests include understanding health care providers’ knowledge and experience with HIV
prevention methods and studying how to increase their awareness of such methods. Research is also examining factors that
affect that affect medication adherence and retention in medical care among older HIV-positive patients in rural areas.
Dr. Joyce Sanchez’s main research interest is in illness related to international travel. She has collaborative projects with the
Department of Microbiology and Immunology investigating immune responses to vector borne illnesses as well as with the
Blood Center of Wisconsin analyzing of human immunity after vaccination to predict pathogen epitopes for improved vaccine
development.
Division of Nephrology
The main research priorities of the Division of Nephrology include:
Kidney Stone Research:The kidney stone research group investigates the pathophysiologic mechanisms mediating the
initiation and progression of urinary tract and kidney stone disease. Research is focused on: (i) studies on the epidemiological
patterns of stone disease, (ii) mechanisms of stone initiation, (iii) genetic linkages between stone disease and hypertension,
(iv) the development of new animal models to study calcium oxalate stone disease, and (v) composition variations in recurrent
stone patients. Targeted research is also conducted on the physical, chemical and physiologic mechanisms of crystal
nucleation, growth, and aggregation of crystals that form within the nephron and in related vascular tissue.
Research in Acute Kidney Injury: One area of laboratory research focuses on ischemic acute kidney injury (AKI), with goals
to: (i) translate laboratory discoveries in AKI to clinical medicine, and (ii) perform experiments that further explore questions
generated at the bedside. Current projects are aimed at: (i) the development of new therapies to prevent or treat AKI based
on an understanding of the genetic, physiologic, and molecular mechanisms that underlie the ischemic kidney injury, and (ii)
evaluation of the long-term effects of acute renal ischemia.
Research in Renal Cell Biology and Signaling: NIH funding supports multiple projects focused on cell signaling as related to
pathobiology of kidney disease. Research is primarily focused on characterizing the molecular mechanisms underlying the
activation and termination of signaling pathways, as well as defining the cellular consequences of specific stimulation of these
cascades in systems relevant for the signaling from G-protein coupled receptors.
Clinical Research on Diabetic Nephropathy, Chronic Kidney Disease (CKD), End-Stage Renal Disease (ESRD), and Renal
Transplantation: There are several areas of ongoing clinical research activity in subjects with CKD and ESRD. Recent trials in
CKD and ESRD have studied new treatments for diabetic nephropathy, secondary hyperparathyroidism, and prevention of
vascular calcification. The Division of Nephrology has participated in several large clinical trials investigating novel
immunosuppressive agents and protocols in patients following kidney transplantation. Other studies have explored
technologies for imaging of maturing dialysis vascular access and gene expression profiling, proteomics and complex trait
genetics in kidney transplantation.

MCW Research Overview
Jump to Table of Contents 233
Division of Pulmonary & Critical Care
The division of Pulmonary and Critical Care Medicine has a rich research environment, where our faculty and research staff
complement departmental goals of identifying ways and/or means of improving outcomes and quality of life for our patients.
Our current research support team features six full-time clinical research coordinators, full-time research assistant, three
basic science support staff and a part-time system specialist to assist the faculty in conducting translational and clinical
research and basic science. With this support, faculty and fellows conduct internally and extramurally funded research,
publish and present findings which further highlight the division’s strong commitment to excellence in research and
outcomes.
The division strives to offer opportunities to our patients to participate in a variety of trials. The faculty, fellows, and research
coordinators are engaged in many clinical and investigator-initiated research projects conducted in collaboration with several
foundations, networks, and industry-sponsored partners. Additionally, our team assists others within the Department of
Medicine as needed to onboard staff/faculty to research, assist in protocol preparation, submissions, regulatory, budgeting
and other tasks as requested.
• Cystic Fibrosis (CF) & Nontuberculous Mycobacterial (NTM) working to improve outcomes and quality of life in
patients. Focus in improving airway and breathing, reducing infections and inflammation, thereby increasing quality
of life and survival time.
• Pulmonary Hypertension (PH) developing registries and new approaches in treatments with an emphasis on
extending survival rates.
• Idiopathic Pulmonary Fibrosis (IPF) education by developing long-term care plans.
• Chronic Obstructive Pulmonary Disease (COPD) identifying safety and efficacy of medications in patients.
• Critical Care (CC) includes quality improvement, investigator initiated, and industry sponsored observational and
randomized controlled trails evaluating therapeutics and outcomes related to sepsis, acute respiratory distress
syndrome, ICU-related delirium, end of life care, family-provider communication, acute pulmonary embolism,
diagnostic reasoning, and nutrition.
• Interventional Pulmonary (IP) incorporating research with the use of advanced diagnostic and therapeutic
techniques.
• Investigator-Initiated Trials (IIT) finding ways to improve critically ill patients how we can provide maximum benefit
and improved outcomes,
Pulmonary & Critical Care Medicine has over 52 active projects, 27 industry, 25 IIT, 7 grants with 1 funding through the
CTSI/AHW and 3 awards with the CF Foundation. These projects are primarily led by: J Biller, MD, V Bonne MD, R Franco MD,
D Ishizawar MD, D Kogan MD, J Kurman MD, R Lipchik MD, MD, R Nanchal MD, J Patel MD, K Presberg MD, V Ramalingam
MD, A Taneja MD, T Ferrer Marrero MD, K Maso MD, & J Truwit MD. Supported by; Jeanette Graf RM, Erin Hubertz, Ashley
Wuerl, Jennifer Peterson, and Amy Blair CRC II, Shannon Broaddrick and Erika Olmos CRC I, Shama Sharwani System Specialist
II.
2019 has brought several new opportunities of research and collaboration to our department, we look forward to the many
new endeavors on the horizon.

MCW Research Overview
Jump to Table of Contents 234
Division of Rheumatology
The Rheumatology Division at the Medical College of Wisconsin has a strong history of research, largely in crystal-related
arthritis, and has continued this focus, while simultaneously pursuing work in Systemic Lupus Erythematosus (SLE) and
scleroderma, and participating in clinical trials of SLE and scleroderma. We are always interested in collaborations and have
expertise that spans bench research, industry-sponsored clinical trials and investigator-initiated human studies. We have
assistance from a clinical research coordinator in the department of medicine and expert laboratory personnel at the VA.
Ann Rosenthal, MD continues to work on crystal arthritis, with a focus on calcium pyrophosphate deposition disease (CPPD).
She runs a federally-funded research program at the Zablocki VA where she is delineating mechanisms of calcium crystal
formation in articular cartilage. Dr. Rosenthal’s current work focuses on the role of the multipass membrane protein known
as ANKH, which was recently described as a novel mediator of ATP efflux in chondrocytes. She has also recently begun a
project to explore the role of osteoprotegerin mutations in CPPD which involves studies of osteoclastogenesis and bone
metabolism. Current local collaborators at MCW include James Ninomiya, M.D. and Brian Volkmann, Ph.D. Dr. Rosenthal is a
standing member of the Skeletal Biology Development and Disease study section at NIH, and a mentor for the US/Canada
Bone and Joint Initiative Young Investigators Workshop. Additionally, she has published work on musculoskeletal
complications of diabetes, osteoarthritis, and gout. She was the site PI for two clinical trials of cardiovascular risk in gout and
osteoarthritis patients at the Zablocki VAMC, where she is Medical Director of the CTSI-funded VA Translational Research
Unit.
Mary-Ellen Csuka, MD is an expert in scleroderma and participates in many research initiatives with this rare disease at the
national and international level. She has received funding with Dr. Kirkwood Pritchard to study IRE5 in scleroderma patient
samples and currently collaborates with Dr. Polly Ryan on an NIH-funded study of health behaviors in osteoporosis patients.
She has active clinical trials in scleroderma, Raynaud’s and autoimmune overlap syndromes.
David Gazeley, MD is developing a research program related to care models and adherence in high risk SLE patients.

MCW Research Overview
Jump to Table of Contents 235
Neurology
Research to improve health care for neurological illness is a major mission of the Department of Neurology, which maintains a wide
range of basic and clinical research programs. Below is a list of just a few of our programs. More detailed descriptions and links to
lab websites can be found on the Neurology website at http://www.mcw.edu/neurology.htm.
Autonomic Disorders: Directed by Dr. Thomas Chelimsky, research focuses on dysautonomias associated with pain such as
functional abdominal pain, irritable bowel syndrome, interstitial cystitis, postural tachycardia syndrome, fibromyalgia, and cyclic
vomiting syndrome. The aims of current studies are to ascertain the co-morbidities of these disorders, the familial occurrence
patterns, and ultimately understand the genetic, epigenetic and environmental changes that influence their emergence across
individuals.
Language Imaging Laboratory: Directed by Jeffrey Binder, this lab conducts basic research on normal and impaired language
functions using functional (fMRI) and structural MRI, event-related potentials (ERP), magnetoencephalography (MEG), transcranial
direct current (tDCS) and magnetic stimulation (TMS). Research focuses on quantitatively characterizing the structural and
functional connections among brain regions in epileptic networks, language mapping prior to brain surgery, and on understanding
and treating aphasia after stroke. Lab members have had continuous funding from the NIH since 1994 and have produced
pioneering studies on the neurobiological basis of language.
Magnetoencephalography (MEG) laboratory: Both clinical and basic neuroscience research are conducted in the Froedtert MEG
laboratory. Clinical research is directed toward developing and refining MEG methodologies for localizing regions of electrical
dysfunction in epilepsy and mapping cortical functions.
Memory Disorders: Established by Dr. Piero Antuono in 1985, the Dementia Research Center employs fMRI techniques to develop
noninvasive early diagnostic tools for predicting the risk of Alzheimer's disease and Mild Cognitive Impairment. Multiple clinical
trials test the effectiveness of promising new therapeutics such as tDCS and drugs for the treatment of MCI and early AD as well as
the prevention of AD in people with normal cognition but who are at high risk of developing the disease.
Multiple Sclerosis Translational Program: Dr. Staley Brod is researching optimal levels of oral ACTH (a natural endogenous protein
showing intrinsic immunomodulation) which could be used as a disease modifying treatment for MS. He also conducts imaging
work aimed at discovering a causal nexus between pro-myelinative proteins in the CSF and blood with decreasing brain
activity as characterized by 7T MRI. The discovery of such proteins could provide future targets for CNS repair. There are also
two clinical trials studying a monoclonal antibody that could stimulate neuronal regeneration.
Whelan Lab: Dr. Harry Whelan has been inducted into the NASA Space Technology Hall of Fame for his research on the use of near-
infrared (NIR) LEDs for wound healing and the treatment of brain tumors and neurofibromatosis. The goal of his research program
is the translational application of infra-red light technology to medicine. His work addresses cell culture, basic biochemistry, animal
models, and human subjects, with active studies at all three translational levels of research.
Clinical Trial Program: Multiple subspecialties are evaluating the safety and efficacy of commercial products. The Amyotrophic
Lateral Sclerosis Team is evaluating three compounds thought to have positive effect on breathing function. In Pediatric Muscular
Dystrophy, several studies for Duchenne’s are underway, including a new cellular therapy trial. Headache Medicine is testing two
compounds for episodic and chronic migraine, and a device for migraine prevention. The Parkinson’s Team is testing a drug for
symptoms such as tremor, stiffness and slowness, and has an immune therapy study that targets cellular pathology. The Stroke
Team has joined the NIH StrokeNet Consortium with two studies pending: a secondary prevention study in patients with
cryptogenic stroke who have evidence of atrial cardiopathy, and a sleep study for stroke management and recovery.

MCW Research Overview
Jump to Table of Contents 236
Obstetrics & Gynecology
The Department of Obstetrics and Gynecology (OB/GYN) is dedicated to improving women’s health care through our
Women's Health Research Program (WHRP). Using WHRP as a vehicle of research, we have leveraged the expertise of MCW
physicians and scientists, hospital partners, and affiliated organizations, to accomplish defined objectives in the field of
gynecology oncology (GYN/ONC) and maternal fetal medicine (MFM). The research continues to grow strongly, and efforts
to further support and serve the research needs of our faculty, fellows, residents and students. This includes monthly WHRP
seminar series given by both internal and external speakers covering wide range of topics in women’s health and twice
monthly department meetings on work in progress.
Notable accomplishments include:
• Dr. Janet Rader, Professor and Chair of OBGYN along with Dr. Kristina Kaljo, assistant professor of OBGYN received
an extramural $943,311 grant award for 5 years from NIH (R25) to conduct their project titled “Student-Centered
Pipeline to Advance Research in Cancer Careers (SPARCC) for Underrepresented Minority Students”. The first class
of SPARCC students graduated on Aug 9
th
.
• Dr. Pradeep Chaluvally- Raghavan received a an R01 titled “Role of RNA activation in Tumor Progression and
Metastasis” to start in August 2019 This was also supported by earlier internal MCWACS Pilot Research grant.
“RNA activation driven ovarian cancer”
• Dr. Allison Linton received $450,00 grant award for 2 years from the AHW- Healthier Wisconsin for project titled,
“Lower Uninsured, STI, & Unintended Pregnancy by Integrating Services at Milwaukee Co. Health Depts.”
• Anna Palatnik, MD received a$75,000 grant award for one year from AMAG Pharmaceuticals for research
“Involvement of micro- RNA 223 in the pathogenesis of preeclampsia through interference with epithelial-
mesenchymal transition of the extravillous trophoblast”
• Gynecological Oncology Fellowship program was approved and fellows will start summer 2020.
Other key programmatic initiatives include:
• WHRP SEMINAR SERIES: This seminar series is held the third Wednesday at noon in the OBGYN conference room.
Speakers from both within and outside the institution are invited, and often new collaborations, and initiatives
emerge from these interactions.
• CLINICAL TRIALS: Overall, we have strong growth in clinical trials. Dr. Denise Uyar’s investigator initiated multi-site
trial for immunotherapy of primary ovarian cancer is actively recruiting and close to accrual. Dr. William Bradley’s
investigator initiated multi-site trial Combining Bevacizumab, Atezolizumab and Rucaparib for the Treatment of
Previously Treated Recurrent and Progressive Endometrial Carcinoma was activated in July. We opened several
phase I trials enabling cancer patients to receive novel drugs and early access to biologic agents. Maternal Fetal
Medicine physicians joined one of the largest NIH consortiums, the MFMU. Also opened studies on fetal therapy
and management of hypertension in pregnancy.
• RESEARCH IN PROGRESS MEETINGS: OB/GYN clinical and research faculty and staff meet twice a month to discuss
work in progress and to critique pre-publication submissions. This interactive format has resulted in progress of
research projects, and general awareness of lab methodology and expertise of members in OB/GYN department.
Lab protocols, unpublished data and research in progress are shared at these meetings. Occasionally, speakers
from other departments at MCW are invited to help with specific methodologies or relay new state-of-the-art
methods to the group.
• MFM/PREECLAMPSIA RESEARCH MEETINGS: Dr. Nicole Lohr, Department of Medicine and Dr. Jennifer McIntosh,
OBGYN faculty member are directing a monthly group meeting that is open to members interested in
placenta/preeclampsia research. This meeting brings together clinicians from obstetrics and gynecology,
cardiology, medicine and pediatrics with basic scientist studying fields related to preeclampsia. The group share
ongoing research, discuss emerging topics, review grant proposals and develop inter-departmental collarboration.

MCW Research Overview
Jump to Table of Contents 237
• PUBLICATIONS: Highlight publication - Dr. William Bradley, associate professor is one of the highest enroller in the
country for Solo 1 trail and an author in New England Journal of medicine titled “Maintenance Olaparib in Patients
with Newly Diagnosed Advanced Ovarian Cancer” N Engl J Med. 2018 Dec 27;379(26):2495-2505.
Where are we heading?
Faculty recruitments in placental angiogenesis is ongoing, and this is a joint recruitment effort with MCW Cardiovascular
Center. A joint GYN/ONC Cancer recruitment effort with MCW Cancer Center is also ongoing. Please visit our website at
http://obgyn.mcw.edu/research.
Interested faculty should contact us for mentoring and collaboration opportunities with fellows, students and physician
scientists in the department.

MCW Research Overview
Jump to Table of Contents 238
Ophthalmology & Visual Sciences
A broad spectrum of funding sources, from individual donations to National Institutes of Health grants, enables our
researchers to take a multidisciplinary approach to improving the fundamental understanding, diagnosis and management
of eye diseases. As a leader in clinical and translational research, Vision Science Research at MCW supports a solid platform
for innovation, collaboration and discovery.
Below are some highlights of noteworthy grants awarded over the past year:
• NIH-NEI U24 Award- Audacious Goals Initiative. Dr. Joseph Carroll, MCW PI (Dr. Jacque Duncan of UCSF other project
PI), assembled a team of investigators across four subcontracting sites for this project, which is titled: “Developing
Cone-Dominant Retinal Disease Models as a Resource for Translational Vision Research”
• NIH-NEI R01 Award-Research Project Grant. Dr. Daniel Lipinski was successful in attaining his first R01 award, which
is titled “Vascular Gene Delivery and Early Disease Biomarkers in Diabetic Retinopathy”
• NIH-NEI- R01 Award-Research Project Grant (Multi-PI). Dr. Joseph Besharse, in collaboration with fellow PI Dr. Brian
Link of the Cell Biology department, was successful in attaining an R01 award, which is titled “RPE Signaling in Ocular
Health and Disease”. Dr. Ross Collery, another research faculty department member, is also a contributor on this
award.
• NIH-NEI- R01 Award-Research Project Grant. Dr. Iris Kassem will receive her first R01 award, which is titled “Diagnosis
and Predictive Value of the Ocular Manifestations of Fabry Disease”
• Foundation Fighting Blindness-Individual Investigator Award. Dr. Daniel Lipinski was successful in attaining an award,
which is titled “Maintaining Proteostasis to Prevent Cone Photoreceptor Degeneration in Retinal Disease”
Regarding the department’s robust Clinical and Translational Research division, during the 2018-2019 academic year, the
department participated in 56 clinical and translational research studies, including 19 clinical trials with a mix of industry and
NIH funding. The Eye Institute was one of only eight US sites to participate in a significant phase III trial for active thyroid eye
disease, which showed a dramatic reduction in proptosis and a substantial improvement in overall response rate in patients
treated with teprotumumab compared with placebo. The Eye Institute also led the way in a single-center controlled pilot
study testing the safety and efficacy of subthreshold photothermal therapy in patients with macular telangiectasia type 2,
which has now reached its recruitment midpoint. In addition to our own research, the department provided ophthalmology
support for 27 clinical trials from other groups across the Froedtert Hospital campus, including the Cancer Center, Pulmonary
Medicine, Obstetrics and Gynecology, Nephrology, and Pediatrics.
Advanced Ocular Imaging Program
The Advanced Ocular Imaging Program (AOIP) was created in 2009 to promote the development and use of translational
ocular imaging tools to improve detection, diagnosis, and management of eye disease. The founding directors were Joseph
Carroll, PhD and Dennis Han, MD, and their initial focus was to create a culture of collaboration between our research faculty
and physicians. What emerged was a truly unique infrastructure, where the common language was imaging. Expanding the
arsenal of imaging equipment in the clinic, bringing the latest ocular imaging technology into the research labs, and
establishing processes through which these resources could be shared were some of the biggest investments early on.
The Department of Ophthalmology & Visual Sciences has made major investments to renovate the laboratory space on the
8th floor of the Eye Institute to house the AOIP. A dedicated waiting area for patients and their families, space for multiple
adaptive optics imaging systems, numerous image processing workstations, dedicated rooms for additional clinical imaging
equipment and eye exams, and a separate research and development lab comprise the AOIP facilities. In addition, there

MCW Research Overview
Jump to Table of Contents 239
continues to be investment in the most valuable resource of the AOIP – people. The AOIP currently consists of over 40 faculty,
staff, and students. Our program members include vision scientists, clinicians, and engineers at the Medical College of
Wisconsin.
While the AOIP provides a solid platform for innovation, collaboration and discovery in ocular imaging, there remains the
commitment to grow and expand. From image interpretation and analysis services, to offering hands-on training on new
imaging technology or simply individual consultation on challenging clinical cases, we will accommodate the expanding needs
of vision scientists and clinicians in an effort to advance knowledge and improve vision through advanced imaging.
Ocular Gene Therapy Lab
Founded in 2016 by Daniel M. Lipinski, DPhil, the Ocular Gene Therapy Laboratory (OGTL) aims to develop broadly applicable
gene-based therapeutics to prevent human blindness arising from neurodegenerative or vascular diseases affecting the
retina. Consisting of faculty, students and staff from a diverse range of academic backgrounds, the OGTL laboratory takes a
highly multidisciplinary and collaborative approach toward research, working with basic science and clinical investigators
worldwide to identify novel therapies for currently untreatable conditions that result in vision loss in humans, including
diabetic retinopathy, age-related macular degeneration and glaucoma.

MCW Research Overview
Jump to Table of Contents 240
Orthopaedic Surgery
Biomaterials and Histopathology Laboratory
The Biomaterials Lab has done its most significant work in the study of calcium phosphate materials. In conjunction with the
Medical College of Wisconsin’s Animal Research Center and Clement J. Zablocki VA Medical Center, the lab studies new
implant materials compatibility. The lab also collaborates with Marquette University’s Biomaterials program.
• Equipment: To evaluate implants and implant materials, the biomaterials and histopathology lab is equipped with
embedding stations, a rotary microtome, a Jung microtome and diamond saws, a tissue pathology laboratory, and
a darkroom equipped for microradiography and autoradiography. Histomorphology and microdensitometry of
bone also are performed.
• Personnel: The OREC Biomaterials Research Laboratory is directed by Jeffrey Toth, BSE, PhD, FAIMBE. Dr. Toth’s
research expertise includes: Bone histology and histomorphometry, Bone Grafts and bone graft substitutes,
Fabrication, characterization, and evaluation of biomaterials, Characterization and pre-clinical testing of
orthopaedic biomaterials, and Mechanisms and clinical uses for osteoinductive substances and materials.
• Research laboratory is staffed by Sara Landschoot, HTL. Sara is a registered histotechnologist. She is HTL certified
by The American Society of Clinical Pathologists. Sara has experience in histologic techniques, including: routine
and special staining; enzyme histochemistry; immunohistochemistry; electron microscopy; molecular pathology;
cytogenetics; Mohs; cytology; grossing; and photography.
Biomechanical Laboratory
The Biomechanics Laboratory conducts a wide range of basic science and applied research projects in orthopaedic
biomechanics. Research methods often encompass in-vitro experiments with human or animal specimens and the use of
computer modeling and analysis.
• Space: The Orthopaedic Biomechanics Lab is designed and maintained to support basic science and applied
research projects in orthopaedic biomechanics. Research methods often encompass in-vitro experiments with
human or animal cadaveric specimens and the use of computer modeling and analysis.
• Equipment
o MTS 809 servo hydraulic axial-torsion material testing system with a pair of hydraulic grips, 8 additional
analogue data collection channels, and FlexTest 40 controller;
o Optotrak Certus Motion Analysis System with 8 additional analogue data collection channels;
o customized load frame for testing with static loads;
o an equine portable radiograph unit;
o Tekscan K-Scan joint pressure measurement system with software and five sensors;
o AMTI six-axis load-cell and signal amplifier and other uni-axial load cells;
o Microstrain 3mm micro-miniature DVRTs,
o various LVDTs displacement transducers;
o miniature pressure transducers,
o assorted power and manual tools and surgical instruments.
• Personnel: The laboratory is staffed with a full-time engineer who holds a degree in Electrical Engineering and
Computer Science and twenty years of experience of working in the lab.
• Funding: The laboratory is supported by the general operating funds of the Department of Orthopaedic Surgery
and grants.
• Current research topics include
o Studies of the stability of total-joint replacement
o Acetabular cup and hip stem micromotion
o Joint mechanics
o Biomechanical analysis of subtalar motion

MCW Research Overview
Jump to Table of Contents 241
o Spine mechanics
o Experimental and computational evaluation of spinal instrumentation
o Bracing in scoliosis and spine fractures
o Planned projects include:
o Three-dimensional finite element modeling of the pelvis
o Strain measurement in the pelvis and ankle ligaments
o A study of femoral neck fractures
Cell Biology Laboratory
The Cell Biology Laboratory investigates the interactions between bone cells and orthopaedic implants. Research activities
include studies into the role of orthopaedic wear debris in the generation of cytokines by cultured osteoblasts, as well as
alterations in bone-associated proteins in response to orthopaedic implant materials. The cell biology laboratory in the
Department of Orthopaedic Surgery provides a unique environment for collaboration between basic scientists and
orthopaedic surgeons.
• cell2Equipment: Tissue culture equipment including incubator, hood, liquid nitrogen tank, centrifuges, water baths
and refrigerators are available as well as gel electrophoresis equipment and software for quantitation,
thermocyclers for reverse transcription and the polymerase chain reaction (RT-PCR), and an ELISA plate reader.
Shared equipment includes ultracold refrigerators, ultracentrifuges, fluorescence spectroscopy, UV-visible
spectroscopy, confocal microscopy and animal surgical facilities.
• Personnel: Dr. James Ninomiya (Lab Director) and Janine Struve (Research Associate) support residents and
students in the laboratory.
Musculoskeletal Functional Assessment Center: Pediatric Orthopaedic Research Lab
The Musculoskeletal Functional Assessment Center supports basic science and clinically related studies involving orthopaedic
conditions, focusing primarily on pediatric spinal deformities. The center is involved in research to better understand the
etiology and effects of pediatric spinal deformities, to analyze and monitor spinal deformities progress using 3D surface
topography and the EOS system, to design and evaluate new spinal implants in animals and in patients, and is collaborating
with researchers in genetics to study children with scoliosis. The center provides research opportunities for medical students,
biomedical engineering students, residents, and physicians. The center advances clinical transitional research that directly
benefits children with orthopaedic deformities.
• Space: The Musculoskeletal Functional Assessment Center: Pediatric Orthopaedic Research Lab is located in the
Pediatric Orthopaedic Clinic at the Children’s Hospital of Wisconsin.
• Equipment: Recently the Milwaukee Spinal Scanner System has replaced the Quantec system for measuring spinal
curvature. The Milwaukee Spinal Scanner System includes a hand held laser scanner, custom spinal curvature
measurement software, a standing patient stabilizing apparatus, and a limb stabilization apparatus. The EOS 3D X-
ray Orthopedic Imaging System that allows low radiation 3D spinal X-rays while the patient is standing.
• Personnel: The laboratory is supported and run by Dr. Xue-Cheng Liu (Lab Director) & Carlos Marquez-Barrientos
MS (Research Associate).
Center for Motion Analysis
The Center for Motion Analysis (CMA) is designed to support a broad scope of both clinical and research oriented projects.
Clinically, the center can provide gait analyses for both pediatric and adult patients, which enhance diagnoses and improve
functional outcomes for neuromuscular and orthopaedic impairments as well as dysfunction caused by other deformities.
Motion abnormalities include complex alterations imposed by the musculoskeletal and neuromuscular systems, as well as
secondary adaptations that the patient makes in order to function. Identification of these patterns is extremely difficult, even
for the trained clinician.
Quantitative motion assessment includes specialty models for the distal extremities (foot and ankle, upper extremity, hand
and wrist, trunk) sports applications and higher speed analysis capability, and rehabilitation (assistive devices, prosthetics

MCW Research Overview
Jump to Table of Contents 242
and orthotics.) Educational support through clinical training and research project participation is provided for research
fellows, orthopaedic residents, medical students and engineering students. Numerous technical development projects are
supported through close collaboration with the Department of Biomedical Engineering at Marquette University. The center
also collaborates with Children’s Hospital of Wisconsin, Froedtert Hospital, and other institutions (MSOE, UWM and CUW).
Research applications include studies of surgical interventions, orthotic and prosthetic treatments, and therapy upon upper
and lower extremity motion and control.
Motion analysis provides a frame-by-frame analysis of the three-dimensional joint motion, limb kinematics, kinetics, and
muscular activity. While changes from activity patterns of age-matched normals are used to formulate a clinical treatment
plan, research studies of pathological motion and muscular control patterns are designed to increase our understanding and
ultimately our ability to improve future diagnosis, treatment and injury prevention.
• Space: The CMA facilities provide a 2,325 sq. ft. test area, examination/preparation area, offices, and storage at the
Children’s Hospital of Wisconsin Greenway Clinic. A 30 ft. walkway is included in the test area for collection of
ambulatory data. A 1,071 sq. ft. area is located adjacent to the testing area for support personnel and includes an
examination room, equipment storage room and test bench, two offices and a working community area for research
fellows and students.
• Equipment: includes twelve T40 Vicon MX cameras for motion capture, two AMTI 6 D.O.F force plates, two Bertec 6
D.O.F force plates,1 Novel EMED pressure platform, 1 Novel PEDAR insole pressure measurement system, F-Scan
foot insole pressure measurement system, 16 channel Delsys Trigno wireless EMG system (surface and fine wire), 8
channel Noraxon surface and fine wire EMG system, Biodex extremity evaluation system, Vicon Nexus software for
data collection and processing, Vicon Polygon software for constructing reports, Vicon Body Builder software for
model construction, EMG analysis software for Delsys and Noraxon, FANDACAL – Foot and ankle motion analysis
software, Walker Assisted Gait (WAG) torso and upper extremity motion analysis software, and Matlab software.
• Personnel: Educational support through clinical training and research project participation is provided by Dr. Roger
Lyon (Medical Director), Dr. Xue-Cheng Liu (Co-Director), Dr. Gerald Harris (Co-Director), Jessica Fritz, PhD, (Research
Assistant Professor) and Amie Chapoupka B.S. (Biomedical Engineer).
Sports Medicine Motion Analysis Laboratory
The Sports Medicine Motion Analysis Laboratory is used for developing, validating, and advancing injury prevention and
performance enhancement in athletes. This facility is designed to be able to stimulate real-life sports environments such as
a pitcher’s mound, golfing tee box, or batting cage so that we can study the motion of the athlete’s body and the forces acting
at their joints. By understanding these motions and loads, we can learn to identify athletes at a greater likelihood of injury
and measures of performance. The goal is to discover the mechanisms behind injury, rehabilitation, and performance, and
apply them to improve the outcomes and optimize performance for the athletes that come through our lab, and to advance
sports medicine research as a whole.
• Space: The 1600 square-foot Sports Medicine Motion Analysis Laboratory is located within the Froedtert and Medical
College Sports Medicine Center.
• Equipment in the laboratory includes a Motion Analysis system with 8 Raptor cameras, 2 PointGrey high speed video
cameras, 2 AMTI force plates, F-Scan foot insole pressure measurement system, EMG system, Biodex extremity
evaluation system, Motion Analysis software for data collection and processing, and Matlab software.
• Personnel: William Raasch MD (Medical Director) & Janelle Cross PhD (Research Director).
• Areas of Research
o Baseball pitching analysis
o ACL injury studies
o Biomechanics of landing/cutting/planting techniques among soccer, basketball, and volleyball athletes
o Biomechanics of a batter’s swing, golf swing, tennis serve, volleyball spike, speed skaters and ballet dance
o Biomechanics of running

MCW Research Overview
Jump to Table of Contents 243
Otolaryngology and Communication Sciences
The Department of Otolaryngology and Communication Sciences has a robust and diverse research program. Many aspects
of Ear, Nose, Throat and Communication Disorders in adults and children are being investigated. Research programs
encompass basic science bench investigations, translational studies, and clinical trials. Funding sources include the NIH, public
and private organizations and foundations, and corporate grant sponsorship.
Otology: Many disorders related to hearing and balance, as well as pathologic diseases of the ear, are under study. Basic
science studies in the laboratory include investigations into the molecular mechanisms underlying otitis media, the
pathogenesis of biofilms in the ear, and genetic diversity related to otitis media. Additional studies have identified a novel
gene related to hearing loss and ongoing studies are characterizing this unique genetic locus. Clinical studies include
investigations into cochlear implant performance and programming, auditory neuropathy spectrum disorder, cholesteatoma,
and cardiovascular disease associations with hearing loss. Quality improvement studies include developing diagnostic
protocols for vestibular disorders.
Laryngology: Basic science and clinical studies into disorders of, and affecting, the upper aerodigestive tract are a strong
component of our research program. Basic science studies are examining the role of pepsin and laryngopharyngeal reflux in
laryngeal injury and carcinogenesis. Clinical and translational studies are examining voice disorders, airway stenosis,
extraesophageal reflux, dysphagia and related disorders, neurolaryngology, vocal fold paralysis, obstructive sleep disorders,
outcomes with tonsillectomy, and modeling of the upper airway. These studies are being pursued in both adult and pediatric
populations.
Rhinology: A major focus of research is modeling nasal air flow in the normal and pathologic conditions using computational
fluid dynamics. These methods are also being extended to other regions of the upper airway. Additional clinical studies
include the use of medication impregnated stents in managing rhinologic disease, the use of steroids in nasal inflammatory
disease, chronic rhinosinusitis in children, and outcomes of nasal obstruction surgery.
Head and Neck: Many studies focus on cancer and on other soft-tissue anomalies in the head and neck. Clinical studies include
head and neck oncologic and reconstructive outcomes, outcomes with minimally invasive head and neck surgery, treatment
of salivary dysfunction and disease, cancer survivorship and quality of life issues, late effects of cancer treatment, and a
number of other outcome and quality studies in pediatric or adult populations.
Quality: The Department of Otolaryngology and Communication Sciences has a strong commitment to quality outcomes.
Many processes in all aspects of ear, nose and throat conditions are in effect to measure quality improvement initiatives.
These range from patient outcomes, to operating room efficiency, to communication strategies, to use of the EMR, to
effective instruction and teaching.
Education: The Department of Otolaryngology and Communication Sciences also has a strong commitment to education. The
Department is a leader in studying the efficacy of objective surgical assessment tools (OSATs) to measure resident progress
in acquiring technical surgical skills.
For information on Department of Otolaryngology and Communication Sciences research, for student opportunities to
participate in research training, and for collaborators wishing to discuss opportunities, please contact:
David R. Friedland MD, PhD
Chief, Division of Research

MCW Research Overview
Jump to Table of Contents 244
Pathology
Mission: The Medical College of Wisconsin Department of Pathology is dedicated to delivering state of the art, subspecialty
laboratory diagnostics to our patients; providing comprehensive and practical pathology training; building a strong
foundation for our medical students; advancing medical knowledge regarding the understanding, diagnosis, and treatment
of human disease through advanced research; serving our community; and developing leaders.
Vision: A nationally recognized pathology department, leading the pursuit of cutting edge diagnostics, education, research,
and community outreach.
Core Values
• Commitment to Excellence: We aim for excellence through a high-performance culture and self-motivation.
• Continuous Improvement: We strive to improve constantly based on evidence and data.
• Diversity: We are stronger because of the diversity in our department, both in us as individuals, and in the broad
scope of work that we do.
Professionalism: We are respectful and considerate in all of our interactions. We hold honesty, integrity, and trust as pillars
of everything we do.
Citizenship: We are all engaged in the pursuit of common goals, working as a collegial team in the fulfillment of the missions
of our department and institutions.
As the provider of diagnostic services in anatomic (tissue) pathology and laboratory medicine, the department plays a critical
support role for the entire medical center and its community of patients, physicians, paramedical personnel and researchers.
Without the provision of high quality diagnostic services in surgical pathology and clinical laboratories, physicians and nurses
in our system would not be able to properly evaluate patients admitted to the hospital or in the outpatient setting, perform
surgery, or treat cancer and other patients.
In addition to patient care activities, pathologists are also critical in the education of the next generation of physicians and
allied professionals. The pathology course for the medical students at the Medical College of Wisconsin provides the
foundation for the understanding of mechanisms of disease, pathogenesis and the cellular substrate of human diseases. As
such, our discipline serves as a bridge between the basic sciences and clinical medicine. In addition, we also educate our
fellow physicians regarding mechanisms of disease and the biologic behavior of the various diseases we routinely examine
and, as such, contribute to the continuing medical education of our peers.
Finally, pathologists play a critical role in biomedical research. In addition to constantly improving diagnostic methods,
developing new criteria for a more accurate and simplified diagnosis, and redefining our understanding of disease processes,
pathologists are uniquely positioned to apply many of the emerging modern biomedical techniques to the study of human
disease. Because pathologists are custodians of the tissue samples obtained from patients admitted to our system, we are
ideally positioned to carry out research that utilizes those tissues to advance our understanding of disease. In fact, because
the natural setting for a pathologist is the laboratory where the diagnostic tests are normally carried out, laboratory research
is merely a natural extension of our job.
In recent years biomedical research has tremendously expanded our understanding of the molecular and genetic mechanisms
of disease. Modern science has exponentially advanced in terms of its ability to perform assay for molecular and genetic
abnormalities that underlie most human disorders. Newer techniques such as DNA in-situ hybridization, polymerase chain
reaction, fluorescence in-situ hybridization and molecular profiling have revolutionized the field of medical research.

MCW Research Overview
Jump to Table of Contents 245
Pathologists are uniquely positioned to apply these techniques for the study of human tissues and, as such, to translate the
knowledge gained from basic science to the bedside. As such, pathologists are the original and quintessential “translational
researchers”.
Funded Research
A variety of funded research activities are carried out by the Department of Pathology at the Medical College of Wisconsin,
including research that is funded by Government Agencies (NIH, DOD, and others), Advancing a Healthier Wisconsin (AHW)
endowment, and various other private and commercial sources. The department also actively collaborates with several of
the other departments on campus and with outside institutions in funded research. Funded research is also supported by the
department through the activities of our MCW Tissue bank, which is housed and operated by the Department of Pathology.
For more information, please visit our webpage: http://pathology.mcw.edu/

MCW Research Overview
Jump to Table of Contents 246
Pediatrics
We support a diverse research agenda in the Department of Pediatrics (DOP) that is translational in nature and achieves focus
through alignment with the priorities of our academic and hospital partners. Our goal is to improve the health of the children,
both in our region and beyond. Toward that end, we incentivize collaboration across divisions to leverage Departmental
strengths, we support a grants development team and other widely used shared services, and we provide strong mentorship
for new investigators. This strategy has resulted in over 47 million dollars in new awards in the past 27 months.
Research in cardiovascular development is one of our key focus areas. Indeed, congenital heart defects are the most common
type of birth defects, affecting nearly 1% - or about 40,000 – births per year in the United States. Our Herma Heart Institute
(HHI) at Children’s Hospital is one of the nation's top programs for medical and surgical treatment of congenital heart defects
and heart disease in children. Founded in the early 1970s, The HHI team performs more than 13,000 diagnostic, therapeutic
and surgical procedures annually and supports outreach programs in six additional locations outside southeast Wisconsin.
Dr. Joy Lincoln joined our team in July 2019. She holds the Sommerhauser Chair for Cardiac Quality, Outcomes and Research
and is the new HHI Research Director. Her work is focused on aortic valve development and calcific disease. Dr. Janette
Strasburger recently received a new R01 to study cardiac development and conditions that result in fetal demise using fetal
magnetocardiography. Dr. Uli Broeckel, another NIH-funded senior member of our cardiovascular research team uses IPSC-
derived cardiomyocytes to study the mechanisms involved in left ventricle hypertrophy and the response of cardiomyocytes
to different medications. Dr. Ramani Ramchandran uses mouse and zebrafish models to study the biology of endothelial cells
and the role of cilia in vascular development. He brought the 2019 Vasculata Conference here to MCW, which educated
trainees and highlighted some of the amazing research done on campus. Dr. Peter Frommelt directs the Echocardiographic
Research Core Lab at CHW. He works closely with the national Pediatric Heart Network in ground-breaking clinical trials
assessing children with Hypoplastic Left Heart Syndrome and the development of new innovative tools for use in the
echocardiographic assessment of children with heart disease.
Premature birth is the leading cause of infant death, and the rate continues to rise both statewide and nationally. Increasing
survival and improving the clinical outcomes of infants born prematurely is a primary goal of our neonatology research
program. Dr. Robert Lane, Pediatrician-in-chief and Chairman of Pediatrics, studies how adverse perinatal environments can
lead to epigenetic modifications that increase susceptibility to certain diseases. Dr. Ganesh Konduri, Section Chief of
Neonatology, recently received 2 R01 grants to study pulmonary angiogenesis and the cellular mechanisms driving persistent
pulmonary hypertension. Dr. Ru-Jeng Teng studies hyperoxia-induced pulmonary injury and pharmacologic approaches to
injury prevention that can be safely applied in premature infants. Dr. Adeleye Afolayan works closely with these investigators
and recently received a K08 award to study how phosphorylation of HSP70 regulates superoxide dismutase 2 function and
controls the redox balance in the neonatal lung. Dr. Nghiem-Rao received a K23 award to study parenteral nutrition-
associated liver disease in infants and Dr. Joanne Lagatta, another recent K23 recipient, is focused on outcomes research for
infants with bronchopulmonary dysplasia.
As indicated by these and other recent mentored NIH awards, the DOP places great value on career development. The DOP
offers multiple structured opportunities for junior faculty to develop competitive grant proposals. These include a weekly “K
Club” for the review of the Specific Aims page and a 3-day grant writing retreat which is held twice a year. Structured
mentored activities are central to the success of both our junior and senior faculty.

MCW Research Overview
Jump to Table of Contents 247
Physical Medicine and Rehabilitation
The PM&R Research Program has been established to advance the science and the practice of physical medicine and
rehabilitation by conducting research aimed at studying and reducing impairments and functional disabilities due to disease
or traumatic events.
We have several collaborations focused on clinical and translational, and community engaged research. Current research
areas include spinal cord injury, physical activity for individuals with disabilities, stroke rehabilitation, spasticity management,
pain, and prosthetics. Our collaborators include faculty from Neurosurgery and Neurology at Froedtert Hospital/The Medical
College of Wisconsin, Marquette University, UW-Milwaukee, and several community organizations.
Our Residency Program offers a Research Intensive Track with protected research time, funding, and significant mentorship
opportunities. Please visit the Residency Program page for more information on resident research.
Research Administration Committee (PM&R)
The RAC is composed of Department of Physical Medicine and Rehabilitation faculty. The RAC is under the direction of the
Research Director. The department sets an annual budget to support research endeavors of faculty, fellows and residents.
These funds will support pilot research proposals, attendance at national and regional meetings to present results of research
and / or accept awards, and to provide assistance with publication costs.
Orthopedic Rehabilitation & Engineering Center
The center was established in 1999 to facilitate research in support of the endeavors of the faculty, fellows, residents and
graduate students participating in the programs of the MCW Departments of Orthopaedic Surgery and Physical Medicine and
Rehabilitation and of the MU School of Dentistry and the MU Department of Biomedical Engineering. The center brings
together common threads within the disciplines of engineering, biomedical sciences, materials sciences, and clinical dentistry.
The result is a unique environment for interdisciplinary applied research.
Human Motion Analysis Laboratory (Gait Lab)
The Department of Physical Medicine and Rehabilitation has collaborated with the Department of Orthopaedic Medicine and
Marquette University to establish the Gait Lab. An agreement with the Gait Lab allows for the use of the facility without
charge for resident research. Funded research budgets provide for financial support of the gait lab.
Rehabilitation Robotic Research and Design Lab (RRRD)
Established in 2004, the RRRD Lab is dedicated to the design, development and therapeutic use of novel, affordable,
intelligent robotic / mechatronic and domotic assistants. It is affiliated with OREC and the Falk Neurorehabilitation Center at
Marquette University.
The lab is focused on:
• Examining underlying causes of upper limb impairment after neural disease, injury or cerebral accident.
• Discovering effective methods to retrain functional recovery on daily living activities.
• Developing new ways of facilitating independent living in daily living environments.

MCW Research Overview
Jump to Table of Contents 248
Plastic Surgery
The Department of Plastic Surgery is committed to providing innovative basic science and clinical research and service to our
community. The Plastic Surgery Research Laboratory works collaboratively with other Medical College of Wisconsin clinical
and basic science departments as well as other U.S. and international institutions to address issues such as treatment of
vibration injury and nerve transfer. Our commitment to community service is noted in our annual medical mission trip and in
our community education presentations. For more than 25 years, physicians and staff at MCW of plastic surgery have
participated in annual mission trips to South America for the purpose of providing surgical services specialty care and medical
collaboration and education to underserved areas.
Our faculty provide comprehensive and specialty clinical care in reconstructive surgery, breast surgery, cosmetic surgery,
hand and upper extremity surgery, pediatric plastic surgery, craniofacial surgery, and cancer reconstruction.
Our research portfolio includes projects with fellows, residents, medical students, and other collaborating researchers from
numerous renowned institutions.
Studies involving Departmental Faculty in the immediate past and current academic years include the following:
1. Comparison of Outcomes and Cost Effectiveness of Unilateral Mastectomy and Contralateral Prophylactic
Mastectomy with Reconstruction in Multicenter Cohort (Erin Doren, MD).
2. Model and mechanisms of surgical intervention for amputation related chronic pain (Gwendolyn Hoben, MD, PhD)
3. Nerve Regeneration in IL-12 KO Mice (Gwendolyn Hoben, MD, PhD).
4. Brain rewiring mechanism in nerve transfer using vagus nerve graft (Ji Geng Yan, MD)

MCW Research Overview
Jump to Table of Contents 249
Psychiatry and Behavioral Medicine
The Department of Psychiatry and Behavioral Medicine is a dedicated community of compassionate, expert, inspired,
professional clinicians, academicians, staff, and trainees committed to improving the lives of persons affected by psychiatric
diseases, concurrent disorders, behavior-related illnesses, and social-environmental conditions impeding mental health. This
mission is accomplished through the pursuit of six core values: (1) scholarship and research, (2) education, (3) clinical service,
(4) community engagement, (5) bioethical principles, and (6) leadership and administration.
Current contributions by faculty within the Department of Psychiatry and Behavioral Medicine include:
Joseph S. Goveas, M.D., Associate Professor
Depressive symptoms, Family History of AD, and Brain Structure and Function: This project will determine the independent
and additive contributions of elevated depressive symptoms and family history of late-onset Alzheimer’s disease on gray
matter volumes, brain function and white matter microstructure in asymptomatic middle-aged adults.
Multimodal Imaging in Depressed Adults at risk for Alzheimer’s Disease: This study will identify the functional and structural
connectivity correlates in depressed adults at risk for Alzheimer’s disease.
Retinal biomarkers of Alzheimer’s disease: This is a collaborative project between MCW faculty from Departments of
Psychiatry, Neurology and Ophthalmology that utilizes novel retinal imaging techniques to detect retinal phenotypes that
discriminates patients with mild cognitive impairment and Alzheimer’s disease from cognitive healthy volunteers.
Ultra-high-field Structural MRI in Late-Life Depression and Normal Aging: This collaborative project between MCW faculty
from the Departments of Psychiatry, Biophysics and Radiology will utilize ultra-high-field structural brain image datasets
obtained on 7T MRI to characterize the medial temporal lobe subregional volumes, and white matter hyperintensities and
cerebral microbleeds that will differentiate late-life depression from healthy volunteers.
In addition, Dr. Goveas has contributed to multiple peer-reviewed publications, was selected as one of sixteen promising
junior investigators in Alzheimer’s disease research at the Charleston Conference on Alzheimer’s Disease, was named in Best
Doctors in America, is a scholar of the NIMH/Weill Cornell Advanced Research Institute in Geriatric Mental Health, is an
invited reviewer for several journals, and is also the reviewer for the Charleston Conference on Alzheimer’s Disease pilot
grants and Ad Hoc Reviewer for Alzheimer’s Association New and Established Investigator Grants program. He is also a
member of the Annual Meeting Program and Research Committees for the American Association of Geriatric Psychiatry.
Jeffrey A. Kelly, Ph.D., Professor and Director
Center for AIDS Intervention Research (CAIR)
The Center for AIDS Intervention Research (CAIR) in the Department of Psychiatry & Behavioral Medicine was first
established in 1994; Kelly has been the Center’s Director since its inception. CAIR adopted a mission statement that
emphasized interventions as the Center’s thematic focus. Much has changed in the field since that time, and CAIR’s research
has evolved in response to new needs. We are now at the pivotal and transformative point when we can end the country’s
HIV epidemic. We have the tools that are needed to drive down HIV incidence and alleviate the burden of HIV/AIDS. This goal
is achievable but requires a new generation of scientific research that optimizes public health outcomes when providers
implement the most recent HIV prevention advances and when our efforts are focused on cities and populations where HIV
incidence is highest.
CAIR’s research agenda has integrated the advancements made in HIV prevention. Early identification of HIV infection
coupled with immediate initiation and sustained use of antiretroviral therapy (ART) protects the health of persons living with
HIV infection (PLH) and eliminates risk of onward transmission. The past decade also saw the discovery that high-risk but
uninfected persons who use pre-exposure prophylaxis (PrEP) are almost fully protected from contracting HIV infection.

MCW Research Overview
Jump to Table of Contents 250
Improved early HIV diagnosis with immediate treatment (“treatment-as-prevention”), scale up in PrEP use by high-risk
uninfected persons, and responding to HIV outbreaks form the central pillars of the National End the HIV Epidemic (EtHE)
Plan that targets counties and states with high HIV incidence.
CAIR’s research incorporates biomedical, policy, behavioral, social science, and community perspectives needed to
successfully scale up evidence-based interventions used by providers in the field; discovering and rolling out interventions
that address critical gaps in the HIV care and prevention continuum; and reducing the country’s longstanding HIV racial
disparities.
CAIR’s mission is to conceptualize, conduct, and
scientifically evaluate the effectiveness of new
intervention strategies to prevent HIV infection in
populations vulnerable to the disease. CAIR’s research also
develops improved strategies to promote health and
alleviate adverse mental health consequences among
persons living with HIV. CAIR is committed to disseminating
its findings both to the scientific community and to public
health providers so they benefit from Center research.
Our approach to achieving this mission is interdisciplinary,
comprehensive, and multidimensional. The Center brings
together outstanding investigators and draws upon models
from the behavioral and social sciences, medicine, public
health, mathematics, economics, communication, law, and
infectious disease epidemiology to develop innovative HIV
prevention methods.
CAIR is the only NIMH-supported HIV behavioral research Center located between the nation’s east and west coasts. We
are a resource to investigators, institutions, and service providers from across the broad midsection of the country. The
Center is also a scientific field leader at both national and international levels.
Within the framework of its thematic mission on intervention research and emerging from intensive Center-wide priority-
setting, the following specific aims guide CAIR’s research:
(1) To advance the field in the development and evaluation of innovative behavioral, social, and structural interventions to
improve PrEP uptake and to improve early identification of HIV infection, linkage and long-term retention of PLH in care, and
attainment of durable viral suppression through ART adherence;
(2) To move the field forward by establishing the effectiveness of a new generation of multi-level HIV prevention approaches
that combine behavioral, biomedical, social, structural, and systems interventions to achieve the greatest public health
impact in disease reduction;
(3) To use dissemination and implementation science paradigms to quickly move HIV prevention interventions found effective
in the research arena to service providers, policymakers, and the public health and provider sectors through an agenda of
research that identifies ways to optimize scale-up and implementation;
(4) To develop strategies that reduce HIV-related disparities through research that identifies and responds to the needs of
racial and ethnic minority populations with greatest HIV incidence and disease burden;
(5) As the only NIMH AIDS Research Center (ARC) located in the center of the United States, to develop, evaluate, and lead in
the implementation of high-impact HIV prevention and to serve as a resource to health departments, providers, researchers,
and community constituencies in mid-sized and underserved cities across the broad midsection of the country.
CAIR’s Core Structure
Administration Core: Strategic planning, administrative
oversight, integrated decision–making._______________
Developmental Core: Innovative new and pilot project
development, early-stage investigator support, Center
seminars, conferences, and internal peer review._______
Methods Core: Resources for consultation, study design,
methods, management, analysis, and interpretation of
qualitative and quantitative data,____________________
Biobehavioral HIV Prevention Core: Resource expertise
to ensure that studies integrate the most recent scientific
advances in biomedical, behavioral, and social science to
improve HIV health outcomes._____________________
Dissemination and Implementation Science Core (DISC):
Resources for partnership development, and the design,
evaluation, and optimization of field effectiveness in HIV
prevention projects.

MCW Research Overview
Jump to Table of Contents 251
Jennifer M. Knight, M.D., M.S., F.A.L.C.P., Associate Professor
Dr. Jennifer Knight has a research interest in psychoneuroimmunology and cancer, specifically regarding the neuroimmune
mechanisms involved in mediating the relationship between psychosocial factors and hematopoietic stem cell
transplantation outcomes. She works in conjunction with the MCW Clinical Cancer Center and the Center for International
Blood and Marrow Transplant Research (CIBMTR) to investigate these mechanisms in nationally representative populations
of stem cell transplant recipients. With American Cancer Society funding, Dr. Knight and her collaborators Dr. J. Douglas Rizzo
(MCW) and Dr. Steve W. Cole (UCLA) identified that stem cell transplant recipients of low socioeconomic status have altered
gene transcription profiles previously characterized as the conserved transcriptional response to adversity. This shift in gene
expression was also associated with adverse outcomes among transplant recipients. Dr. Knight has received subsequent
Leidos Biomed/NCI funding to conduct a prospective randomized controlled trial of propranolol among autologous transplant
recipients at MCW to alter this adverse gene expression profile. She also collaborates with Drs. Hillard and Drobyski at MCW
investigating the neuropsychiatric effects of inflammation as a function of tocilizumab administration among allogeneic
transplant recipients (Advancing a Healthier Wisconsin funding).
Jeffrey M. Engelmann, Ph.D., Assistant Professor
Dr. Engelmann has a research interest in using neuroscience to better understand behaviors that put individuals at risk for
cancer, with the aim of developing more effective cancer prevention strategies. His research focuses on using functional
magnetic resonance imaging (fMRI) to identify brain systems and processes involved in the development and maintenance
of nicotine dependence, with the long-term goal of translating these laboratory findings into safer, more effective, and more
specific behavioral and pharmacological interventions for tobacco use and abuse.
Dr. Engelmann completed his Ph.D. in cognitive and biological psychology at the University of Minnesota and a postdoctoral
fellowship in addiction neuroscience and cancer prevention at the University of Texas MD Anderson Cancer Center. His
earliest research findings demonstrated that potentiated startle can be used as a measure of negative affect in both nicotine-
dependent rodents and humans, demonstrating its translational potential and promise as a biomarker for negative affect in
preclinical studies of new medications for nicotine dependence. In the human study, he expanded upon the traditional
approach to studying cue reactivity that only compares responses to smoking cues and neutral stimuli to an approach that
compares the relative reactivity to smoking cues and neutral, pleasant, and unpleasant stimuli. With National Cancer Institute
funding, Dr. Engelmann used fMRI to study the neurobiological basis of relative differences in cue reactivity. He found that
brain responses to smoking-related and pleasant cues in the striatum, a brain area involved in reward processing, are
predictive of long-term smoking cessation: smokers with larger responses to pleasant stimuli than smoking-related cues are
more likely to successfully quit than those with larger responses to smoking-related cues than to pleasant stimuli.
Interestingly, smokers in the “lower risk” group (pleasant stimuli > smoking cues) showed equal benefit from varenicline or
bupropion for smoking cessation, but those in the “higher risk” group (smoking cues > pleasant stimuli) were more likely to
benefit from varenicline than bupropion, which suggests that pre-quit assessment of relative cue reactivity might contribute
to the personalization of smoking cessation treatment. With funding from the Greater Milwaukee Foundation, Dr. Engelmann
is extending this finding to a more diverse and representative group of smokers. This new project will also examine how the
use of mentholated tobacco products might contribute to lower smoking cessation rates among African American smokers.
The data from this project will be used to support an R01 application to the National Cancer Institute, the goal of which is to
better understand neurobiological mechanisms that underlie racial disparities in tobacco use behaviors. Dr. Engelmann is also
the recipient of a mentored career development award from the National Institute on Drug Abuse. The goal of this grant is
to investigate the effect of the imminent possibility of smoking on brain responses to smoking-related cues, a condition that
more closely resembles relapse. He is currently analyzing the data from this project.

MCW Research Overview
Jump to Table of Contents 252
Alan Nyitray, Ph.D., Associate Professor of Epidemiology.
Dr. Nyitray’s research has focused on the natural history of anal HPV infection and, most recently, anal cancer screening. The
anal HPV epidemiology research has included studies with gay, bisexual, and other men who have sex with men, heterosexual
couples, and heterosexual men. His current research assesses protocols for anal precancer and cancer screening including
determining compliance with annual HPV DNA self-screening among HIV-positive and HIV-negative gay and bisexual men,
assessment of a methylation biomarker for anal cancer screening, and assessing the sensitivity and specificity of self- and
partner palpation for anal abnormalities. He has published more the 60 peer-reviewed papers on these topics and is funded
by the National Cancer Institute. Prior to his HPV research, Dr. Nyitray delivered HIV prevention in a service capacity for 15
years.

MCW Research Overview
Jump to Table of Contents 253
Radiation Oncology
Cancer Center Clinical Trials
Froedtert & the Medical College of Wisconsin Cancer Center physicians and staff are dedicated to providing their patients
with the most up-to-date cancer treatment options. Radiation Oncology participates in offering eligible patients access to
clinical trials that investigate improved survival and quality of life for patients with cancer. The link to related studies is
provided below.
http://www.froedtert.com/research/clinical-trials/cancer
Cancer Cell Biology Research
Cancer is a leading cause of morbidity and mortality for Wisconsin residents. Cancers that are aggressive and that become
resistant to therapies lead to recurrence, metastasis, and even death. Cancer cell biology research is studying the
manipulation of oncogenes and tumor suppressor genes to enhance the effectiveness of cancer therapy. This knowledge can
be used to identify and create novel therapeutic strategies to reduce the human burden of cancer in Wisconsin and in the
United States.
Radiation Biology Research
Radiation is required in the treatment of approximately 50% of all cancer cases at diagnosis; for 75% of patients at some time
during their disease course. The radiation biology group is developing ways to decrease toxicity associated with therapeutic
uses of radiation in cancer treatment. In addition, they assess the risk of exposure to ionizing and non-ionizing radiation and
study medical countermeasures that mitigate radiation injury from radiation accidents and potentially from acts of terrorism.
Radiation Oncology Medical Physics Research
The Radiation Oncology Medical Physics section works to research and develop the most accurate and efficient manner of
delivering radiation therapy to patients. Some of these innovative developments include adaptive dosimetric planning,
magnetic resonance image (MR)-based planning and other image-guided techniques for delivering a highly conformal
radiation tumor and target dose, while minimizing dose to normal structures. Most recently this team is working to develop
MR image-guided linear accelerator delivery techniques; a breakthrough technology at the cutting edge of modern radiation
therapy.

MCW Research Overview
Jump to Table of Contents 254
Radiology
The MCW Department of Radiology, under the leadership of Dr. Vince Mathews, Chair of Radiology, has continued to
demonstrate the values of innovation and discovery that are hallmarks of Froedtert and the Medical College of Wisconsin.
The scientific accomplishments of both the Radiology department and the Medical College promote a strong relationship
with our community and peers both nationally and internationally.
Over the past year, the Department of Radiology has restructured our research program. Kevin Koch PhD, the current Director
of the Center for Imaging Research, and Sarah White, MD, MS, FSIR have been named Co-Vice Chairs of Radiology Research.
In their roles, Dr. Koch will oversee the basic and translation research laboratories, and Dr. White will focus on Clinical
Research and developing relationships with external collaborators including other departments and industry partners. In
order to expand the research mission, a new infrastructure has been developed. Each section has named a Director of
Research (DoR) to serve as a liaison between research administration and clinicians. Drs. Koch and White will meet with the
DoRs quarterly to provide and receive updates regarding research in each division.
In addition to the DoRs, the Department of Radiology has and continues to grow a robust administrative research
infrastructure to support research. Brad Condon serves as the Research Administrator for Radiology. He manages all the
research staff, including the research coordinators as well as providing financial and compliance oversight and program
budgeting. With 10 years at MCW, Brad has the institutional savvy to help facilitate research endeavors on this campus. Jodi
Nicolai-Johnson is the Radiology Program Manager and is an expert in grant submission and post grant award follow-up. After
the grant is awarded, Jodi will track the budget and time lines for the follow-up of deliverables. Jodi has been with Radiology
for almost 5 years and brings a perspective of a scientist and former lab manager to her role. Due to the large volume of
research currently being performed, Melissa Hollister and Christi Reichert were recently hired as Clinical Research
Coordinators. In their roles they will help navigate the regulatory processes necessary to conduct research and recruit and
consent patients. Melissa and Christi were previously radiology technologists and their knowledge of radiology provides for
an extremely efficient work flow. Elizabeth Weil continues to serve as Research Coordinator for Vascular & Interventional
Radiology (VIR), navigating the regulatory processes for all VIR research including chart reviews to multi-center international
randomized trials. This year Elizabeth began a new role as Research Ambassador through MCW’s Office of Research new
Research Ambassador Program. Elizabeth and Dr. Sarah White will also serve as committee members on MCW’s Office of
Research Committee on Regulatory Burden which will work to reduce administrative burdens associated with regulatory
compliance. Lastly, Diana Kane serves as Radiology’s Database Administrator. Diana has made manual chart reviews a thing
of the past. If given data elements, Diana has the IT knowledge necessary to build databases and populate the databases with
the necessary data elements. This allows the extraordinarily laborious chart review to be fast and allows the researcher to
focus on data analysis.
Together Drs. Koch and White have obtained MCW IRB approval for an umbrella protocol that can be used by all radiology
faculty. This radiology umbrella protocol was modeled after the VIR umbrella protocol which has been in use for 2 years. The
radiology umbrella protocol allows research of all imaging studies and their comparators to be reviewed. In addition, Dr.
Andrew Nencka is the PI of an umbrella MRI protocol that allows for clinical and research technology investigations. This
protocol can be used for investigations of new sequences and processing applications on consenting volunteers and clinical
subjects.
The benefits of an increased and strengthened research support staff are already apparent with many process innovations
and new opportunities. Dr. Koch was awarded a DOD (Department of Defense) Grant for Quantitative MRI of the Post-Injury
Instrumented Spinal Cord, beginning soon. Dr. Peter LaViolette received a supplement to his NIH Brain Cancer MRI R01 to
study Alzheimer’s Disease. Dr. Yang Wang Received a Multi-PI R01 with Dr. Michael McCrea for Effects of Head Impact
Exposure During Contact Sport on Middle School and High School Athletes.
The overall research activity within the Department of Radiology continues to grow. Within the past year, the Department
has submitted approximately 44 grant applications, and has collaborate on over 38 other grant applications. Current fiscal
year research revenue includes $880K NIH funding, we also have several multi-PI Federal Grants submitted with other
institutions.

MCW Research Overview
Jump to Table of Contents 255
Other Extramural revenue stayed strong at $446K, but was less than prior years due to timing of milestones and extension of
several projects. Several multi-year projects are ongoing with GE Healthcare, Novocure, Guerbet, and the Focused Ultrasound
Foundation. Sponsors with recognizable names such as Radiological Society of North America, Siemens, CR BARD, Cook
Medical, Penumbra, DFINE, W.L. Gore and Associates, Medtronic, InSightec, Instylla, BTG, The Froedtert Hospital Foundation,
Myocardial Solutions, and PRISM, have new and ongoing collaborations with the Department of Radiology.
We continue to receive awards on campus from the Cancer Center, CTSI, and the Center for Imaging Research (CIR) Pilot
grants. The Department is also continuing Investigator Initiated Studies, to further the partnership with Industry.
Taken together these many initiatives and successes being in Radiology Research should enable both physician and PhD
researchers to provide even more benefit to the community in a more timely and efficient manner.
For the 2018-2019 academic year, the MCW Division of VIR continued to expand its clinical and translational research
activities. Dr. White’s translational Interventional Oncology (IO) lab published 3 papers (and 2 in progress), 7 abstracts, 6
ongoing grants, awards from JVIR and SIO and 3 invited lectures. The Division opened 2 new clinical trial and continued
research activities in 7 ongoing clinical trials. Their research endeavors have resulted in 1 publication, 3 grants, 10 abstracts
and 8 poster presentations at national and international meetings. Herein we will highlight some of the pivotal trials our
faculty have been involved with over the past year:
• Vice-chair, Clinical Operations-Image Guided Procedures, William S. Rilling, MD, FSIR continues to build his
research interests, which are focused on image guided therapy for cancer. We received IRB approval for a phase 2
HCC study evaluating a new drug combating the hypoxic response in combination with transarterial embolization.
Dr. Rilling will be national PI for an upcoming multi-center clinical trial looking at an arterial embolization medical
device system. He will also be PI for a multi-center, randomized cancer trial comparing CIS-GEM chemotherapy
with and without Y-90 as first line treatment in patients with unresectable intrahepatic cholangiocarcinoma.
• Vice Chair, Radiology Faculty Affairs, Sean M. Tutton, MD, FSIR continues to work on the development of
techniques for image guided orthopedic applications. Dr. Tutton also has the largest cohort of patients with extra-
abdominal desmoids in the country and recently published, in the Journal of Surgical Oncology, his innovative
approach to treat this incurable cancer. Additionally, he is the PI on all MR guided Focused Ultrasound clinical
trials currently underway here at MCW/FH. He is currently developing an international registry to track safety and
efficacy of MSK interventions. He is also collaborating on a protocol evaluating the abscopal effect of ablation in
combination with immunotherapy in a mouse model. Dr. Tutton developed a research protocol that surveyed, on a
national level, the current training that interventional radiologists get in palliative care and a manuscript is in
process.
• Chief of the Clement J. Zablocki VA Medical Center, Robert A. Hieb, MD, FSIR is serving as PI for the JET RANGER
study which is evaluating whether Jetstream atherectomy followed by drug coated balloon improves target lesion
revascularization at 1 year compared to balloon angioplasty followed by drug coated balloon in the treatment of
complex lesions in femoropopliteal arteries. Dr. Hieb is also the lead in a local study that applies a novel software
system to post process angiographic images in patients with critical limb ischemia (CLI). The software “removes”
the blood vessels to view the underlying parenchyma for blood flow and assess for changes post treatment.
• VIR Division Chief, Eric J. Hohenwalter, MD, FSIR is PI for several clinical trials. He completed enrollment of
patients in the PRESERVE study which evaluated the safety and effectiveness of IVC filters. He is also PI for a
prospective study of a novel class of software working with Siemens Medical Solutions, USA, Inc. Dr. Hohenwalter
is actively recruiting for the C-TACT trial. CTRACT is a NIH-funded randomized controlled trial that is examining
new treatments for vein damage caused by blood clots (DVT). Patients with established moderate to severe Post-
Thrombotic Syndrome will be randomized to either endovascular therapy (EVT) or No-EVT treatment groups. All
study patients in both groups will receive active treatment for their leg problem and will be monitored
closely. This trial aims to understand which treatment strategy is most effective in improving patients’ symptoms
and quality of life. Later this year, Dr. Hohenwalter plans to start enrollment in an investigator initiated trial in
collaboration with cardiology and GI physicians. Funded by the Radiological Society of North America (RSNA), the
study will determine the impact of the transjugular intrahepatic portosystemic shunt (TIPS) procedure on cardiac
function.

MCW Research Overview
Jump to Table of Contents 256
• Parag J. Patel, MD, MS, FSIR serves as PI for BEST-CLI which is a multicenter trial of endovascular vs. open surgical
revascularization in patients with CLI and infrainguinal peripheral arterial occlusive disease who are candidates for
both treatments.
• Co-Vice Chair, Radiology Research, Sarah B. White, MD, MS, FSIR continues work in her translational research
laboratory at MCW with an emphasis on interventional oncology. She recently started her second term on the
MCW IACUC committee. She continues to run the Medical Student Summer Research program, and this year the
Division welcomed 2 medical students. Through the Society of Interventional Radiology (SIR) a third medical
student was funded to spend time in VIR participating in research. Additionally, Dr. White organized Radiology’s
participation in hosting 2 SPARCC (Student-Centered Pipeline to Advance Research in Cancer Careers) students.
The 2 students each had a 2-week rotation observing and learning about interventional and digital radiology and
the research done in the department. Dr. White continues to be PI for the RETNET trial, evaluating the efficacy of
liver directed therapy in metastatic neuroendocrine cancer. On a national level, Dr. White continues to serve as the
Chair of the Clinical Research and Registries for the Society of Interventional Radiology.
• Alexandra H. Fairchild, MD has been working on a quality improvement project with the purpose of educating
Radiology and VIR residents on procedural consenting skills. Dr. Fairchild has been instrumental in manuscript
development for a project that evaluated the palliative care education among interventional radiology fellows.
• Matthew J. Scheidt, MD recently joined the group. He will be PI for an upcoming study assessing the safety and
effectiveness of a new type of IVC filter. Dr. Scheidt has also provided research mentorship to trainees and
medical students. Due to his excellent instruction he was awarded the 2019 Teacher of the Year by the 2018-2019
VIR fellows.

MCW Research Overview
Jump to Table of Contents 257
Surgery
The Medical College of Wisconsin Department of Surgery, led by Chairman Douglas Evans, MD, is dedicated to laboratory,
translational, and clinical research in all nine clinical divisions including Adult Cardiothoracic Surgery, Colorectal Surgery,
Congenital Heart Surgery, General Surgery, Pediatric Surgery, Surgical Oncology, Transplant Surgery, Trauma and Critical Care,
and Vascular and Endovascular Surgery. The Department’s dedication to research is further demonstrated in the recent
addition of the Division of Research. Research efforts by faculty, residents, and medical students continue to have resulted
in numerous research manuscripts published, research talks and posters presented, scientific meetings conducted,
collaborations fostered and funding received.
Surgery faculty worked one-on-one with a significant number of medical students in the Scholarly Pathways program during
the 2018-19 academic year. In addition, a large number of the student–faculty pairings were undertaken in the “Physician
Scientist Pathway” whereby the surgeon mentors a student on his or her own research project throughout the academic year.
Division of Research
Since the founding of the DOS Division of Research (DoR) in June 2017, the Division has been actively working to build
infrastructure to facilitate research, promote research education and dissemination, and advance research activities in the
Division of Research and Department of Surgery as a whole.
Key achievements include establishment of a monthly Surgery Research Conference (SRC), development and continued
enhancement of the DoR website, management of the department biostatistics integration agreement, design and
implementation of a monthly research newsletter “On the Cutting Edge,” launch of a campus-wide Clinical Research Power
Lunch series, formation of a centralized supplemental clinical research service, and, most recently, initiation of a department
grant application support service (SurPASS).
For students interested in identifying a research mentor in the Department of Surgery and do not have an established
connection, please contact Krissa Packard at kpackard@mcw.edu, who may facilitate an introduction with a faculty member.
Division faculty and their research interests:
Gwen Lomberk, PhD, serves as the Chief for the Division of Research, Director of Basic Research and Associate Professor of
Surgery and Pharmacology & Toxicology. Dr. Lomberk’s research program is broadly focused on the epigenetic landscapes
that characterize subtypes of pancreatic cancer (PDAC) and refining the utility of epigenetic inhibitors for treatment and re-
sensitization to conventional therapies. Epigenomic-based pharmacology has the potential to serve as a robust tool to
improve the treatment of PDAC. Her laboratory seeks to contribute to the field of experimental therapeutics through
combined inhibition of genetic-to-epigenetic pathways, as an important and provocative consideration for harnessing the
capacity of cell cycle inhibitors in efforts to enhance future use of epigenetic inhibitors.
Young-In Chi, PhD, Assistant Professor, recently joined us from Kyongpook National University Medical Center in Daegu,
Korea where he was a Research Professor in the Center for Drug Discovery and Development for Diabetes and Metabolic
Disease. Dr. Chi is a member of Dr. Raul Urrutia’s team in the Genomic Sciences and Precision Medicine Center and will be
conducting basic science research in the areas of molecular modeling, variant analysis, and precision medicine of pancreatic
cancer.

MCW Research Overview
Jump to Table of Contents 258
Michael James, PhD, has a laboratory focused on understanding key tumor cell survival and therapy resistance mechanisms
and exploiting them for better cancer therapy. Broadly, his expertise lies in molecular and cellular pathobiology of cancer. He
applies this expertise to the functional evaluation of novel tumor-associated proteins. The application of murine modeling,
cell biology and molecular biology techniques has allowed him to elucidate CLPTM1L/CRR9 as a novel anti-apoptotic oncology
target that is necessary for oncogene-induced transformation and tumorigenesis. Dr. James has developed disease-
representative, patient-derived, 3D organoid models of pancreatic cancer in collaboration with Drs. Evans and Tsai, building
upon their surgical biorepository for pancreatic cancer. These personalized models have been utilized in the study of stromal
and immune interaction with pancreatic tumor tissues.
Angela Mathison, PhD, Assistant Professor, joined the Department of Surgery in August 2018 from the Genomic Sciences and
Precision Medicine Center where she is the Technology Development Director. Dr. Mathison’s research focuses on the role
epigenetics play in the development and progression of pancreatic cancer and the potential to target these cellular
mechanisms for novel therapies.
Raul Urrutia, MD, serves as the Director of the Genomic Sciences and Precision Medicine Center, Warren P. Knowles
Professor of Genomics and Precision Medicine and Professor in the Department of Surgery. Dr. Urrutia’s laboratory focuses
on precision medicine as it applies to pancreatic cancer, as well as other diseases. Precision Medicine is a clinical discipline
that was born from basic science in genetics, as well as engineering, representing a translational science “par excellence”
with an actual marriage of basic science with clinical science. Through the combination of three innovative tools of Cancer
Precision Medicine, namely multi-omics, computational modeling, and patient-derived models, his research program seeks
to identify new mechanisms, diagnostic markers, and therapeutic targets for pancreatic cancer. His laboratory has been
focused on investigating how epigenomic regulators work as nuclear effectors of common mutations (e.g. KRAS) associated
with human pancreatic diseases.
Division of Cardiothoracic Surgery, Adult
David Joyce, MD is the Site Principal Investigator for the pilot study “Quantification of Cell Free DNA to Determine Rejection
Following Lung Transplantation” sponsored by TAI Diagnostics, Inc. The objective of this study is to quantify levels of
circulating donor-specific cell free DNA in lung transplant recipients. The study will allow investigators to describe
relationships between cell free DNA and important clinical events, such as rejection, which may allow use of this technology
as a noninvasive alternative to biopsy for monitoring the health of transplanted lungs.
Dr. David Joyce is also the Principal Investigator for the compassionate use of “Heart-Plug Used for LVAD Explant”. The
objective of this study is to plug the hole in the apex of the heart after an LVAD explant. This procedure has been performed
successfully on one patient, with more to follow. MCW is currently the only site in the United States to receive IRB
compassionate use approval for this procedure.
Dr. David Joyce leads the “SynCardia 70cc Total Artificial Heart (TAH-t) for Destination Therapy (DT)” and the “SynCardia 50cc
Temporary Total Artificial Heart (TAH-t) as a Bridge to Transplant (BTT)” clinical trials at MCW. The Total Artificial Heart is a
pulsatile biventricular device that replaces the heart’s two ventricles and four heart valves, relieving the heart’s workload by
pumping blood to both the lungs and the body. The purpose of these studies is to evaluate whether the TAH-t can support
patients with life-threatening irreversible biventricular heart failure who are not candidates for a left ventricular device or
heart transplantation. The 50cc TAH is used for patients with chest cavities that are too small for the 70cc TAH.
Dr. David Joyce is the MCW Principal Investigator for the “TandemHeart Experiences and Methods THEME Registry”. The
TandemHeart percutaneous extracorporeal ventricular assist system is used to support circulation. It is anticipated that
analysis will provide insight into disease defining characteristics resulting in the clinical decision to use TandemHeart for
mechanical support and enhance knowledge of best practice regarding clinical management, weaning and removal.

MCW Research Overview
Jump to Table of Contents 259
Lucian Durham, MD, PhD is the MCW Principal Investigator for the “Organ Care System (OCS
TM
) Lung Thoracic Organ Perfusion
Post Approval Registry”. The OCS Lung System is a portable organ perfusion, ventilation, and monitoring medical device
indicated for the preservation of donor lungs in a near physiologic, ventilated and perfused state prior to lung transplantation.
Chart Review Studies:
• Short and Long-Term Outcomes in Mechanical Circulatory Support (MCS) Devices (D. Joyce)
• Determining if Use of Bipolar Sealers During LVAD Implantation Reduces Take-Back Rates for Bleeding (D. Joyce)
• Differences in CardioMEMS Pulmonary Artery Pressure Readings in Heart Failure Patients with Reduced vs. Preserved
Ejection Fraction (D. Joyce)
• Case Study Report of Patient Outcomes in Mechanical Circulatory Support in Cardiogenic Shock: Comparing Impella,
IABP, and ECMO (D. Joyce)
• The Clinical and Biochemical Effects of Thiamine, Asorbic Acid, and Low Dose Steroid on Cardiopulmonary Bypass
Associated Vasoplegia (D. Joyce)
• A Bridge to the Fridge? Changes in BMI Post Left Ventricular Assist Device Implant (D. Joyce)
• Percutaneous Right Internal Jugular and Right Subclavian Arterial Biventricular Support In The Management Of Adult
Cardiogenic Shock (D. Joyce)
• Long Term Efficacy and Safety of Epicardial Ablation for Paroxysmal Atrial Fibrillation (D. Joyce)
• Use of Recombinant Factor VIIa in Complex Aortic Surgery, a Single Center Experience (C. Rokkas)
Manuscripts:
Outcomes of intracoronary shunting in off-pump coronary artery bypass grafting and left ventricular dysfunction: A single-
center prospective randomized control trial
Smith NJ, Miles B, Cain MT, Joyce LD, Pearson P, Joyce DL.Minimally invasive single-vessel left internal mammary to left
anterior descending artery bypass grafting improves outcomes over conventional sternotomy: A single-institution
retrospective cohort study. J Card Surg. 2019;1-8. https://doi.org/10.1111/jocs.14144
Division of Congenital Heart Surgery
The Division of Congenital Heart Surgery is actively involved in clinical and translational research to improve outcomes for
children with congenital heart disease (CHD). Our team of highly skilled scientists are successful principal investigators,
mentors and co-investigators on numerous studies in collaboration with many MCW departments and external institutions.
Viktor Hraska, MD, PhD leads a multi-disciplinary team that is testing and validating a NIR imaging system meant to provide
adequate contrast for anatomical and functional assessment of thoracic duct during surgery. Dr. Hraska received We Care
funding to support a pilot study that is studying neonates undergoing the Norwood operation with the intent to optimize
cardiopulmonary bypass to support cerebral and somatic perfusion during arch reconstruction. Dr. Hraska is also studying
pulmonary cell plasticity during single ventricle palliation and the hydrodynamics of arch reconstruction in HLHS.
Dr. Ronald K. Woods, MD, PhD is an investigator on 16 active clinical or basic science studies. His research includes clinical,
surgical, quality of life, and value improvement/ quality assurance initiatives, as well as laboratory surgical investigations that
utilize animal models. He is the site PI for 2 large multicenter studies and has organized a multicenter registry to evaluate
mechanical circulatory support in single-ventricle patients. He regularly mentors medical students on clinical projects which
often lead to podium presentations and publications.
Michael E. Mitchell, MD and Aoy Tomita-Mitchell, PhD manage the Mitchell lab. The long term goal of the Mitchell lab is to
understand how the integration of genetic and genomic information with clinical variability and clinical outcomes in CHD can
be used to identify predictors of clinical outcomes in CHD, and to understand mechanisms of healing and plasticity following
surgical repair. Dr. Michael Mitchell is PI of the CHD Tissue Bank, a biorepository of DNA and surgical discards from CHD
patients. He is the PI of a HHI Innovation grant investigating the role of the MYH6 gene in Hypoplastic Left Heart Syndrome
(HLHS) using patient specific induced pluripotent stem cells. Dr. Aoy Mitchell and her collaborators received a CTSI grant to
study the effect of MYH6 variants on cardiomyocyte biomechanics and patient outcomes in HLHS. She and her collaborators

MCW Research Overview
Jump to Table of Contents 260
have also received a grant from the Greater Milwaukee Foundation to bioprint patient-specific cardiac cells on a 3D tissue
construct. Other significant studies in the Mitchell lab include investigating the etiology of Ebstein’s Anomaly with Left
Ventricular Noncompaction, and testing a Newborn Screening assay for 22q11.2 Deletion Syndrome. The lab is also exploring
the role of metakaryotic stem cells in transplant atherosclerosis, coronary artery disease, and progressive pulmonary venous
stenosis. Dr. Michael Mitchell is also the PI of a multi-site, five year, NHLBI/NIH R01 grant to study cell-free DNA in cardiac
transplant rejection.
Professor John Baker's research program serves as a nexus to translate basic science discoveries into clinical applications. Dr.
Baker is studying why survivors of childhood cancer, who have been treated with radiation therapy, have an increased risk
for heart disease and how to mitigate this deleterious outcome. Dr. Baker is funded by NASA to determine the increased risk
for developing degenerative cardiovascular disease from exposure to components of space radiation. During exploratory
missions to the Moon and Mars, astronauts will be exposed to penetrating galactic cosmic rays and solar particles. Ground-
based animal studies are being used to assess the increased risk for developing degenerative cardiovascular disease.
Division of Colorectal Surgery
The research efforts within the Division of Colorectal Surgery remain robust. Dr. Kirk Ludwig continues as the institutional
principal investigator for a Cooperative Group Colorectal Cancer Trial at Froedtert and MCW Cancer Center. The purpose of
the trial is to explore the use of neoadjuvant chemotherapy for treatment of locally advanced rectal cancer. Dr. Ludwig also
serves as the Division Chief and holds the Vernon O. Underwood Endowed Chair. Under his supervision, the Division has
begun to carefully track functional outcomes in those undergoing resections for rectal cancer and the treatment of anal
cancer. Dr. Ludwig has a national reputation as an expert in the surgical treatment of rectal cancer with special emphasis on
sphincter sparing techniques.
Dr. Mary Otterson maintains a primary clinical and research focus on inflammatory bowel disease. She is currently the MCW
site PI for a prospective, multi-institutional study evaluating bowel and sexual function following ileal pouch anal anastomosis
surgery with the hopes of identifying surgical and disease-specific factors predictive of improved function. Furthermore, she,
along with the other faculty in the Division of Colorectal Surgery, are participating in the ADMIRE-CD II trial, a phase III,
randomized, double blind, parallel group, placebo controlled, international, multicenter study assessing the efficacy and
safety of adult allogeneic expanded adipose-derived stem cells for the treatment of complex perianal fistula(s) in patients
with Crohn’s disease.
Dr. Timothy Ridolfi recently completed a 3-year project aimed at evaluating the changes in enteric nervous system following
low anterior resection. This work allowed him to complete a Master’s Degree in Clinical and Translational Science. He is also
interested in the evaluation for complete response in the setting of neoadjuvant therapy for rectal cancer. This work is done
in collaboration with the Departments of Pathology, Radiology, and Biophysics and relies heavily on advanced MRI techniques
that are currently only offered at MCW. Additionally, Dr. Ridolfi is using the Vizient dataset, which includes outcome data
from more than 100 medical centers, to evaluate the most beneficial aspects of enhanced recovery after surgery programs
in regard to colon and rectal surgery.
Dr. Carrie Peterson continues to pursue her research interests in minimally invasive colorectal surgery and surgical outcomes.
She is heavily involved in several research projects evaluating improvements in quality and perioperative process
improvements. Along with the others in the Division of Colorectal Surgery, Dr. Peterson is participating in a prehabilitation
project in the frail undergoing colon resection. The project is aimed at both improving frailty preoperatively as well as
improving postoperative functional recovery.
Dr. Katherine Hu continues as the 2018-2020 Colorectal Research Resident. Dr. Hu is completing her General Surgery
residency at MCW and will be working with the Division for 2 years. She has a very active role in the multitude of current
ongoing projects within the Division. She is currently compiling MCW patient data for our participation in an international,
multi-institutional effort to benchmark values for best outcomes following colorectal surgery for patients with varying
preoperative risk factors.
MCW Research Overview
Jump to Table of Contents 261
Utilizing funds from the Lachman Family Summer Research Student Foundation and the Quasi Endowment, this year, our
Division supported the summer research efforts of one medical student. Student Doctor Tara Mather investigated racial
differences in HPV infections and subsequent formation of anal dysplasia. The Division always welcomes medical students to
actively participate in clinical research projects.
Kathryn Hoffman continues in the position of Clinical Research Coordinator to assist in the organization and successful
completion of the ever-expanding list of research projects within the Division.
Division of General Surgery
The Division of General Surgery supports the Department’s commitment to excellence in education and research. Over the
2018-2019 academic year, faculty and research staff collaborated to develop 17 new research protocols, showcased the
institution’s innovative efforts through presentations at local, regional, and national meetings, and brought in over $350,000
in research funding. Throughout the academic year the division faculty mentored 19 medical students and 7 general surgery
residents. Our research is focused in the domains of foregut surgery, bariatric surgery, and hernia surgery.
Bariatric Surgery: The bariatric surgery program at Froedtert and the Medical College of Wisconsin is accredited as a
Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) Comprehensive Center with
Adolescent Qualifications. Accreditation requires an annual Quality Improvement (QI) Project. The 2018-2019 QI project was
led by Rana Higgins, MD and Tammy Kindel, MD, PhD who also collaborated with faculty from the Department of Anesthesia
to develop a randomized, prospective study on the impact of preoperative carbohydrate loading on postoperative nausea
and vomiting. Throughout the academic year the division’s faculty, staff, residents, and students published multiple peer-
reviewed bariatric surgery manuscripts in journals that including Surgery for Obesity and Related Diseases, JAMA Surgery,
Surgical Endoscopy, Obesity Surgery, the American Journal of Surgery, and Surgery.
Foregut Surgery: In the 2018-2019 academic year, the division participated in numerous multi-institutional sponsored trials
on gastroesophageal reflux disease (GERD) surgical outcomes using implantable medical devices. We continued to review
long-term outcomes for patients following surgery that received an implanted magnetic sphincter augmentation device
(LINX). Faculty continued to examine long-term patient experiences following implantation of a gastric electrical stimulation
device (Enterra) in patients with medically refractory gastroparesis. The Division presented findings in foregut surgery
outcomes at Wisconsin Surgical Society, Academic Surgical Congress, and Society of American Gastrointestinal and
Endoscopic Surgeons (SAGES). Peer-reviewed manuscripts were accepted to Surgical Endoscopy, the Journal of
Gastrointestinal Surgery, and Surgery.
Hernia Surgery: Sponsored and investigator-initiated studies in the hernia domain included studies designed to evaluate
quality and recovery outcomes following implantation of various types of mesh. In the 2018-2019 academic year, the division
joined the Medtronic Parietene™ DS Composite Mesh in Ventral Hernia Repair Study under Dr. Matthew Goldblatt. The
Division continues to participate in the Americas Hernia Society Quality Collaborative, a national quality improvement effort
aimed at improving the quality of care provided to hernia patients. The Division’s hernia research efforts were presented
locally at MCW, regionally at the Wisconsin Surgical Society, and nationally at meetings of the Academic Surgical Congress,
Southwest Surgical Association, and the International Hernia Congress.
The Division of General Surgery is proud of the quality people and projects it produces year after year and looks forward to
continuing this work in 2019-2020 and beyond.

MCW Research Overview
Jump to Table of Contents 262
Division of Pediatric General and Thoracic Surgery
The Division of Pediatric General and Thoracic Surgery houses a highly successful and thriving research program with
prestigious studies in both the bench and clinical science. In our bench research, Dr. Kirkwood Pritchard has an NIH R01 grant
to research mechanisms of oxidative stress and inflammation in sickle cell disease. His interests also include examining the
role of oxidative stress and inflammation in murine models of stroke, multiple sclerosis and rodent models of hyperoxic lung
injury in neonatal rat pups. Dr. Pritchard celebrated a new licensing agreement for MCW startup ReNeuroGen, LLC. to develop
and test a new treatment for secondary brain injury after stroke, which can result in significant brain damage and create
severe disability. ReNeuroGen has been funded by the Small Business Innovation Research (SBIR) program, and made it into
the top 12 of the 2018 Wisconsin Governor's Business Plan Competition.
Our clinical research program is one of the founding members of the Midwestern Pediatric Surgical Consortium (MWPSC). As
part of the MWPSC, a number of our surgeons participate in multi-institutional clinical studies examining congenital
pulmonary airway malformations, anorectal malformations, spontaneous pneumothorax, esophageal atresia and
tracheoesophageal fistula (EA/TEF), adolescent breast masses, treatment of pediatric adenexal masses, and appendicitis.
One of the first major initiatives of the MWPSC was led by Dr. Dave Lal to examine the treatment of EA/TEF. Dr. Lal is also
the site PI for the MWPSC clinical trial funded by PCORI to investigate parental choice in the operative versus non-operative
management of acute appendicitis. Dr. Lal is a site PI for a study working to reduce the number of unnecessary
oophorectomies in girls.
Under the direction of Dr. David Gourlay, MWPSC developed a protocol to prospectively study venous thromboembolism
prophylaxis in trauma patients. Dr. Gourlay is also co-Investigator on an NIH study to investigate mechanisms of injury and
need for a trauma center in pediatric patients.
Dr. Casey Calkins is our site’s PI in an NIH-sponsored study led by Vanderbilt University examining early versus late repair for
neonates with inguinal hernias, in what is known as the HIP study. Dr. Calkins is also a steering committee member of a
national registry of anorectal malformations (Pediatric Colorectal and Pelvic Learning Consortium). This multi-center
consortium will investigate variations in care of these patients that lead to optimal outcomes. PCPLC recently began a study
to investigate Patient and Parent Reported Outcome Measures (PROMs) of patients with colorectal disease.
Dr. Amy Wagner oversees the GOOD study, a large, multi-institutional study endorsed by the North American Fetal Therapy
Network examining the outcomes of early versus late delivery in prenatally diagnosed gastroschisis. The GOOD Study is
currently seeking funding from both the March of Dimes and the NIH. Additionally, she has a number of research projects
related to maternal-fetal care.
Dr. Keith Oldham is the PI of Children’s Hospital of Wisconsin’s Clinical Outcomes Registry (COR), which continues to collect
annual quality of life data from over 500 neonatal surgery patients. Dr. Oldham current research relates to optimize pediatric
surgical outcomes and improving global access to pediatric surgical care.
Dr. Sabina Siddiqui is the division’s global health liaison, studying surgical illness across the globe and a member of Global
Initiative of Children Surgery (GICS). Dr. Siddiqui is establishing partnerships to examine improvement is global surgical care.
Dr. Siddiqui is also a founding Board member (and Chief Medical Officer) of Brio Device LLC, a company who develops
technology to increase efficiency and effectiveness in airway management. Dr. Siddiqui is also examining the role of implicit
racial bias and its potential impact on patient care.
Dr. John Densmore has a strong clinical interest in Congenital Chest Wall Malformations and currently investigating the use
of non-operative means to correct chest wall anomalies. He is active in research related to identifying variabilities that impact
the cost of pediatric surgical care.
Dr. Thomas Sato spearheaded a study examining the clinical course and healthcare costs of patients with acute appendicitis,
specifically looking at differences of duration of symptoms at time of presentation, perforation rates, length of hospital stay,
and complications of patients with private insurance and patients who are uninsured or are covered by government assisted
programs.
Dr. Kyle Van Arendonk is currently investigating the impact of patient size on port placement. Dr. VanArendonk is also
examining surgical treatment modalities for patients with gastroesophageal reflux disease.

MCW Research Overview
Jump to Table of Contents 263
Lastly, our program has several retrospective chart review projects, including projects investigating the pain management
and opioid use in appendicitis patients, outcomes in ovarian torsion, management of intussusception, and surgical site
infection prophylaxis in neonates.
Division of Transplant Surgery
The Research Program in the Division of Transplant Surgery focuses on liver and kidney transplantation and surgical diseases
of the liver and bile duct. As a multi-faceted program, basic science research is undertaken in the laboratory of Chief and
Professor Johnny Hong, MD; clinical science and translational research is pursued by transplant faculty and researchers at
Froedtert Hospital, Children’s Hospital of Wisconsin, The Blood Center of Wisconsin, UW Milwaukee, Concordia University,
Cleveland Clinic, and Washington University in St. Louis. MCW Transplant Surgeons have served over 5000 patients since
1967.
Our comprehensive clinical data from years of patient care is a critical element of the Transplant Division’s growing research
infrastructure. As part of the Transplant Surgery’s academic infrastructure over the years, an extensive clinical database has
been maintained and, in 2014, with IRB approval, transferred to a REDCap database entitled the Solid Organ Transplantation
Data Bank. This bank has data available for program management, quality assurance, and research.
Another element of the research infrastructure is Dr. Johnny Hong’s basic science laboratory housed in the Cardiovascular
Research Center. Current research is focused on regulated hepatic reperfusion, to mitigate the adverse effects of ischemia
and reperfusion injury (IR) in porcine circulatory death liver transplant model. In addition, Dr. Hong’s lab is studying the
effects of hepatic steatosis on IRI in a rat model, and the influence of extracellular adenosine in a mouse IRI model.
Dr. Hong was just recently awarded a Department of Surgery We Care Award for two years. Partnering with Dr. Raul Urrutia
in the GSPMC, the award focuses on The Effects of Ischemia and Reperfusion Injury in Liver Transplantation on Epigenetic
Profiles.
Current ongoing studies involving Divisional Faculty in academic year 2018-2019 include the following:
1. Determine the effect of regulated hepatic reperfusion in a DCD swine liver transplant model and mitigate IRI through
novel treatment.
2. Assessment of hepatic IRI measured by bile transporter expression in a rat IRI model with hepatic steatosis.
3. Investigate the influence of extracellular adenosine signaling on leukocyte-mediated hepatic injury in a mouse IRI
model.
4. Pre-Habilitation in Patients Awaiting Liver Transplantation.
5. Incompatible Organ Transplantation in High Risk Donors.
6. Cycle Ergometer Therapy in Transplant ICU patients.
7. Liver Biopsies to study Ischemic Reperfusion Injury
8. A Randomized, Controlled, Open Label Clinical Trial of Thymoglobulin Induction and Extended Delay of Calcineurin
Inhibitor Therapy for Renal Protection after Liver Transplantation.
9. Staged Bile Duct Reconstruction in the Share 35 Era
10. Outcomes in Transplant Mental Health Group Therapy
11. Platelet Refractoriness and Alloimmunization in Liver Transplantation
12. The Effect of Race on Transplant Outcomes. A single center experience.
Collaborative efforts with other MCW researchers include:
a) Application of novel cardiac blood enyzyme tests for the solid organ transplant population under the direction of
Michael Mitchell, MD, Professor of Surgery in the Pediatric Congenital Cardiac Surgery Division at MCW, sponsored
by TAI Diagnostics.
b) Addiction in End Stage Renal Disease: Identification of Neurocognitive Profiles and Risk Factors for Transplant with
David Sabsevitz PhD, Professor of Clinical Neuropsychology at MCW.

MCW Research Overview
Jump to Table of Contents 264
Division of Trauma & Critical Care
The Division of Trauma and Acute Care Surgery focuses its research in several areas of expertise including: emergency
intervention, evaluation of current practices for improved outcomes/recovery of trauma related injuries, measuring patient
outcomes after injury, cost effectiveness, surgical infections, palliative care, early diagnosis for symptoms of post-traumatic
stress disorders, ethics, educational research, quality, health disparities, patient safety, geriatrics, nutrition, and disease
modeling. These clinical entities fall under the three chief timeframes during the continuum of patient care from Pre-
Hospital/Acute to Subacute to the Long-Term Recovery/Rehabilitation phases. Throughout the 2019 academic year, we have
had internal and external funding, including from non-profit, government and industry sources.
Dr. Marc de Moya’s, Chief of Trauma & Acute Care Surgery, research focus is in prospective controlled trials for improving
surgical outcomes in trauma, acute care surgery, and surgical critical care patients. In addition, he is growing his research
experience in Global Surgery.
Dr. Marshall Beckman’s research is focused in bioethics.
Dr. Tom Carver completed a randomized controlled trial of early ketamine administration in adult and elderly multiple rib
fracture patients in hopes to reduce pain and to decrease overall opiate requirements and side effects.
Dr. Panna Codner is currently funded to research dysbiosis in the traumatically injured patient, as well as focusing on the role
of nutrition and frailty in patient outcomes.
Dr. Terri deRoon-Cassini is funded to focus on developing acute neurobiological risk factors and treatment targets for PTSD
and depression in adult injured trauma survivors.
Dr. Chris Davis is investigating the role of the Stop the Bleed training on students and computed tomography prediction of
need for rib stabilization.
Dr. Chris Dodgion is researching the burden of surgical disease on global populations including in Haiti and utilizing national
databases to understand the incidence of acute medical issues in need of surgical intervention.
Dr. Anu Elegbede is studying the impact of a dedicated Geriatric Trauma co-management program with internal medicine.
Dr. Joshua Hunt utilizes advanced statistical methods to understand factors that constitute PTSD and the confluence in risk
for poor outcomes in those with and without a traumatic brain injury.
Dr. Jeremy Juern is conducting research on the utility of endoscopic retrograde cholangiopancreatography in bile leaks.
Dr. David Milia’s research focus includes a multicenter trial relate to venous thromboembolism in trauma patients,
complications related to tracheostomies, and incidence of UTIs in trauma patients.
Dr. Todd Neideen studies necrotizing soft tissue infections, evaluation of beta blockers in geriatric trauma patients, and
medical student perceptions of important residency attributes.
Dr. Jill Streams is studying gender disparities in trauma research authorship and trauma outcomes.
Dr. Colleen Trevino leads research focused on understanding the conversion from acute to chronic pain in adult injured
patients and developing novel models of multidisciplinary care to prevent chronic pain and psychological distress.
Dr. Travis Webb is leading research related to frailty in the geriatric trauma population and the impact of traumatic brain
injury on the elderly patient, as well as a focus on small bowel obstruction in the acute care surgery patient.
Continuing Research Education: Drs. Joshua Hunt and Panna Codner have completed the first year of the MCW CTSI Clinical
Research Scholars Program. Dr. Panna Codner has also started in the MS in Clinical and Translational Science program at
MCW.

MCW Research Overview
Jump to Table of Contents 265
Division of Vascular Surgery
The MCW Division of Vascular and Endovascular Surgery continued to expand its clinical research activities throughout the
Academic Year 2018/2019 by continuing a NIH trial in collaboration with the Division of Interventional Radiology and an aortic
device trial. Additionally, the division participated in several retrospective chart reviews, vascular device registries, and other
device trials.
Peter Rossi, MD, Chief of the Division of Vascular/Endovascular Surgery, as site PI (Principal Investigator) at FH (Froedtert
Hospital), is one of the top enrolling for “A Prospective, Multicenter, Non-Blinded, Non-Randomized Study of the RELAYPRO®
Thoracic Stent-Graft in Subjects with Traumatic Injury of the Descending Thoracic Aorta” with Bolton Medical. Dr. Rossi
continues to oversee the GREAT Registry (Global Registry for Endovascular Aortic Treatment Outcomes Evaluation). This
registry, sponsored by WL Gore, collects data on Gore vascular grafts utilized by the vascular surgeons at FH. Dr. Rossi is also
site PI for Gore’s study entitled “Evaluation of the GORE® EXCLUDER® Iliac Branch Endoprosthesis for the Treatment of
Common Iliac Artery Aneurysms or Aorto-iliac Aneurysms.” In this project, Dr. Rossi oversees the collection of data to assess
the outcomes associated with the use of the GORE® EXCLUDER®, an approved iliac graft. Dr. Rossi continues to oversee two
chart reviews he authored: “Vascular Surgery Groin Infections” and “Outcomes of Ruptured Abdominal Aneurysms”.
Vascular/Endovascular Surgery also continues to enroll with Parag Patel, MD, Interventional Radiologist, the NIH-sponsored
study entitled “BEST-CLI.” This trial is a randomized, multicenter, controlled trial, comparing the Best Endovascular versus the
best Surgical Therapy in patients with Critical Limb Ischemia. As of summer 2019, national enrollment has reached nearly
1800 patients with MCW as one of the top enrolling sites. The Divisions of Vascular and Endovascular Surgery and
Vascular/Interventional Radiology continue to collaborate on four active trials.
Dr. Rossi also recently acquired two ongoing Endologix clinical trials, the Nellix® EndoVascular Aneurysm Sealing System and
the LEOPARD trial, in which patients are randomized to the Endologix AFX® system or the leading competitor devices for
EVAR (Endovascular Aneurysm Repair) both continue to follow patients for outcomes.
Vascular surgeons, Brian Lewis, MD, Kellie Brown, MD, Michael Malinowski, MD, and most recently, Abby Rothstein, MD, are
co-investigators on open and accruing Vascular and Endovascular Surgery protocols and continue to author and co-author
articles and presentations with other division faculty including former Division Chief, Dr. Gary Seabrook and Charles Edmiston,
PhD. Dr. Michael Malinowski has 3 manuscripts in review for publications concerning medical school teaching and trends.
Several of our faculty are also involved in research at the Clement J Zablocki VA Medical Center where they have privileges
and conduct research trials.
Contributions to the division’s research efforts have also been made by MCW 2018/2019 Vascular/Endovascular Surgery
fellows, Nicholas Saguan, MD and Jacob Wood, MD, along with the department’s research residents, most notably, Nathan
Kugler, MD (who will be transitioning into Vascular/Endovascular Surgery Fellow this fall of 2019). Dr. Kugler has published
and presented at several conferences his “Outcomes Following TEVAR for Management of Complicated Acute Aortic
Syndromes”. Finally, medical students, our postdoctoral research fellow, and our research Nurse Coordinator, Beth
Weseman, RN are invaluable and remain critical elements to the success of the Vascular Surgery research program.
Division of Surgical Oncology
Section of Breast Surgery
The Section of Breast Surgery includes Amanda L. Kong, MD, MS (Section Chief), Caitlin R. Patten, MD, Miraj G. Shah-Khan,
MD, Alonzo P. Walker, MD, and Tina W.F. Yen, MD, MS. The group has an active clinical, translational and outcomes research
program, addressing the treatment and outcomes of both benign and malignant diseases of the breast. Funded health
services research related to breast cancer, its treatment and outcomes is performed in affiliation with MCW’s Center for

MCW Research Overview
Jump to Table of Contents 266
Advancing Population Science (formerly MCW’s Patient Care and Outcomes Research Center). Our faculty also collaborate
with the basic science faculty at the medical school on translational research projects.
As active members of the Cancer
Center, our faculty participate in
numerous clinical trials sponsored
by industry and the National Cancer
Institute through cooperative
groups, including the Alliance for
Clinical Trials in Oncology, NRG
Oncology, and ECOG-ACRIN cancer
research group. Tina Yen, MD, MS,
serves as the institutional principal
investigator for the Alliance for
Clinical Trials in Oncology
cooperative group and Alonzo
Walker, MD, is the institutional
surgical oncology leader for the NRG
Oncology cooperative group. These
trials examine different ways to
improve breast cancer treatment
involving new surgical approaches,
combination therapies, the delivery
of radiation, and new drug agents. In addition, the Breast Surgery Program maintains a multidisciplinary breast clinical
research database that is maintained by a dedicated program database coordinator, overseen by Amanda Kong, MD, MS, and
is an active participant in MCW’s Central Tissue Bank, which stores blood as well as healthy and tumor tissue for research
purposes.
Section of Endocrine Surgery
The Section of Endocrine Surgery has a robust research program, active in clinical, translational, and outcomes research,
focused on benign and malignant diseases of the thyroid, parathyroid, and adrenal glands. During the 2014 – 2019 academic
years, the Endocrine Surgery research program had nearly oral/poster presentations at the national/regional/local level and
published >35 peer-reviewed publications and book chapters. During the 2019-2020 academic year, the research program
continues to work with MCW medical students and Department of Surgery residents and fellows.
The Section of Endocrine Surgery maintains three prospectively-collected clinical databases (thyroid, parathyroid, and
adrenal), which serve as the foundation for the research program. In addition, the Section participates in the American
Association of Endocrine Surgeons (AAES) Collaborative Endocrine Surgery Quality Improvement Program (CESQIP), a quality
improvement program that allows for collection of longitudinal outcomes specific to Endocrine Surgery. Institutional
members of CESQIP include faculty from the Department of Surgery, Division of Surgical Oncology (Endocrine Surgery and
Hepatobiliary Surgery) and Department of Otolaryngology, Head and Neck Surgery.
Our faculty are also actively engaged in both the Surgical Oncology Tissue Bank and the MCW Central Tissue Bank to store
healthy and tumor tissue that would otherwise be discarded at surgery. This tissue is then made available to cancers
researchers who have obtained the proper institutional permissions to conduct research using it. The Section was a member
of The Cancer Genome Atlas (TCGA) Pheochromocytoma/Paraganglioma (PCPG) Working Group. The Endocrine Surgery
program was also one of the fourteen founding members of the Australian-American-Asian Adrenal Alliance (A5), a multi-
institutional collaborative on the study of adrenal disease.

MCW Research Overview
Jump to Table of Contents 267
Section of Gastrointestinal (GI) Surgery
The Gastrointestinal (GI) Section of the Division of Surgical Oncology’s active clinical, translational, outcomes and basic
science research program involves six GI surgeons, research scientists and staff, fellows, post-docs, and a myriad of medical
students. The GI section has been involved in research projects spanning both benign and malignant diseases of the
hepatopancreaticobiliary system (liver, pancreas, gall bladder) as well as sarcomas, peritoneal carcinomatosis, and other
gastrointestinal cancers as well as palliative care. This has resulted in multiple national oral presentations and publications.
The section is committed to developing novel investigator-initiated clinical trials. These include the current PANC trial, which
is an adaptive clinical trial utilizing biomarkers to guide total neoadjuvant therapy in pancreatic cancer and the SOFT trial,
which is a randomized controlled trial comparing neoadjuvant stereotactic body radiation as compared to conventional
radiation for pancreatic cancer. The pancreatic cancer trials are the top accruing clinical trials in the cancer center. As active
members of the MCW Cancer Center, Surgical Oncology GI Faculty also participate in numerous NIH-sponsored cooperative
group clinical trials coordinated by the Cancer Center Clinical Trials Office.
Since its inception the Surgical Oncology Tissue Bank has enrolled over 2800 patients. This bank stores blood throughout a
patient’s oncologic treatment from the time of diagnosis and throughout treatment. Benign and malignant pancreas, liver
and adrenal tissues that would otherwise be discarded at surgery are banked. The bank has been instrumental in a multi-
center NIH collaborative examining non-coding RNA for early detection of pancreatic cancer. Specimens have also been
utilized the development of a novel platform to perform chemotherapeutic testing on pancreatic cancers ex vivo and to
examine the germline variants of uncertain significance in patients with sporadic pancreatic cancer. The bank supports one
of five Post-mortem Tumor Donation Program which allows patients to donate their remains for pancreatic cancer research
following death. The Tissue Bank collaborates with multiple research collaborations including external collaborations with
MIT, Van Andel Institute, University of Wisconsin-Madison, and City of Hope, as well as internal collaborations within MCW.
Clinical databases maintained in GI Surgery Oncology included efforts in gastric, sarcoma, liver, pancreas, and regional
therapies. Outcomes research projects and manuscripts are abundant and have been extremely productive. Faculty have
contributed to over 26 peer-reviewed publications and 18 book chapters since 2017. Pancreatic cancer research has been
presented at 12 national meetings during this time, including the 138th American Surgical Meeting. Furthermore, the clinical
program supports infrastructure for innovative quality programs including the development of ERAS pathway following
pancreatectomy, longitudinal quality of life surveys for patients with pancreatic cancer, and the implementation of universal
genetic testing.

MCW Research Overview
Jump to Table of Contents 268
Urology
Biomedical research is a core component of the mission of the Department of Urology. To this end, the Department is actively
involved in both clinical and basic science research ranging from self-initiated to industry sponsored trials and single site to
collaborative, multi-institutional efforts. Urology residents and fellows are expected to actively participate in ongoing
research projects throughout their training.
Current research projects within the Department of Urology include:
Bladder cancer
• Evaluating various measures of oxidative stress associated with Bacillus Calmette–Guérin’s (BCG) effect on bladder
cancer
• Optimizing immunotherapy in the treatment of bladder cancer
• Outcomes of robotic assisted bladder cancer surgery
• Quality of life after urinary diversion
Prostate cancer
• Use of MRI as a tool in the surgical planning for prostate cancer
• Evaluation of robotic techniques to decrease the morbidity of radical prostatectomy
• Outcomes comparison between open and robotic prostatectomy
• Factors leading to readmission after prostatectomy
Kidney cancer
• Multicenter outcome assessment of robotic partial nephrectomy for large renal tumors
Genital issues/benign prostate disease
• Studying complications of HoLEP (holmium laser enucleation of prostate)
• Outcomes of surgery for buried penis
• Outcomes of surgery for giant genital condyloma
Urinary stone disease
• Outcomes of urinary stone treatment (multicenter study)
• Comparison of 2 different types of lithotripsy (stone disruption) for bladder stones
• Dietary modification in the management of urinary stones in obese patients
• Comparison of different laser fibers with respect to damage to ureteroscopes
Infertility
• Testicular tissue harvesting for research in stem cell isolation/cryopreservation with the hopes of reimplantation
after cure
• Genetic testing for evaluation of severe male factor infertility
• Outcomes research for men with male infertility and varicoceles
• Research in characteristics of men undergoing vasectomy

MCW Research Overview
Jump to Table of Contents 269
Voiding dysfunction
• Comparison of different injection techniques for injecting onabotulinum toxin (Botox) in the management of
neurogenic bladder
• Assessment of patient characteristics in neurogenic bladder patients with recurrent urinary tract infections
• Assessment of adequacy of improvement criteria in predicting long term efficacy of sacral neuromodulation for
overactive bladder
Education
• Use of robotic simulators in residency training
• Accuracy of resident surgical case logs
• Familiarity trends in successful urology residency match applicants




